Abstract
Objective:
Chikungunya is generally a mild disease, rarely requiring Intensive Care Unit (ICU) admission. However, certain populations may develop organ dysfunction necessitating ICU admission. The purpose of the study was to assess the clinical profile and course of chikungunya patients admitted to the ICU, and to ascertain factors linked with poor outcome.
Methods:
All patients with chikungunya admitted to ICU were included in the study. Admission Acute Physiology and Chronic Health Evaluation (APACHE) II score and sequential organ failure assessment (SOFA) score were calculated. Primary outcome measured was 28-day mortality and secondary outcomes measured were length of hospital and ICU stay and the need for vasopressor support, renal replacement therapy (RRT), and mechanical ventilation (MV). Logistic regression analysis was performed to identify factors predicting mortality.
Results:
The most common complaints were fever (96.67%) and altered sensorium (56.67%). Mean admission APACHE II and SOFA scores were 17.28 ± 7.9 and 7.15 ± 4.2, respectively. Fifty-one patients had underlying comorbidities. Vasopressors were required by 46.76%; RRT by 26.67%, and MV by 58.33%, respectively. The 28-day mortality was 36.67%. High APACHE II score (odds ratio: 1.535; 95% confidence interval: 1.053–2.237; P = 0.026) and need for dialysis (odds ratio: 833.221; 95% confidence interval: 1.853–374,664.825; P = 0.031) could independently predict mortality.
Conclusions:
Patients with chikungunya fever may require ICU admission for organ failure. They are generally elderly patients with underlying comorbidities. Despite aggressive resuscitation and organ support, these patients are at high risk of death. Admission APACHE II score and need for dialysis may predict patients at higher risk of death.
Keywords: Acute Physiology and Chronic Health Evaluation II score, chikungunya, sequential organ failure assessment score, viral tropism
INTRODUCTION
Chikungunya is a rapidly emerging health problem, especially in developing countries, causing about 3 million infections each year. It is estimated that about 1.3 billion people are living in areas at risk of chikungunya virus (CHIKV) transmission.[1]
CHIKV is a single-stranded RNA virus belonging to the alphavirus genus of the family Togaviridae. It is an arthropod-borne virus transmitted to humans primarily by the bite of Aedes aegypti mosquito. CHIKV infection is usually a benign disease classically associated with fever, rash, myalgia, and arthralgia. Severe forms of CHIKV infection, though rare, have been reported in the past with occurrence of CHIKV-related deaths.[2,3,4]
The first outbreak of chikungunya infection dates back to 1952 in Tanzania,[5] while in India, the first outbreak was reported in 1963 in Calcutta.[6] After a dormancy of nearly 41 years, a number of outbreaks of chikungunya have been reported in India and Southeast Asia, over the past decade.[7,8]
Up until 1973, the attack rate of chikungunya in India was 37.5%, which considerably rose to 45% in the 2006 epidemic.[9] Even though no deaths were directly attributable to the disease, an increased mortality rate was observed during the epidemic when compared to previous year death rates.
Organ dysfunction in CHIKV infection may manifest as encephalopathy or encephalitis, respiratory failure, hepatic impairment, renal impairment, bleeding manifestations, and cardiovascular dysfunction or collapse.[10] Such patients require rigorous monitoring and care, and their outcome depends on early recognition and aggressive management of shock and organ failure. The need for Intensive Care Unit (ICU) admission for severe chikungunya infection was first reported during the Reunion Island epidemic in 2006.[4] Over the past couple of years, we have witnessed an increasing need for ICU admission in patients with chikungunya infection.[2,3]
The objective of our study was to observe the clinical profile, laboratory parameters, ICU course, complications, and outcome of critically ill patients with CHIKV infection and to identify any risk factors associated with increased mortality.
METHODS
This was a prospective, observational study conducted in the medical ICUs of a tertiary care hospital in New Delhi, India, over a period of 6 months, from May 2016 to October 2016. All adult patients diagnosed with chikungunya and admitted to the ICU were included in the study. Infection was confirmed either by positive reverse transcriptase-polymerase chain reaction assay (Geno Sen's chikungunya) or by the presence of serum immunoglobulin-M antibodies (Advantage chikungunya IgM card – J. Mitra and Co. Pvt. Ltd.) to CHIKV. The study protocol was approved by the Institutional Ethics Committee.
All patients underwent a detailed clinical examination. Routine investigations such as complete hemogram, kidney function tests, liver function tests, coagulation profile, and chest X-ray were done for all patients on admission. Standardized proforma was used to collect and analyze the clinical and laboratory data. Since there is no specific antiviral therapy for CHIKV infection, patient management was mainly directed toward symptom relief, optimizing hemodynamic parameters, and organ support.
Severity of illness and organ failure was assessed by Acute Physiology and Chronic Health Evaluation (APACHE) II score[11] and sequential organ failure assessment (SOFA) score,[12] respectively, calculated at the time of ICU admission. Organ failure was defined as a SOFA score >2 for that particular organ system. Admission lactate values were recorded. Sepsis and septic shock were defined as per Sepsis 3.0 definition.[13]
The primary outcome measured was 28-day mortality and the secondary outcomes measured were the length of stay in hospital, length of stay in ICU, and the need for vasopressor support, renal replacement therapy (RRT), and mechanical ventilation (MV).
Nonsurvivors were defined as those who died either during their ICU stay or within 28 days of ICU discharge.
Statistical analysis
We used SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) software for the statistical analysis. The means of continuous variables were compared using Student's t-test, and the categorical variables were compared using Chi-square test or Fisher's exact test as appropriate, with P < 0.05 being considered statistically significant. Univariate and multivariate logistic regression analyses were performed to assess factors predicting mortality.
OBSERVATIONS AND RESULTS
Out of the total 756 admissions during the study period, sixty patients, who were diagnosed with acute chikungunya infection, were included in the study. Our study population had a male predominance, there being 43 males (71.67%) and 17 females (28.33%). The mean age was 65.72 ± 17.4 years, with an age range of 18–88 years. Fifty-one patients (85%) suffered from underlying comorbidities such as diabetes mellitus (DM), hypertension (HTN), hypothyroidism, ischemic heart disease (IHD), Parkinson's disease, myasthenia gravis, and chronic kidney disease.
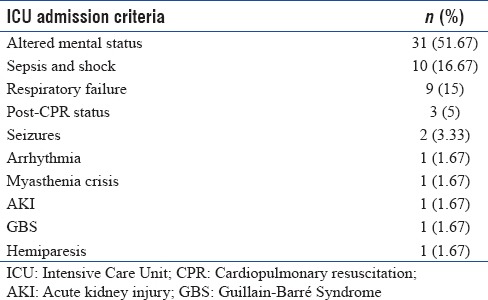
The most common complaints were fever (96.67%) followed by altered sensorium (56.67%) [Table 1]. Rash (8.33%) and bleeding manifestations (3.33%) were rare. The most common reason for ICU admission was altered sensorium which was seen in 31 patients (51.67%) [Table 2]. Other reasons for ICU admission were sepsis and shock in ten patients, respiratory failure in nine patients, seizures in two patients, and arrhythmia, decreased urine output, myasthenic crisis, Guillain-Barré syndrome, and focal neurological deficit in one patient each. Three patients were admitted to the ICU after cardiac arrest. Two of these three patients suffered from aspiration pneumonia secondary to low Glasgow coma scale score while one patient had multiorgan dysfunction which led to cardiac arrest. All three patients were elderly and suffered from multiple comorbidities such as DM, HTN, chronic obstructive pulmonary disease, and IHD.
Table 1.
Most common presenting complaints (n=60)
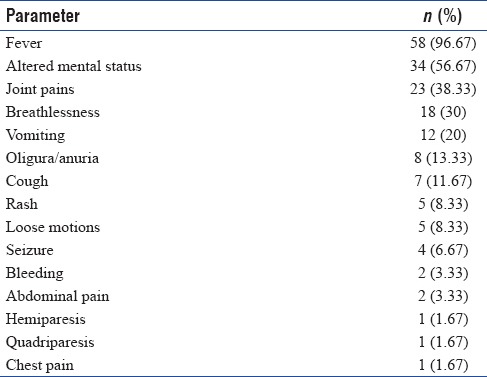
Table 2.
Intensive Care Unit admission criteria (n=60)
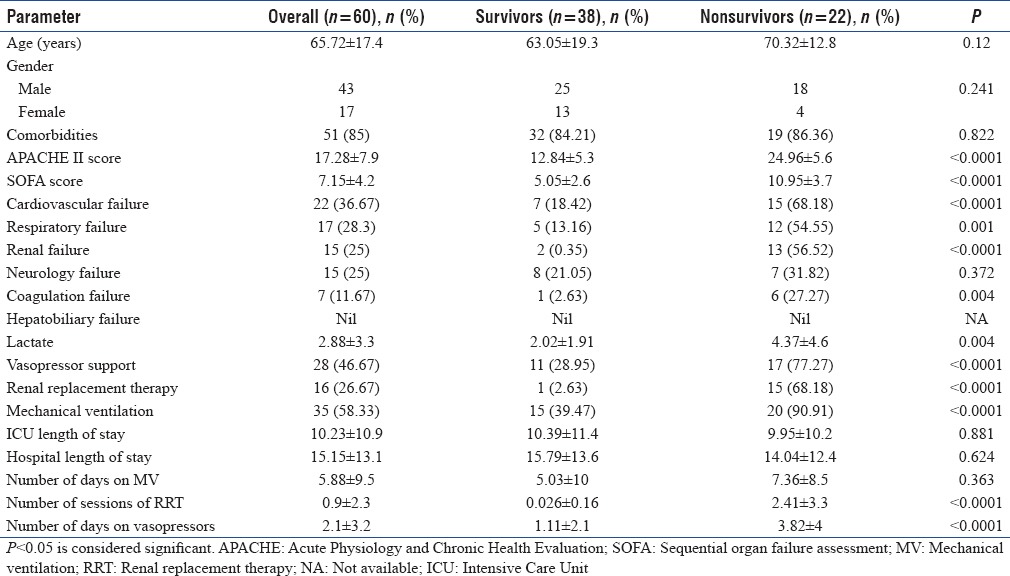
The mean lactate level on admission was 2.88 ± 3.3. Mean admission APACHE II and SOFA scores were 17.28 ± 7.9 and 7.15 ± 4.2, respectively. The most common organ failure was cardiovascular (36.67%), followed by respiratory failure (28.33%) and renal failure (25%). MV was required in 58.33%, vasopressors by 46.67%, and RRT by 26.67% cases, respectively. The average total number of days on MV was 5.88 ± 9.5, RRT was 0.9 ± 2.3, and vasopressor support was 2.1 ± 3.2. The mean length of ICU stay was 10.23 ± 10.9 days, while the average duration of hospital stay was 15.15 ± 13.1 days. The primary outcome, i.e., the 28-day mortality, was 36.67%.
Six factors, which were statistically significant in univariate analysis [Table 3], serum lactate levels, APACHE II score, SOFA score, and need for MV, RRT, and vasopressors, were analyzed in a multivariate analysis model. On multivariate analysis, only two parameters, i.e., high APACHE II score (odds ratio, 1.53; 95% confidence interval: 1.05–2.24; P = 0.030) and need for RRT (odds ratio, 946.63; 95% confidence interval: 1.85–374664.83; P = 0.031) could independently predict mortality.
Table 3.
Comparison of baseline patient characteristics between survivors and nonsurvivors
DISCUSSION
Majority of patients with chikungunya infection exhibit a self-limiting disease. There are no known predictors for the development of severe life-threatening disease. However, extremes of age and preexisting comorbidities increase the risk for such severe disease and may necessitate ICU admission.[14] Timely diagnosis, aggressive therapy, and careful observation for deterioration would help improve outcome in such patients. However, the presence of any organ failure may indicate a more serious form of disease requiring ICU admission and may be associated with increased mortality. We observed a staggering 28-day mortality of 36.67% in our study. Admission APACHE II score and need for RRT were found to be independent predictors of mortality.
In our study population, the mean age was 65.72 years, signifying an older age group being more commonly affected with the severe form of the disease. However, there was no significant age difference between survivors and nonsurvivors. Males were more commonly affected as compared to females. A majority (85%) of our patients had preexisting comorbidities. This is in agreement with previous studies,[2,4,15] wherein a more severe form of disease was witnessed in patients with known debilitating conditions.
The most common symptom at presentation was fever followed by altered mental status. The most common reason for ICU admission was altered mentation. This is in sync with the study by Lemant et al.,[3] wherein encephalopathy was the most common manifestation for ICU admission. Similarly, in a study by Crosby et al.,[2] 17% of the admitted patients presented with neurological dysfunction possibly related to CHIKV infection.
Sepsis and shock needing intensive care were seen in ten patients and was the second most common reason for ICU admission. Sepsis and shock though considered uncommon with chikungunya have been reported during the Caribbean outbreak in 2013–2014,[2] and in some patients from Venezuela[15] and Colombia.[16] Although the exact pathophysiology for hemodynamic failure is unknown, it may be similar to that observed in other arbovirus diseases such as dengue fever.
The mean admission APACHE II score in our study was high (17.28 ± 7.9) further underlining the severity of the disease, with a significant difference between survivors and nonsurvivors (P < 0.0001). However, APACHE II score is not specific for chikungunya infection and only helps assess the severity of illness, to determine which patients may have an unfavorable outcome.
The mean SOFA score on admission was high, but there was no significant difference between survivors and nonsurvivors on multivariate analysis.
Organ failure scores showed that the most common organ failures (in decreasing order of frequency) were cardiovascular followed by respiratory, renal, neurological, and coagulation. Even though a few patients had transaminitis, none had hepatobiliary failure. Only the need for RRT showed statistically significant difference between survivors’ and nonsurvivors. A similar study in Yemen showed that about 220 patients with chikungunya, had acute renal failure with 78 (35%) of these, needing dialysis and 59 (27%) of those succumbed to illness.[17] These observations highlight the neurological and myocardial tropism exhibited by the CHIKV.[18]
The 28-day mortality of 36.67% in our study population is higher than that reported in past literature.[2,4] This may be explained by the fact that our study population comprised of severe cases of chikungunya admitted to the ICU of a tertiary care setup and not the overall number of chikungunya cases admitted to the hospital.
Limitations
Although this is one of the larger studies conducted in chikungunya patients admitted in ICU, our study did have a few limitations. This was a single-center study, conducted at a tertiary care hospital with advanced facilities and hence application of results to the population as a whole may be difficult.
CONCLUSIONS
Patients with severe form of chikungunya may require ICU admission with early institution of aggressive organ support and care. A higher APACHE II score is associated with a poorer outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nsoesie EO, Kraemer MU, Golding N, Pigott DM, Brady OJ, Moyes CL, et al. Global distribution and environmental suitability for chikungunya virus, 1952 to 2015. Euro Surveill. 2016:21. doi: 10.2807/1560-7917.ES.2016.21.20.30234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crosby L, Perreau C, Madeux B, Cossic J, Armand C, Herrmann-Storke C, et al. Severe manifestations of chikungunya virus in critically ill patients during the 2013-2014 Caribbean outbreak. Int J Infect Dis. 2016;48:78–80. doi: 10.1016/j.ijid.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Lemant J, Boisson V, Winer A, Thibault L, André H, Tixier F, et al. Serious acute chikungunya virus infection requiring intensive care during the Reunion Island outbreak in 2005-2006. Crit Care Med. 2008;36:2536–41. doi: 10.1097/CCM.0b013e318183f2d2. [DOI] [PubMed] [Google Scholar]
- 4.Economopoulou A, Dominguez M, Helynck B, Sissoko D, Wichmann O, Quenel P, et al. Atypical Chikungunya virus infections: Clinical manifestations, mortality and risk factors for severe disease during the 2005-2006 outbreak on Réunion. Epidemiol Infect. 2009;137:534–41. doi: 10.1017/S0950268808001167. [DOI] [PubMed] [Google Scholar]
- 5.Robinson MC. An epidemic of virus disease in Southern Province, Tanganyika Territory, in 1952-53. I. Clinical features. Trans R Soc Trop Med Hyg. 1955;49:28–32. doi: 10.1016/0035-9203(55)90080-8. [DOI] [PubMed] [Google Scholar]
- 6.Shah KV, Gibbs CJ, Jr, Banerjee G. Virological investigation of the epidemic of haemorrhagic fever in Calcutta: Isolation of three strains of Chikungunya virus. Indian J Med Res. 1964;52:676–83. [PubMed] [Google Scholar]
- 7.Azami NA, Salleh SA, Shah SA, Neoh HM, Othman Z, Zakaria SZ, et al. Emergence of chikungunya seropositivity in healthy Malaysian adults residing in outbreak-free locations: Chikungunya seroprevalence results from the Malaysian cohort. BMC Infect Dis. 2013;13:67. doi: 10.1186/1471-2334-13-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pulmanausahakul R, Roytrakul S, Auewarakul P, Smith DR. Chikungunya in Southeast Asia: Understanding the emergence and finding solutions. Int J Infect Dis. 2011;15:e671–6. doi: 10.1016/j.ijid.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Mavalankar D, Shastri P, Bandyopadhyay T, Parmar J, Ramani KV. Increased mortality rate associated with chikungunya epidemic, Ahmedabad, India. Emerg Infect Dis. 2008;14:412–5. doi: 10.3201/eid1403.070720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajapakse S, Rodrigo C, Rajapakse A. Atypical manifestations of chikungunya infection. Trans R Soc Trop Med Hyg. 2010;104:89–96. doi: 10.1016/j.trstmh.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 11.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 12.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 13.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atlanta: Chikungunya Virus; [Last accessed on 2017 Dec 31]. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/chikungunya/hc/clinicalevaluation.html . [Google Scholar]
- 15.Torres JR, Leopoldo Códova G, Castro JS, Rodríguez L, Saravia V, Arvelaez J, et al. Chikungunya fever: Atypical and lethal cases in the Western hemisphere: A Venezuelan experience. IDCases. 2015;2:6–10. doi: 10.1016/j.idcr.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoz JM, Bayona B, Viloria S, Accini JL, Juan-Vergara HS, Viasus D, et al. Fatal cases of Chikungunya virus infection in Colombia: Diagnostic and treatment challenges. J Clin Virol. 2015;69:27–9. doi: 10.1016/j.jcv.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Al Nsour M, Kaiser R, Abd Elkreem E, Walke H, Kandeel A, Bloland R, et al. Highlights and conclusions from the Eastern Mediterranean Public Health Network (EMPHNET) conference 2011. East Mediterr Health J. 2012;18:189–91. doi: 10.26719/2012.18.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pellot AS, Alessandri JL, Robin S, Sampériz S, Attali T, Brayer C, et al. Severe forms of chikungunya virus infection in a pediatric Intensive Care Unit on Reunion Island. Med Trop (Mars) 2012;72:88–93. [PubMed] [Google Scholar]


