Abstract
CONTEXT:
Digital retinal imaging with the application of telemedicine technology shows promising results for screening of diabetic retinopathy in the primary care setting without requiring an ophthalmologist on site.
AIMS:
We assessed whether the establishment of telemedicine technology was an effective and efficient way to increase completion of annual eye examinations among underserved, low-income (Medicaid) diabetic patients.
SETTINGS AND DESIGN:
A cross-sectional study in a primary care setting.
SUBJECTS AND METHODS:
Health care claims data were collected before the establishment of telemedicine technology in 2010 and after its implementation in 2012 for Medicaid patients at East Baltimore Medical Center (EBMC), an urban health center that is part of Johns Hopkins Health System.
STATISTICAL ANALYSIS USED:
The primary outcome measure was the compliance rate of patients with diabetic eye examinations; calculated as the number of diabetic patients with a completed telemedicine eye examination, divided by the total number of diabetic patients.
RESULTS:
In 2010, EBMC treated 213 Medicaid diabetic patients and in 2012 treated 228 Medicaid patients. In 2010, 47.89% of patients completed their annual diabetic eye examination while in 2012 it was 78.07% (P < 0.001). After adjustment for age, gender, HgBA1C, disease severity, using resource utilization band score as a proxy, and medication possession ratio; telemedicine technology significantly increased the compliance (odds ratio: 4.98, P < 0.001).
CONCLUSIONS:
Adherence to annual eye examinations is low in the studied Medicaid diabetic population. Telemedicine technology in a primary care setting can increase compliance with annual eye examinations.
Keywords: Diabetic eye examination, Medicaid patients, telemedicine technology
Introduction
There are approximately 93 million people with diabetic retinopathy (DR) around the world.[1] DR is known as a leading cause of new-onset blindness in the high income, industrialized countries and an increasing cause in many middle-income countries.[2]
While about 98% of diabetic patients visit their primary care physician or endocrinologist at least once a year, the number is much lower for ophthalmology visits.[3] About 30% of diabetic patients with a high risk of vision loss never receive an eye examination and <40% ever receive treatment.[4,5]
Digital retinal imaging with the application of telemedicine technology shows promising results for screening and detection of DR in the primary care setting without requiring an ophthalmologist or retina specialist on site.[6,7,8,9,10] East Baltimore Medical Center (EBMC) is a primary care clinic, serving an underserved urban population in East Baltimore. Located close to Johns Hopkins Hospital, EBMC is considered the main outpatient health-care facility for a large number of underserved, low-income (Medicaid) patients in East Baltimore. In 2011 EBMC started a program to improve the completion rate for annual diabetic eye examination by application of telemedicine technology. The center implemented a nonmydriatic fundoscopic camera that would capture retinal images to be read off-site. In this report, we intend to assess whether the establishment of telemedicine technology was an effective and efficient way to increase the completion of annual diabetic eye examinations among Medicaid patients at EBMC and what the barriers to obtaining the eye examinations were. We also assessed the referral rate to ophthalmology office for those patients with positive findings in their primary image.
Subjects and Methods
Study design and setting
This cross-sectional study tested telemedicine technology in improving the completion rate for annual diabetic eye examinations among the Medicaid population at EBMC. We chose the Medicaid population because health-care claims data for all EBMC Medicaid patients were accessible through Johns Hopkins HealthCare LLC (JHHC), an entity of the Johns Hopkins Health System that administers the Medicaid Managed Care Organization.
Telemedicine technology
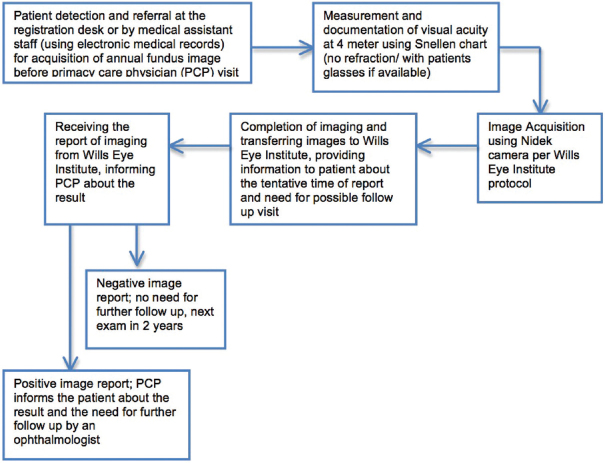
A Nidek camera retina imaging implemented in 2011 made it possible for the clinic to take retinal images of eligible diabetic patients during the time of their primary care visit without the necessity for pupil dilation. Clinic staff, a trained technician, acquired the images of both eyes of a patient while they were waiting to be seen by their primary care physicians, or after their visit before departure. The image acquisition was performed once for each patient. The images were sent to Wills Eye Institute in Philadelphia, Pennsylvania using image transfer software. Retina specialists at Wills Eye Institute reviewed transferred images and the results were sent back to EBMC within 1–2 business days. Primary care physicians would inform patients about the results of their scan by phone. Those with any sign of DR in their scan were advised to see an ophthalmologist for a full dilated eye examination and treatment as needed. The DR grading was done using the National Health Service's DR grading classification system.[11] Those with normal retina were advised to follow-up with another retina image in 2 years unless any new symptoms were detected. Figure 1 presents the process of image acquisition and communication with Wills Eye Institute as well as communication with patients about the result of their examination.
Figure 1.
Annual diabetic eye examination and referral process at East Baltimore Medical Center
Data collection
We collected health care claims data in January to December 2010 (before the establishment of the diabetic eye examination program) and January to December 2012 (after the establishment of the program) from the JHHC claims database. The study and data accumulation were carried out with approval from the Johns Hopkins Institutional Review Board. The study was conducted in accordance with HIPAA (Health Insurance Portability and Accountability Act of 1996; the United States legislation that provides data privacy and security provisions for safeguarding medical information) regulations. The data were released by JHHC for research only after the JHHC Data Sharing for Research Review Committee had approved the release.
To define diabetes, we applied the Healthcare Effectiveness Data and Information Set (HEDIS) codes defined by the National Committee for Quality Assurance,[12] HEDIS defined diabetic patients as patients aged 18–75 years of age with a diagnosis of diabetes type 1 or type 2. The patients required to be continuously enrolled in Medicaid with no more than one gap of up to 45 days during the measurement year. Medicaid verified enrolment monthly and used pharmacy data and claim/encounter data to identify members, but members were only required to be in one database for inclusion.[13] Completion of annual diabetic eye examination was defined as having one gradable image during the annual diabetes visit, reviewed and graded by retina specialists at Wills Eye Institute. If the patient required more than one visit for management of their disease the image acquisition would not be repeated in 1 year.
We collected data on several characteristics which could potentially affect compliance with the annual diabetic eye examination among Medicaid diabetic patients. These included age, gender, compliance with recommended glycated hemoglobin (HbA1C) measurements, financial incentive offered to the primary care system for completion of eye examinations, financial incentives offered to patients who completed a diabetic eye examination, medication possession ratio (MPR) which measured the percentage of time a patient had access to medication, and resource utilization band (RUB) score. RUB score was defined as a ranking system of overall morbidity level. It would group together the individuals who were expected to use the same level of resources. The scoring system was defined by the Johns Hopkins Adjusted Clinical Group Mix System (the ACG System[14]). The ACG System as a predictor of health care utilization has been validated in multiple settings.[15,16] The RUB values are: 0 – No or Only Invalid Diagnosis, 1 – Healthy Users, 2 – Low, 3 – Moderate, 4 – High, and 5 – Very High Users.
To calculate the referral rate to an ophthalmologist among those with positive finding of DR we reviewed the results of the Nidek screenings and those with any sign of DR were extracted. We used reports provided by retina specialists at Wills Eye Institute, using the National Health Service's DR grading classification system to identify those with any signs of DR.[11] The health care claims data for any ophthalmology visit in the patient population were collected from JHHC, and the referral rate to ophthalmology was calculated.
Primary and secondary variables and hypothesis
The primary outcome measure was efficacy of the diabetic eye examination program, calculated as the number of patients with completed annual diabetic eye examination during the study years, divided by the total number of diabetic patients seen during the study years, based on HEDIS codes. The secondary outcome measure was the referral rate among those with signs of DR in their study. We assessed factors playing a role in noncompliance for annual diabetic eye examination as the secondary outcome. We hypothesized that use of the telemedicine technology increases the rate of annual diabetic eye examination among Medicaid population.
Statistical analysis
We performed descriptive and univariate analysis to assess the completion rate of diabetic eye examinations and referral to ophthalmology in 2010 and 2012. We also performed multivariate logistic regression analysis to evaluate potential risk factors (independent variables) for nonadherence to diabetic eye examination. In our initial model, we included all of the independent variables which could potentially affect adherence with annual diabetic eye examination screening (the outcome variable) among Medicaid diabetic patients. We then deleted the independent variables which did not affect the outcome of the model. Some independent variables were not statistically significant in the model but were included in the final one since they impacted the relationship of other independent variables with the outcome variable.
Results
Baseline characteristics
There were 213 Medicaid patients with a diagnosis of diabetes using HEDIS codes in 2010 and 228 patients in 2012. Age and gender distributions were not statistically significantly different in 2010 and 2012; mean age of 51.4 and 52.3 years in 2010 and 2012 (P = 0.16), 82.6% and 82.0% were female in 2010 and 2012 (P = 0.87). In 2010, 84.0% of patients received annual HbA1C measurements while the HbA1C rate increased to 93.9% in 2012 (P = 0.00). In 2012, 69.3% of primary care providers and 88.6% of patients received incentives, a gift card of $20, to complete the diabetic eye examination. It is important to note that the provider incentives were paid to Johns Hopkins Community Physicians and were not paid specifically to individual providers. There was no offer for incentives to physicians and patients in 2010. The mean medication possession ratio (MPR) score for diabetic medications in 2010 was 0.70 (standard deviation (SD): 0.02), and it was 0.71 (SD: 0.02) in 2012. The difference was not statistically significant (P = 0.57). In 2010, RUB was moderate for 39.4%, high for 34.3%, and very high for 23.9% of patients. In 2012, RUB was moderate for 36.8%, high for 29.8%, and very high for 32.5% of patients.
Annual diabetic eye examination and risk factor for noncompliance with the exam
In 2010, 47.9% of patients completed their annual diabetic eye examination while in 2012 the completion rate increased to 78.1% (P < 0.001). Table 1 presents the result of multivariate logistic regression model for compliance with an annual diabetic eye examination. The odds ratio (OR), 95% confidence interval (95% CI), and P value for each of the covariates in the model are reported in Table 1.
Table 1.
Multivariate logistic regression for annual diabetic eye examination and risk factor for noncompliance with the exam
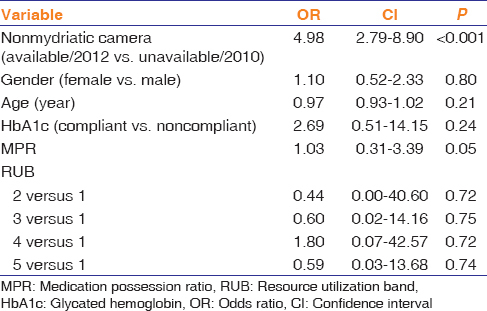
The OR for completing an annual diabetic eye examination was 4.98 (95% CI; 2.79, 8.90) comparing 2012 (when patients had access to nonmydriatic camera) to 2010 (where there was not access to a nonmydriatic camera) (P < 0.001). The OR of having an annual diabetic eye examination to not having an examination was 0.97 (95% CI; 0.93, 1.02) with each 1 year increase in age. Those receiving annual HbA1C measurement had an OR of 2.69 (95% CI; 0.51, 14.15) for completing an annual diabetic eye examination compared to those who did not receive annual HbA1C measurement. Comparing low, moderate, high, and very high RUB to healthy users the OR for completing the annual diabetic eye examination was 0.44 (95% CI; 0.00, 40.60), 0.60 (95% CI; 0.02, 14.16), 1.80 (95% CI; 0.07, 42.57), and 0.59 (95% CI; 0.03, 13.68), respectively.
Referral to ophthalmologists
We reviewed the nonmydriatic camera reports of the annual diabetic eye examinations for patients at EBMC in 2012. Of 228 patients with a diagnosis of diabetes based on HEDIS codes, 179 (79%) completed an annual diabetic eye examination. This included either an eye examination by an ophthalmologist/optometrist or imaging by nonmydriatic camera at EBMC. Diabetic eye examination reports were available for 146 patients, and for the remaining patients either the scan report was missing in the system or the scan was of poor quality and the presence or absence of DR could not be determined based on the scan. 25 out of 146 (17%) patients had DR identified in their scan, of which 3 patients had a health care claim from an ophthalmology visit (completed referral rate of 12%).
Discussion
We found that the establishment of telemedicine technology was an effective and efficient way to increase the completion rate of annual diabetic eye examinations among underserved, low-income patients in an urban primary care setting. The completion rate for annual diabetic eye examinations in our population increased from 47.9% in 2010 to 78.1% in 2012. After adjustment for other factors, the OR for completing the annual diabetic eye examination was 4.98 comparing 2012 with access to nonmydriatic camera technology, to 2010 where there was not access to onsite camera. With the development of telemedicine technology for DR screening, various DR screening programs have been tested in the United States and around the world. This new telemedicine technology has made it possible for diabetic patients to receive an annual diabetic eye examination without an ophthalmology visit.[17] In the urban setting in which this study focuses, the presence of an onsite screening tool that did not require patients to have their pupils dilated was seen as a key factor in increased screening rates. With telemedicine technology, health care services may be located in shops, workplaces, residences, schools and primary care physician offices, and patients can provide a retinal image for screening without the need for pupil dilation or the presence of an ophthalmologist or retinal specialist.[3] These health care services in connection with an ophthalmology center would complete the annual eye examination process, by reviewing the scanned images, and assessing for the need for further medical intervention.
Telemedicine technology has shown promising results for screening and detection of DR.[6] Studies have shown high sensitivity and specificity for telemedical digital imaging in distinguishing DR severity levels. There is favorable concordance between telemedical digital imaging and the gold standard of dilated fundoscopy examination, in identifying DR severity and DR-related lesions.[6,7] Studies have reported high inter-grader reliability for telemedicine technology, indicating that DR is similarly detected and scored, in terms of DR severity and retinal lesions, when images are read by different image graders.[6] Onsite telemedicine screening is reported as convenient by many patients and results in high patient satisfaction and increased adherence to annual screening.[6,7,8] Telemedicine technology has successfully assisted the health-care system to resolve social and cultural barriers and has facilitated greater access to care for remote communities and those with less access to traditional methods of screening.[9,10] It is also a cost-effective method for reducing disparities in DR screening services for underserved areas, especially in clinical settings with a large patient population.[18,19]
Among factors playing a role in patients' adherence to annual diabetic eye examinations, HbA1C measurement, higher MPR, and higher RUB score showed a potential relationship with higher rate of compliance. Although each of these variables was not statistically significant, we did not delete them from the final model due to their impact on final outcome. Patients who received annual HbA1C measurement showed a two-fold rate in receiving a diabetic eye exam. Those with higher MPR had a slightly higher rate of annual diabetic eye examination. Patients with higher RUB (those with more severe disease) had a higher rate of examination as well. We believe the first two indices are indicators of patient engagement in managing their diabetic disease. Those with a more active role in the management of their diabetic disease, namely those compliant with HbA1C measurement and with a higher MPR, may be more engaged in controlling their disease and may be more likely to complete their annual eye exam. Those with higher RUB score and higher risk of DR have a higher rate of completion of eye examination. The exception to this is in high acuity patients with RUB score of 5. In these patients, the severity of disease and the possible presence of life-threatening DM complications may prevent them from completing their annual diabetic eye exam.
A major issue in the control of DR is providing resources for those with any sign of DR in their annual screening. In our population, only 3 out of 25 patients with DR identified in their retinal scan had a health care claim from an ophthalmology visit (rate of 12%). This might be an underestimation of rate since for some patients, an ophthalmologist performed the annual diabetic eye examination and no further workup or treatment was needed at the time of DR diagnosis. The claims data also does not reflect those ophthalmology visits where the patient did not use their insurance service or where there might be coding errors which did not reflect diagnosis or treatment of DR. The communications between physicians and patients regarding the results of the screening and the next required step based on the results of the current screening requires some improvement. We could consider the automatic communication of the results with the primary care physician, the primary care clinic, and if available with the patients through cell phone. It would be advisable to state the next screening time for the patients if no intervention is needed at this stage. Establishment of a referral system for those patients with positive findings in their screening examination is necessary for the success of the screening program in improving patients' outcomes.
The increase in annual diabetic eye examination rates in our Medicaid population is consistent with findings in other studies on minorities and those with less access to health care services.[9,10] Although we only evaluated this system among Medicaid patients in an urban setting, it may generalize to other patient populations. The establishment of this technology could be easily adapted in other primary care settings.
This study has important implications for clinical practice. Beyond increasing screening rates in a practice's diabetic population, another benefit is that it would allow precious outreach efforts to be focused on fewer patients needing eye examinations, or on other quality of care metrics. In addition, the occasion of the DR screening could be used to provide health promotion and increase the awareness regarding the condition and required follow-up examinations.
The current study has some limitations. Application of health care claims data relies on the quality of reported claims and coding of services, which might not be complete. This method also misses patients who seek services outside their insurance network. Further, the study reflects the behaviors of patients and providers in one geographic region – urban Mid-Atlantic, which may limit its generalizability. The gender disparity of the study population, with more than 80% of participants being female, might affect the generalization of this result to the general population. In addition, the population was selected based on HEDIS code set, which is fairly rigorous. Thus, some patients with diabetes may have been excluded from the analysis. The financial incentive considered for patients and providers in this setting would be an issue in countries with low income and middle income. In such countries, one should entirely rely on personal motivation among patients and providers.
Conclusions
The rate of annual diabetic eye examination completion is low in our diabetic Medicaid population. Application of telemedicine technology in the primary care setting can increase the rate of annual diabetic eye examinations in under-served, low-income populations such as Medicaid patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Prevention of Blindness from Diabetes Mellitus. [Last accessed on 2016 Aug 29]. Available from: http://www.who.int/blindness/PreventionofBlindnessfromDiabetesMellitus.with.cover.small.pdf .
- 4.Vitale S. The Wisconsin epidemiologic study of diabetic retinopathy: What can we learn at 14 years? Ophthalmology. 1998;105:1799–800. doi: 10.1016/S0161-6420(98)91019-3. [DOI] [PubMed] [Google Scholar]
- 5.Moss SE, Klein R, Klein BE. Factors associated with having eye examinations in persons with diabetes. Arch Fam Med. 1995;4:529–34. doi: 10.1001/archfami.4.6.529. [DOI] [PubMed] [Google Scholar]
- 6.Vaziri K, Moshfeghi DM, Moshfeghi AA. Feasibility of telemedicine in detecting diabetic retinopathy and age-related macular degeneration. Semin Ophthalmol. 2015;30:81–95. doi: 10.3109/08820538.2013.825727. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed J, Ward TP, Bursell SE, Aiello LM, Cavallerano JD, Vigersky RA, et al. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Diabetes Care. 2006;29:2205–9. doi: 10.2337/dc06-0295. [DOI] [PubMed] [Google Scholar]
- 8.Conlin PR, Fisch BM, Cavallerano AA, Cavallerano JD, Bursell SE, Aiello LM, et al. Nonmydriatic teleretinal imaging improves adherence to annual eye examinations in patients with diabetes. J Rehabil Res Dev. 2006;43:733–40. doi: 10.1682/jrrd.2005.07.0117. [DOI] [PubMed] [Google Scholar]
- 9.Arora S, Kurji AK, Tennant MT. Dismantling sociocultural barriers to eye care with tele-ophthalmology: Lessons from an Alberta Cree community. Clin Invest Med. 2013;36:E57–63. doi: 10.25011/cim.v36i2.19567. [DOI] [PubMed] [Google Scholar]
- 10.Mansberger SL, Gleitsmann K, Gardiner S, Sheppler C, Demirel S, Wooten K, et al. Comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: A randomized controlled trial. Telemed J E Health. 2013;19:942–8. doi: 10.1089/tmj.2012.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harding S, Greenwood R, Aldington S, Gibson J, Owens D, Taylor R, et al. Grading and disease management in national screening for diabetic retinopathy in England and Wales. Diabet Med. 2003;20:965–71. doi: 10.1111/j.1464-5491.2003.01077.x. [DOI] [PubMed] [Google Scholar]
- 12.The National Committee for Quality Assurance HEDIS & Performance Measurement. [Last accessed on 2016 Aug 29]. Available from: http://www.ncqa.org/HEDISQualityMeasurement.aspx .
- 13.The National Committee for Quality Assurance. Technical Updates. [Last accessed on 2016 Aug 29]. Available from: http://www.ncqa.org/portals/0/PolicyUpdates/HEDIS%20Technical%20Updates/09_CDC_Spec.pdf .
- 14.The Johns Hopkins ACG® System, Version 9.0. [Last accessed on 2016 Aug 29]. Available from: http://www.acg.jhsph.org/
- 15.Petersen LA, Pietz K, Woodard LD, Byrne M. Comparison of the predictive validity of diagnosis-based risk adjusters for clinical outcomes. Med Care. 2005;43:61–7. [PubMed] [Google Scholar]
- 16.Orueta JF, Urraca J, Berraondo I, Darpón J, Aurrekoetxea JJ. Adjusted clinical groups (ACGs) explain the utilization of primary care in Spain based on information registered in the medical records: A cross-sectional study. Health Policy. 2006;76:38–48. doi: 10.1016/j.healthpol.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Conlin PR, Fisch BM, Orcutt JC, Hetrick BJ, Darkins AW. Framework for a national teleretinal imaging program to screen for diabetic retinopathy in Veterans Health Administration patients. J Rehabil Res Dev. 2006;43:741–8. doi: 10.1682/jrrd.2005.08.0146. [DOI] [PubMed] [Google Scholar]
- 18.Hazin R, Barazi MK, Summerfield M. Challenges to establishing nationwide diabetic retinopathy screening programs. Curr Opin Ophthalmol. 2011;22:174–9. doi: 10.1097/ICU.0b013e32834595e8. [DOI] [PubMed] [Google Scholar]
- 19.Kirkizlar E, Serban N, Sisson JA, Swann JL, Barnes CS, Williams MD, et al. Evaluation of telemedicine for screening of diabetic retinopathy in the Veterans Health Administration. Ophthalmology. 2013;120:2604–10. doi: 10.1016/j.ophtha.2013.06.029. [DOI] [PubMed] [Google Scholar]