Abstract
Background:
Breathing exercises have been described to be useful in asthma management by few researchers in the past.
Objective:
To assess the efficacy of breathing exercises (Pranayamas) added to regular optimal medications in asthma patients in improving health impairment using St. George's Respiratory Questionnaire (SGRQ).
Methods:
Sixty stable asthma patients (34 females) receiving optimal treatment at our institute for 3 months or more as per the Global Initiative for Asthma guidelines were included in the study. They performed seven breathing exercises under supervision at yoga center of our institute for 3 months in addition to their regular medications. SGRQ (1 month symptoms version) was used to assess the quality of life before and after breathing exercises intervention for following subsets: Symptom score, activity score, impact score, and total score to assess the efficacy of breathing exercises.
Results:
Of 60 asthma patients, 34 were females and 26 were males, and their mean age was 25.45 ± 5.41 years. Their baseline spirometric values were as follow: Forced expiratory volume in 1 s (FEV1) - 2.492 ± 0.358 L and peak expiratory flow rate (PEFR) - 283.82 ± 51.12 L/min. The SGRQ scores after breathing exercises intervention decreased from 45.98 ± 5.61 to 38.78 ± 4.92 for symptom subset, from 15.45 ± 3.33 to 12.34 ± 2.39 for activity subset, from 17.95 ± 4.22 to 12.12 ± 3.82 for impact subset, and from 25.83 ± 8.31 to 19.20 ± 7.09 for total scores. All these reductions were statistically highly significant (P < 0.001). Decrease in symptoms, activity, and total SGRQ scores each was significantly correlated with FEV1, FEV1/forced vital capacity (FVC) ratio, and PEFR; decrease in impact score was significantly related only with FEV1/FVC ratio.
Conclusions:
Breathing exercises significantly decreased all component scores of SGRQ, signifying a global improvement in health impairment due to asthma; this improvement was in addition to that was achieved with optimal asthma therapy alone.
Keywords: Asthma, breathing exercises, pranayamas, quality of life, St. George's Respiratory Questionnaire
Introduction
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation.[1] Globally, around 300 million people have asthma, with 250,000 annual deaths attributed to the disease, most of which are preventable.[2] According to ISAAC group,[3] asthma, rhinitis, and eczema in children are increasing in Western and developing countries and the prevalence of wheeze varies widely. The high prevalence (>20%) was generally observed in Latin America and English-speaking countries of Australasia, Europe, and North America as well as South Africa. The low prevalence (<5%) was observed in the Indian subcontinent, Asia-Pacific, Eastern Mediterranean, and Northern and Eastern Europe. The gaps between varied prevalence are now closing, due to a rise in prevalence in low- and middle-income countries and plateauing in high-income countries. The rate of asthma increases as communities adopt Western lifestyles and become urbanized. According to the Global Burden of Asthma Report by Global Initiative for Asthma (GINA),[4] with the anticipated increase in the proportion of the world's population, that is, urban, from 45% to 59% in 2025, a marked increase in the number of asthmatics worldwide is projected over the next decades. It is estimated that there may be an additional 100 million persons with asthma by 2025.
Asthma is a chronic health problem that usually encompasses the patient's entire lifetime and may result in physical, emotional, and social limitations for patients. These limitations often impair quality of life. Asthma can affect patients’ quality of life in many different ways.[5,6,7] It has been documented that the quality of life impairment in asthma patients is proportional to the severity of disease.[8] A recent US study found that adolescents with asthma and symptoms reported worse health-related quality of life compared with those with asthma but not reporting symptoms and those without asthma.[9] People with asthma suffer from impaired quality of life compared with people without asthma. Rational asthma management leads to disease control and better quality of life. It is, therefore, considerably important to evaluate the quality of life of the patients in addition to the symptoms in order to fully assess the asthma management.
There have been great efforts to evolve an ideal respiratory questionnaire to assess the health-related quality of life in asthma patients. In recent years, various generic and specific instruments have been developed to estimate the impact that diseases have over the health-related quality of life. The St. George's Respiratory Questionnaire (SGRQ), developed by Jones et al.,[10] is a specific questionnaire for assessing quality of life in patients with chronic respiratory diseases, and is widely used to assess health-related quality of life in asthma patients. In the present study, SGRQ was used to assess the advantage of seven breathing exercises, Pranayamas, when added to regular optimal medications, in asthma patients in improving health impairment quality of life.
Methods
Place of study
The present study was undertaken at the Departments of Physiology and Respiratory Medicine at our Institute. The patients were attending Respiratory Medicine out-patient department at our Institute where they were diagnosed and clinical care was provided. For the purpose of breathing exercises intervention, the patients attended Yoga Centre in the Department of the Physiology.
Study subjects and inclusion criteria
The diagnosis of asthma was made on the basis of clinical symptoms and presence of variable expiratory airflow limitation. The clinical features considered for asthma diagnosis included (i) presence of any one or more symptoms of wheeze, shortness of breath, cough, and chest tightness, (ii) symptoms worsening during night or in the early morning, (iii) symptoms varying over time and intensity, and (iv) symptoms triggered by viral infection, exercise, allergens, change in weather, laughter, or irritants such as smoke, fumes, or strong smells. The diagnosis of asthma in patients with these clinical characteristics was confirmed by spirometry that was assessed before and after the inhaled beta-2-agonist bronchodilators. An increase in forced expiratory volume in 1 s during forced expiratory maneuver (FEV1) by 200 ml or more than 12% of baseline value on repeat spirometry 20 min after inhalation of 200 mcg of levosalbutamol given through a metered dose inhaler along with a spacer was considered as a diagnosis of reversible airflow obstruction as per the American Thoracic Society guidelines.[11] Clinically suspected asthma patients who had reversible airflow obstruction and those who consented for the study as per the study plan were enrolled in the study. All study participants were residing within a radius of 15 km from our institute with easy access to institute for interventional breathing exercises. Patients with any cardiovascular complication were excluded from the study.
Study design
Each of eligible asthma patients had a regular follow-up for last 6 months before inclusion to the study and had no hospitalization due to asthma exacerbation during this period. The study patients had regular follow-up visits to clinical department at least once in a month with assessment of their clinical course, relevant laboratory, and spirometric evaluation. The study required a stable course during the last 3 months, and medicines in each patient were optimized before the last 3 months and continued during this period. The same individualized medicines were continued during the study intervention of breathing exercises.
Study interventions
As per the study protocol, all patients continued with their optimum individualized medication throughout the study period. The present study was designed to assess the benefit of addition of 3 months supervised breathing exercises to optimal medications in each study participant. Before being included to the study, the patients received detailed instructions regarding these exercises for 1 week to make the participants acquainted with nature and strenuosity of the exercises and to assess their willingness for consent to the study. After inclusion to the study, the study participants performed breathing exercises daily in front of the instructor for a week, and thereafter, till completion of 3 months, thrice a week on alternate days in front of the instructor and on rest of 4 days per week at home but with full support and understanding to attend the instructor for further supervisions. All patients maintained the diary for recording the duration and timing of the exercises and also to record the symptoms.
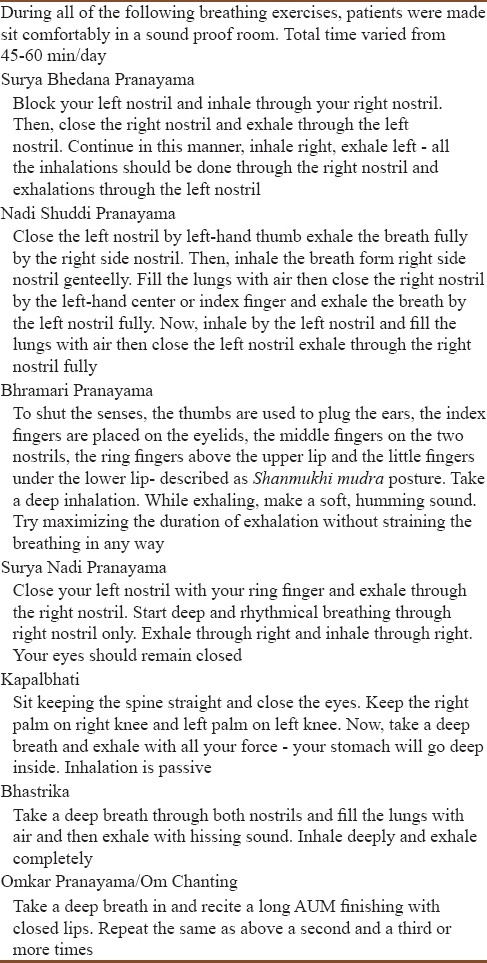
The breathing exercises assessed in the present study were all standard pranayamas; we adopted the methods described by Joshi.[12] The breathing exercises included Surya Bhedana Pranayama, Nadi Shuddi Pranayama, Bhramari Pranayama, Surya Nadi Pranayama, Kapalbhati, Bhastrika, and Omkar Pranayama/Om Chanting. A brief synopsis of these breathing exercises is shown in Table 1.
Table 1.
A brief synopsis of breathing exercises (Pranayamas)
Study parameters
SGRQ was used to assess the changes in health-related quality of life due to the study intervention. The used SGRQ had a 50-item questionnaire developed to measure health status suggesting quality of life in patients with airways obstruction. One month symptoms version of SGRQ was used to assess (i) symptom score, (ii) activity score, (iii) impact (Psychosocial) components scores, and (iv) total scores. Psychometric testing has been demonstrated its repeatability, reliability, and validity. Sensitivity has been demonstrated in clinical trials.[10] The SGRQ has been correlated significantly with other disease-related variables such as cough, dyspnea, 6-min walk test, and FEV1 as well as other measures of general health.[13]
SGRQ score assessments were done at baseline, i.e., at the initiation of breathing exercises intervention, and after the patients have completed 3 months of regular breathing exercises. The questionnaire was completed in a quiet room, free from distraction, and the patient sitting comfortably [Figure 1].
Figure 1.
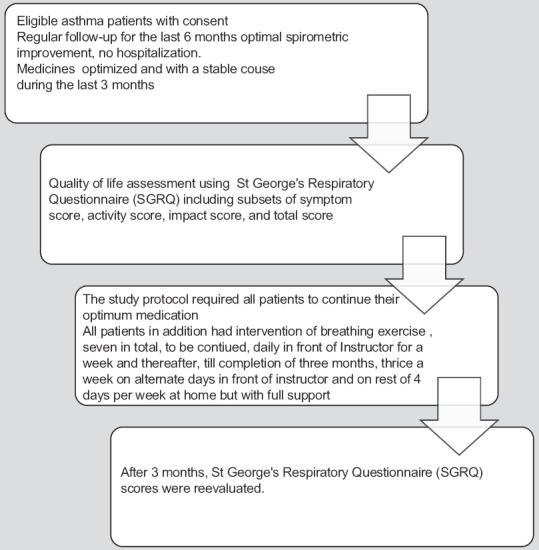
Patients’ flow during the study period
Results
A total of 60 asthma patients completed the entire study. There were 34 female and 26 male asthma patients. Each patient had diagnosed asthma for two or more years with a persistent but clinically stable course of the disease with individualized medications as per the GINA guidelines suitable to the requirements. All patients were nonsmokers. They were compliant to their medications and were attending the institute with regular follow-up. The medications for each study participant were optimized before the start of the additional intervention of breathing exercises and continued without any change throughout the study period. None of the patients had severe asthma, and also, there was no hospitalization for asthma-related illness during preceding 6 months.
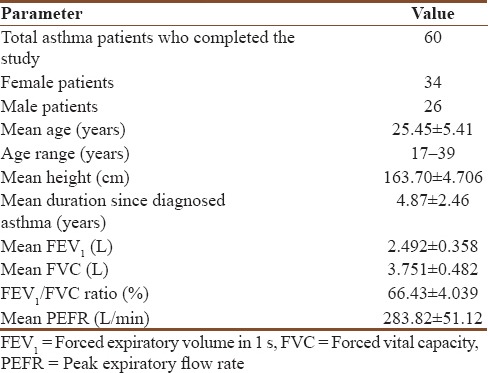
The baseline characteristics of the patients are described in Table 2. Their mean age was 25.45 ± 5.41 years, mean FEV1 was 2.492 ± 0.358 L, mean forced vital capacity (FVC) was 3.751 ± 0.482 L, FEV1/FVC ratio was 66.43 ± 4.039, and mean peak expiratory flow rate (PEFR) was 283.82 ± 51.12 L/min. Each of the study patients recruited to the study was able to carry out the scheduled breathing exercises under supervision as per the protocol. None of the participants had any acute exacerbation of asthma during the study period; there was no emergency department visit or any hospitalization due to asthma during this period. There was no drop-out from the study.
Table 2.
Patients’ baseline characteristics before starting the breathing exercises intervention
The mean SGRQ scores of all study patients for all subsets before and after the additional breathing exercises are shown in Table 3 and graphically depicted in Figure 2. SGRQ Symptoms scores decreased from 45.98 ± 5.61 to 38.78 ± 4.92, suggesting a significant decrease (P < 0.001) with breathing exercises. A significant improvement in activities of study patients was suggested by a decline in SGRQ Activity scores from 15.45 ± 3.33 to 12.34 ± 2.39. SGRQ impact scores significantly decreased from 17.95 ± 4.22 to 12.12 ± 3.82 (P < 0.001). The impact score component of SGRQ provides information regarding a range of disturbances of psychosocial function. This component relates in part to respiratory symptoms, but it also correlates with exercise performance, breathlessness in daily life, and disturbances of mood.
Table 3.
St. George's Respiratory Questionnaire subsets and total scores before starting and after completion of the breathing exercises
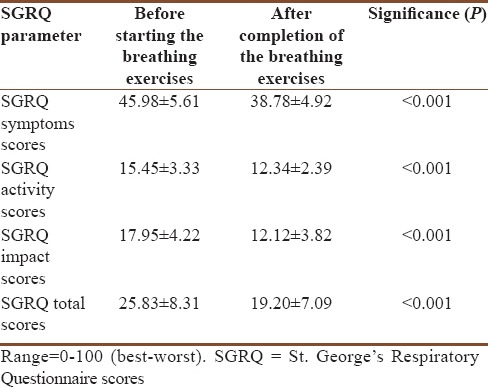
Figure 2.
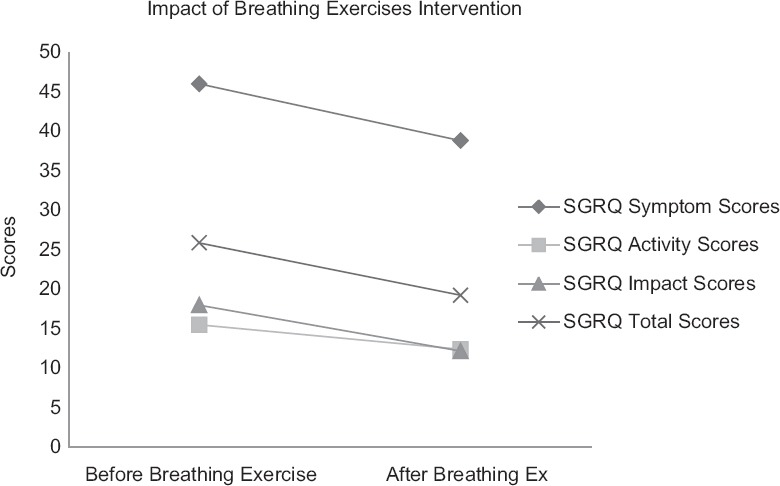
Reduction in St. George's Respiratory Questionnaire subsets and total scores after 3 months intervention of additional breathing exercises
The total SGRQ scores were also significantly decreased from 25.83 ± 8.31 to 19.20 ± 7.09 (P < 0.001) after breathing exercises intervention [Figure 2], signifying a global improvement in health-related quality of life.
The data from the present study suggest a decline in asthma symptoms, improvement with respect to activity limitations, and decline in adverse impact of asthma over the psychosocial life of the study patient by intervening breathing exercises when added to optimal pharmacological medications in patients with persistent bronchial asthma. A global improvement in quality of life of asthma patients was seen due to addition of breathing exercises.
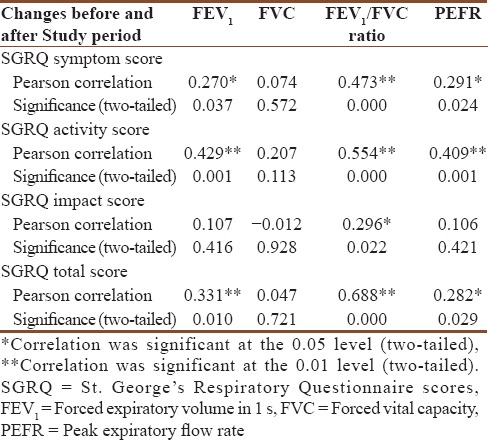
We also analyzed for correlations between baseline spirometric indices and the changes in SGRQ subsets scores as well as SGRQ total scores [Table 4]. There were significant correlations between decrease in symptoms, activity and total SGRQ scores and FEV1, FEV1/FVC ratio, and PEFR. Decrease in impact score was significantly related only with FEV1/FVC ratio.
Table 4.
Correlations between changes in St. George's Respiratory Questionnaire scores subset scores and the spirometric indices indicating disease severity
Discussion
As we know, asthma is a chronic disease with a major worldwide impact in terms of the extent and duration of disability. During the last couple of decades, there has been tremendous increase in our understanding regarding the pathogenesis and disease course in asthma leading to significant enhancement of medications armamentarium. In spite of availability of a wide variety of highly effective inhaled and oral pharmacological options for the treatment of asthma, the prevalence of asthma has been constantly increasing, currently very high and also projected to further rise in the near future. Many controlled clinical trials have observed asthma patients achieving high levels of control with optimized pharmacotherapy. However, recent assessments have shown that this optimism was unwarranted; asthma is still among the most common long-term conditions, it is incurable, and outcomes are not improving as expected.[14] Perhaps, an inappropriate sense of complacency arose with a feeling that we have mastered asthma, and asthma slipped down in priority in the health agenda. In “real-life” practice, poor control of asthma is common with over-reliance on rescue bronchodilator medication and patients continue to suffer from ongoing symptoms and quality-of-life impairment. Surveys show that the majority of people with asthma experience regular symptoms,[15] resulting in an impaired ability to lead a full productive life and a huge direct and indirect costs.[16] As the normal course of the disease is often characterized by recurrent episodes even with the best medications available, the major focus needs to be shifted to improve quality of life and the psychosocial well-being of asthma patients. The search for missing element to treat asthma may provide scope for nonpharmacological strategies such as breathing exercises, allergen avoidance, and lifestyle changes that we could make use of to help our patients cope better and to reduce the impact of asthma on their lives.
Breathing exercises are not new and have been taught for hundreds of years in both Eastern and Western societies for numerous conditions including asthma.[17] Collective evidence from the traditional practice of yoga and other similar physical therapies frequently indicates an improvement and sometimes elimination of asthma symptoms.[18] With the introduction of any new pharmacological molecule for control of asthma symptoms, the study trial grants were readily available to research workers by pharmaceutical companies to authenticate their medicines for obvious commercial uses and due to lack of incentives, research in nonpharmacological remained deprived. This is one of the reasons that there are no large-scale multicenter trials for evaluation of efficacy of breathing exercises in asthma patients.
There have been few studies or trials with small sample size to assess the efficacy of breathing exercises over the asthma outcome. There had been variations across different trials in terms of type of breathing exercise performed, number of study patients included, procedural differences, variations in efficacy parameters, statistical analyses, and outcomes of data. The outcomes more frequently measured were quality of life, asthma symptoms, number of acute exacerbations, and lung function. At least three different breathing techniques are used in these studies: (i) Buteyko method from Russia, (ii) Papworth method from the UK, and (iii) Pranayamas from India.
The Buteyko method that derives its name from a Ukrainian doctor Konstantin Pavlovich Buteyko proposes the use of breathing exercises as a treatment for asthma as well as other conditions such as sleep apnea, anxiety, and others. The Buteyko method is based on the concept that asthma is linked to undiagnosed hyperventilation.[19] The three-core principles of Buteyko are nasal breathing, reduced breathing, and relaxation. The British Thoracic Society stated that the Buteyko method may be considered to help patients control the symptoms of asthma while recognizing the lack of data showing an objective improvement in prior studies.[20]
In Papworth Method, a specific diaphragmatic breathing technique is taught to replace the use of inappropriate accessory muscles of respiration.[21] Emphasis, when relaxed, is placed on calm, slow nasal expiration. Patients are encouraged for nasal breathing rather than mouth breathing and for reduction of habits such as yawning and sighing.
The word Pranayama has derived from two Sanskrit words: Prana = life force and Yama = control, or mastery. Sri Patanjali, considered the “father of yoga,” is credited with compiling the Yoga Sutras.[22] Increasingly, yoga has become a transnational world practice with international followers with observation of the International Yoga Day on June 21, 2015 (the longest day of the year in Northern hemisphere), recognized by the United Nations General Assembly; the same is proposed to be repeated annually. The renewed public interest in physical therapy and other therapies is apparent by the proliferation of self-help books and an increase in the demand for complementary therapies.
There have been few prior studies which have assessed for the benefits of Pranayama or breathing exercises in asthma. The study by Nagarathna and Nagendra included 53 study participants of asthma and found significantly greater improvement in the group who practiced yoga in the weekly number of attacks of asthma, scores for drug treatment, and peak flow rate.[23]
In another study, yoga training was given for 7 days to nine bronchial asthma patients.[24] There was a reduction in sympathetic reactivity and an improvement in the pulmonary ventilation probably due to relaxation of voluntary inspiratory and expiratory muscles. The changes in lifestyle based on yoga training had significant benefits even within a short period.
One study included patients with bronchial asthma and had a study intervention of deep breathing, Brahmari, Anuloma viloma, and Omkara in 25 study patients along with 25 participants in control group.[25] They observed significant improvement in symptoms, FEV1, and PEFR. Many other studies[26,27,28] have also reported the beneficial effect of various pranayamas breathing exercises in management of asthma.
Cochrane review in 2013 observed that there were few high-quality studies looking at the efficacy of treating asthma with breathing retraining methods in general, which include the Buteyko method, yoga training, and other relaxation techniques and observed that no reliable conclusions could be determined based on limited available evidence.[29] This review concluded that while there are insufficient data for firm conclusions about efficacy, there is enough evidence to justify further trials.[29] Many studies that have evaluated breathing retraining have some methodological flaws, including small sample sizes; these studies are also hampered by the lack of proper blinding for obvious reasons and placebo control which could have introduce some bias into these studies.[30] The studies that have assessed quality of life reported an improvement in this outcome. The outcome from majority of studies favors breathing exercises for asthma symptoms though the impact over lung functions has been variable. As a result of substantial heterogeneity among the studies, meta-analysis was possible only for asthma symptoms and changes in the Asthma Quality of Life Questionnaire and showed a significant difference favoring breathing exercises. The reviews noted these techniques should only be used as adjuncts to conventional pharmacotherapy for symptom control. The British Thoracic Society stated that the Buteyko method might be considered to help patients control the symptoms of asthma while recognizing the lack of data showing an objective improvement in prior studies. The guideline also grades clinical research on Buteyko with a “B” classification – indicating that high quality supporting clinical trials are available.[31]
Psychological factors are observed to interact with the asthmatic diathesis to alter the course of the disease. Goyeche et al. claimed that the psychosomatic imbalance is present in many, if not all patients with asthma.[32] Suppressed emotion, anxiety, dependence, and extreme self-consciousness may all be accompanied by generalized and localized muscle tension, including that of the voluntary respiratory musculature. Modification of vagal efferent activity seems to affect the caliber of airways and may actually decrease or increase the effects of pharmacological stimuli on the airways. The role of the psychic factor in inducing or prolonging attacks in acute exacerbations may vary from patient to patient, and in an individual patient, from episode to episode.[23]
An expert guideline by the GINA noted that breathing exercises may be a useful supplement to asthma pharmacotherapy.[33] It has been suggested that improvement in symptoms by breathing exercises may be due to causes other than changes in the underlying physiology of the disease, such as relaxation, voluntary reduction in medication use, and increased participation of the patients in their own care. This result suggests that patients who experience anxiety or who overuse their rescue inhalers, in particular, may benefit from any breathing technique as an adjunct to conventional treatments. Regardless of whether the answers lie in a new physiological explanation or in an understanding of psychological reactions to the presence of a disease, the finding that something has made patients feel better means we cannot ignore this option. However, the supervisory breathing exercises are not available in many parts of the world and even if available cost of using these techniques may be prohibitive.[33]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reddel HK, Bateman ED, Becker A, Boulet LP, Cruz AA, Drazen JM, et al. A summary of the new GINA strategy: A roadmap to asthma control. Eur Respir J. 2015;46:622–39. doi: 10.1183/13993003.00853-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Croisant S. Heterogeneity in Asthma. US: Springer; 2014. Epidemiology of asthma: Prevalence and burden of disease; pp. 17–29. [DOI] [PubMed] [Google Scholar]
- 3.Mallol J, Crane J, von Mutius E, Odhiambo J, Keil U, Stewart A. the international study of asthma and allergies in childhood (ISAAC) phase three: A global synthesis. Allergol Immunopathol (Madr) 2013;41:73–85. doi: 10.1016/j.aller.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Global Burden of Asthma. [Last accessed on 2015 Jan 05]. Available from: http://www.ginasthma.org/Global-Burden-of-Asthma .
- 5.Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: Development of a questionnaire for use in clinical trials. Thorax. 1992;47:76–83. doi: 10.1136/thx.47.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams R, Wakefield M, Wilson D, Parsons J, Campbell D, Smith B, et al. Quality of life in asthma: A comparison of community and hospital asthma patients. J Asthma. 2001;38:205–14. doi: 10.1081/jas-100000107. [DOI] [PubMed] [Google Scholar]
- 7.Adams RJ, Wilson DH, Taylor A, Daly A, d’Espaignet E, Ruffin RE. Psychological distress and quality of life among people with asthma in the Australian population. Respirology. 2003;8:67–81. [Google Scholar]
- 8.Juniper EF. Assessing asthma quality of life: Its role in clinical practice. Breathe. 2005;1:192–205. [Google Scholar]
- 9.Cui W, Zack MM, Zahran HS. Health-related quality of life and asthma among United States adolescents. J Pediatr. 2015;166:358–64. doi: 10.1016/j.jpeds.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis. 1992;145:1321–7. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 11.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 12.Joshi KS. Yogic Pranayama. New Delhi: Orient Paperbacks; 1982. [Google Scholar]
- 13.Sanchez FF, Faganello MM, Tanni SE, Lucheta PA, Padovani CR, Godoy I. Relationship between disease severity and quality of life in patients with chronic obstructive pulmonary disease. Braz J Med Biol Res. 2008;41:860–5. doi: 10.1590/s0100-879x2008005000043. [DOI] [PubMed] [Google Scholar]
- 14.Martinez FD, Vercelli D. Asthma. Lancet. 2013;382:1360–72. doi: 10.1016/S0140-6736(13)61536-6. [DOI] [PubMed] [Google Scholar]
- 15.Demoly P, Gueron B, Annunziata K, Adamek L, Walters RD. Update on asthma control in five European countries: Results of a 2008 survey. Eur Respir Rev. 2010;19:150–7. doi: 10.1183/09059180.00002110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996;9:636–42. doi: 10.1183/09031936.96.09040636. [DOI] [PubMed] [Google Scholar]
- 17.Vedanthan PK, Kesavalu LN, Murthy KC, Duvall K, Hall MJ, Baker S, et al. Clinical study of yoga techniques in university students with asthma: A controlled study. Allergy Asthma Proc. 1998;19:3–9. doi: 10.2500/108854198778557971. [DOI] [PubMed] [Google Scholar]
- 18.Chandra FA. Respiratory Practices in Yoga. In: Timmons BH, Ley R, editors. Behavioral and Psychological Approaches to Breathing Disorders. New York: Plenum Press; 1994. pp. 221–32. [Google Scholar]
- 19.Cooper S, Oborne J, Newton S, Harrison V, Thompson Coon J, Lewis S, et al. Effect of two breathing exercises (Buteyko and pranayama) in asthma: A randomised controlled trial. Thorax. 2003;58:674–9. doi: 10.1136/thorax.58.8.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy ML, Thomas M, Small I, Pearce L, Pinnock H, Stephenson P. Summary of the 2008 BTS/SIGN British Guideline on the management of asthma. Prim Care Respir J. 2009;18(Suppl 1):S1–16. doi: 10.3132/pcrj.2008.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holloway EA, West RJ. Integrated breathing and relaxation training (the Papworth method) for adults with asthma in primary care: A randomised controlled trial. Thorax. 2007;62:1039–42. doi: 10.1136/thx.2006.076430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mishra SK, Singh P, Bunch SJ, Zhang R. The therapeutic value of yoga in neurological disorders. Ann Indian Acad Neurol. 2012;15:247–54. doi: 10.4103/0972-2327.104328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagarathna R, Nagendra HR. Yoga for bronchial asthma: A controlled study. Br Med J (Clin Res Ed) 1985;291:1077–9. doi: 10.1136/bmj.291.6502.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khanam AA, Sachdeva U, Guleria R, Deepak KK. Study of pulmonary and autonomic functions of asthma patients after yoga training. Indian J Physiol Pharmacol. 1996;40:318–24. [PubMed] [Google Scholar]
- 25.Saxena T, Saxena M. The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2:22–5. doi: 10.4103/0973-6131.53838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nagendra HR, Nagarathna R. An integrated approach of yoga therapy for bronchial asthma: A 3-54-month prospective study. J Asthma. 1986;23:123–37. doi: 10.3109/02770908609077486. [DOI] [PubMed] [Google Scholar]
- 27.Singh V, Wisniewski A, Britton J, Tattersfield A. Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with asthma. Lancet. 1990;335:1381–3. doi: 10.1016/0140-6736(90)91254-8. [DOI] [PubMed] [Google Scholar]
- 28.Manocha R, Marks GB, Kenchington P, Peters D, Salome CM. Sahaja yoga in the management of moderate to severe asthma: A randomised controlled trial. Thorax. 2002;57:110–5. doi: 10.1136/thorax.57.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freitas DA, Holloway EA, Bruno SS, Chaves GS, Fregonezi GA, Mendonça KP. Breathing exercises for adults with asthma. Cochrane Database Syst Rev. 2013;10:CD001277. doi: 10.1002/14651858.CD001277.pub3. [DOI] [PubMed] [Google Scholar]
- 30.Ernst E. Breathing techniques – adjunctive treatment modalities for asthma? A systematic review. Eur Respir J. 2000;15:969–72. doi: 10.1183/09031936.00.15596900. [DOI] [PubMed] [Google Scholar]
- 31.British Thoracic Society Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma. Thorax. 2008;63(Suppl 4):iv1–121. doi: 10.1136/thx.2008.097741. [DOI] [PubMed] [Google Scholar]
- 32.Goyeche JR, Abo Y, Ikemi Y. Asthma: The yoga perspective. Part II: Yoga therapy in the treatment of asthma. J Asthma. 1982;19:189–201. doi: 10.3109/02770908209104756. [DOI] [PubMed] [Google Scholar]
- 33.Global Strategy for Asthma Management and Prevention. 2015. [Last accessed on 2016 May 26]. Available from: http://www.ginasthma.org/documents/4 .


