Abstract
Background:
Yoga is considered to be one of the most important, effective, and valuable tools available for man to overcome various physical and psychological problems. Stress contributes significantly to the pathogenesis of periodontal diseases; hence, it becomes important to reduce the level of stress for prevention and management of diseases.
Aims and Objectives:
The present study was aimed: (1) To understand and analyze the possibilities of employing yogic practices in the treatment of periodontal disease along with conventional dental therapy, (2) to understand the effect of stress on periodontal treatment outcome, (3) to evaluate the efficacy of yoga in the management of periodontal disease with reference to stress.
Materials and Methods:
An outpatient department-based parallel group randomized study was performed with standard treatment for periodontal disease yoga therapy as Group II and only standard treatment as Group I. Periodontal health status was recorded using indices of modified plaque index (PI), bleeding on probing (BOP), probing depth, and clinical attachment loss (CAL). The Cohen's perceived stress questionnaire was also used to determine stress severity. The yogic intervention consists of lectures and practical sessions on asanas, pranayama, kriyas, and meditation.
Results:
Repeated measure analysis of variance revealed a significant difference (P < 0.001) in all the outcome variables with respect to time in both groups. It was observed that mean PI score reduced by 1.35 in Group II as compared to 0.54 in Group I, mean probing pocket depth reduced by 1.60 in Group II as compared to only 0.68 in Group I, and mean CAL score reduced by 1.60 in Group II as compared to 0.68 in Group I. Similarly, Cohen's perceived stress scale score also reduced by 18.76 points in Group II as compared to only 2.58 points in Group I, BOP also shows better improvement in Group II with a reduction of 0.68 as compared to reduction of only 0.08 in Group I. The results obtained ascertained the role of yoga in stress reduction in periodontal disease.
Conclusion:
Although yoga does not play a direct role in improving periodontal disease, it accelerates the treatment outcomes by combating the stress which is a major factor affecting the treatment of periodontal disease.
Keywords: Periodontal disease, repeated measure analysis of variance, stress management, yoga
Introduction
Periodontal disease is one of the major dental diseases that affect human populations worldwide at high prevalence rates. The WHO reported that 10%–15% of the world population suffers from severe periodontitis. In India, according to the WHO data, the prevalence of severe periodontitis was in the range of 19%–32%. Significant disparities appear to exist in the level of periodontitis among young, adults, and senior populations in the world.[1] The most prevalent form of periodontal disease is a mild form called gingivitis. Gingivitis affects 75% of adults in the United States and is characterized by inflammation of gums, redness, swelling, and frequent bleeding. More advanced forms of periodontitis are also prevalent, affecting approximately 30% (moderate disease) and 10% (advanced disease) of the adult population in the United States.[2] This process is characterized by destruction of periodontal attachment apparatus, loss of crestal alveolar bone, apical migration of the epithelial attachment, and formation of periodontal pockets.[3] The signs and symptoms of periodontitis include swollen gums, deepening of gingival crevice leading to the formation of periodontal pocket, bleeding on brushing, increased spacing between the teeth, loose teeth, tooth loss, and edentulism.[4]
Stress and periodontal disease
The psychological response of the organism to a perceived challenge or threat is referred to as stress.[5] It is found that individuals with high levels of trait, anxiety appeared to be more prone to periodontal disease.[6] The function of the stress response is to prepare the organism to meet the challenge or threat appropriately and is therefore homeostatic. Stress becomes dangerous for the organism only when it is sustained or when one or more aspects of the neuroendocrine response act on an organ system which, for some reason, is already predisposed to pathology. The immune system is bidirectionally linked to the psyche, the nervous system, and the endocrine system, and the brain areas involved in the classical stress response regulate the immune response to bacterial and other antigenic challenges.[7,8] Psychological stress has been suggested as a disruptive factor in the homeostasis of oral bacteria and the host's immune system. We may expect different outcome of periodontal disease depending on the interplay of virulent bacteria, host inflammatory responses, stress experiences of the individual (trait characteristics), and stress characteristics of his/her current situation (state characteristics).[9]
Psychosocial stress can affect the periodontal tissues directly through biological mechanism and indirectly through the changes in lifestyle such as ignoring oral hygiene measures, smoking more heavily, and consuming more fat and sugar in diet. Hence, there are two proposed mechanistic links: One biological and the other behavioral.[10] In general, depressed patients pay less attention to the oral hygiene practices and also to keep them motivated is difficult as they are found to be ignorant. According to Azmi et al., more depressed a patient was, the more pain they had postperiodontal surgery, the stronger the pain medication they used, and the more delayed their wound healing was after surgery.[11]
Yoga and stress
Yoga is considered to be one of the most important, effective, and valuable tools available for man to overcome various physical and psychological problems. According to Kuvalayananda and Vinekar (1968), yoga includes cultivation of correct attitudes and reconditioning of the neuromuscular systems. Yoga helps the whole body to enable it to withstand greater stress and strain. Yoga aims at integrated and harmonious development of all the potentialities of man. Anxiety and stress are the major problems of the modern world, particularly of the youth and college going students who are losing their health and well-being. Good health is one of the greatest resources for vitality, creativity, and wealth, in contrast to poor health and negative feelings, which lead to various physical and psychological problems.[12] The psychological factors, including anxiety, contribute significantly not only to the pathogenesis of medical illness but also affect their course and may be a target for effective intervention. Hence, it becomes important to reduce the level of anxiety as a part of prevention and management of diseases. Among the various approaches to reduce the level of anxiety, yoga is one that combines the physical elements of a healthy lifestyle with prescriptions for abiding mental peace. Further, the growth of psychoneuroimmunology has strengthened the scientific foundations of mind-body medicine.[13] Yoga is believed to have beneficial effects on cognition, attenuation of emotional intensity, and stress reduction.[14] Studies in the past by several researchers have shown a direct impact of yoga on stress reduction. Furthermore, the role of stress has been established to effect the inflammatory destruction which is the basis of periodontal disease progression. However, in some studies, the retrograde effect of stress (i.e., reduction in stress) has been studied to positively affect the treatment outcomes and reduced severity of the disease. Hence, a study is needed to establish the direct effect of the factors reducing stress, i.e., yoga on the treatment outcome of the periodontal disease process, so that the factors reducing the stress can be used as an adjunct with the standard periodontal therapy for better treatment outcome.
Yoga is an ancient Indian practice being used for maintaining good health and to prevent the occurrence of many diseases. Till date, no study has been done to study the effects of yoga in dental care. Therefore, this study was conducted.
Materials and Methods
Aims and objectives
The present study was taken up to further validate the impact of yoga in stress management and on the treatment outcome of periodontal diseases. The objectives of the present study were (1) to understand and analyze the possibilities of employing yogic practices in the treatment of periodontal disease along with conventional dental therapy, (2) to understand the effect of stress on periodontal treatment outcome, and (3) to evaluate the efficacy of yoga in management of periodontal disease with reference to stress. The patients suffering from periodontitis were screened for recruitment in the study. After initial screening of the patients from outpatient department, only those who were in the age group of 15–45 years, were suffering from periodontal disease, were having more than 15 teeth, and were found fit and were willing to do yoga sessions daily were recruited in the study. The patients who were suffering from other oral diseases also were excluded from the study. Similarly, mentally ill patients, patients with a history of systemic illness, pregnant and lactating females, patients taking tobacco in any form, and patients who have undergone oral prophylaxis during the past 6 months were also excluded from the study. Mentally ill patients and patients with any systematic illness were diagnosed only on the basis of patient's history taken at the time of recruitment. Patients were asked about the history of previous and present illness at the time of recruitment and patients on medication for depression, diabetes, hypertension, cardiac problems were excluded.
Sample size and randomization
A total of eighty patients were recruited in the study and were randomized (40 in each group) by a computer-generated random numbers in two groups. Sample size calculations were based on expected change in Probing pocket depth (PPD) in both groups with 95% confidence interval and 80% power including a dropout rate of 20%. Expected change in PPD and standard deviation used for sample size calculation were based on the reference from the previous study published in 2008 in Brazilian Dental Journal.[15]
Outcome measures
Periodontal health status was recorded using indices of modified plaque index (PI), bleeding on probing (BOP), probing depth (PPD), and clinical attachment loss (CAL). They were assessed at 6 sites per tooth (mesiobuccal, buccal, distobuccal, mesiolingual, lingual, and distolingual) of all erupted teeth using a manual periodontal probe (William's periodontal probe). Mouth mirror, William's periodontal probe (API), and illuminated light source are used for the examination. The Cohen's perceived stress questionnaire was also used to determine stress severity and was correlated with periodontal status.
Plaque index (0–3)
The measurement of the state of oral hygiene by Silness and Loe PI is based on recording both soft debris and mineralized deposits on the teeth. Each of the 4 surfaces of the teeth (buccal, lingual, mesial and distal) is given a score from 0-3. The scores from the 4 areas of the tooth are added and divided by 4 to give the PI for the tooth. The index for the patient is obtained by summing the indices for all six teeth and dividing by number of teeth present.[16] The index ranges from 0 to 3.
Probing pocket depth (mm)
The measurement of probing pocket depths (PPD) is a clinical diagnostic test to assess the coronoapical extension or the depths of the periodontal pocket, respectively. In this test, periodontal probe is inserted into the periodontal pocket with defined force (0.2-0.3N) in an apical direction parallel to the tooth axis between gingiva and tooth surface until probing pressure and tissue resistance are in balance. The probing pocket depth is read out in relation to the gingival margin using the markings of the periodontal probe.[17]
Clinical attachment loss (mm)
CAL is defined as the distance between the cementoenamel junction (CEJ) and the base of the probable pocket because the apical termination of the junctional epithelium is normally located at the CEJ, there should be no CAL when the periodontal tissues are healthy, and there is no history of periodontitis. When the gingival margin is located coronal to the CEJ, CAL is measured by subtracting the distance of the free gingival margin (FGM) to CEJ from the PD. Thus, CAL = PD - (FGM - CEJ). When there is a gingival recession, CAL is calculated by adding the PD and the amount of recession (CAL = PD + gingival recession). PD and CAL are measured to the nearest millimeter using William's periodontal probe (API).[17] PD and CAL were measured twice and the average of the pair of measurements has been used for analysis.
Bleeding on probing (0 or 1)
BOP is an important indicator of gingival inflammation within the periodontal pocket. It occurs because of micro ulcerations in the junctional epithelium.[17] BOP is influenced by repeated probe insertions in the short time as well as by the use of excessive force (>25N).
The Cohen's perceived stress scale
Cohen's perceived stress scale (CPSS) was used to determine stress severity. Each item in this scale has been rated on a 5-point scale ranging from never (0) to almost always (4). Positively worded items are reverse scored, and the ratings are summed, with higher scores indicating more perceived stress. PSS-10 scores are obtained by reversing the scores on the four positive items – e.g.: 0=4, 1=3, 2=2 etc and then summing across all 10 items. Items 4, 5, 7 & 8 are positively stated items.[18,19]
Yoga intervention
Patients assigned to the yoga group were trained in a comprehensive yogic intervention [Table 1]. The yogic intervention mainly included yoga practices and related components such as stress management program for about 1 week. Following 1 week of training, the same schedule was advised to practice daily 1 h for 6 days a week for 3 months. The program consists of lectures and practical sessions on asanas (physical postures), pranayama (breathing techniques), kriyas (cleansing techniques), meditation, and shavasana (relaxation techniques). The lectures were on yoga, its place in daily life, its application to stress management, fundamentals of nutrition, and health education relevant to their illness. Each participant was also given at least one session of individualized counseling. The protocol of the course is given in Table 1, and the set of yoga practices included in the course is shown in Table 2.
Table 1.
Protocol of the yogic intervention
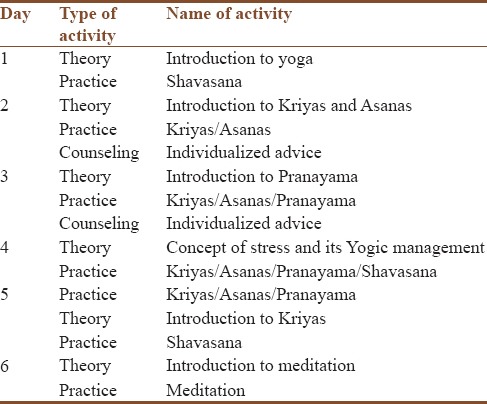
Table 2.
List of yogic practices
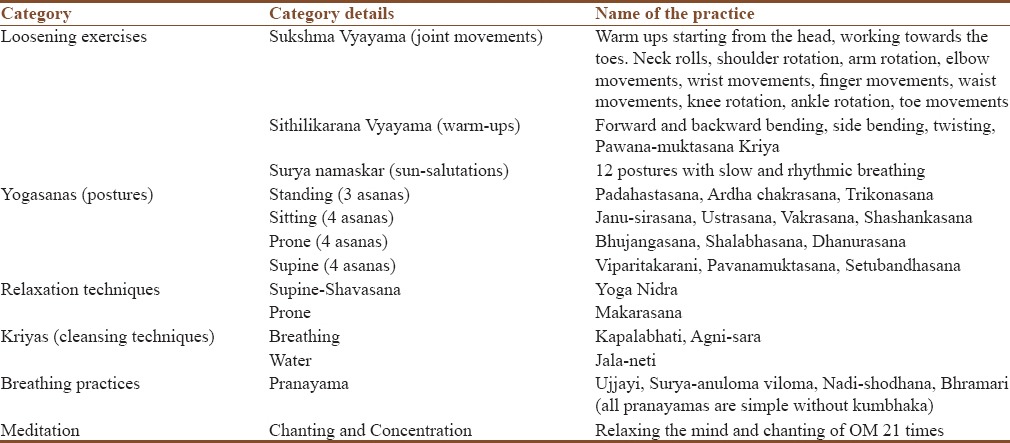
The physical practices consist of preliminary breathing exercises and loosening exercises, followed by asanas under four categories (standing, sitting, prone, and supine), pranayama techniques, kriyas, and meditation. Participants were instructed to follow a specific breathing pattern during each asana and asked to hold each pose in the final position for up to 30 s without holding their breath. Each posture was followed by an appropriate relaxation posture for a short period. All the patients from yoga group were encouraged to follow a standard sequence of practices to maintain homogeneity with similar benefits.
Results
A total of eighty patients were recruited in the study and were randomized in the ratio of 1:1 in both groups [Figure 1]. The patients were assessed at baseline, i.e., on the day of enrollment and thereafter, at an interval of 30 days for 90 days. The brief demographic history of the patient and the data related to the oral hygiene practiced by them were recorded on enrolment day. The baseline characteristics of the patients in both groups were compared which does not show any significant difference. Kolmogorov–Smirnov test was used to check the normality of the data before applying parametric tests. Tables 3 and 4 show the baseline characteristics of the patients in both groups. It was observed that the majority of the patients in both groups were from lower and upper lower income group as assessed by Kuppuswamy socioeconomic scale. The past studies have also shown a significant correlation in the socioeconomic status of the patients and the presence of periodontal disease. The baseline data recorded during this study further validate the same. There was no significant difference in the various methods of oral hygiene practiced by the patients in both groups [Table 3]. In both groups, most of the patients used to clean their teeth once in a day with tooth brush and paste. Majority of them does not used mouth wash and additional methods of plaque control when assessed at baseline [Table 4].
Figure 1.
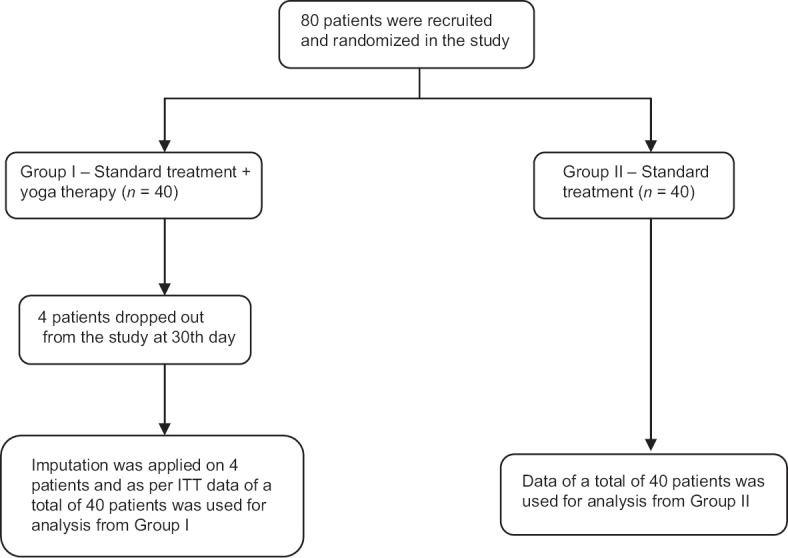
Outflow of the patients in the study
Table 3.
Baseline characteristics of the patients
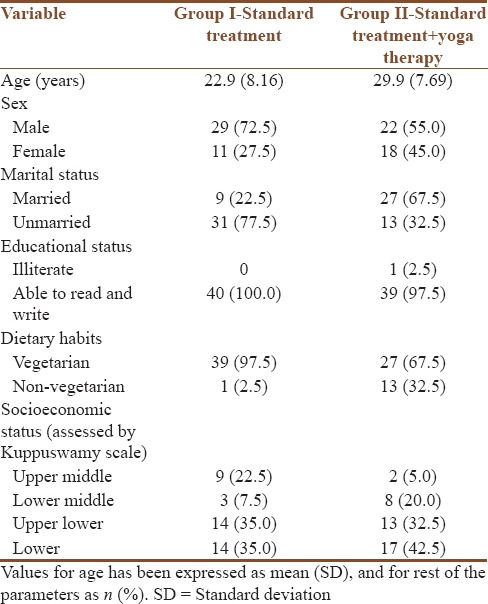
Table 4.
Comparison of oral hygiene practiced by the patients at baseline
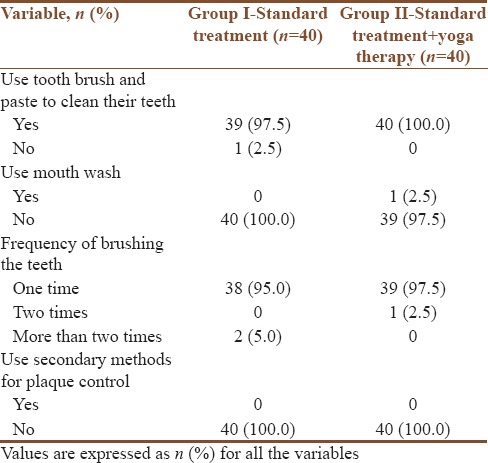
Repeated measure analysis of variance was used to assess the within-group difference in the outcome variables, namely, PI score (PIS), probing pocket depth, CAL, and CPSS. GLM analysis shows that there was a significant difference (P < 0.001) in all the outcome variables with respect to time in both groups. Between-group analysis was done using independent sample t-test on the change in outcome variables, namely, PIS, BOP, Pocket probing depth (PPD), CAL, and CPSS, which revealed a significant difference (P < 0.001) between two groups for all the variables. It is further evident from Table 5 that change in scores evaluated before and after treatment for PIS, BOP, PPD, CAL, and CPSS was better in Group II (standard treatment + yoga therapy) as compared to Group I (standard treatment).
Table 5.
Comparison of outcome variables at the end of the study
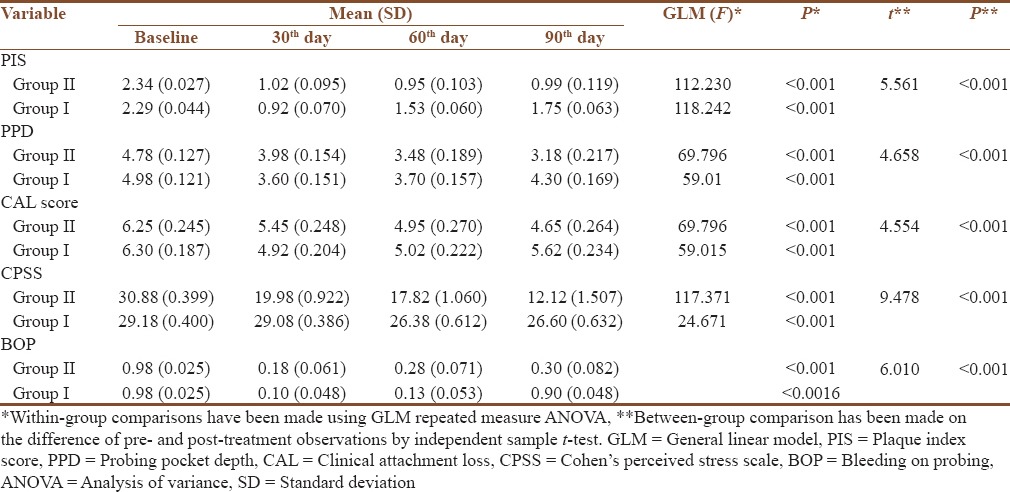
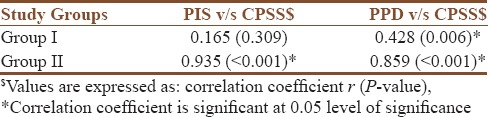
The correlation coefficient was computed between PIS and CPSS score and between pocket probing depth (PPD) and stress scale score to further evaluate the relationship between stress and periodontal disease. Table 6 shows the values of correlation coefficient and their corresponding P values for both groups. It was evident from Table 6 that there is a positive correlation between stress and periodontal disease. It was noticed that the PIS and pocket probing depth in the patients reduce with the reduction in stress scale scores. The values of Correlation coefficient in Group I between PIS and CPSS (r = 0.165, P = 0.309), and between PPD and CPSS (r = 0.428, P = 0.006) validates the fact that PIS and PPD in the patients has reduced with the reduction in CPSS scores. The fact was further validated in Group II also where the values of correlation coefficient between PIS and CPSS was (r = 0.935, P <= 0.001), and between PPD and CPSS was (r = 0.859, P = 0.001).
Table 6.
Correlation between PIS v/s CPSS and between PPD v/s CPSS
Discussion
The present study was to done to bridge the gap between the treatments of periodontal diseases including the yogic intervention. Researchers in the past have studied that the stress reduction can be done by practicing yoga, and the dentists have concluded earlier that after smoking, stress is the major factor affecting the periodontal condition. After assessing and statistically evaluating the results of the present study, it was concluded that yoga helps in overcoming inflammation and pain, which has also been one of the reasons that positive results have been seen in Group II (standard treatment + yoga therapy). Physical activity is an important factor in overcoming inflammation. People who are physically active have lesser inflammatory markers as compared to people with a sedentary lifestyle. Regular physical activity is associated with lower levels of interleukin-6 (IL-6) and other pro-inflammatory cytokines. Exercises boost production and release of IL-6 from muscles which, in turn, can reduce inflammation.[20] It was evident from the study results that PIS, BOP, CAL, pocket probing depth all these outcome variables have shown a significant improvement in Group II (standard treatment + yoga therapy) in comparison to Group I (standard treatment). Correlation coefficient computed between stress and PPD and between stress and PIS has also ascertained a positive relationship between stress and periodontal disease which, in turn, can be one of the reasons that better results have been achieved in Group II where the patients have practiced yoga along with standard treatment. However, several studies have been done in the past establishing the fact that yoga helps in combating stress, there is a need for long-term studies with greater number of patients to further validate the effect of yoga in the management of periodontal disease.
Conclusion
Though there were allusions to yoga in Vedic period and the knowledge was shared and transferred based on the personal experience, yet the science of yoga had yet to be systemized and formulated. The present study was done to observe the effect of yoga on periodontal health through stress reduction. Researchers who have studied the effect of yoga on the general health and coping behaviors in the past have observed that stress reduction can be done by yoga practice and researchers in the field of dentistry have observed and stated in the past that the stress is one of the most common risk factor (after smoking) affecting periodontal condition. The fact has been further validated by the outcome of this study as well. However, other factors affecting periodontal health should be taken care of in future studies to understand role of yoga in oral health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jacob S. Global prevalence of periodontitis, a literature review. IAJD. 2012;3:26–30. [Google Scholar]
- 2.Kim J, Amar S. Periodontal disease and systemic conditions: A bidirectional relationship. Odontology. 2006;94:10–21. doi: 10.1007/s10266-006-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Assuma R, Oates T, Cochran D, Amar S, Graves DT. IL-1 and TNF antagonists inhibit the inflammatory response and bone loss in experimental periodontitis. J Immunol. 1998;160:403–9. [PubMed] [Google Scholar]
- 4.Gurav AN. The association of periodontitis and metabolic syndrome. Dent Res J (Isfahan) 2014;11:1–10. [PMC free article] [PubMed] [Google Scholar]
- 5.Torabi-Gaarden R, Breivik T, Frode Hansen B, Malt UF, Gjermo PE. Negative life events, anxiety, depression and coping ability (stress) as related to chronic periodontitis. Periodontics. 2004;1:35–42. [Google Scholar]
- 6.Vettore MV, Leão AT, Monteiro Da Silva AM, Quintanilha RS, Lamarca GA. The relationship of stress and anxiety with chronic periodontitis. J Clin Periodontol. 2003;30:394–402. doi: 10.1034/j.1600-051x.2003.10271.x. [DOI] [PubMed] [Google Scholar]
- 7.Ader R, Cohen N, Felten D. Psychoneuroimmunology: Interactions between the nervous system and the immune system. Lancet. 1995;345:99–103. doi: 10.1016/s0140-6736(95)90066-7. [DOI] [PubMed] [Google Scholar]
- 8.Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332:1351–62. doi: 10.1056/NEJM199505183322008. [DOI] [PubMed] [Google Scholar]
- 9.Axtelius B, Söderfeldt B, Edwardsson S, Attström R. Therapy-resistant periodontitis (II). Compliance and general and dental health experiences. J Clin Periodontol. 1997;24(9 Pt 1):646–53. doi: 10.1111/j.1600-051x.1997.tb00243.x. [DOI] [PubMed] [Google Scholar]
- 10.Bansal J, Bansal A, Shahi M, Kedige S, Narula R. Periodontal emotional stress syndrome, review of basic concepts, mechanism and management. Open J Med Psychol. 2014;3:250–61. [Google Scholar]
- 11.Azmi SA, Fatima Z, Bey A, Gupta ND, Sharma V. Depression and periodontal diseases. Delhi Psychiatry J. 2014;17:7–10. [Google Scholar]
- 12.Jadhav SG, Havalappanavar NB. Effect of yoga intervention on anxiety and subjective well-being. J Indian Acad Appl Psychol. 2009;35:27–31. [Google Scholar]
- 13.Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle Intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50:41–7. [PubMed] [Google Scholar]
- 14.Rocha KK, Ribeiro AM, Rocha KC, Sousa MB, Albuquerque FS, Ribeiro S, et al. Improvement in physiological and psychological parameters after 6 months of yoga practice. Conscious Cogn. 2012;21:843–50. doi: 10.1016/j.concog.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 15.de Queiroz AC, Taba M, Jr, O’Connell PA, da Nóbrega PB, Costa PP, Kawata VK, et al. Inflammation markers in healthy and periodontitis patients: A preliminary data screening. Braz Dent J. 2008;19:3–8. doi: 10.1590/s0103-64402008000100001. [DOI] [PubMed] [Google Scholar]
- 16.Peter S. Essential of Preventive and Community Dentistry. 1st ed. New Delhi: Arya (Medi) Publishing House; 1999. [Google Scholar]
- 17.New Man MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. 8th ed. Noida: Saunders, Reed Elsevier India Pvt. Ltd; 1996. [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 19.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 20.Kiecolt-Glaser JK, Christian L, Preston H, Houts CR, Malarkey WB, Emery CF, et al. Stress, inflammation, and yoga practice. Psychosom Med. 2010;72:113–21. doi: 10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]


