Abstract
Natural killer/T-cell lymphoma (NKTCL) is a rare subtype of non-Hodgkin lymphoma that is associated with a poor outcome. Currently, the treatment needs of NKTCL remain unmet, and efforts to further improve treatment are urgently needed. Herein, seven patients with NKTCL who failed to respond to various types of chemotherapies were treated with the anti-programmed death 1 (anti-PD-1) antibody pembrolizumab at 100 mg every 3 weeks. After a median of four cycles of treatment (range 2–18), four out of seven patients responded (two complete response, two partial response, overall response rate 57%). Expression of PD1-ligand available was 50, 20, 30, 70, and 30% of five patients respectively. It is negative in one patient and not tested in one patient. Adverse events, which mostly ranged from grade I to grade III, were tolerable and could be safely handled, although immune-related pneumonitis was notable. Overall, PD-1 blockade with pembrolizumab represents a favorable strategy for the treatment of refractory/relapsed NKTCL.
Keywords: NK/T-cell lymphoma, PD-1 blockade, Pembrolizumab
Background
Immunotherapeutics, specifically immune checkpoint inhibitors of the PD-1 (programmed death 1)/PD-L1 (programmed death ligand 1) pathway, is an extremely active area of laboratory and clinical investigation [1] and has demonstrated utility as targets in advanced cancer, with evidence of both an overall survival benefit and durable responses [2, 3]. Many clinical trials of PD-1 blockade treatment in solid tumors and hematological tumors (including malignant lymphoma) have been conducted [4–6]. Pembrolizumab and Nivolumab have been approved for use in multiple types of cancer, including melanoma, non-small cell lung cancer, renal cell carcinoma and squamous cell carcinoma, which has led to unprecedented clinical progress [7–9].
The administration of immune checkpoint inhibitors in hematological tumors, especially classic Hodgkin lymphoma, has developed fast these years [10]. Classical HL proves to be a promising target for anti-PD-1 therapy because PD-L1 is overexpressed by Reed-Sternberg cells [11] and PD-1 blockade Nivolumab has been tested in many clinical trials and obtained favorable results [12, 13]. It was also evaluated in a cohort of patients with relapsed or refractory lymphoid malignancies, including 29 with B-NHL, 2 with PMBCL, and 23 with T-NHL. Four (36%) patients with DLBCL, four (40%) with FL, two (15%) with mycosis fungoides, and two (40%) with peripheral T cell lymphoma responded to the therapy, among whom one patient (9%) with DBLCL and one (10%) with FL achieved CR [14, 15]. In general, non-Hodgkin lymphomas (NHLs) do not share cHL’s vulnerability to PD-1 inhibitors, and the majority of NHLs appear to be minimally sensitive to PD-1 blockade [1].
NK/T cell lymphoma, which has a distinctive morphology, immunophenotype, and biological behavior, relapses frequently and progresses rapidly. However, there are few investigations into relapsed/refractory NK/T cell lymphoma and no standard treatments yet available. Only sporadic studies about PD-1/PD-L1 blockade treating NK/T cell lymphoma have been reported [16].
In our retrospective study, a total of seven patients with refractory/relapsed NKTCL were treated with pembrolizumab at our lymphoma diagnosis and treatment center. Herein, we report our findings of PD-1 blockade with pembrolizumab in these highly refractory NKTCL patients.
Patients and methods
Patients and treatment
A total of seven patients with refractory/relapsed NKTCL were treated with the anti-PD1 antibody pembrolizumab. All patients had received at least two prior chemotherapy regimens. Pembrolizumab at 100 mg was administered every 3 weeks in all patients. All patients were fully informed about the nature and possible toxicities of the treatment protocol and gave informed consent.
Response assessments and monitoring
A computed tomography (CT) scan with contrast and/or fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) were used to assess treatment responses according to the Revised Response Criteria for Malignant Lymphoma. Circulating EBV (Epstein Barr virus) DNA and lactate dehydrogenase (LDH) levels were measured. Adverse events (AEs) were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
Results
Patients
A total of seven patients with refractory/relapsed NKTCL were enrolled. All seven patients (median age: 47, range 17–61 years) had one to two of Eastern Cooperative Oncology Group performance status (ECOG PS). The median number of prior treatment regimens was four (range 3–10). The patient characteristics are shown in Table 1.
Table 1.
Patient characteristics
| Case | Sex | Age (years) | Bone marrow | Stage | PINK score | Sites | Prior treatment | |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 39 | Negative | IV | 2 | Nasal cavities, skin of upper and lower limbs, cervical, axillary and inguinal lymph nodes | DDP+VP16+IFO(2); pegaspargase+MTX+ examethasone (2); liposomal doxorubicin+gemcitabine+pegaspargase+dexamethasone(3) | |
| 2 | M | 31 | Negative | II | 3 | Mediastinal, hilar, para-aortic, mesenteric, right iliac vessels lymph nodes, intestinal, transverse colon and rectum | pegaspargase+MTX+dexamethasone(4); hydroxycamptothecin+paclitaxel+mitoxantrone+methylprednisolone(6); Auto-HSCT | |
| 3 | F | 61 | Negative | II | 4 | Left cervical, inguinal lymph nodes, left upper arm, right forearm, buttock, subcutaneous soft tissue of left lower leg, left lung upper lobe, and right lung middle lobe | CTX+VCR+adriamycin+prednisone(8); pegaspargase +DDP+gemcitabine+ dexamethasone(4) | |
| 4 | M | 53 | Negative | II | 1 | Sinus | DICE+L-Asp(4); CHOP+L-Asp(3) | |
| 5 | M | 61 | Negative | IV | 3 | Left posterior lateral wall of the oropharynx, left cervical lymph nodes, right lung, spleen, and adrenal gland | GDPT(6); DDGP(2) | |
| 6 | M | 47 | Negative | IIIEB | 3 | Parotid gland, oropharynx, nasopharynx, spleen, cervical, left supraclavicular, hilar, mediastinal, and inguinal lymph nodes | DICE+L-Asp(2); DICE+pegaspargase(2) | |
| 7 | F | 17 | Negative | IEB | 0 | Left nasal cavity, chest wall | VIPD(3); DDGP(4) |
The baseline characteristics of seven cases, including gender, age, organ involvement, and main previous treatment regimens
DDP, cisplatin; VP16, etoposide; IFO, ifosfamide; MTX, methotrexate; Auto-HSCT, autologous hematopoietic stem cell transplantation; CTX, cyclophosphamide; VCR, vincristine; DICE, dexamethasone, ifosfamide, cisplatin and etoposide; L-Asp, L-asparaginase; CHOP, cyclophosphamide, epirubicin, vincristine and prednisone; GDPT, gemcitabine, cisplatin, dexamethasone and thalidomide; DDGP, cisplatin, dexamethasone, gemcitabine and pegaspargase; VIPD, cisplatin, etoposide, ifosfamide and dexamethasone
Clinical outcomes
A median of four (range, 2–18) cycles of pembrolizumab was administered. The overall response rate (ORR) was 57.1% (95% confidence interval [CI], 18 to 90%), with a complete response (CR) occurring in two (28.6%) patients and a partial response (PR) observed in two (28.6%) patients. Response duration, PFS, and OS of seven patients are 4.1 months, 4.8 months, and 5.0 months respectively.
Case 1 had biopsy-confirmed extensive skin involvement. Pembrolizumab treatment led to rapid improvement of skin lesions, and PET/CT scans after 4 cycles showed a metabolic CR. The skin lesions in this patient’s lower limbs disappeared (Fig. 1) and were replaced by granulation tissue 5 cycles later. EBV DNA level was measured before treatment. At the time of this report, this patient has completed 18 cycles of pembrolizumab treatment.
Fig. 1.

Lesion changes of case 1 before and after pembrolizumab treatment. a The skin lesions of lower limbs of case 1 at the time of relapse. b The skin lesions responded after the first cycle. After 4 cycles, her crust of the lesions fell off and ulcers healed
The EBV DNA levels in case 2 (Fig. 2) fell from 1330 copies/ml to < 500 copies/ml after 5 cycles, and the LDH levels fell from 298 U/L to 147 U/L. A PET/CT scan showed a metabolic CR after 2 cycles (Fig. 3).
Fig. 2.
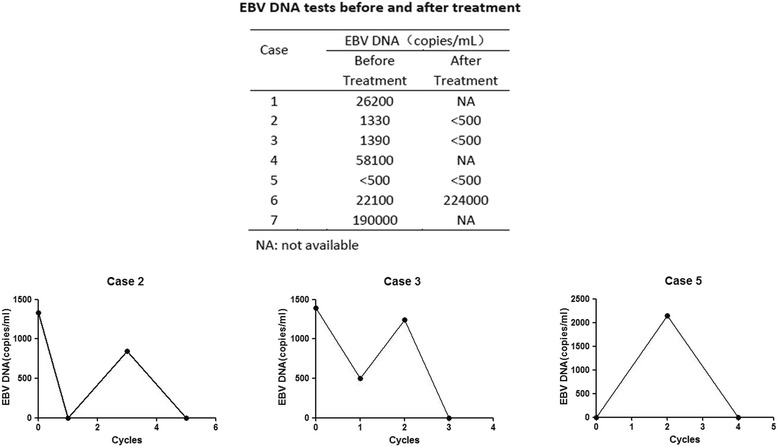
Changes in circulating EBV DNA with pembrolizumab treatment. The EBV DNA levels in case 2 fell from 1330 copies/ml to < 500 copies/ml after 5 cycles. The EBV DNA levels in case 3 fell from 1390 copies/ml to < 500 copies/ml after 3 cycles. The EBV DNA levels in case 5 rose from normality to 2140 copies/ml after 2 cycles and went back to normal 4 cycles later. The EBV DNA levels of case 6 rose from 22,100 copies/ml to 224,000 copies/ml after 3 cycles. The EBV DNA levels of case 7 rose gradually from 10,900 copies/ml to 190,000 copies/ml prior to pembrolizumab treatment
Fig. 3.
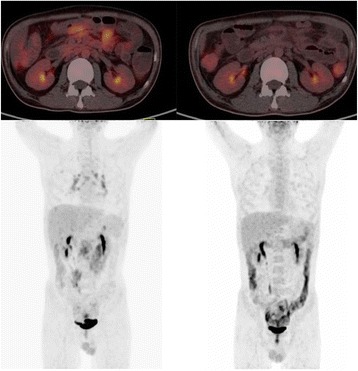
PET/CT results of case 2. The scan of case 2 in the left two images showed a relatively hypermetabolic lesion in mediastinal, hilar lymph nodes, and intestines after using pembrolizumab for 1 cycle. The two images on the right showed that the lesions were metabolically less active 2 cycles later
The EBV DNA levels in case 3 (Fig. 2) fell from 1390 copies/ml to < 500 copies/ml after 3 cycles. CT scans in cases 3 and 5 showed PR status.
Case 4 developed symptoms of dyspnea and low oxygen saturation. Consequently, pembrolizumab was discontinued. The EBV DNA levels in case 5 (Fig. 2) rose from normality to 2140 copies/ml after 2 cycles and went back to normal 4 cycles later. The EBV DNA levels of case 6 (Fig. 2) rose from 22,100 copies/ml to 224,000 copies/ml after 3 cycles, and this patient ultimately developed hemophagocytic syndrome (HPS). The symptoms of case 6 did not abate after the application of anti-HPS therapy, and the patient died of progressive disease (PD). The EBV DNA levels of case 7 (Fig. 2) rose gradually from 10,900 copies/ml to 190,000 copies/ml prior to pembrolizumab treatment.
PD-L1 expression on lymphoma cells
PD-L1 expression was measured by immunochemistry on formalin-fixed, paraffin-embedded tissue sections (Fig. 4). The expression percentage of PD-L1 expressed on lymphoma cells of case 1, case 3, case 5, case 6, and case 7 is 50, 20, 30, 70, and 30% respectively (Table 2). PD-L1 expression data were not available for case 2. We haven’t observed direct connection between PD-L1 expression and clinical response.
Fig. 4.
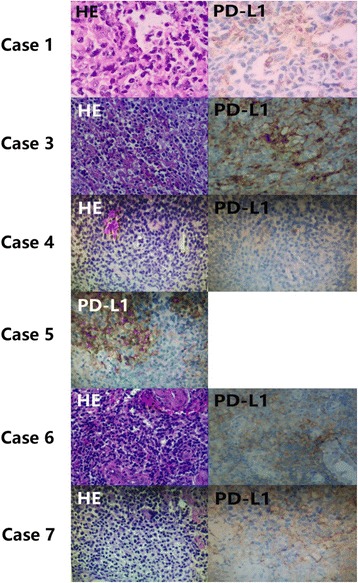
HE staining and IHC of six patients available. The scan of case 2 in the left two images showed a relatively hypermetabolic lesion in mediastinal, hilar lymph nodes, and intestines after using pembrolizumab for 1 cycle. The two images on the right showed that the lesions were metabolically less active 2 cycles later
Table 2.
The expression of PD-L1, CD3, CD4, CD8, and EBER
| Case | PD-L1 | CD3 | CD4 | CD8 | EBER |
|---|---|---|---|---|---|
| 1 | 50% | + | NA | NA | + |
| 2 | NA | + | − | + | + |
| 3 | 20%+ | + | NA | NA | + |
| 4 | − | + | NA | NA | NA |
| 5 | 30%+ | + | + | NA | + |
| 6 | 70%+ | NA | + | + | + |
| 7 | 30%+ | + | NA | NA | + |
The expression of PD-L1, CD3, CD4, CD8, and EBER on lymphoma cells. PD-L1: It is not available for case 2 and negative for case 4. The expression ratio of the other five cases is 50, 20, 30, 70, and 30% respectively. Most cases have positive CD3 expression except case 6. EBER is not available for case 4 and the remaining six cases are positive. More than half of the cases didn’t receive CD4 and CD8 tests
NA, not available
Adverse events
Treatment-related AEs of any grade occurred in 71.4% of patients. The main AEs were pneumonitis and laboratory abnormalities. Cases 2 and 6 suffered from diarrhea. Case 3 experienced a fever. Case 4 developed grade 3 thrombocytopenia. The patient was treated with thrombocyte transfusion and recombinant human thrombopoietin, and the thrombocyte count climbed to normality. Cases 4 and 7 presented with grade 3 pneumonitis. Both of them suffered from respiratory failure and did not respond well to corticosteroid and advanced respiratory support treatment. The other patients experienced no treatment-related AEs (Table 3).
Table 3.
Adverse events possibly related to pembrolizumab
| Event | Grade 1 | Grade 2 | Grade 3 | Total n = 7(%) |
|---|---|---|---|---|
| Pneumonitis | 0 | 0 | 2 | 2 (28.6%) |
| Diarrhea | 1 | 0 | 0 | 1 (14.3%) |
| Pyrexia | 1 | 0 | 0 | 1 (14.3%) |
| Anemia | 1 | 1 | 0 | 2 (28. 6%) |
| Neutropenia | 1 | 1 | 0 | 2 (28. 6%) |
| Thrombocytopenia | 1 | 0 | 1 | 2 (28. 6%) |
| Increased ALT | 0 | 1 | 0 | 1 (14.3%) |
| Increased AST | 2 | 0 | 0 | 2 (28. 6%) |
Adverse events we encountered during the course of pembrolizumab treatment. Most adverse reactions belong to grade I to grade II. Two cases suffered from pneumonitis and one case developed thrombocytopenia
ALT, alanine aminotransferase; AST, aspartate aminotransferase
Discussion
NK/T-cell lymphoma (NKTCL) is a subtype of non-Hodgkin lymphoma that is more prevalent in China than in Western countries [17, 18]. Moreover, traditional treatments offer especially poor efficacy and prognoses [19, 20]. Studies have shown that NKTCL cells play an important role in the activation and tolerance of T cells, as these cells can avoid immune surveillance and the consequent killing of NKTCL, resulting in a poor prognosis.
The consensus on standard treatment for NK/T cell lymphoma has not been reached until now. Current data indicate that advanced-stage and relapsed/refractory NK/T-cell lymphoma should be treated with L-asparaginase-containing regimens that incorporate non-MDR-dependent drugs [17, 21–23]. Additionally, HSCT has been explored in NK/T-cell lymphoma [24, 25]. Treatment options, especially targeted drugs for patients with relapsed/refractory NKTCL are limited. A retrospective study has shown that the estimated 5-year OS of 47 patients undergoing autologous HSCT was 56% [26]. In another retrospective analysis, three patients with NK/T-cell lymphoma undergoing allogeneic HSCT were studied, and the 3-year OS and PFS were 55 and 53% [27]. Continued efforts should be made to improve chemotherapeutic regimens and other targeted drugs.
Few studies have been conducted to explore the application of PD-1 blockade in the treatment of NKTCL. Therefore, large-scale clinical trials on pembrolizumab remain to be conducted to assess and confirm the treatment outcomes in NKTCL. The B7 family co-stimulatory molecule PD-L1 plays a key role in the activation and tolerance of T cells [28, 29]. PD-L1 interacts with its receptor, PD-1, and transmits a negative regulatory signal that induces tumor antigen-specific T-cell apoptosis and immune dysfunction and promotes immune escape of lymphoma cells [30, 31].
Programmed death receptor 1 (PD-1) is an inhibitory receptor expressed on the surface of activated T cells and is normally involved in immune tolerance and the prevention of tissue damage associated with chronic inflammation. Interactions of PD-1 with its ligands, PD-L1 and PD-L2, inhibit T-cell receptor signaling by downregulating T-cell activation and proliferation and blunting T-cell-mediated anti-tumor immune responses [32, 33]. Thus, the PD-1 pathway represents an immune checkpoint that acts to suppress anti-tumor immunity. Studies have shown that T-cell function and anti-tumor responses can be enhanced by anti-PD-1 and anti-PD-L1 antibodies in mouse models of various types of tumors [34–39].
In our study, the expression ratio of PD-L1 expressed on lymphoma cells of case 1, case 3, case 5, case 6, and case 7 is 50, 20, 30, 70, and 30% respectively. In case 4, there was no detected PD-L1 expression, and data were not available for one patient (case 2). We found that cases 1 and 3 achieved a CR and PR, respectively; case 5 achieved a PR. However, two patients (cases 6 and 7) had disease progression. We did not find out a direct relation between the expression of PD1-ligand and clinical response. Due to availability of the drug and financial limitations, our cases received lower dosages of pembrolizumab, which could have accounted for the difference in response rate. Additional factors may affect the responses to PD-1 blockade. One study found that PD-L1 expression was positively correlated with EBV-driven LMP1 (latent membrane protein 1) expression at both the protein and mRNA levels in NKTCL and NK cells [40]. Among three patients mentioned in another study, EBV DNA copy numbers were downregulated after pembrolizumab treatment, which might indicate that EBV infection acts as a possible mechanism for inducing PD-L1 expression [41]. Considering the relationship between PD-L1 expression and EBV activity [42], PD-1 blockade may play a significant part in restoring immunologic function and reducing EBV copy numbers. In addition, EBV copy numbers may serve as a predictive indicator of both the treatment outcome and prognosis of NKTCL. In this study, patients (cases 6 and 7) with higher post-treatment EBV level had worse response than that in patients with lower post-treatment EBV level. The study of Kwong et al. showed that in all clinical subtypes of NK cell lymphomas, EBV DNA was an important prognostic element for disease-free survival (DFS) and overall survival (OS) [43, 44].
One of the seven patients in the study developed mild pyrexia. Cytokine release and nonspecific activation of an immune response is postulated to account for the development of fever [45]. Hepatic AEs occurring after treatment with immune checkpoint inhibitors are mainly characterized by asymptomatic elevations in aspartate aminotransferase and alanine aminotransferase level [46]. In some large-scale clinical trials of anti-PD1 antibodies, the occurrence rate of hepatitis was under 5%, and grade 3 or 4 toxicity was rarely observed [47, 48]. Pneumonitis is generally defined as inflammation of the pulmonary parenchyma. In our study, both cases 4 and 7 suffered from serious pneumonitis. Accordingly, it is critical to initiate treatment of pneumonitis as soon as possible. In terms of treatment, corticosteroids remain fundamental for treating immune-related adverse events (irAEs) [49]. Case 2 experienced diarrhea, and considering that this patient was diagnosed with enteropathy-associated T-cell lymphoma, his symptoms were not solely derived from PD-1-related colitis. PD1/PD-L1 blockade therapies have been associated with a lower risk of hematologic toxicities [49]. Furthermore, cases 4 and 6 had previously been treated with various types of chemotherapies. Thus, we assumed that the hematologic toxicities of these two patients were primarily consequences of their prior chemotherapies. As immunotherapies become more common in the clinical management of patients with many different types of cancer, it is essential to understand irAEs. Moreover, tumor neoantigens and normal tissue antigens can be cross-reactive, leading to irAE generation during immunotherapy [50, 51]. Cytopenia is rarely associated with immune checkpoint blockade in patients with solid tumors but appears to occur more frequently in patients with lymphoma [52]. For cases 4 and 6, the unexplained elevation of serum levels of hepatic alanine aminotransferase and aspartate aminotransferase enzymes suggested the presence of immune-related hepatitis. In general, the majority of AEs related to pembrolizumab treatment were mild and controllable, mostly grade 1 or 2 in our study, demonstrating that pembrolizumab can be safely administered to patients with NKTCL.
Conclusions
This retrospective study of seven patients with refractory NKTCL shows that pembrolizumab administered at doses of 100 mg every 3 weeks were effective. The relationship between PD-L1 expression and response to PD-1 blockade is inconclusive in this analysis because of small sample size. Further studies are warranted to evaluate and confirm the activity of PD-1 blockade in patients with NKTCL.
Acknowledgements
We are indebted to the Lymphoma Diagnosis and Treatment Cancer Center of Henan Province for providing technical assistance. We also thank all the patients for allowing us to analyze their data.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81172118).
Availability of data and materials
The material supporting the conclusion of this study has been included within the article.
Abbreviations
- Anti-PD-1
Anti-programmed death 1
- CI
Confidence interval
- CR
Complete response
- CT
Computed tomography
- DFS
Disease-free survival
- EBV
Epstein Barr virus
- FDG
Fluorodeoxyglucose
- irAEs
Immune-related adverse events
- LDH
Lactate dehydrogenase
- LMP1
Latent membrane protein 1
- MAPK
Mitogen-activated protein kinase
- ORR
Overall response rate
- OS
Overall survival
- PD-L1
Programmed death ligand 1
- PET/CT
Positron emission tomography/computed tomography
- PR
Partial response
Authors’ contributions
XL, JQY, LL, XRF, XDZ, YC, ZCS, HY, LZ, XHW, JJW, ZML, FFN, LT, and WCL provided the clinical data. YSC collected the data and wrote the manuscript. Both XL and YSC interpreted the data. XL and MZZ revised the manuscript. MZZ and KHY conceived the concept of this study. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Zhengzhou University First Affiliated Hospital. All patients provided informed consent.
Consent for publication
Written informed consent for publication was obtained.
Competing interests
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xin Li, Email: lixiaoxin86@126.com.
Yasong Cheng, Email: ycyouman@163.com.
Mingzhi Zhang, Phone: +8613838565629, Email: mingzhi_zhang1@126.com.
Jiaqin Yan, Email: 13838273309@163.com.
Ling Li, Email: lingl510@126.com.
Xiaorui Fu, Email: zymfxr_2006@126.com.
Xudong Zhang, Email: feverxxd@126.com.
Yu Chang, Email: changyufly@126.com.
Zhenchang Sun, Email: suny006@163.com.
Hui Yu, Email: Yuhui@zzu.edu.cn.
Lei Zhang, Email: zl2909@163.com.
Xinhua Wang, Email: 15036115299@163.com.
Jingjing Wu, Email: wjjing1205@163.com.
Zhaoming Li, Email: zhaomingli2013@163.com.
Feifei Nan, Email: nanfeifei2008@126.com.
Li Tian, Email: qisile123654@163.com.
Wencai Li, Email: liwencaipatho@yahoo.com.
Ken H. Young, Email: khyoung@mdanderson.org
References
- 1.Merryman RW, Armand P, Wright KT, Rodig SJ. Checkpoint blockade in Hodgkin and non-Hodgkin lymphoma. Blood Adv. 2017;1(26):2643–2654. doi: 10.1182/bloodadvances.2017012534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robert C, Thomas L, Bondarenko I, O'Day S, Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, Davidson N, Richards J, Maio M, Hauschild A, Miller WH, Jr, Gascon P, Lotem M, Harmankaya K, Ibrahim R, Francis S, Chen TT, Humphrey R, Hoos A, Wolchok JD. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 4.Hude I, Sasse S, Engert A, Brockelmann PJ. The emerging role of immune checkpoint inhibition in malignant lymphoma. Haematologica. 2017;102(1):30–42. doi: 10.3324/haematol.2016.150656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Im A, Pavletic SZ. Immunotherapy in hematologic malignancies: past, present, and future. J Hematol Oncol. 2017;10(1):94. doi: 10.1186/s13045-017-0453-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ok CY, Young KH. Checkpoint inhibitors in hematological malignancies. J Hematol Oncol. 2017;10(1):103. doi: 10.1186/s13045-017-0474-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu B, Song Y, Liu D. Recent development in clinical applications of PD-1 and PD-L1 antibodies for cancer immunotherapy. J Hematol Oncol. 2017;10(1):174. doi: 10.1186/s13045-017-0541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strome SE, Dong H, Tamura H, Voss SG, Flies DB, Tamada K, Salomao D, Cheville J, Hirano F, Lin W, Kasperbauer JL, Ballman KV, Chen L. B7-H1 blockade augments adoptive T-cell immunotherapy for squamous cell carcinoma. Cancer Res. 2003;63(19):6501–6505. [PubMed] [Google Scholar]
- 11.Green MR, Monti S, Rodig SJ, Juszczynski P, Currie T, O'Donnell E, Chapuy B, Takeyama K, Neuberg D, Golub TR, Kutok JL, Shipp MA. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116(17):3268–3277. doi: 10.1182/blood-2010-05-282780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry D, Freeman GJ, Rodig SJ, Chapuy B, Ligon AH, Zhu L, Grosso JF, Kim SY, Timmerman JM, Shipp MA, Armand P. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med. 2015;372(4):311–319. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ansell SM. Nivolumab in the treatment of Hodgkin lymphoma. Clin Cancer Res. 2017;23(7):1623–1626. doi: 10.1158/1078-0432.CCR-16-1387. [DOI] [PubMed] [Google Scholar]
- 14.Lesokhin AM, Ansell SM, Armand P, Scott EC, Halwani A, Gutierrez M, Millenson MM, Cohen AD, Schuster SJ, Lebovic D, Dhodapkar M, Avigan D, Chapuy B, Ligon AH, Freeman GJ, Rodig SJ, Cattry D, Zhu L, Grosso JF, Bradley Garelik MB, Shipp MA, Borrello I, Timmerman J. Nivolumab in patients with relapsed or refractory hematologic malignancy: preliminary results of a phase Ib study. J Clin Oncol. 2016;34(23):2698–2704. doi: 10.1200/JCO.2015.65.9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xia Y, Jeffrey Medeiros L, Young KH. Signaling pathway and dysregulation of PD1 and its ligands in lymphoid malignancies. Biochim Biophys Acta. 2016;1865(1):58–71. doi: 10.1016/j.bbcan.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwong YL, Chan TSY, Tan D, Kim SJ, Poon LM, Mow B, Khong PL, Loong F, Au-Yeung R, Iqbal J, Phipps C, Tse E. PD1 blockade with pembrolizumab is highly effective in relapsed or refractory NK/T-cell lymphoma failing l-asparaginase. Blood. 2017;129(17):2437–2442. doi: 10.1182/blood-2016-12-756841. [DOI] [PubMed] [Google Scholar]
- 17.Tse E, Kwong YL. How I treat NK/T-cell lymphomas. Blood. 2013;121(25):4997–5005. doi: 10.1182/blood-2013-01-453233. [DOI] [PubMed] [Google Scholar]
- 18.Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee JH, Lee DH, Huh J, Oh SY, Kwon HC, Kim HJ, Lee SI, Kim JH, Park J, Oh SJ, Kim K, Jung C, Park K, Kim WS. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006;24(4):612–618. doi: 10.1200/JCO.2005.04.1384. [DOI] [PubMed] [Google Scholar]
- 19.Kwong YL, Anderson BO, Advani R, Kim WS, Levine AM, Lim ST. Management of T-cell and natural-killer-cell neoplasms in Asia: consensus statement from the Asian Oncology Summit 2009. Lancet Oncol. 2009;10(11):1093–1101. doi: 10.1016/S1470-2045(09)70265-7. [DOI] [PubMed] [Google Scholar]
- 20.Li X, Cui Y, Sun Z, Zhang L, Li L, Wang X, Wu J, Fu X, Ma W, Zhang X, Chang Y, Nan F, Li W, Su L, Wang J, Xue H, Zhang M. DDGP versus SMILE in newly diagnosed advanced natural killer/T-cell lymphoma: a randomized controlled, multicenter, open-label study in China. Clin Cancer Res. 2016;22(21):5223–5228. doi: 10.1158/1078-0432.CCR-16-0153. [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi M, Kwong YL, Kim WS, Maeda Y, Hashimoto C, Suh C, Izutsu K, Ishida F, Isobe Y, Sueoka E, Suzumiya J, Kodama T, Kimura H, Hyo R, Nakamura S, Oshimi K, Suzuki R. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-cell tumor study group study. J Clin Oncol. 2011;29(33):4410–4416. doi: 10.1200/JCO.2011.35.6287. [DOI] [PubMed] [Google Scholar]
- 22.Kwong YL, Kim WS, Lim ST, Kim SJ, Tang T, Tse E, Leung AY, Chim CS. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood. 2012;120(15):2973–2980. doi: 10.1182/blood-2012-05-431460. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Y, Xu W, Liu H, Li J. Therapeutic options in peripheral T cell lymphoma. J Hematol Oncol. 2016;9:37. doi: 10.1186/s13045-016-0267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwong YL. Hematopoietic stem cell transplantation in natural killer cell lymphoma and leukemia. Int J Hematol. 2010;92(5):702–707. doi: 10.1007/s12185-010-0724-4. [DOI] [PubMed] [Google Scholar]
- 25.Kwong YL. High-dose chemotherapy and hematopoietic SCT in the management of natural killer-cell malignancies. Bone Marrow Transplant. 2009;44(11):709–714. doi: 10.1038/bmt.2009.239. [DOI] [PubMed] [Google Scholar]
- 26.Lee J, Au WY, Park MJ, Suzumiya J, Nakamura S, Kameoka J, Sakai C, Oshimi K, Kwong YL, Liang R, Yiu H, Wong KH, Cheng HC, Ryoo BY, Suh C, Ko YH, Kim K, Lee JW, Kim WS, Suzuki R. Autologous hematopoietic stem cell transplantation in extranodal natural killer/T cell lymphoma: a multinational, multicenter, matched controlled study. Biol Blood Marrow Transplant. 2008;14(12):1356–1364. doi: 10.1016/j.bbmt.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 27.Murashige N, Kami M, Kishi Y, Kim SW, Takeuchi M, Matsue K, Kanda Y, Hirokawa M, Kawabata Y, Matsumura T, Kusumi E, Hirabayashi N, Nagafuji K, Suzuki R, Takeuchi K, Oshimi K. Allogeneic haematopoietic stem cell transplantation as a promising treatment for natural killer-cell neoplasms. Br J Haematol. 2005;130(4):561–567. doi: 10.1111/j.1365-2141.2005.05651.x. [DOI] [PubMed] [Google Scholar]
- 28.Ma W, Gilligan BM, Yuan J, Li T. Current status and perspectives in translational biomarker research for PD-1/PD-L1 immune checkpoint blockade therapy. J Hematol Oncol. 2016;9(1):47. doi: 10.1186/s13045-016-0277-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang J, Yuan R, Song W, Sun J, Liu D, Li Z. PD-1, PD-L1 (B7-H1) and tumor-site immune modulation therapy: the historical perspective. J Hematol Oncol. 2017;10(1):34. doi: 10.1186/s13045-017-0403-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han L, Liu F, Li R, Li Z, Chen X, Zhou Z, Zhang X, Hu T, Zhang Y, Young K, Sun S, Wen J, Zhang M. Role of programmed death ligands in effective T-cell interactions in extranodal natural killer/T-cell lymphoma. Oncol Lett. 2014;8(4):1461–1469. doi: 10.3892/ol.2014.2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Atanackovic D, Luetkens T, Kroger N. Coinhibitory molecule PD-1 as a potential target for the immunotherapy of multiple myeloma. Leukemia. 2014;28(5):993–1000. doi: 10.1038/leu.2013.310. [DOI] [PubMed] [Google Scholar]
- 32.Latchman Y, Wood CR, Chernova T, Chaudhary D, Borde M, Chernova I, Iwai Y, Long AJ, Brown JA, Nunes R, Greenfield EA, Bourque K, Boussiotis VA, Carter LL, Carreno BM, Malenkovich N, Nishimura H, Okazaki T, Honjo T, Sharpe AH, Freeman GJ. PD-L2 is a second ligand for PD-1 and inhibits T cell activation. Nat Immunol. 2001;2(3):261–268. doi: 10.1038/85330. [DOI] [PubMed] [Google Scholar]
- 33.Liu D, Wang S, Bindeman W. Clinical applications of PD-L1 bioassays for cancer immunotherapy. J Hematol Oncol. 2017;10(1):110. doi: 10.1186/s13045-017-0479-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L, Carcereny E, Ahn MJ, Felip E, Lee JS, Hellmann MD, Hamid O, Goldman JW, Soria JC, Dolled-Filhart M, Rutledge RZ, Zhang J, Lunceford JK, Rangwala R, Lubiniecki GM, Roach C, Emancipator K, Gandhi L. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 35.Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, Majem M, Fidler MJ, de Castro G, Jr, Garrido M, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet (London, England) 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 36.Muro K, Chung HC, Shankaran V, Geva R, Catenacci D, Gupta S, Eder JP, Golan T, Le DT, Burtness B, McRee AJ, Lin CC, Pathiraja K, Lunceford J, Emancipator K, Juco J, Koshiji M, Bang YJ. Pembrolizumab for patients with PD-L1-positive advanced gastric cancer (KEYNOTE-012): a multicentre, open-label, phase 1b trial. Lancet Oncol. 2016;17(6):717–726. doi: 10.1016/S1470-2045(16)00175-3. [DOI] [PubMed] [Google Scholar]
- 37.Nghiem PT, Bhatia S, Lipson EJ, Kudchadkar RR, Miller NJ, Annamalai L, Berry S, Chartash EK, Daud A, Fling SP, Friedlander PA, Kluger HM, Kohrt HE, Lundgren L, Margolin K, Mitchell A, Olencki T, Pardoll DM, Reddy SA, Shantha EM, Sharfman WH, Sharon E, Shemanski LR, Shinohara MM, Sunshine JC, Taube JM, Thompson JA, Townson SM, Yearley JH, Topalian SL, et al. PD-1 blockade with pembrolizumab in advanced Merkel-cell carcinoma. N Engl J Med. 2016;374(26):2542–2552. doi: 10.1056/NEJMoa1603702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, Gottfried M, Peled N, Tafreshi A, Cuffe S, O'Brien M, Rao S, Hotta K, Leiby MA, Lubiniecki GM, Shentu Y, Rangwala R, Brahmer JR. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–1833. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 39.Schachter J, Ribas A, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, Larkin J, Lorigan P, Neyns B, Blank C, Petrella TM, Hamid O, Zhou H, Ebbinghaus S, Ibrahim N, Robert C. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006) Lancet (London, England) 2017;390(10105):1853–1862. doi: 10.1016/S0140-6736(17)31601-X. [DOI] [PubMed] [Google Scholar]
- 40.Bi XW, Wang H, Zhang WW, Wang JH, Liu WJ, Xia ZJ, Huang HQ, Jiang WQ, Zhang YJ, Wang L. PD-L1 is upregulated by EBV-driven LMP1 through NF-kappaB pathway and correlates with poor prognosis in natural killer/T-cell lymphoma. J Hematol Oncol. 2016;9(1):109. doi: 10.1186/s13045-016-0341-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Green MR, Rodig S, Juszczynski P, Ouyang J, Sinha P, O'Donnell E, Neuberg D, Shipp MA. Constitutive AP-1 activity and EBV infection induce PD-L1 in Hodgkin lymphomas and posttransplant lymphoproliferative disorders: implications for targeted therapy. Clin Cancer Res. 2012;18(6):1611–1618. doi: 10.1158/1078-0432.CCR-11-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tse E, Kwong YL. The diagnosis and management of NK/T-cell lymphomas. J Hematol Oncol. 2017;10(1):85. doi: 10.1186/s13045-017-0452-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Au WY, Pang A, Choy C, Chim CS, Kwong YL. Quantification of circulating Epstein-Barr virus (EBV) DNA in the diagnosis and monitoring of natural killer cell and EBV-positive lymphomas in immunocompetent patients. Blood. 2004;104(1):243–249. doi: 10.1182/blood-2003-12-4197. [DOI] [PubMed] [Google Scholar]
- 44.Park S, Lee J, Ko YH, Han A, Jun HJ, Lee SC, Hwang IG, Park YH, Ahn JS, Jung CW, Kim K, Ahn YC, Kang WK, Park K, Kim WS. The impact of Epstein-Barr virus status on clinical outcome in diffuse large B-cell lymphoma. Blood. 2007;110(3):972–978. doi: 10.1182/blood-2007-01-067769. [DOI] [PubMed] [Google Scholar]
- 45.Schwartz RN, Stover L, Dutcher J. Managing toxicities of high-dose interleukin-2. Oncology (Williston Park) 2002;16(11 Suppl 13):11–20. [PubMed] [Google Scholar]
- 46.Naidoo J, Page DB, Li BT, Connell LC, Schindler K, Lacouture ME, Postow MA, Wolchok JD. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol. 2015;26(12):2375–2391. doi: 10.1093/annonc/mdv383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C, Kalinka-Warzocha E, Savage KJ, Hernberg MM, Lebbe C, Charles J, Mihalcioiu C, Chiarion-Sileni V, Mauch C, Cognetti F, Arance A, Schmidt H, Schadendorf D, Gogas H, Lundgren-Eriksson L, Horak C, Sharkey B, Waxman IM, Atkinson V, Ascierto PA. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372(4):320–330. doi: 10.1056/NEJMoa1412082. [DOI] [PubMed] [Google Scholar]
- 48.Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, Dronca R, Gangadhar TC, Patnaik A, Zarour H, Joshua AM, Gergich K, Elassaiss-Schaap J, Algazi A, Mateus C, Boasberg P, Tumeh PC, Chmielowski B, Ebbinghaus SW, Li XN, Kang SP, Ribas A. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Champiat S, Lambotte O, Barreau E, Belkhir R, Berdelou A, Carbonnel F, Cauquil C, Chanson P, Collins M, Durrbach A, Ederhy S, Feuillet S, Francois H, Lazarovici J, Le Pavec J, De Martin E, Mateus C, Michot JM, Samuel D, Soria JC, Robert C, Eggermont A, Marabelle A. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol. 2016;27(4):559–574. doi: 10.1093/annonc/mdv623. [DOI] [PubMed] [Google Scholar]
- 50.Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, Walsh LA, Postow MA, Wong P, Ho TS, Hollmann TJ, Bruggeman C, Kannan K, Li Y, Elipenahli C, Liu C, Harbison CT, Wang L, Ribas A, Wolchok JD, Chan TA. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014;371(23):2189–2199. doi: 10.1056/NEJMoa1406498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Powles T, Eder JP, Fine GD, Braiteh FS, Loriot Y, Cruz C, Bellmunt J, Burris HA, Petrylak DP, Teng SL, Shen X, Boyd Z, Hegde PS, Chen DS, Vogelzang NJ. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature. 2014;515(7528):558–562. doi: 10.1038/nature13904. [DOI] [PubMed] [Google Scholar]
- 52.Gordon IO, Wade T, Chin K, Dickstein J, Gajewski TF. Immune-mediated red cell aplasia after anti-CTLA-4 immunotherapy for metastatic melanoma. Cancer Immunol Immunother. 2009;58(8):1351–1353. doi: 10.1007/s00262-008-0627-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The material supporting the conclusion of this study has been included within the article.


