Abstract
Aims:
Dengue is currently one of the most important mosquito-borne viral infections. Acute renal failure (ARF) is a serious complication among children suffering from dengue infection.
Subjects and Methods:
A retrospective cohort review of baseline characteristics, disease outcomes, and risk factors of dengue-infected patients, with and without renal failure (RF), were compared.
Results:
Among 97 children with dengue, 13.4% had RF (estimated glomerular filtration rate <60 ml/min/1.73 m2) at presentation. In comparison to all children (100%) of RF cohort, only 32% children of non-RF cohort (P < 0.0001) were suffering either from dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS). The 7-day survival rate was 61.5% (8/13) among RF group as compared to 96.4% (81/84) in non-RF group (P < 0.001). When a fraction of patients who needed vasopressor support were significantly higher in RF cohort (70% vs. 14% for RF and non-RF, respectively, P < 0.001), requirement of mechanical ventilation (15% vs. 11%, P = 0.67) was comparable in both cohorts.
Conclusions:
DHF/DSS is an independent risk factor for the development of ARF in patients with dengue infection. Mortality rate is high once RF develops in these children.
Keywords: Acute renal failure, dengue hemorrhagic fever, dengue shock syndrome, pediatric dengue infection
INTRODUCTION
Dengue is a systemic acute febrile tropical illness caused by dengue viruses (DEN-1 to DEN-5) and transmitted mostly by Aedes aegypti mosquitoes.[1] Despite socioeconomic development, the incidence rate of dengue viral infection is increasing with an annual estimate of 50–100 million cases worldwide.[2,3,4] The clinical presentations of dengue infections range from asymptomatic infection or a flu-like illness in classical dengue fever (DF) to the severe forms of dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS), which may cause fatalities. Acute kidney injury (AKI) is a serious complication of dengue. There are few studies in the literature demonstrating the impact of acute renal failure (ARF) in pediatric dengue infection.
SUBJECTS AND METHODS
Study design and setting
We retrospectively reviewed the medical records of all children (< 14 years) diagnosed with dengue between April 2012 and April 2016. The study was approved by the Institutional Review Board, and we adhered to the Declaration of Helsinki in conducting the study.
Inclusion and exclusion criteria
The diagnostic criteria for dengue infection were febrile illnesses associated with one of the following laboratory confirmation tests: (1) positive reverse transcriptase polymerase chain reaction, (2) detection of nonstructural protein 1 antigen, and (3) detection of dengue-specific IgM antibody-capture enzyme-linked immunosorbent assay antibody. Cases with only a single-positive dengue IgG result and/or history of preexisting chronic kidney disease or without detailed history were excluded.
Definitions
According to the criteria of the World Health Organization (WHO), patients who have DF and hemorrhagic manifestations, low platelet count (≤1 lac/μl), and objective evidence of leaky capillaries (≥20% elevation in hematocrit, lower serum albumin, and pleural or other effusions) are classified as having DHF (WHO classification, DHF Grades I/II). Those with evidence of circulatory failure (pulse pressure ≤20 mmHg, hypotension, or frank shock) are classified as having DSS (WHO classification, DHF Grades III/IV). We defined renal failure (RF) if estimated glomerular filtration rate (eGFR) was <60 ml/min/1.73 m2 at admission. eGFR was calculated according to the modified Schwartz formula.
Baseline parameters and follow-up data
The included dengue patients were divided into two groups: patients who developed ARF (study group) and those who did not (control group). For each patient, the following data were collected: gender, demographic data, age, clinical manifestations, treatment received, medical history of any underlying diseases, history of dengue infection, clinical course, and final outcome. The data were compared between two groups.
Outcome measurement
The primary outcome was patient survival. Secondary outcomes were renal survival, duration of support with mechanical ventilation or vasopressor, and time to hospital discharge. Clinical course of the disease and final outcome-related data were recorded daily until 7 days following hospital admission.
Statistical analysis
Between groups, data for continuous variables were evaluated using a t-test for independent variables. Comparisons of proportions were made using Chi-squared testing. Kaplan–Meier survival analysis was performed, and the survival probability was compared between the study arms using log-rank test. Throughout the text, data are expressed as means ± standard deviations, medians (lower and upper extremities), and percentages, as appropriate, and P < 0.05 was considered statistically significant. The SPSS for Windows version 16 software (SPSS Inc., Chicago, Illinois, USA) was used for all statistical analyses.
RESULTS
Baseline demographics
A total of 97 children were diagnosed with dengue infection during the study period. Of them, 13 (13.4%) patients had eGFR <60 ml/min/1.73 m2 at admission and classified as RF cohort. The baseline patient characteristics of two treatment cohorts are summarized in Table 1. All children (100%) of RF cohort were either with DHF or DSS.
Table 1.
Baseline characteristics and fatalities of patients of both cohorts
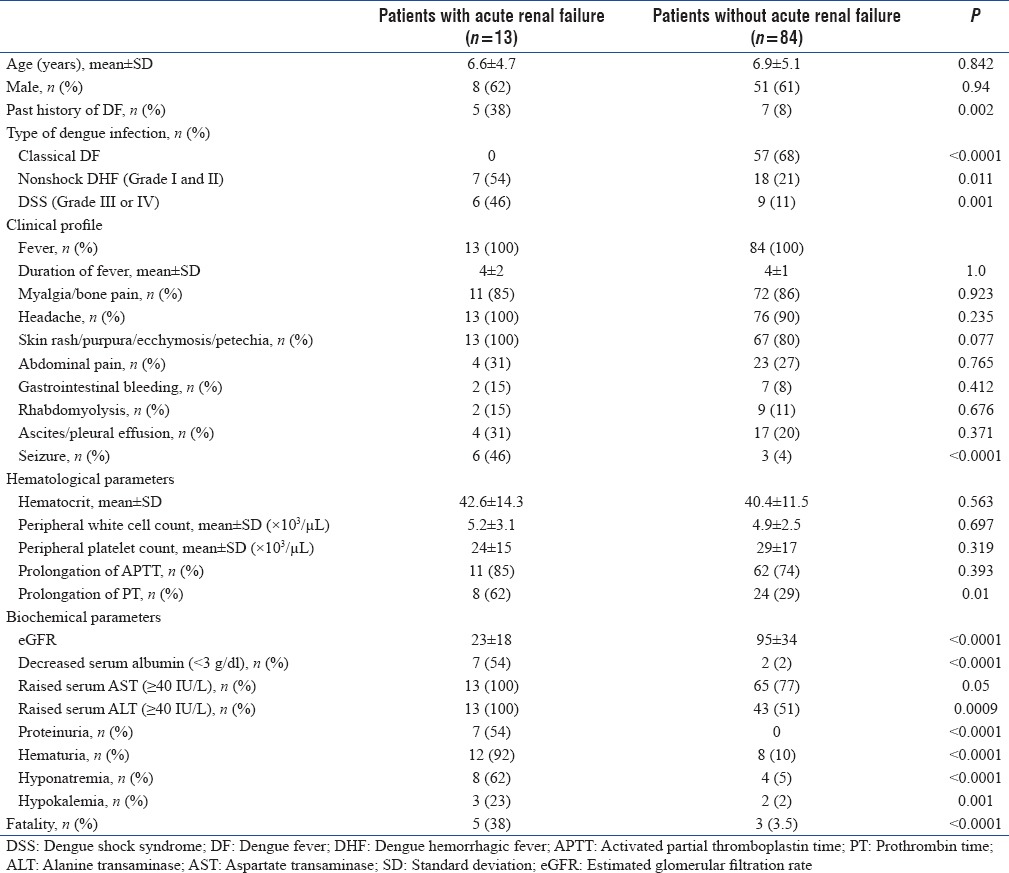
Clinical course
Management of dengue was done according to the WHO guideline, 2009. A fraction of patients in need of vasopressor were significantly higher in RF cohort in comparison to non-RF cohort (70% vs. 14% for RF and non-RF, respectively, P < 0.001). However, requirement of mechanical ventilation (15% vs. 11% for RF and non-RF, respectively, P = 0.67) was comparable in both cohorts. Total duration (days) of mechanical ventilation (2 ± 1 vs. 4 ± 1, P < 0.001) and of vasopressor use (2 ± 1 vs. 3 ± 1, P = 0.001) was significantly lower in the non-RF than in the RF group. Duration of hospital stay was also longer among RF patients (median 6 days; range 4–18 days) when compared to others (median 4 days; range 1–12 days) (mean 2 ± 1 vs. 4 ± 1 days, P < 0.001).
Patient survival
A total of 8 (21.6%) patients died within 7 days of hospital admission. There was no further disease-related mortality after the 1st week. Among eight deaths, five were from RF cohort and three were from the other cohort. All five deaths (two of them were on renal replacement therapy [RRT]) of RF cohort were either due to refractory shock or due to multiple-organ dysfunction syndrome. Among three deaths in non-RF cohort, one died from refractory shock and two patients died due to associated overwhelming secondary sepsis. All five deaths of RF cohort were categorized as DSS, whereas there was only single death among patients with DSS of the other cohort. The actuarial patient survival by cohort is given in Figure 1. The 7-day survival rate was 61.5% (8/13) in the RF group as compared to 96.4% (81/84) in the non-RF group (P < 0.001) [Figure 1].
Figure 1.
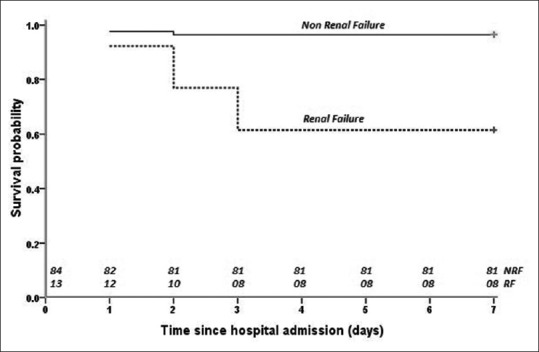
Kaplan–Meier survival curve of nonrenal failure and renal failure cohorts over the study period (log-rank P < 0.001)
Renal outcome
Among 13 patients of RF cohort, eight patients require RRT for varying period (median 2 days; range 1–6 days). The mean biochemical indices of kidney function improved in all RF patients from day 1 of hospital admission. All surviving patients with RF had come off dialysis within 7 days. Renal recovery continued during further follow-up.
Prognostic factors
In comparison to all children (100%) of RF cohort, only 32% children of non-RF cohort were suffering either from DHF or DSS. Among total eight deaths of both cohorts, 6 (75%) were below 5 years of age. Hence, these factors might be associated with unfavorable treatment response.
DISCUSSION
AKI is a significant, albeit poorly studied, complication of dengue. There are few studies in the literature demonstrating impact of ARF in pediatric dengue infection. In this retrospective cohort study, we investigated the potential impact of ARF on patient survival and renal recovery in the management of pediatric dengue infection. As a tertiary referral center, the higher incidence (13%) of complicated ARF with DHF/DSS in our study population might be biased by patient selection and referral pattern. The reported frequency of this association exhibits wide variation in accordance to the particular population being assessed, severity of dengue, criteria used for the diagnosis of RF, and time of evaluation.[4,5,6,7] Studies reported an incidence of 0.9%–4% AKI among children with dengue depending on the diagnostic criterion.[4,5,6,7] A study that used the AKI Network (AKIN) criteria for diagnosis showed that the incidence of AKI was 10.8% among dengue patients.[7] In another retrospective analysis, AKI was detected among 13.3% cases, using the same AKIN criteria.[8]
In line with the previously published studies, all patients with RF were presented with either DHF or DSS in our study population. This study demonstrates that patients with DHF and especially DSS have significantly higher risks of RF and mortality. Hence, DHF/DSS and RF generate a vicious cycle in these patients resulting in poor survival. Retrospective studies of case series of dengue have shown that the development of RF was associated with a longer hospital stay and higher mortality.[8,9]
Several mechanisms have been proposed to account for the etiopathogenesis of RF in dengue, including direct action by the virus, hemodynamic instability, rhabdomyolysis, hemolysis, and acute glomerular injury.[10]
Notably, most deaths in both cohorts occurred within 3 days of hospital admission, pointing to disease severity at presentation rather than the disease progression during hospital stay as the leading cause of mortality. In spite of adequate RRT, increased mortality in RF group pointed toward predominant hazard in the successful management of more severe disease (DHF/DSS) when complicated with RF linked to the intermittent dialysis procedure. This is also suggested by the higher need for vasopressor support observed during treatment with RF cohort as compared to non-RF cohort. On the contrary, two fatalities in the non-RF group occurred due to overwhelming sepsis whereas only one expired because of refractory shock.
Vigilant assessment of the warning signs of dengue and the patient's blood volume are crucial for the prevention of AKI. Fluid replacement should be performed carefully to avoid hypovolemia or fluid overload, which detrimentally affects mortality. RRT is currently indicated as conventionally used to treat RF patients because there are no specific recommendations for the proper time to begin treatment, dosing, or modality in dengue patients. Dialytic management in our children was individualized by a pediatric intensivist and nephrologist team based on the patient's specific clinical and hemodynamic status. In general, we preferred peritoneal dialysis in children <5 years of age and hemodialysis for older children.
We recognize several limitations of our study. These included its retrospective character and the relatively small group sizes which precluded a powerful statistical analysis.
CONCLUSION
In conclusion, our data showed that DHF/DSS is an independent risk factor for the development of ARF in patients with dengue infection. Mortality rate is high once RF develops in these children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Normile D. Tropical medicine. Surprising new dengue virus throws a spanner in disease control efforts. Science. 2013;342:415. doi: 10.1126/science.342.6157.415. [DOI] [PubMed] [Google Scholar]
- 2.Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11:480–96. doi: 10.1128/cmr.11.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kautner I, Robinson MJ, Kuhnle U. Dengue virus infection: Epidemiology, pathogenesis, clinical presentation, diagnosis, and prevention. J Pediatr. 1997;131:516–24. doi: 10.1016/s0022-3476(97)70054-4. [DOI] [PubMed] [Google Scholar]
- 4.Malavige GN, Fernando S, Fernando DJ, Seneviratne SL. Dengue viral infections. Postgrad Med J. 2004;80:588–601. doi: 10.1136/pgmj.2004.019638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinheiro FP, Corber SJ. Global situation of dengue and dengue haemorrhagic fever, and its emergence in the Americas. World Health Stat Q. 1997;50:161–9. [PubMed] [Google Scholar]
- 6.Halstead SB. Is there an inapparent dengue explosion? Lancet. 1999;353:1100–1. doi: 10.1016/S0140-6736(05)76460-6. [DOI] [PubMed] [Google Scholar]
- 7.Mehra N, Patel A, Abraham G, Reddy YN, Reddy YN. Acute kidney injury in dengue fever using acute kidney injury network criteria: Incidence and risk factors. Trop Doct. 2012;42:160–2. doi: 10.1258/td.2012.120023. [DOI] [PubMed] [Google Scholar]
- 8.Khalil MA, Sarwar S, Chaudry MA, Maqbool B, Khalil Z, Tan J, et al. Acute kidney injury in dengue virus infection. Clin Kidney J. 2012;5:390–4. doi: 10.1093/ckj/sfs117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalil MA, Tan J, Khalil MA, Awan S, Rangasami M. Predictors of hospital stay and mortality in dengue virus infection-experience from Aga Khan university hospital Pakistan. BMC Res Notes. 2014;7:473. doi: 10.1186/1756-0500-7-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lima EQ, Nogueira ML. Viral hemorrhagic fever-induced acute kidney injury. Semin Nephrol. 2008;28:409–15. doi: 10.1016/j.semnephrol.2008.04.009. [DOI] [PubMed] [Google Scholar]


