Abstract
A thorough evaluation of the hip must include a comprehensive medical and surgical history focused on the hip joint, surrounding soft tissues, and the associated structures of the spine, pelvis, and lower extremities. These details can guide the physical examination and provide insight into the cause of the patient's chief complaints. A proper examination includes physical examination while the patient is in the upright, supine, prone, and lateral position, as well as an evaluation of gait. Guided by a thorough history, the physical examination enables the surgeon to distinguish between intra-articular and extra-articular contributors to hip pain, selection of appropriate imaging modalities, and ultimately supports medical decision making.
The understanding of hip pathologies has evolved, and concurrently more specific tests and focused physical examination are being employed to yield a more accurate and specific diagnosis. The subjective report of hip-related pain can be vague leading to difficulty with localization to a specific structure, due in part to the complexity and inter-relatedness of the regional anatomy and overlapping pain characteristics. However, a thorough history, including prior hip injury, is essential for evaluation of patients with hip pain.
Causes of hip pain can be divided into intra-articular and extra-articular pathology, and it is important to differentiate between several entities. Femoroacetabular impingement (FAI) is increasingly recognized as a common intra-articular cause of hip pain and may include labral tears (possibly with associated chondral lesions) and synovitis (Table 1). Extra-articular soft tissue causes include greater trochanteric bursitis, gluteus medius/minimus tendinopathy or tearing, iliopsoas or rectus femoris tendinosis, and hamstring tendinosis. Abnormalities in bony morphology may lead to impingement with hip motion during certain activities and result in abnormal bony contact; this may involve the greater trochanter, lesser trochanter, extracapsular femoral neck, ilium or ischium, resulting in classic FAI as well as iliopsoas impingement, subspine impingement, ischiofemoral impingement, and greater trochanteric-pelvic impingement (Table 1).1, 2
Table 1.
Common Intra- and Extra-articular Causes of Hip Pain
| Intra-articular Causes of Hip Pain | Extra-articular Causes of Hip Pain |
|---|---|
| • Labral tear | • Extra-articular bony impingement |
| • Loose bodies | • Iliopsoas tendonitis |
| • Femoroacetabular impingement | • Internal or external snapping hip |
| • Synovitis | • Abductor tears |
| • Tears of the ligamentum teres | • Greater trochanteric bursitis |
| • Chondral injury | • Femoral neck stress fracture |
| • Proximal adductor, hamstring, or rectus injuries | |
| • Piriformis syndrome | |
| • Deep gluteal syndrome | |
| • Sacroiliac joint pain | |
| • Athletic pubalgia | |
| • Osteitis pubis |
A recent systematic review identified the most common causes of hip-related pain in athletes including FAI (32%), athletic pubalgia (24%), adductor-related pathology (12%), and inguinal pathology (10%).3, 4 The potential overlap of these clinical entities requires integrating a detailed medical history, physical examination, and radiographic studies to develop an accurate diagnosis in this patient population presenting with hip pain.3 The accuracy of isolated physical examination for diagnosing FAI is limited because of etiologic heterogeneity of impingement and structural complexity of the hip joint.5 The purpose of this Technical Note is to describe a standardized step-by-step hip physical examination to better evaluate specific anatomic pain generators through physical examination tests and maneuvers.
Detailed History
A detailed history provides insight into a patient's pathologic condition and is the essential starting point for evaluation. A history of trauma or childhood hip disease such as slipped capital epiphysis or Legg-Calve-Perthes disease must be recorded and can help to focus the examination.6 Previous treatments, including medications, physical therapy, or other therapeutic modalities to address the hip pain, should be recorded along with their effectiveness. Specific hip pathology can be associated with participation in certain activities, so it is important to determine the type, intensity, and frequency of athletic activity performed currently and previously (including during adolescence). It is also important to gauge the patient's current activity level and expectations of treatment.
Locking, snapping, or other mechanical symptoms are common complaints associated with hip pain, and the inciting movements/activities can provide clues to symptom cause. Other important factors including localization of pain symptoms and associated paresthesia or neurologic deficits must also be identified. A study evaluating pain localization patterns of athletes with hip pathology reported groin, thigh, and buttock pain in 55%, 57%, and 71% of athletes, respectively.7
Because hip pain can be nonspecific, differentiating hip and lumbar spine pathology is challenging. A thorough lumbar spine examination should be included when evaluating the hip. The presence of a limp, groin pain, or limited hip internal rotation should lead the examiner toward hip pathology causing the pain and dysfunction, because athletes with limited internal rotation were 14 times more likely to have hip versus spine pathology.8 Intra-articular hip injections have commonly been used to differentiate intra-articular hip pain from extra-articular sources based on relief of symptoms.9 Khan et al.10 performed a systematic review of the utility of intra-articular hip injections in the diagnosis and management of FAI and found that pain relief obtained from an intra-articular hip injection supports the diagnosis of FAI.
General Physical Examination
After completing a detailed medical history, physical examination begins with assessment of the patient's general appearance, including body habitus, weight distribution, mood, and posture. We advocate a complete, albeit, brief physical examination of numerous systems including the head, ears, eyes, nose, throat, neck, respiratory, cardiovascular, abdomen, lymphatic, and skin. Many insurance providers and regulatory agencies require thorough medical documentation of the patient's complete physical examination despite the patient presenting for focused hip pain (Video 1).
Gait and Upright Examination
Gait evaluation is an essential component of the hip examination and certain gait patterns can predict a diagnosis before focused examination and provocative testing. Gait should be assessed with adequate space to allow 3 to 4 stride lengths in front and behind the patient. Antalgic gait, Trendelenburg gait, excessive internal or external rotation, and abnormal foot progression should all be assessed. Antalgic gait is a shortened stance phase due to ipsilateral lower extremity pain and is nonspecific to hip pathology. Trendelenburg gait is seen with abductor weakness or injury and is commonly seen with degenerative hips or after total hip arthroplasty. Single leg stance with the “hop test” is a functional assessment of the ability of the abductors to hold the pelvis in a balanced position. With the patient standing, lumbar lordosis and pelvic tilt can also be evaluated. Asking the patient to activate his gluteus maximus musculature may show correction of anterior pelvic tilt. A lack of correction can indicate weakness of the musculature or a fixed deformity. The performance of a single leg squat, which activates gluteal musculature, can be used to assess subtle abductor weakness or irritation associated with FAI or intra-articular pathology. Gait can also be evaluated ascending or descending stairs, an activity necessitating increased hip flexion compared with ambulation on flat surfaces, and may highlight symptomatic impingement or osteoarthritis.11
Hypermobility of joints (thumb, forearm, elbow, shoulder, and knee) should also be assessed if there is concern for connective tissue disorders or hip dysplasia with the Beighton score. A positive thumb-to-wrist examination, hyperextension of the knee and elbow beyond 5°, and a positive sulcus sign are findings suggestive of generalized hyperlaxity of the ligaments.12 The dial test is used to evaluate capsular laxity, and is discussed in the subsequent section.
Supine Examination
When comparing the examination techniques of several leading hip arthroscopic surgeons, the supine examination showed the greatest consistency.13 Inspection begins with a side-to-side comparative evaluation to identify quadriceps atrophy, leg length discrepancy, and pelvic obliquity. Palpation is less specific in hip than other joints but certain patterns, such as flexor tendinosis, are associated with hip pathology.
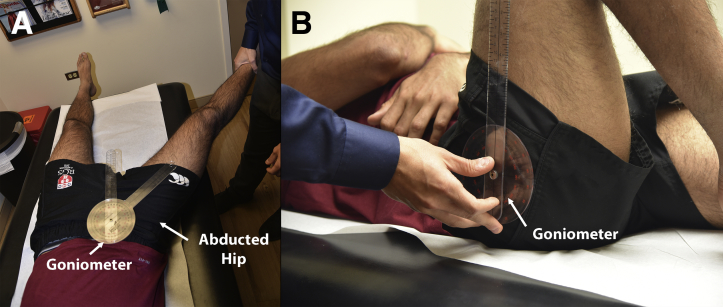
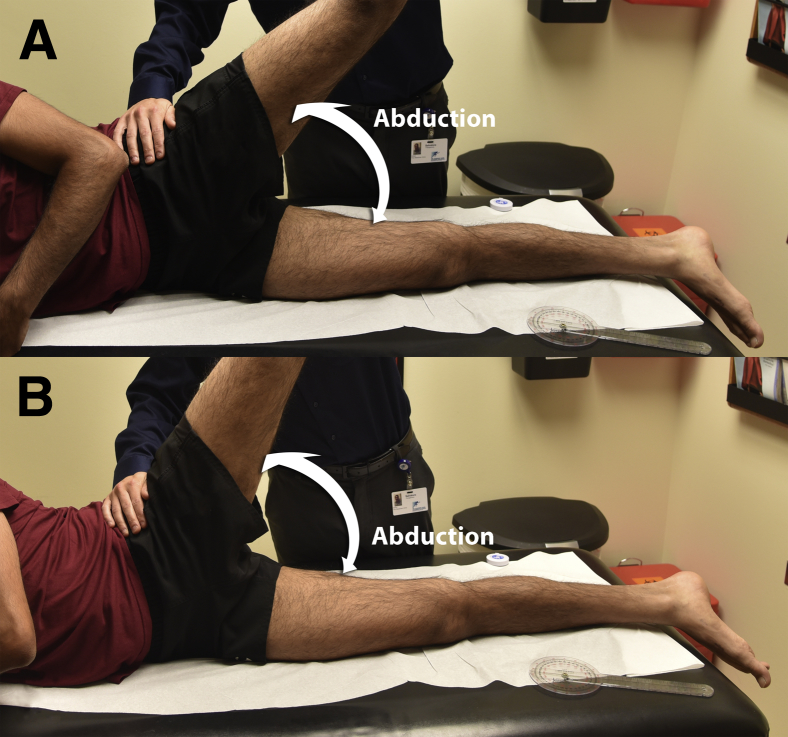
Palpation of bony prominences should be performed, including the anterior superior iliac spine, pubis, and ischial tuberosity. With the hip in an abducted and externally rotated position, the adductor musculature is palpated for tightness and tenderness, which may also be associated with intra-articular pathology. The “C” sign, where the patient cups his hand over the greater trochanter when asked to localize his pain, was found to be associated with intra-articular hip pathology.14 Range of motion is evaluated in the supine position with a goniometer (Fig 1). Passive range of motion of the symptomatic hip is compared with the contralateral side, and pain with each maneuver should be recorded. Hip forward flexion, internal and external rotation (with the hips flexed in the supine position), abduction, and adduction can be evaluated in both the supine and seated positions with the hip flexed to 90° (Fig 1).
Fig 1.
Photograph of a patient in the supine position during physical examination. To accurately determine the range of motion the use of a goniometer is advocated. As seen in this picture, the abduction (A) and forward flexion (B) measurements are being performed on a right hip.
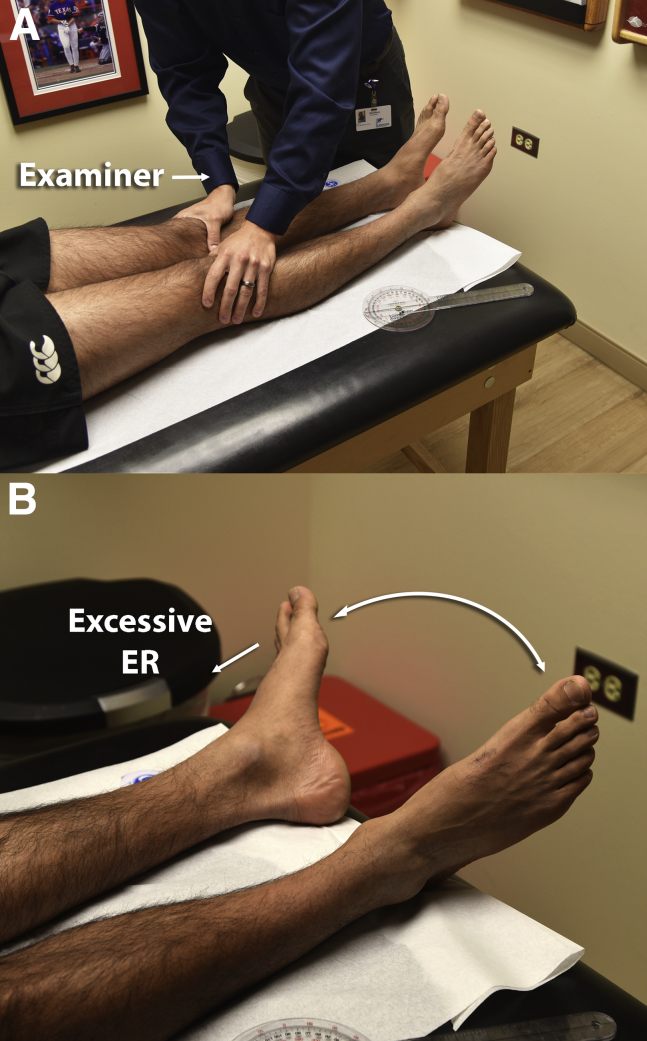
The dial test is then performed in the supine position to evaluate hip capsular hyperlaxity.15 The examiner places his hand on the femur and the tibia while internally rotating the lower leg (Fig 2A). The examiner then releases the limb allowing it to passively rotate externally (Fig 2B). A positive hip dial test occurs when there is external rotation beyond 45°, with the lack of a definitive mechanical endpoint. A study by our group reported the dial test findings in 426 patients evaluated for symptomatic FAI, and it was found that those with a positive test were 11 times more likely to have symptomatic instability and 89% had evidence of labral tearing at the time of surgery (Fig 2).16
Fig 2.
Photograph showing the dial test to evaluate capsular laxity. The examiner ensures that the hips are relaxed with the knees and toes in a perpendicular position to the examination table (A). The examiner then releases the legs, allowing them to fall into a naturally externally rotated position. Excessive external rotation in the effected leg (left leg in this figure) indicates capsular laxity or insufficiency (B). (ER, external rotation.)
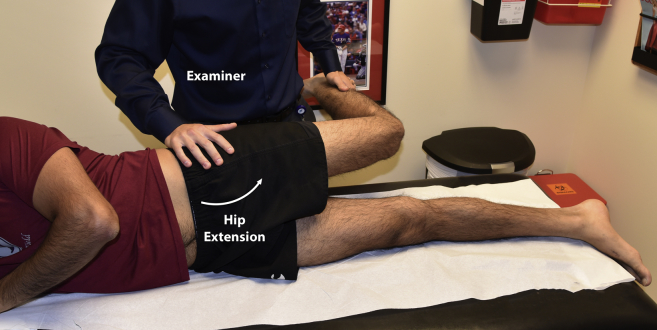
Prone Examination
Palpation of the proximal hamstring tendon and the origin at the ischial tuberosity may reveal tenderness consistent with tendinosis, which is often associated with FAI.17 The sacroiliac joints and lumbar spine should also be palpated to evaluate for tenderness. Internal and external rotation should be measured in a prone position (with the hips extended). Excessive internal rotation can indicate increased femoral anteversion and is associated with snapping psoas and posterior trochanteric impingement.18 Obligatory external rotation or significant limitation with internal rotation can indicate FAI, and increased internal and external rotation can be associated with hip dysplasia.19
Prone examination also allows evaluation of the gluteus maximus muscle firing. Instructing the patient to extend his extremity through the hip should reveal the gluteus maximus contracting before the hamstring musculature. This can be palpated by placing the examiner's small finger on hamstring, both thumbs on the gluteus maximus, and the contralateral small finger at the quadratus lumborum. Latency of gluteus maximus firing is often identified and is thought to contribute to dynamic impingement caused by increased pelvic tilt, as well as hamstring-related symptoms due to overfiring.20
Lateral Examination
The patient should then be assessed in the lateral position, where the iliotibial band, abductors, and greater trochanter can be evaluated. The trochanter and peritrochanteric area should be palpated for trochanteric bursitis and pain around the gluteus medius or minimus, both of which are commonly associated with intra-articular pathology. Modified Ober's maneuvers for passive adduction are used to evaluate tensor fascia lata, gluteus medius, and gluteus maximus contractures.21 The tensor fascia lata is assessed by passive adduction from an abducted position and with the hip and knee in full extension. The gluteus medius is then evaluated by taking tension off the tensor by flexing the knee 90° and repeating this maneuver (Fig 3). The gluteus maximus is then evaluated by squaring the shoulders to the examination table and flexing the hip while maintaining knee extension and repeating the passive adduction maneuver.14 External snapping, caused by the iliotibial band and associated bursitis, is usually reproduced on demand by patients but can also be elicited with the patient in the lateral position with the painful hip brought from hip extension to flexion with slight abduction (Fig 3).22
Fig 3.
Lateral position evaluation showing the modified Ober test for ITB or gluteus medius tightness on a left lower limb. If the examiner releases the leg with his left hand and the patient is unable to passively adduct the right lower extremity, the test is considered positive. (ITB, iliotibial band.)
Impingement-Specific Testing
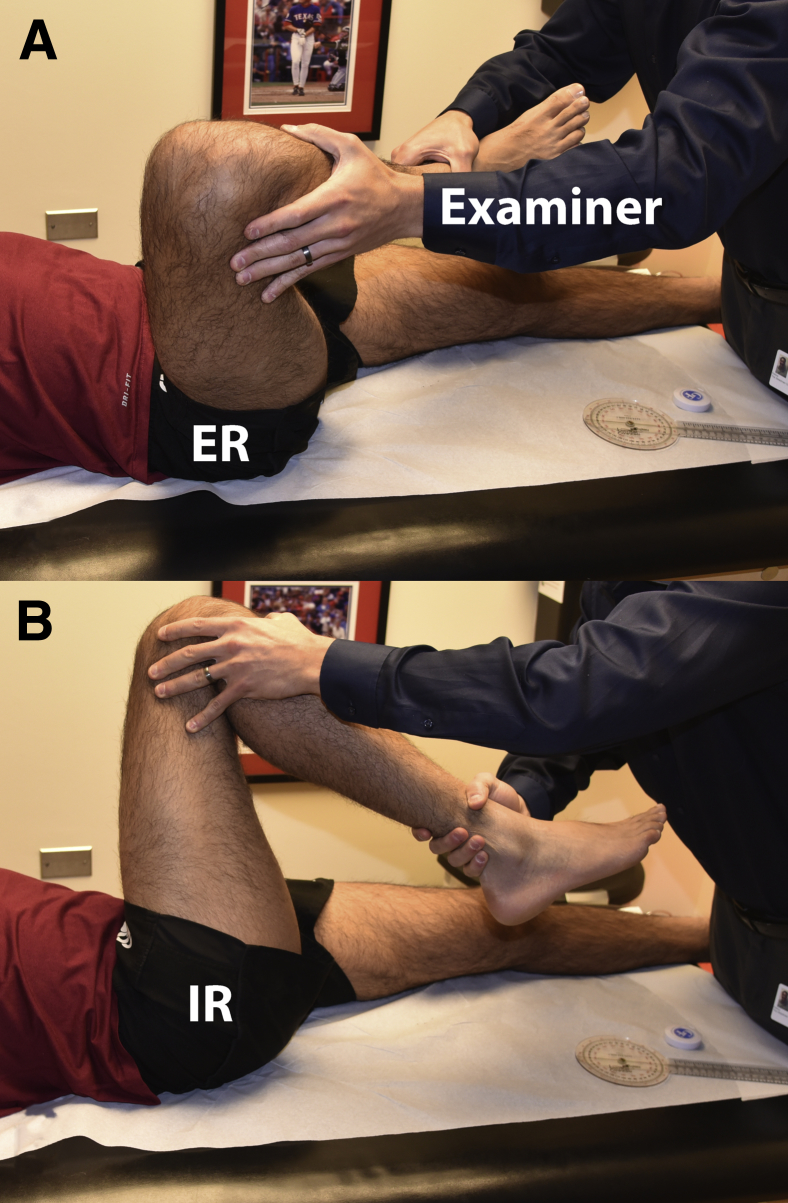
The flexion, internal rotation, and adduction (FADIR) test evaluates anterior rim FAI by passively flexing the hip to 90°, with adduction and internal rotation (Fig 4). A study by Wyss et al.23 showed an inverse relationship between the amount of passive hip internal rotation at 90° of flexion and the severity of a cam lesion. Posterior rim impingement is evaluated by extending the hip in an abducted and externally rotated position (hanging the affected leg off the edge of the examination table). The hip is then brought through a progression of passive flexion to extension while maintaining hip abduction with pain or resistance indicating a positive test (Fig 4).24
Fig 4.
Testing for anterior impingement (FADIR) on a right hip on a patient in the supine position. The examiner takes the relaxed extremity into a flexed slight abducted position (A) into a flexed, adducted, and internally rotated position (B). Pain or clicking indicates a positive test for anterior impingement. (ER, external rotation; FADIR, flexion, internal rotation, and adduction; IR, internal rotation.)
Placing the hip in a flexed abducted and externally rotated position (FABER) is traditionally used to elicit sacroiliac joint pain, but can also reveal a “captured hip” due to FAI or psoas irritation. One must assess pain provocation, location of pain, and range of motion during this examination. Posterior hip pain may be indicative sacroiliac joint involvement, whereas anterior hip or groin pain may indicate intra-articular hip pathology. The final component of the FABER test is the assessment of side-to-side difference external rotation by measuring the distance from the lateral epicondyle of the knee to the table with the use of a ruler (Fig 5). It is important to ensure that the pelvis does not rotate during these measurements to avoid overestimation of the values of external rotation. An increased FABER distance on the involved side indicates capsular tightness and irritation or psoas irritation, and is indicative of intra-articular disease.21 The logroll test is evaluated in the supine position with the hip and knee fully extended. Distally hold the extremity with one hand above and below the knee joint and externally rotate the leg to evaluate external rotation. A lack of resistance to external rotation, or greater external rotation compared with the contralateral side, can indicate a stretched or incompetent iliofemoral ligament.25 The extent of motion in all cases is determined by a firm endpoint or pain with resistance (Fig 5).
Fig 5.
Faber testing on a right hip on a patient in the supine position. With the pelvis in neutral rotation, the hip is flexed, abducted, and externally rotated, with the foot resting proximal to the contralateral knee. Measurements are taken from the inferior aspect of the knee to the examination table and compared with the contralateral side.
Dynamic internal and external rotary impingement testing evaluates the impingement arc of internal and external rotation with the hip flexed and abducted past 90° while eliminating lumbar lordosis by holding the contralateral hip in flexion beyond 90°. These maneuvers are positive when pain is elicited or an audible pop is induced. After range of motion testing, strength of the hip musculature should be assessed in the supine and prone position for pain or weakness. The hamstrings and quadriceps muscle strength are tested in the prone position, with the pelvis in a stable neutral position. The gluteus medius and minimus are tested in the lateral position with active abduction of the upper leg against resistance with pressure placed proximal to the fully extended knee. Resisted straight leg raise (RSLR) should be performed with the patient in a supine position, knee in an extended position, with active hip flexion to 45° against resisted pressure placed above the knee. Weakness or pain elicited with this maneuver indicates hip flexor/psoas inhibition due to tendinosis or capsule irritation, as the psoas presses against the capsule during active resistance.
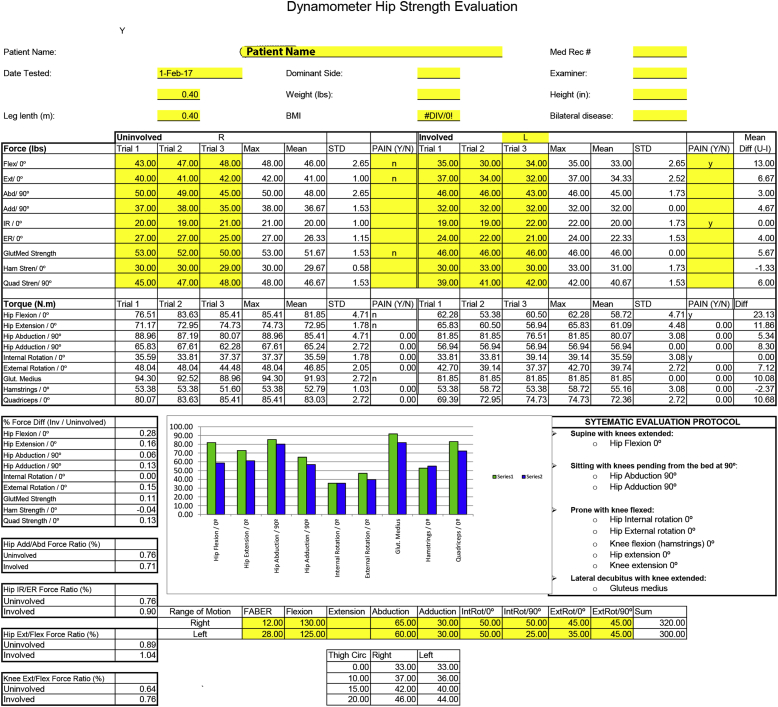
At our institution we objectively quantify strength preoperatively to assess progression postoperatively (Fig 6). This also provides the patient the opportunity to visualize the weaknesses present and allows the patient and therapist to target deficiencies during rehabilitation, and monitor improvement.
Fig 6.
Example of a dynamometer testing evaluation, which is performed during preoperative evaluation. Detailed strength testing provides valuable information for operative planning and more importantly, preoperative and postoperative rehabilitation.
Extra-articular-Specific Testing
Extra-articular conditions share similar clinical features as the intra-articular pathologies but also contain some unique characteristics. Clinicians must have a working knowledge of the clinical presentation of these conditions to enhance accuracy during the examination and differential diagnosis process.
Iliopsoas impingement is often associated with anterior labral tears caused by capsular scarring combined with iliopsoas tendon inflammation that causes impingement during hip extension.5 Positive examination findings include positive FADIR and RSLR testing and can be further confirmed with diagnostic injection into the tendon under ultrasound guidance resulting in relief of pain symptomatology.25 Internal snapping hip may be elicited on provocative testing with active abduction and flexion followed by adduction and hip extension.
Subspine impingement is caused by anterior inferior iliac spine bony protrusion, either congenital or a result of traumatic malunion that abnormally abuts the femoral neck.26 Although no studies have validated the efficacy of specific tests, Poultsides et al.2 described a subspine impingement test that includes passive maximal hip flexion in neutral rotation and adduction, with reproduction of anterior hip or groin pain considered positive.
Ischiofemoral impingement has been described as bony contact between the ischial tuberosity and the lesser trochanter resulting in repetitive impingement of the quadratus femoris, often seen on magnetic resonance imaging as increased signal in the muscle belly correlating with pain during provocative maneuvers. Patients typically report nonspecific pain in the hip, groin, and buttocks with adduction and external rotation. There are no specific physical examination tests for this condition; however, pain can sometimes be provoked during prone testing with the hip in extension during external rotation and adduction, which extenuates the bony contact during rotation. Alternatively, a diagnostic injection can be used to both confirm and treat ischiofemoral impingement.4
The greater trochanter can impinge on the ilium when the hip moves into abduction and extension. Cases are usually a result of a congenital deformity or insult to the physis of the greater trochanter.5 Patients' complaints often stem from abductor weakness. Examination will reveal limited or painful hip abduction and extension, and an abductor-deficient gait pattern. The “gear-stick” sign was developed to help differentiate trochanteric impingement from other sources of hip pain.27 With the patient in a lateral position, the symptomatic hip is passively abducted in extension with reproduction of the patient's symptoms representing a positive sign (Fig 7).27 Pearls and pitfalls for a comprehensive physical examination of the painful hip are detailed in Table 2.
Fig 7.
“The gear-stick” sign. The affected hip (left) is fully extended and adducted and passively ranged from a slightly abducted position (A) to a hyperabducted position (B). Reproduction of the patient's painful symptoms equals a positive test for greater trochanteric impingement.
Table 2.
Pearls and Pitfalls of Physical Examination of the Hip
| Pearls | Pitfalls |
|---|---|
| • Slight abduction while internally rotating during anterior impingement testing in the supine position will fully engage the cam component of FAI on the anterior labrum | • Focusing on intra-articular causes of hip pain can often mask extra-articular conditions |
| • The dial test is a crucial component of the examination to identify capsular laxity and microinstability | • Pain with palpation over the greater trochanter is not always bursitis, and can be a result of intra-articular pathology or a gluteus medius tear |
| • The FABER distance should be measured with slight pressure placed on the inner thigh to distinguish guarding from true hip capture | • Do not assume that radiating pain is radicular. Flexor irritation and intra-articular pathology can result in radiating pain that can extend distally |
| • In a patient with previous repair and suspected re-tear on MRI, in-line traction on the effected leg with the pelvis stabilized can reveal an audible click and confirm reinjury | |
| • Quantitative strength assessment is an objective measure that can help document progress before and after surgery | |
| • Functional testing may be performed with the Hip Sport Test. This is a timed test performed at our institution to assess the patients’ ability to perform repetitive single knee bends and forward box lunges, as well as both lateral and diagonal agility drills. |
FABER, flexed abducted and externally rotated position; FAI, femoroacetabular impingement; MRI, magnetic resonance imaging.
Discussion
Enabled by advancements in diagnostic techniques and improved understanding of hip pathomechanics, groin pain can now be better treated with fewer complications and a faster rehabilitation rate in the athletic population. Recent studies have shown that surgical treatment of FAI and related conditions with hip arthroscopy is effective and can lead to symptomatic relief and return to sport. In a meta-analysis of groin pain requiring surgery, there was a distribution of both intra-articular and extra-articular causes, and the top 5 associated diagnoses were FAI (32%), athletic pubalgia (24%), adductor-related pathology (12%), inguinal-related pathology (10%), and labral pathology (5%).5
Specifically evaluating FAI, Mosler et al.28 reviewed examination findings that were positive in those with hip or groin pain versus those who do not experience pain and found that those patients with pain have lower strength on the adductor squeeze test and reduced range of motion in hip internal rotation; hip external rotation range of motion was equivalent to controls. Tijssen et al.29 evaluated 14 studies that assessed accuracy of physical examination in diagnosing intra-articular hip pathology and reported the highest sensitivity (>90%) with the anterior impingement test, FADIR, and FABER testing. The anterior impingement test, FABER, and RSLR tests were found to be >90% specific for intra-articular hip pathology among the studies analyzed. Because of heterogenous data, the study concluded that not enough uniform literature exists to reliably diagnose FAI and/or labral pathology with the physical examination alone. However, with modern imaging, the physical examination can be used preoperatively in conjunction with advanced radiographic imaging to better elucidate the cause of hip pain in the athletic population.
A recent meta-analysis by Reiman et al.30 concluded that FADIR (94% to 97% sensitive) and flexion-internal rotation (96% sensitive) were the only examination tests that were investigated in enough studies of substantial quality to direct clinical decision making. A systematic review by Pacheco-Carrillo and Medina-Porquere14 in 2016 specifically examined the diagnostic accuracy of testing in FAI and found dynamic internal rotation testing and FABER testing to be the most sensitive for diagnosis. Our group evaluated 300 patients who underwent arthroscopic surgery for FAI, and found groin pain (81%) to be the most common complaint, and the anterior impingement test and FABER test were positive 99% and 97% of the time, respectively.21
Extra-articular hip impingement is caused by abnormal contact between the extra-articular regions of the proximal femur and pelvis and may coexist with intra-articular FAI. A study by Larson et al.31 reported that patients with athletic pubalgia and concomitant intra-articular pathology and solely managed for either intra- or extra-articular pathology did worse than those who were managed for both. A systematic review by de Sa et al.5 isolating extra-articular causes of hip pain concluded that little evidence exists supporting the surgical interventions for these conditions and that further research is necessary. The lack of evidence leaves a gap in our understanding of the pathophysiology of these extra-articular hip pain conditions and how they relate to intra-articular pathology; however, recognition is important and contributes to the spectrum of pathology that can be assessed with a thorough physical examination.
A comprehensive physical examination is an essential component of the evaluation of the athlete with hip pain and several examination maneuvers have been described with excellent sensitivity. When the physical examination is paired with a thorough assessment of clinical medical history and an imaging evaluation (radiographs and magnetic resonance imaging), an accurate diagnosis and successful treatment regimen can be devised.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.M. receives American Board of Medical Specialties (ABMS)-American Board of Orthopaedic Surgeons (ABOS) Visiting Scholars Grant; he was also awarded with US Patent 08926626. M.J.P. receives support from ISHA, Smith & Nephew, MIS, MJP Innovations, LLC, Ossur, Siemens, Vail Valley Medical Center, Arthrosurface, DonJoy, Slack, Elsevier, and Linvatec.
Supplementary Data
Video showing that after a complete history, all patients presenting with hip pain should undergo a comprehensive physical examination of the lumbar spine and bilateral lower extremities. Although the specific order in which the examination steps are performed can vary based on the patient's chief complaint and the preferences of the clinician, a stepwise approach to the examination of both hips, including gait, inspection, palpation, range of motion, sensation, strength, and stability, as well as provocative tests, must be performed for each patient. Typically evaluation of the asymptomatic hip is performed first to obtain a baseline for the “normal” findings of any given patient. In addition, the joints proximal to (lumbosacral spine, sacroiliac joint) and distal to the (knee) hip should be examined in an effort to eliminate extra-articular sources of referred hip pain. All patients shoulder undergo a complete neurovascular examination of the bilateral lower extremities, including strength, sensation, and perfusion. Several aspects of the examination are performed with the patient in the standing position, whereas others are performed in the supine, prone, and lateral position as outlined in the video.
References
- 1.Clohisy J.C., St John L.C., Schutz A.L. Surgical treatment of femoroacetabular impingement: A systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poultsides L.A., Bedi A., Kelly B.T. An algorithmic approach to mechanical hip pain. HSS J. 2012;8:213–224. doi: 10.1007/s11420-012-9304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reiman M.P., Mather R.C., Hash T.W., Cook C.E. Examination of acetabular labral tear: A continued diagnostic challenge. Br J Sports Med. 2014;48:311–319. doi: 10.1136/bjsports-2012-091994. [DOI] [PubMed] [Google Scholar]
- 4.Agten C.A., Sutter R., Buck F.M., Pfirrmann C.W. Hip imaging in athletes: Sports imaging series. Radiology. 2016;280:351–369. doi: 10.1148/radiol.2016151348. [DOI] [PubMed] [Google Scholar]
- 5.de Sa D., Holmich P., Phillips M. Athletic groin pain: A systematic review of surgical diagnoses, investigations and treatment. Br J Sports Med. 2016;50:1181–1186. doi: 10.1136/bjsports-2015-095137. [DOI] [PubMed] [Google Scholar]
- 6.Nepple J.J., Prather H., Trousdale R.T. Clinical diagnosis of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(suppl 1):S16–S19. doi: 10.5435/JAAOS-21-07-S16. [DOI] [PubMed] [Google Scholar]
- 7.Lesher J.M., Dreyfuss P., Hager N., Kaplan M., Furman M. Hip joint pain referral patterns: A descriptive study. Pain Med. 2008;9:22–25. doi: 10.1111/j.1526-4637.2006.00153.x. [DOI] [PubMed] [Google Scholar]
- 8.Brown M.D., Gomez-Marin O., Brookfield K.F., Li P.S. Differential diagnosis of hip disease versus spine disease. Clin Orthop Relat Res. 2004:280–284. doi: 10.1097/00003086-200402000-00044. [DOI] [PubMed] [Google Scholar]
- 9.Jacobson J.A., Bedi A., Sekiya J.K., Blankenbaker D.G. Evaluation of the painful athletic hip: Imaging options and imaging-guided injections. Am J Roentgenol. 2012;199:516–524. doi: 10.2214/AJR.12.8992. [DOI] [PubMed] [Google Scholar]
- 10.Khan W., Khan M., Alradwan H., Williams R., Simunovic N., Ayeni O.R. Utility of intra-articular hip injections for femoroacetabular impingement: A systematic review. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115601030. 2325967115601030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Livingston L.A., Stevenson J.M., Olney S.J. Stairclimbing kinematics on stairs of differing dimensions. Arch Phys Med Rehabil. 1991;72:398–402. [PubMed] [Google Scholar]
- 12.Beighton P., Solomon L., Soskolne C.L. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin H.D., Kelly B.T., Leunig M. The pattern and technique in the clinical evaluation of the adult hip: The common physical examination tests of hip specialists. Arthroscopy. 2010;26:161–172. doi: 10.1016/j.arthro.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Pacheco-Carrillo A., Medina-Porqueres I. Physical examination tests for the diagnosis of femoroacetabular impingement. A systematic review. Phys Ther Sport. 2016;21:87–93. doi: 10.1016/j.ptsp.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 15.Troum O.M., Crues J.V. The young adult with hip pain: Diagnosis and medical treatment, circa 2004. Clin Orthop Relat Res. 2004:9–17. doi: 10.1097/00003086-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Philippon M.J., Patterson D.C., Briggs K.K. Hip arthroscopy and femoroacetabular impingement in the pediatric patient. J Pediatr Orthop. 2013;33(suppl 1):S126–S130. doi: 10.1097/BPO.0b013e318274f834. [DOI] [PubMed] [Google Scholar]
- 17.Hammoud S., Bedi A., Voos J.E., Mauro C.S., Kelly B.T. The recognition and evaluation of patterns of compensatory injury in patients with mechanical hip pain. Sports Health. 2014;6:108–118. doi: 10.1177/1941738114522201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nepple J.J., Smith M.V. Biomechanics of the hip capsule and capsule management strategies in hip arthroscopy. Sports Med Arthrosc. 2015;23:164–168. doi: 10.1097/JSA.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 19.Ranawat A.S., Schulz B., Baumbach S.F., Meftah M., Ganz R., Leunig M. Radiographic predictors of hip pain in femoroacetabular impingement. HSS J. 2011;7:115–119. doi: 10.1007/s11420-010-9192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross J.R., Nepple J.J., Philippon M.J., Kelly B.T., Larson C.M., Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med. 2014;42:2402–2409. doi: 10.1177/0363546514541229. [DOI] [PubMed] [Google Scholar]
- 21.Philippon M.J., Maxwell R.B., Johnston T.L., Schenker M., Briggs K.K. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 22.Yoon J.Y., Kwak H.S., Yoon K.S., Chang J.S., Yoon P.W. Arthroscopic treatment for external snapping hip. Hip Pelvis. 2014;26:173–177. doi: 10.5371/hp.2014.26.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wyss T.F., Clark J.M., Weishaupt D., Nötzli H.P. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. doi: 10.1097/BLO.0b013e3180399430. [DOI] [PubMed] [Google Scholar]
- 24.Berkes M.B., Cross M.B., Shindle M.K., Bedi A., Kelly B.T. Traumatic posterior hip instability and femoroacetabular impingement in athletes. Am J Orthop (Belle Mead NJ) 2012;41:166–171. [PubMed] [Google Scholar]
- 25.Domb B.G., Brooks A.G., Byrd J.W. Clinical examination of the hip joint in athletes. J Sport Rehabil. 2009;18:3–23. doi: 10.1123/jsr.18.1.3. [DOI] [PubMed] [Google Scholar]
- 26.Hetsroni I., Larson C.M., Dela Torre K., Zbeda R.M., Magennis E., Kelly B.T. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: A series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644–1653. doi: 10.1016/j.arthro.2012.05.882. [DOI] [PubMed] [Google Scholar]
- 27.Macnicol M.F., Makris D. Distal transfer of the greater trochanter. J Bone Joint Surg Br. 1991;73:838–841. doi: 10.1302/0301-620X.73B5.1894678. [DOI] [PubMed] [Google Scholar]
- 28.Mosler A.B., Agricola R., Weir A., Hölmich P., Crossley K.M. Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. Br J Sports Med. 2015;49:810. doi: 10.1136/bjsports-2015-094602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tijssen M., van Cingel R., Willemsen L., de Visser E. Diagnostics of femoroacetabular impingement and labral pathology of the hip: A systematic review of the accuracy and validity of physical tests. Arthroscopy. 2012;28:860–871. doi: 10.1016/j.arthro.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Reiman M.P., Goode A.P., Cook C.E., Hölmich P., Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: A systematic review with meta-analysis. Br J Sports Med. 2015;49:811. doi: 10.1136/bjsports-2014-094302. [DOI] [PubMed] [Google Scholar]
- 31.Larson C.M., Pierce B.R., Giveans M.R. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: A case series. Arthroscopy. 2011;27:768–775. doi: 10.1016/j.arthro.2011.01.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video showing that after a complete history, all patients presenting with hip pain should undergo a comprehensive physical examination of the lumbar spine and bilateral lower extremities. Although the specific order in which the examination steps are performed can vary based on the patient's chief complaint and the preferences of the clinician, a stepwise approach to the examination of both hips, including gait, inspection, palpation, range of motion, sensation, strength, and stability, as well as provocative tests, must be performed for each patient. Typically evaluation of the asymptomatic hip is performed first to obtain a baseline for the “normal” findings of any given patient. In addition, the joints proximal to (lumbosacral spine, sacroiliac joint) and distal to the (knee) hip should be examined in an effort to eliminate extra-articular sources of referred hip pain. All patients shoulder undergo a complete neurovascular examination of the bilateral lower extremities, including strength, sensation, and perfusion. Several aspects of the examination are performed with the patient in the standing position, whereas others are performed in the supine, prone, and lateral position as outlined in the video.