Abstract
Background & objectives:
Trauma is known to lead to systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome (MODS), which is often a cause of late deaths after injury. SIRS and MODS have been objectively measured using scoring systems. This prospective observational study was carried out in a tertiary care hospital in India to evaluate SIRS and MODS following trauma in terms of their incidence, the associated risk factors and the effect on the outcome.
Methods:
All adult patients with major life- and limb-threatening trauma were included. Patients who died within 24 h, those with severe head injury, known comorbidity, immunocompromised state, on immunosuppressants or pregnancy were excluded. SIRS and MODS scores were recorded after initial management (baseline score), on days 3 and 6 of admission. SIRS was defined as SIRS score of ≥2 and MODS was defined as MODS score of ≥1.
Results:
Two hundred patients were enrolled. SIRS was noted in 156 patients (78%). MODS was noted in 145 (72.5%) patients. Overall mortality was 39 (19.5%). Both SIRS and MODS scores were significantly associated with age >60 yr, blunt injury, (lower) revised trauma score hypotension on admission and (higher) injury severity score, but not with gender, pre-hospital time or operative treatment.
Interpretation & conclusions:
Both SIRS and MODS scores were associated with longer Intensive Care Unit (ICU) stay, more ICU interventions and higher mortality. Incidence of MODS was significantly higher in patients with SIRS. Both scores showed rising trend with time in non-survivors and a decreasing trend in survivors. The serial assessment of scores can help prognosticate outcome and also allocate appropriate critical care resources to patients with rising scores.
Keywords: Injury, MODS Score, multiple organ dysfunction syndrome, SIRS, Systemic inflammatory response syndrome score, trauma
Mortality occurring early after injury is due to vital organ injury, hypoxia, haemorrhage or head trauma. Among those who survive the initial phase of injury, there is activation of the immune system and the early inflammatory immune response. It is believed that inappropriate inflammatory response may lead to end-organ damage manifesting as multiple organ dysfunction1. It is considered as a disease continuum beginning as systemic inflammatory response syndrome (SIRS) progressing to multiple organ dysfunction syndrome (MODS) in some cases. The inflammatory response is further compounded by iatrogenic trauma of surgery, secondary infections, or ischaemia/reperfusion, which may also lead to the development of multiorgan dysfunction and occasionally death1.
SIRS with a documented source of infection is termed as sepsis. When there is infection along with one or more organ failure, it is termed as severe sepsis, and haemodynamic instability in the presence of sepsis is known as septic shock. Trauma, burns and pancreatitis are known to induce systemic inflammatory response and multiple organ dysfunction in the absence of infection2.
Tissue injury releases mediators of inflammation into the circulation, initiating a pro-inflammatory response, consisting of neuroendocrine, metabolic and immunological components. The extent of this response is determined by several factors such as the tissue injury, hypovolemic shock, further trauma of surgery, infection and compensatory anti-inflammatory response1,3. The inappropriate response may damage vital organs such as lungs, kidneys, liver, brain, coagulation system and cardiovascular system, leading to MODS, ultimately leading to death.
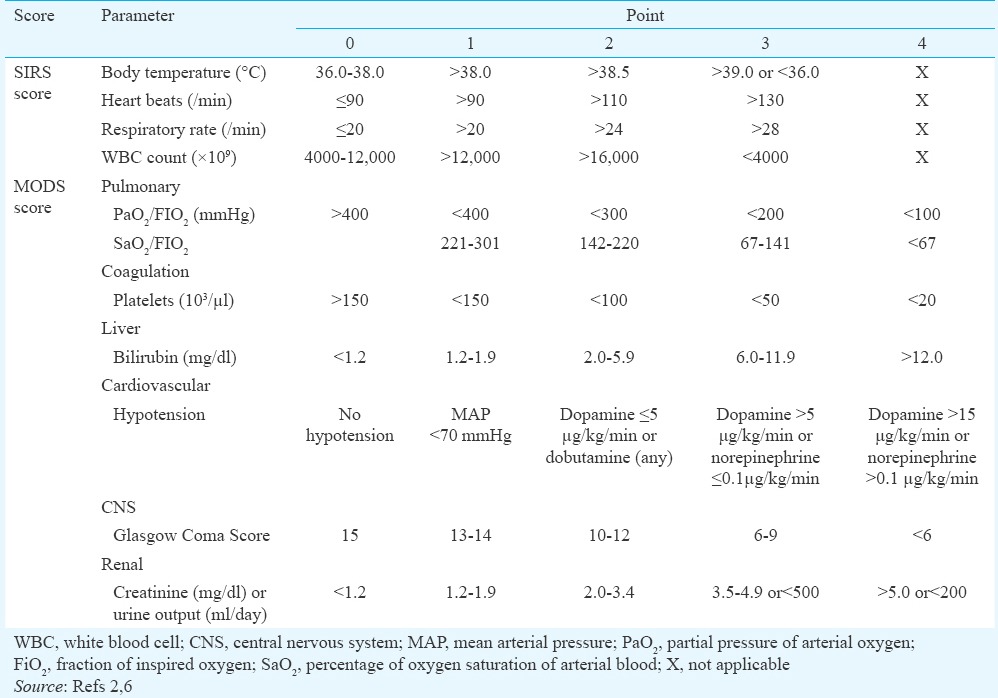
Various scoring systems have been described to measure the extent of inflammatory response and the organ damage. Systemic inflammatory response presents with alteration in body temperature (>38 or <36°C), tachycardia (pulse >90/min), tachypnoea (respiratory rate >20/min) or alteration in white cell count (<4000 or >12,000/μl)2. SIRS is defined as the presence of any two of these features2. Several scoring systems have been used to assess organ dysfunction in a critical patient. The Acute Physiology and Chronic Health Evaluation (APACHE) score version II4 and III5 are popular, but cumbersome to calculate. Multiple organ dysfunction (MOD) score6, sequential organ failure assessment (SOFA)7 and logistic organ dysfunction (LOD) score8 have been specifically used to assess organ dysfunction in sepsis syndrome. They consider six organ systems - respiratory, cardiovascular, central nervous systems, renal, coagulation and liver and all have been reported to be satisfactory in predicting mortality9.
The purpose of this study was to observe the burden of inflammatory response and organ dysfunction in major trauma patients in a tertiary care hospital in India using SIRS and MODS scores, respectively, noting the incidence, associated risk factors and outcome in terms of the need for critical care, duration of Intensive Care Unit (ICU) stay, hospital stay and survival. Associations between SIRS score and MODS score and their change with time were also evaluated.
Material & Methods
This study was carried out in the Trauma Service by the department of General Surgery at Lokmanya Tilak Municipal Medical College and General Hospital in Mumbai, India, as a prospective and observational study after obtaining approval from the institutional ethics committee from January 2012 to November 2013. The reported incidence of SIRS varies widely from 28 to 88 per cent10,11,12,13. Taking median incidence of 53.3 per cent reported by Sakamoto et al10, with 80 per cent power of analysis and 5 per cent confidence interval, a sample size of 154 was obtained. Considering wide variation in reported incidence, the possibility of dropout due to loss to follow up or missing data, a larger sample size of 200 was planned. Patients with life- or limb-threatening injuries were included, namely those with haemodynamic instability [systolic blood pressure (BP) <90 mmHg, respiratory rate <10 or >29/min, pulse >100/min or need for ventilator support], altered consciousness [Glasgow Coma Score (GCS) <13], tender chest or abdomen, fracture pelvis, fracture spine, fracture femur, two or more long bone fractures, amputation above ankle or wrist, penetrating trauma to head, neck, torso or proximal extremity and mangled, degloved, crushed or pulseless extremity. Those with hospital stay less than 24 h and those with very severe injury with poor chance of survival beyond 24 h were excluded as the basic aim was to observe the development of organ dysfunction over time, namely, non-responders to resuscitation, GCS <9 despite resuscitation and fixed dilated pupils. Patients with known pre-existing organ dysfunctions e.g. renal failure, cardiac failure, liver failure, pulmonary failure or coagulopathy were excluded as possible confounders to assessment of MODS. Those with known altered immune response i.e. immunocompromised state (including chronic steroid therapy and cancer chemotherapy) and pregnant women were also excluded. Age, gender, mechanism of injury (blunt/penetrating) and injury to admission intervals were noted. Revised Trauma Score (RTS) was calculated assigning 0-4 points each for GCS, systolic BP and respiratory rate, with possible range from 0 to 1214. Injury Severity Score (ISS) was the sum of squares of highest abbreviated injury score of any three of the six body regions with possible range from 0 to 7515. ISS values of 9 or less, 10-15 and 16 or above were defined as mild, moderate and severe injury, respectively. SIRS score was calculated by assigning 0 to 3 points each for body temperature, pulse rate, respiratory rate and white blood cell count and ranged from 0 to 12 (Table I)2. SIRS was defined as score of 2 or more. MODS scores were calculated by assigning 0-4 points for 6 organ systems (pulmonary, coagulation, liver, renal, cardiovascular and central nervous system), with the possible range from 0 to 24 points (Table I)6. Presence of MODS was defined as score of 1 or more, 1-2 being mild MODS and 3 or more being considered as severe MODS6. The SIRS score and the MODS score were calculated for the patients after resuscitation (baseline score), on days 3 and 6 of admission, irrespective of the hospital stay. The treatment plan whether operative or conservative was noted. The need for interventions for organ dysfunction e.g. ventilatory support, blood or component transfusion, inotropic support and haemodialysis was noted. The duration of hospital stay, ICU stay and final outcome (death, discharge) were recorded. Changes in SIRS and MODS scores on days 3 and 6 with respect to the baseline score were noted.
Table I.
Systemic Inflammatory Response Syndrome (SIRS) score and Multiple Organ Dysfunction Syndrome (MODS) score
Statistical analysis: SPSS for Windows, version 16 (SPSS Inc, Chicago, IL, USA) was used for data analysis. Chi-square test was used to study association between categorical variables. For ordinal data, Chi-square test for trend was used. The means were compared using ANOVA.
Results
In all, 200 patients were enrolled in the study. The Figure shows patients’ course from screening till final outcome. There were 167 (83.5%) men and 33 women. Age ranged from 18 to 85 yr [mean: 35.48, standard deviation (SD): 15.71, median: 30, interquartile range (IQR): 22]. Median pre-hospital time (injury to hospital time) was five hours (IQR: 5, range: 0.5-72 h). Mechanism of injury was blunt in 171 and penetrating in 29 patients. Sixty patients (30%) presented in shock (systolic BP <90 mmHg). Glasgow Coma Score ranged from 9 to 15 (mean: 13.83, SD: 1.98, median: 15, IQR: 2). RTS ranged from 8 to 12 (mean: 11.23, SD: 0.94, median: 11, IQR: 1). ISS ranged from 4 to 27 (mean: 16.82, SD: 6.39, median: 16, IQR: 14). Ninety two patients (46%) needed surgical management while 108 (54%) patients were managed without any surgical intervention. In all, 156 patients (78%) developed SIRS (SIRS score ≥2), 145 patients (72.5%) developed MODS (MODS score ≥1) and 39 patients (19.5%) died.
Figure.
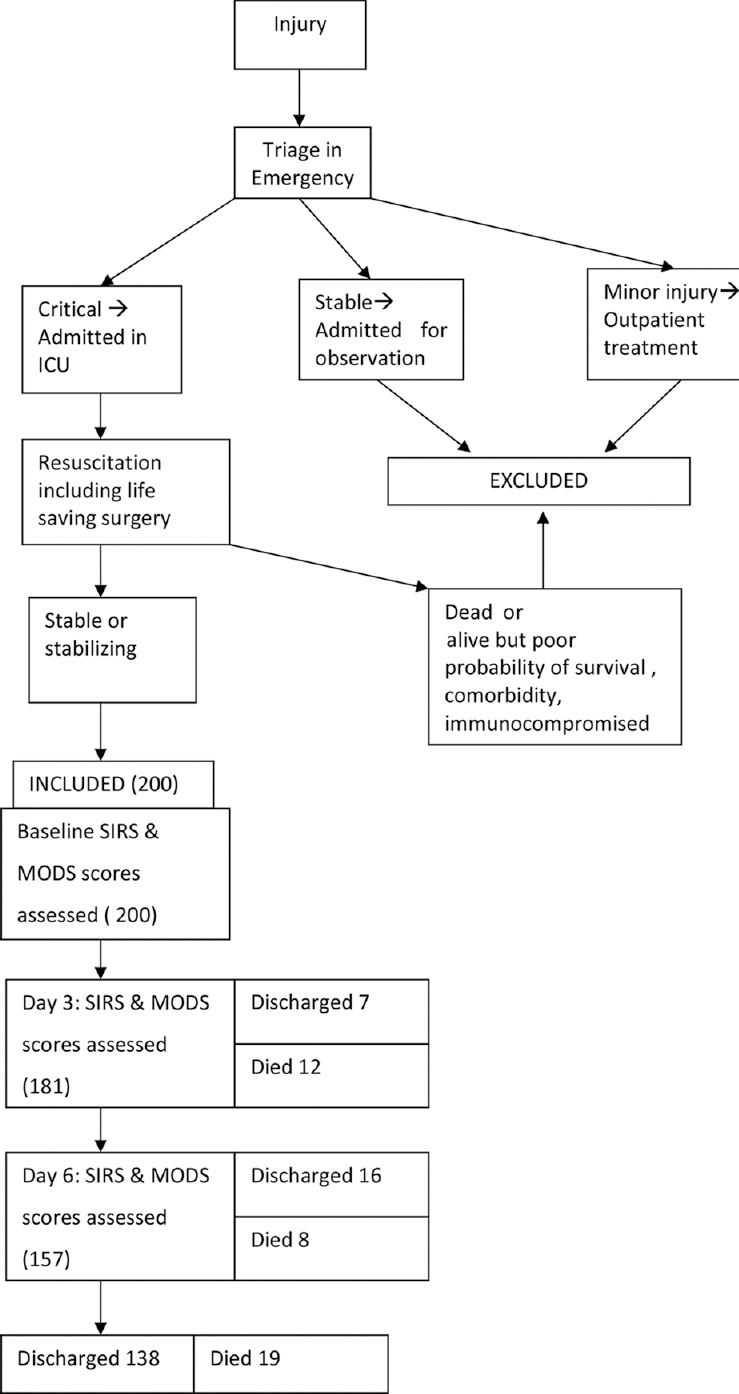
Flow chart showing patients’ course from screening to final outcome. SIRS Systemic Inflammatory Response Syndrome; MODS, Multiple Organ Dysfunction Syndrome; ICU, Intensive Care Unit.
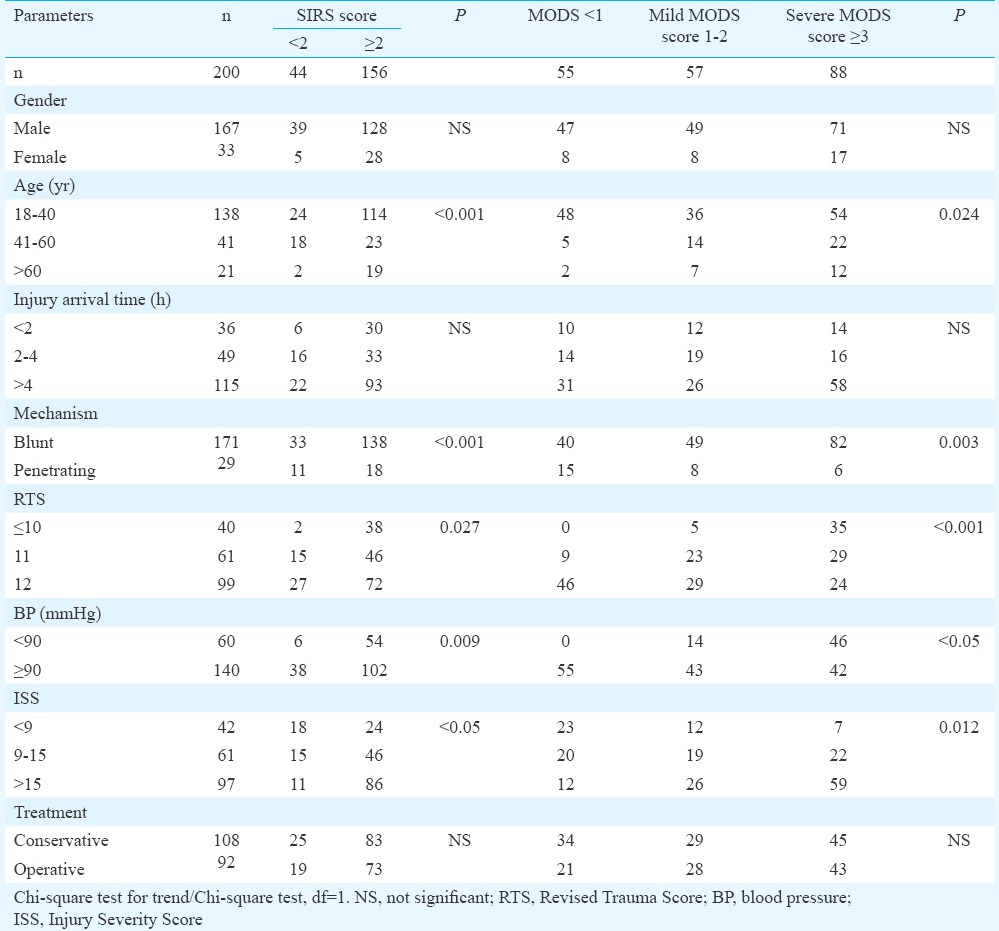
Table II depicts the association of baseline SIRS and MODS scores with demographic and clinical variables. SIRS (SIRS score ≥2) and MODS (MODS score ≥1) were associated with advanced age >60 yr, mechanism of injury and physiological and anatomical indicators of injury severity, namely, RTS, systolic BP <90 mmHg and ISS, but not with gender, prehospital time and treatment whether operative or conservative.
Table II.
Factors associated with systemic inflammatory response syndrome (SIRS score ≥2) and multiple organ dysfunction syndrome (MODS score ≥1)
ICU stay ranged from 1 to 27 days (mean: 2.97, SD: 3.96, median: 2, IQR: 2). Hospital stay ranged from 1 to 38 days (mean: 10.10, SD: 6.65, median: 9, IQR: 6). Sixty two patients (31%) needed red cell transfusion (single or multiple units), 32 (16%) needed fresh frozen plasma, while 16 (8%) needed platelet transfusion, 52 (26%) needed ventilatory support, while five needed dialysis for acute renal failure. In all, 33 patients needed inotropic support. Table III shows the association of length of ICU stay, hospital stay, need for critical care resources and mortality with SIRS and MODS scores. SIRS and MODS scores were associated with prolonged ICU stay and the need for critical care resources. SIRS score was also associated with prolonged hospital stay of >10 days.
Table III.
Association of Systemic Inflammatory Response Syndrome (SIRS score ≥2) and Multiple Organ Dysfunction Syndrome (MODS score ≥1) on Intensive Care Unit (ICU) resources, ICU stay, hospital stay and mortality
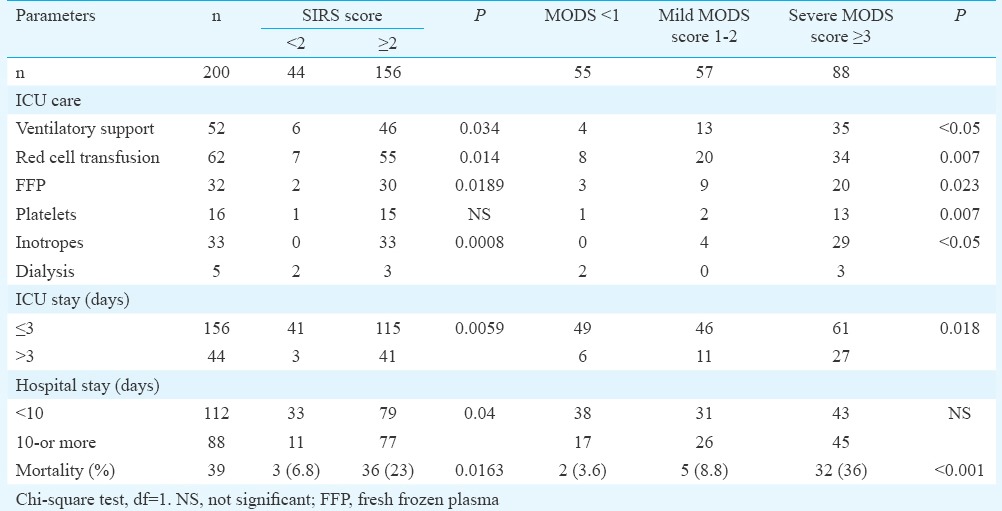
Table IV shows association between SIRS score and MODS score. Significantly higher number of patients who had SIRS developed multiple organ dysfunction in comparison to patients who did not have SIRS on arrival (baseline). There were 39 deaths. The cause of death was continuing haemorrhage in six and multiple organ dysfunction in 32 patients. One patient had sudden death and the exact cause could not be ascertained. Of the 32 deaths due to MODS, only two (6.25%) were observed to be due to single organ dysfunction and the remaining 30 deaths (93.75%) had dysfunction of two or more organs.
Table IV.
Association between Systemic Inflammatory Response Syndrome (SIRS) score and Multiple Organ Dysfunction Syndrome (MODS) score
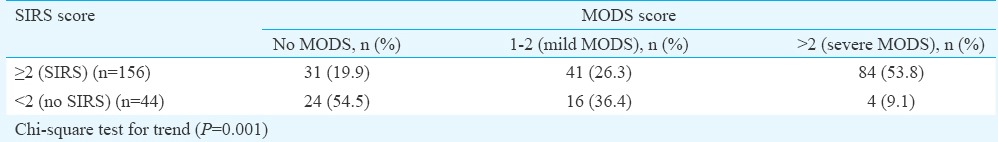
Of the 156 patients who had SIRS on day 1, 36 (23%) died. In comparison, three deaths (6.8%) occurred in 44 patients who had no signs of SIRS on day 1 (P=0.016). Of the 88 patients who had severe MODS on day 1, 32 (36%) died; of the 57 who had mild MODS on day 1, five patients (8.8%) died while only two deaths (3.6%) occurred in 55 patients who did not develop MODS on day 1 (P<0.001). Thus, mortality was significantly associated with the development of SIRS and MODS as defined by the scores.
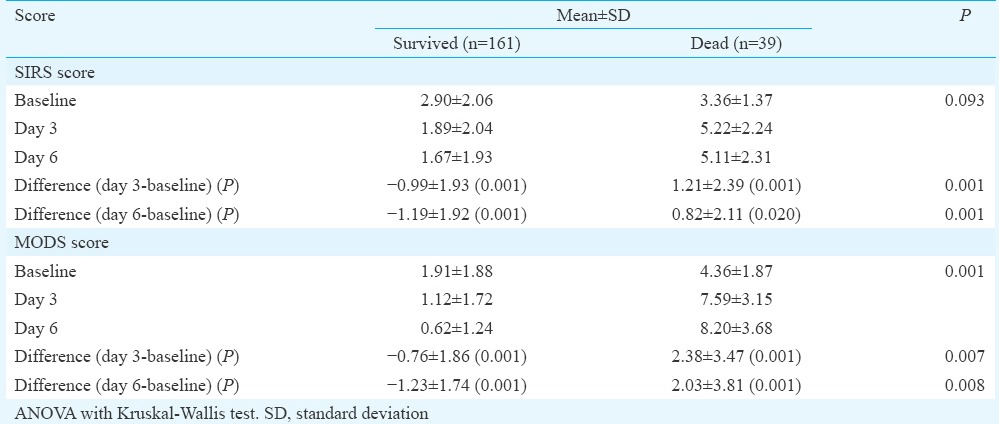
The scores in survivors and non-survivors were compared. There was no significant difference in the baseline SIRS scores. In comparison, baseline mean MODS score of 4.36 was significantly (P<0.001) higher among non-survivors (Table V). The mean SIRS and MODS scores on days 3 and 6 were calculated for all available patients. The mean SIRS and MODS scores among survivors and non-survivors against time showed progressive rise among non-survivors and progressive fall among survivors. The change in scores on days 3 and 6 with respect to the baseline score was calculated for each available patient. The difference in the means of change in scores on days 3 and 6 among survivors and non-survivors was significant. The decline of scores on days 3 and 6 among survivors and the rise of scores on days 3 and 6 among non-survivors with respect to the baseline were also significant (Table V).
Table V.
Changes in systemic inflammatory response syndrome (SIRS) score and multiple organ dysfunction syndrome (MODS) score with time among survivors and non-survivors
Discussion
The study showed that post-traumatic inflammation and organ dysfunction as assessed by SIRS score and MODS score were common after major injury. The incidence of SIRS (SIRS score ≥2) was 78 per cent and MODS (MODS score ≥1) was 72.5 per cent on the day after initial resuscitation. The incidence reported in the literature varies from 28 to 88 per cent in different series10,11,12,13. This divergence in the incidence of SIRS seems to be due to variability in inclusion criteria [whether all hospitalized patients (lower incidence), patients admitted in ICU and high dependency unit or major trauma patients (higher incidence)].
Although our study did not show any association with gender, some experimental studies have observed protective effect of oestrogens in animals with trauma, haemorrhage and sepsis16. Not only gender, but racial difference also has been reported to determine inflammatory response with lesser incidence in women and in African-Americans13. The present study showed significantly higher incidence of SIRS, MODS and mortality in elderly patients (age >60 yr), similar to observations by other researchers17,18. This may be because of their susceptibility to infection due to inappropriate immune response and limited physiological reserves18.
SIRS and MODS scores were significantly associated with severity of injury as assessed by both physiological score (RTS) and anatomical scores (ISS) and also post-traumatic shock, confirming the findings of other researchers10,11. No association was observed between injury to arrival interval and development of SIRS and MODS. It is possible that patients with severe injuries do not survive till they reach a tertiary care hospital and those who survive and reach the tertiary hospital have less severe injuries.
Patients with SIRS and MODS were found to consume significantly higher critical care resources in terms of ventilator support, blood components and dialysis. This has been observed by others also11,19,20. Both SIRS and MODS were associated with higher mortality; similar to observations by other authors19,20,21.
SIRS score of two and above was associated with higher MODS score in significantly more number of patients. This observation supports the concept that MODS is a sequel to SIRS occurring in an inflammatory or infective disease process. The SIRS and MODS scores showed a decreasing trend with time among survivors and an increasing trend among non-survivors. This finding has also been supported by literature12,22. The delta value (i.e. the difference between initial and maximum MODS score) among survivors and non-survivors has been found to be significantly high among non-survivors23. This also was similar to the findings of this study.
SIRS score could also be raised because of secondary infection, which may occur in patients with major trauma. In a patient with major trauma, who is developing organ dysfunction, it is necessary to rule out infection. The weakness of this study is that it has not captured the information regarding secondary infections arising in such patients. One study has observed that in major trauma patients, early MODS is often associated with hypotension and massive volume administration but very rarely with infection, despite the high rate of SIRS24. In contrast, other studies have found higher SIRS score, particularly in the second and third weeks to be predictor of infection in trauma patients25,26. Various inflammatory markers such as serum interleukin-6 have been studied in search of a predictor of infection27.
The rise in pro-inflammatory markers has been reported among patients undergoing early surgery for trauma as compared to patients not undergoing surgery and control group28. However, in the present study, the trauma of surgery performed for treatment of injury did not seem to significantly contribute to this post-traumatic inflammation, organ dysfunction or mortality. Life saving surgery in trauma is carried out to control haemorrhage, prevent contamination and sepsis, decompress closed spaces and immobilize and reperfuse ischaemic limb. Although the trauma of surgery may enhance inflammation, its effect may reduce the organ damage.
Systemic inflammatory response and subsequent organ dysfunction are commonly observed after major trauma, predominantly in patients with severe injury and those in shock. Patients with SIRS score of 2 or more on day 1 after arrival to the hospital are more likely to develop MODS and are therefore, likely to need prolonged ICU stay and critical care interventions such as ventilatory support, blood and blood products and at times, inotropic support. It is useful to monitor SIRS and MODS scores serially, because their rising trend over time is suggestive of worsening condition and indicates the need for close monitoring and timely and appropriate critical care support. This should also be useful in counselling about prognosis.
Footnotes
Conflicts of Interest: None.
References
- 1.Lenz A, Franklin GA, Cheadle WG. Systemic inflammation after trauma. Injury. 2007;38:1336–45. doi: 10.1016/j.injury.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine Chest. 1992;101:1644–55. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 3.Brøchner AC, Toft P. Pathophysiology of the systemic inflammatory response after major accidental trauma. Scand J Trauma Resusc Emerg Med. 2009;17:43. doi: 10.1186/1757-7241-17-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 5.Wong DT, Knaus WA. Predicting outcome in critical care: The current status of the APACHE prognostic scoring system. Can J Anaesth. 1991;38:374–83. doi: 10.1007/BF03007629. [DOI] [PubMed] [Google Scholar]
- 6.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: A reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–52. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in Intensive Care Units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, et al. The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the Intensive Care Unit. ICU Scoring Group. JAMA. 1996;276:802–10. doi: 10.1001/jama.276.10.802. [DOI] [PubMed] [Google Scholar]
- 9.Khwannimit B. A comparison of three organ dysfunction scores: MODS, SOFA and LOD for predicting ICU mortality in critically ill patients. J Med Assoc Thai. 2007;90:1074–81. [PubMed] [Google Scholar]
- 10.Sakamoto Y, Mashiko K, Matsumoto H, Hara Y, Kutsukata N, Yokota H. Systemic inflammatory response syndrome score at admission predicts injury severity, organ damage and serum neutrophil elastase production in trauma patients. J Nippon Med Sch. 2010;77:138–44. doi: 10.1272/jnms.77.138. [DOI] [PubMed] [Google Scholar]
- 11.Baek JH, Kim MS, Lee JC, Lee JH. Systemic inflammation response syndrome score predicts the mortality in multiple trauma patients. Korean J Thorac Cardiovasc Surg. 2014;47:523–8. doi: 10.5090/kjtcs.2014.47.6.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muckart DJ, Bhagwanjee S. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med. 1997;25:1789–95. doi: 10.1097/00003246-199711000-00014. [DOI] [PubMed] [Google Scholar]
- 13.NeSmith EG, Weinrich SP, Andrews JO, Medeiros RS, Hawkins ML, Weinrich MC. Demographic differences in systemic inflammatory response syndrome score after trauma. Am J Crit Care. 2012;21:35–41. doi: 10.4037/ajcc2012852. [DOI] [PubMed] [Google Scholar]
- 14.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma. 1989;29:623–9. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 16.Choudhry MA, Bland KI, Chaudry IH. Trauma and immune response – Effect of gender differences. Injury. 2007;38:1382–91. doi: 10.1016/j.injury.2007.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stephen AH, Heffernan DS, Monaghan SF, Adams CA, Cioffi WG. The presence, but not the degree of systemic inflammatory response syndrome (SIRS) in elderly trauma patients is predictive of mortality. J Surg Res. 2010;158:351–2. [Google Scholar]
- 18.Smith RM. Immunity, trauma and the elderly. Injury. 2007;38:1401–4. doi: 10.1016/j.injury.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 19.Malone DL, Kuhls D, Napolitano LM, McCarter R, Scalea T. Back to basics: Validation of the admission systemic inflammatory response syndrome score in predicting outcome in trauma. J Trauma. 2001;51:458–63. doi: 10.1097/00005373-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Napolitano LM, Ferrer T, McCarter RJ, Jr, Scalea TM. Systemic inflammatory response syndrome score at admission independently predicts mortality and length of stay in trauma patients. J Trauma. 2000;49:647–52. doi: 10.1097/00005373-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Pettilä V, Pettilä M, Sarna S, Voutilainen P, Takkunen O. Comparison of multiple organ dysfunction scores in the prediction of hospital mortality in the critically ill. Crit Care Med. 2002;30:1705–11. doi: 10.1097/00003246-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Talmor M, Hydo L, Barie PS. Relationship of systemic inflammatory response syndrome to organ dysfunction, length of stay, and mortality in critical surgical illness: Effect of Intensive Care Unit resuscitation. Arch Surg. 1999;134:81–7. doi: 10.1001/archsurg.134.1.81. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs S, Zuleika M, Mphansa T. The Multiple Organ Dysfunction Score as a descriptor of patient outcome in septic shock compared with two other scoring systems. Crit Care Med. 1999;27:741–4. doi: 10.1097/00003246-199904000-00027. [DOI] [PubMed] [Google Scholar]
- 24.Smail N, Messiah A, Edouard A, Descorps-Declère A, Duranteau J, Vigué B, et al. Role of systemic inflammatory response syndrome and infection in the occurrence of early multiple organ dysfunction syndrome following severe trauma. Intensive Care Med. 1995;21:813–6. doi: 10.1007/BF01700964. [DOI] [PubMed] [Google Scholar]
- 25.Bochicchio GV, Napolitano LM, Joshi M, McCarter RJ, Jr, Scalea TM. Systemic inflammatory response syndrome score at admission independently predicts infection in blunt trauma patients. J Trauma. 2001;50:817–20. doi: 10.1097/00005373-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Hoover L, Bochicchio GV, Napolitano LM, Joshi M, Bochicchio K, Meyer W, et al. Systemic inflammatory response syndrome and nosocomial infection in trauma. J Trauma. 2006;61:310–6. doi: 10.1097/01.ta.0000229052.75460.c2. [DOI] [PubMed] [Google Scholar]
- 27.Lausevic Z, Lausevic M, Trbojevic-Stankovic J, Krstic S, Stojimirovic B. Predicting multiple organ failure in patients with severe trauma. Can J Surg. 2008;51:97–102. [PMC free article] [PubMed] [Google Scholar]
- 28.Tschoeke SK, Hellmuth M, Hostmann A, Ertel W, Oberholzer A. The early second hit in trauma management augments the proinflammatory immune response to multiple injuries. J Trauma. 2007;62:1396–403. doi: 10.1097/TA.0b013e318047b7f0. [DOI] [PubMed] [Google Scholar]


