Abstract
Introduction:
Urosepsis is one of the common causes of admission to the Intensive Care Unit (ICU). It has traditionally been treated with antibiotics, but surgical management with Double J [DJ] ureteral stents is gaining popularity. This study compares patients with complicated urosepsis who underwent surgical source control by ureteral stenting with those managed medically.
Materials and Methods:
The study enrolled patients admitted to a tertiary adult ICU with a diagnosis of urosepsis over a period of 2 years. The primary outcomes were renal replacement therapy (RRT) requirement and ICU mortality. The secondary outcomes were ICU and hospital length of stay, ventilator-free days, and inotrope free days. Patients were divided those with obstructive and nonobstructive urinary tract infection (UTI).
Results:
A total of 58 patients met the criteria, of who 32 had obstructive UTI and were included in Group A, with the remaining 26 with nonobstructive UTI comprised Group B. In Group A, 27 patients underwent source control with ureteral DJ stenting, three patients recovered with medical management, and two who were advised source control did not consent to the procedure. Seventeen patients in Group A and seven patients in Group B required RRT (P = 0.044). There was no significant difference in ICU mortality, hospital mortality, and 28 days survival between the two groups.
Conclusion:
With early source control, obstructive UTI outcomes were comparable to nonobstructive UTI. However, despite undergoing ureteric stenting, more patients with obstructive UTI required RRT than those with nonobstructive UTI.
Keywords: Early source control in urosepsis, nonobstructive uropathy, obstructive uropathy, ureteral stent
INTRODUCTION
Urinary tract infections (UTIs) admitted to THE Intensive Care Unit (ICU) have a high morbidity and may also carry a high mortality rate, especially in the late stage of presentation. Clinical features may range from asymptomatic bacteriuria to sepsis or septic shock, depending on localized or systemic extension.[1] A complicated UTI usually occurs in a patient with a structural or functional abnormality of the genitourinary tract. Morbidity and outcomes in these patients are principally determined by the underlying abnormality rather than the infection.[2]
UTIs have traditionally been treated with antibiotics. Surgical management with Double J [DJ] ureteral stents is gaining popularity in the treatment of obstructive UTI. This is an indwelling ureteral stent used to bypass intrinsic obstructions due to stones or ureteropelvic junction abnormalities and extrinsic compression, for example, by retroperitoneal tumors.[3] The device provides free drainage to the bladder, reduces or eliminates urine leakage, and allows for earlier discharge from the hospital of patients without external catheters.[4]
A Turkish study in 2014 concluded that DJ insertion in symptomatic pure gestational hydronephrosis adds no benefit to conservative treatment.[5] This study aims to compare the outcome in patients managed conservatively with those who underwent surgical source control.
MATERIALS AND METHODS
Design
This is a longitudinal study conducted at a tertiary referral ICU. It included all urosepsis patients admitted to ICU over a 20 months period from December 2013 to October 2015. The study was approved by the Institutional Ethical Board. Patients with a diagnosis of complicated urosepsis proven by evidence on abdominal ultrasonography or contrast-enhanced CT scan were included in the study. Exclusion criteria were age below 16 years and those with additional sources of sepsis. Patients were divided into two groups, Group A, who had obstructive UTI and underwent surgical intervention and Group B with nonobstructive UTI who were managed conservatively.
Data collection
Data were retrieved from the electronic medical records and daily case sheets, including demographics, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, and laboratory and imaging studies. The primary outcomes were renal replacement therapy (RRT) requirement and ICU mortality. The secondary outcomes were ICU and hospital length of stay, hospital mortality, 28 days survival, ventilator-free days, and inotrope-free days.
Statistical analysis
Data were analyzed using the statistical software SPSS (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY, IBM Corporation). Mann–Whitney U-test was used to compare the two groups. Skewed data, such as ICU length of stay, ventilator-free days, and hospital length of stay, were summarized in terms of median and IQR. P < 0.05 was considered as statistically significant.
RESULTS
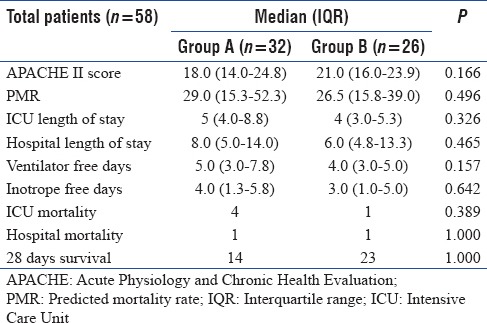
There were a total of 58 patients with complicated urosepsis, of whom 32 had obstructive UTI and were included in Group A. The remaining 26 had nonobstructive UTI and were included in Group B. Both groups had comparable demographics, as shown in Table 1. In Group A, 27 patients underwent source control with ureteral DJ stenting within the first 48 h of admission. Three patients recovered with medical management and two who were advised source control did not consent to the procedure. Three patients who recovered with medical management alone were not advised source control. The two patients who did not consent to the procedure were excluded from the final statistical analysis. Patients in Group A had higher creatinine levels at admission in comparison to Group B, but showed a consistent improvement in this, over the initial 3 days, as shown in Table 2. Seventeen patients in Group A and seven patients in Group B required RRT (P = 0.044). APACHE II scores and other outcome measures are shown in Table 3. There were four deaths in Group A and one in Group B while in ICU and 1 death in each group after shifting to wards. There was no significant difference in ICU and hospital length of stay, ICU mortality, hospital mortality, 28 days survival, ventilator, and inotrope free days in between the two groups.
Table 1.
Distribution of urosepsis patients according to age and gender
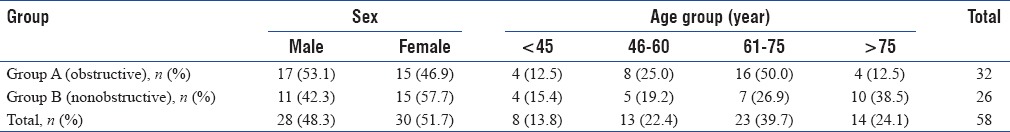
Table 2.
Number of patients requiring renal replacement therapy and creatinine trends
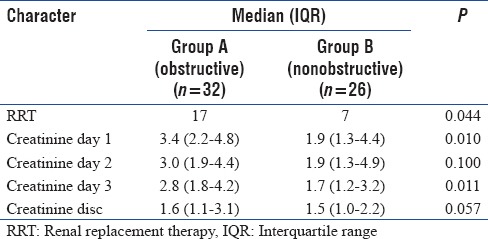
Table 3.
Comparison of Acute Physiology and Chronic Health Evaluation II scores, primary and secondary outcome measures
DISCUSSION
Obstruction to outflow of urine (obstructive uropathy) can occur anywhere in the urinary tract and is important to recognize early, as, if untreated, it can progress to urosepsis.[6] Antibiotics and supportive therapies form the mainstay of treatment in UTIs. A common site of obstruction is the ureter, due to stone, ureteropelvic junction stenosis, ureteral stricture, and genitourinary malignancies. In such cases, source control is possible by ureteroscopic insertion of DJ ureteral stents.[7]
In the present study, patients with obstructive uropathies (Group A) had higher creatinine levels at admission compared to those with nonobstructive urosepsis (Group B), but showed a steady reduction in this, following source control, such that both groups had comparable creatinine levels by day 3 of admission and at discharge. The creatinine levels were 2.8 and 1.7 in Group A and Group B, respectively, on day 3 of admission. The creatinine levels were 1.6 (Group A) and 1.5 (Group B) at discharge. However, despite this improvement in creatinine, more patients in Group A did require RRT than in group B, mainly due to metabolic acidosis. Escherichia coli was the most common causative organism, a finding is shared by a study on emphysematous pyelonephritis by Das and Pal[8] Carbapenems were the first choice of antibiotic.
Patients with obstructive uropathy are expected to have higher mortality. This study suggests that the early source control with both antibiotics and ureteral stenting can lead to comparable outcomes in obstructive uropathy and nonobstructive UTI, in terms of ICU and hospital length of stay, mortality, and 28 days survival.
There are several studies describing the various methods of source control, including DJ stenting and percutaneous nephrostomy (PCN) and their outcomes. These two methods have been described as minimally invasive.[9] In the study by Das and Pal,[8] out of 15 patients of emphysematous pyelonephritis, seven underwent JJ [DJ] stenting and four PCN and the rest improved by medical management alone. In all cases, source control was achieved within 48 h, as in our study. Again, E. coli were the most common causative organism as in our study. All patients showed improvement in renal function on follow-up. JJ stenting was the preferred method over PCN, as the former had a lesser morbidity and better outcome.
In another study on emphysematous pyelonephritis by Sharma et al.,[9] six out of fourteen patients required percutaneous drainage or DJ stenting. Of these six, one did not respond to the drainage procedures and had to undergo open drainage. On follow up, three patients did not recover renal function adequately and required nephrectomy. In both of the above studies, renal replacement therapy (RRT) was instituted when needed.
In a case report by Arsene et al.,[10] out of five patients with emphysematous pyelonephritis, one underwent both nephrostomy and ureteral stenting, one underwent ureteral stenting alone, another underwent nephrostomy, and two patients required nephrectomy. In our study, source control was achieved by DJ stenting alone, and none of the patients required nephrectomy.
Çeçen and Ülker in their study[5] comparing ureteral stenting and conservative management of Severe pure gestational hydronephrosis, suggest that DJ stent insertion in symptomatic pure gestational hydronephrosis has no benefit over conservative treatment and that it should be reserved for cases with complications or additional obstructive diseases.
CONCLUSION
Early source control in obstructive uropathy with broad-spectrum antibiotics and ureteral stenting can lead to outcomes comparable to nonobstructive UTI. However, despite undergoing ureteric stenting, more patients with obstructive UTI required RRT than those with nonobstructive UTI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wagenlehner FM, Pilatz A, Naber KG, Weidner W. Therapeutic challenges of urosepsis. Eur J Clin Invest. 2008;38(Suppl 2):45–9. doi: 10.1111/j.1365-2362.2008.02008.x. [DOI] [PubMed] [Google Scholar]
- 2.Nicolle LE AMMI Canada Guidelines Committee*. Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol. 2005;16:349–60. doi: 10.1155/2005/385768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Docimo SG, Dewolf WC. High failure rate of indwelling ureteral stents in patients with extrinsic obstruction: Experience at 2 institutions. J Urol. 1989;142:277–9. doi: 10.1016/s0022-5347(17)38729-3. [DOI] [PubMed] [Google Scholar]
- 4.Finney RP. Experience with new Double J ureteral catheter stent. J Urol. 1978;120:678–81. doi: 10.1016/s0022-5347(17)57326-7. [DOI] [PubMed] [Google Scholar]
- 5.Çeçen K, Ülker K. The comparison of Double J stent insertion and conservative treatment alone in severe pure gestational hydronephrosis: A case controlled clinical study. ScientificWorldJournal. 2014;2014:989173. doi: 10.1155/2014/989173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalra OP, Raizada A. Approach to a patient with urosepsis. J Glob Infect Dis. 2009;1:57–63. doi: 10.4103/0974-777X.52984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wenzler DL, Kim SP, Rosevear HM, Faerber GJ, Roberts WW, Wolf JS, Jr, et al. Success of ureteral stents for intrinsic ureteral obstruction. J Endourol. 2008;22:295–9. doi: 10.1089/end.2007.0201. [DOI] [PubMed] [Google Scholar]
- 8.Das D, Pal DK. Double J stenting: A rewarding option in the management of emphysematous pyelonephritis. Urol Ann. 2016;8:261–4. doi: 10.4103/0974-7796.184881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma PK, Sharma R, Vijay MK, Tiwari P, Goel A, Kundu AK, et al. Emphysematous pyelonephritis: Our experience with conservative management in 14 cases. Urol Ann. 2013;5:157–62. doi: 10.4103/0974-7796.115734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arsene C, Saste A, Arul S, Mestrovich J, Kammo R, Elbashir M, et al. A case series of emphysematous pyelonephritis. Case Rep Med. 2014;2014:587926. doi: 10.1155/2014/587926. [DOI] [PMC free article] [PubMed] [Google Scholar]


