Abstract
Background & objectives:
Despite an impetus for strengthening public sector district hospitals for provision of secondary health care in India, there is lack of robust evidence on cost of services provided through these district hospitals. In this study, an attempt was made to determine the unit cost of an outpatient visit consultation, inpatient bed-day of hospitalization, surgical procedure and overall per-capita cost of providing secondary care through district hospitals.
Methods:
Economic costing of five randomly selected district hospitals in two north Indian States - Haryana and Punjab, was undertaken. Cost analysis was done using a health system perspective and employing bottom-up costing methodology. Quantity of all resources - capital or recurrent, used for delivering services was measured and valued. Median unit costs were estimated along with their 95 per cent confidence intervals. Sensitivity analysis was undertaken to assess the effect of uncertainties in prices and other assumptions; and to generalize the findings for Indian set-up.
Results:
The overall annual cost of delivering secondary-level health care services through a public sector district hospital in north India was  11,44,13,282 [US Dollars (USD) 2,103,185]. Human resources accounted for 53 per cent of the overall cost. The unit cost of an inpatient bed-day, surgical procedure and outpatient consultation was
11,44,13,282 [US Dollars (USD) 2,103,185]. Human resources accounted for 53 per cent of the overall cost. The unit cost of an inpatient bed-day, surgical procedure and outpatient consultation was  844 (USD 15.5), i; 3481 (USD 64) and
844 (USD 15.5), i; 3481 (USD 64) and  170 (USD 3.1), respectively. With the current set of resource allocation, per-capita cost of providing health care through district hospitals in north India was
170 (USD 3.1), respectively. With the current set of resource allocation, per-capita cost of providing health care through district hospitals in north India was  139 (USD 2.5).
139 (USD 2.5).
Interpretation & conclusions:
The estimates obtained in our study can be used for Fiscal planning of scaling up secondary-level health services. Further, these may be particularly useful for future research such as benefit-incidence analysis, cost-effectiveness analysis and national health accounts including disease-specific accounts in India.
Keywords: Cost per capita, cost per case operated, cost per inpatient bed-day, cost per outpatient consultation, district hospital, economic evaluation, secondary healthcare
District hospitals are the hub of provision of secondary care services in India, with a hospital present in each district. Cases requiring specialist care are referred from a primary health centre to a community health centre or a district hospital. In view of staff shortages at lower levels, district hospitals provide the bulk of secondary health care services1,2.
Various publicly financed health insurance schemes, which cover more than 300 million Indian population, focus on the provision of secondary health care services, with some schemes focusing on tertiary care3. However, when it comes to paying providers for the provision of secondary care, there is no robust evidence of cost of provision of secondary care services. The World Health Organization CHOosing Interventions that are Cost-Effective (WHO-CHOICE) estimates though available, but may not be completely generalizable to Indian setting4. Most of the costing studies available from India are for specific services such as paediatric care5,6 and referral transport7. Although Chatterjee et al8 comprehensively estimated the cost of provision of hospital care, only one typical district hospital from public sector was included in the study. Moreover, this hospital was also chosen using convenience sampling, thus limiting generalizability8. Hence, there is a need to generate evidence for cost of provision of secondary services through district hospitals in public sector in India. We, therefore, undertook this study to estimate the cost of provision of secondary health care services through public sector district hospitals in north India.
Material & Methods
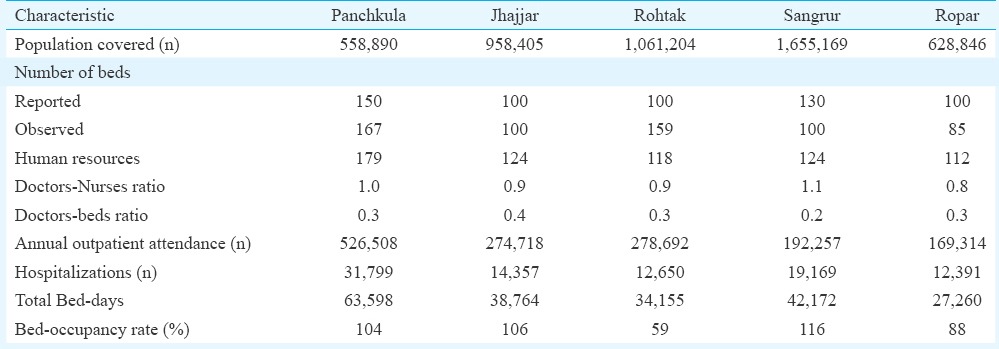
This study was conducted in two north Indian States of Haryana and Punjab. Of the total 43 district hospitals in the two States, five were chosen using simple random sampling: three in Haryana (Panchkula, Jhajjar and Rohtak) and two in Punjab (Sangrur and Ropar). In terms of financing, these hospitals were predominantly tax-funded, with user charges contributing just about 5-10 per cent of revenue9. Table I provides the profile of the study districts and their hospitals.
Table I.
Profile of hospitals studied
Cost data collection: Economic costing was done from a health system perspective and a bottom-up costing methodology was employed10,11. Cost centres at each district hospital were identified in terms of patient care cost centres (PCCs) and support cost centres (SCCs). PCCs, such as the inpatient department, outpatient department (OPD) and operating theatre, are responsible for direct patient services. SCCs provide support for patient care through administration, laundry, kitchen, transport and other units. Data on all resources, capital and recurrent, consumed from April 2012 to March 2013 were collected. Routine records at the district hospital (such as outpatient register, inpatient register, operation theatre register, stock register, indent book and monthly reports) were used to collect the data. This was supplemented with data on incentives paid under various health schemes (to service providers or beneficiaries in case of conditional cash transfers), untied funds and annual maintenance grants, which were collected from the Office of Civil Surgeon (chief of district health administration) at district level. Facility survey of district hospital was undertaken to assess the capital resources i.e. building. Non-consumable stock register was reviewed for a number of equipment's and other capital goods. This was supplemented by physical observation of facility.
The staff members at the district hospital were interviewed using a semi-structured interview schedule on time allocation for different services. At least one specialist in each speciality of the district hospital was interviewed. If there were more than one specialist, then one of them was randomly selected for assessment. In case of paramedical staff, 30 per cent of the total staff at each functional cost centre, i.e. having similar activities, were randomly selected and interviewed. A tool was developed to capture details of all such activities undertaken at different frequencies such as once or twice a year, once a quarter, monthly or weekly, besides daily activities, and time spent each time when the activity was carried out. Output of each activity session was retrieved from the routine records and reports and validated by observation during the period of data collection. Fixed-time equivalents of each staff were estimated. Data on services provided and other demographic details of the population covered were collected from routine monthly reports and respective service registers.
Data analysis: Shared resources were apportioned to outpatient and inpatient care, and to various contributing departments. The joint or shared costs for drugs, consumables, diagnostics and overheads were apportioned at two levels i.e. various departments and between outpatient and inpatient care. For the former, the proportion of patients reported was used for various specialities to allocate the joint costs. In case of allocation between outpatient and inpatient care, the average proportional time allocation of the human resources in the given department was used. In the specific case of electricity and sanitation costs, proportional floor area used for particular services to apportion joint costs was considered. Equivalent annualized cost was computed for each capital item which was based on the life of equipment and a discount rate of 3 per cent. Replacement cost was used instead of original cost. In terms of cost of space, rental price and floor area of space were used to assess the opportunity cost.
Unit costs: Unit costs for outpatient care (per patient OPD visit) and inpatient care (per bed-day hospitalization) were estimated for each speciality. Since the capacity utilization varied across the sites, we standardized the costs using bed occupancy as the indicator for capacity utilization10. The costs were considered under heads of human resource, drugs and consumables, laboratory and utilities while adjusting for capacity utilization. Costs not sensitive to capacity utilization i.e. capital costs, medical equipment and other non-medical items (such as furniture and air-conditioners) were not adjusted. Finally, the population of the district was used as the denominator to estimate the per-capita cost of provision of secondary health care services through public sector district hospitals. All costs were converted to 2012 prices and monthly average for conversion of Indian Rupees ( ) to US Dollar (USD) was used to report the costs in USD (1 USD=
) to US Dollar (USD) was used to report the costs in USD (1 USD= 54.4).
54.4).
Sensitivity analysis: A univariate sensitivity analysis was done wherein the base value of salaries, price of equipment, building cost, rental prices and assumptions on time allocation varied by 25 per cent on either side. Prices of drugs and consumables showed wide variation; hence, we varied these by 100 per cent on either side. Second, a probabilistic sensitivity analysis was done to assess the effect of joint uncertainty on unit costs and to compute 95 per cent confidence interval (CI) of unit cost estimates. Using Monte-Carlo method, the unit cost was simulated over 1000 times. A uniform distribution was assumed to randomly select one price assumption for each simulation. The distribution of simulated unit costs was used to compute median, 2.5th and 97.5th percentiles12.
The study was approved by the Ethics Committee of the Post Graduate Institute of Medical Education and Research, Chandigarh, India. Administrative approval was taken from the Department of Health of respective State Governments; Civil Surgeons of respective districts and the in-charge medical officer of each district hospital. Written informed consent was taken from participants to interview staff for time allocation.
Results
A total of five district hospitals were covered in the two States: Panchkula, Jhajjar and Rohtak districts in Haryana and Sangrur and Ropar districts in Punjab. While the annual outpatient attendance ranged from 169,314 in Ropar to 526,508 in Panchkula, the number of inpatient hospitalizations varied from 12,391 in Ropar to 31,799 in Panchkula (Table I). The bed-occupancy rate reported ranged between 59 per cent in Rohtak and 116 per cent in Sangrur.
Annual costs: The median annual cost for providing the gamut of secondary health care services in the study hospitals was  114.4 million (2.5th - 97.5th percentile; 94-138). While the total capital cost was
114.4 million (2.5th - 97.5th percentile; 94-138). While the total capital cost was  17.1 million (7.3-29.9), recurrent cost was
17.1 million (7.3-29.9), recurrent cost was  97.4 million (86.6-107.7) (Table II). Human resources accounted for 53 per cent of the overall costs, while drugs, consumables and building, and grants accounted for 14 and 10 per cent, respectively. The sensitivity analysis showed that annual cost was most sensitive to variation in prices of drugs and consumables (Figure).
97.4 million (86.6-107.7) (Table II). Human resources accounted for 53 per cent of the overall costs, while drugs, consumables and building, and grants accounted for 14 and 10 per cent, respectively. The sensitivity analysis showed that annual cost was most sensitive to variation in prices of drugs and consumables (Figure).
Table II.
Annual cost of delivering secondary health care services at public sector district hospitals in north India
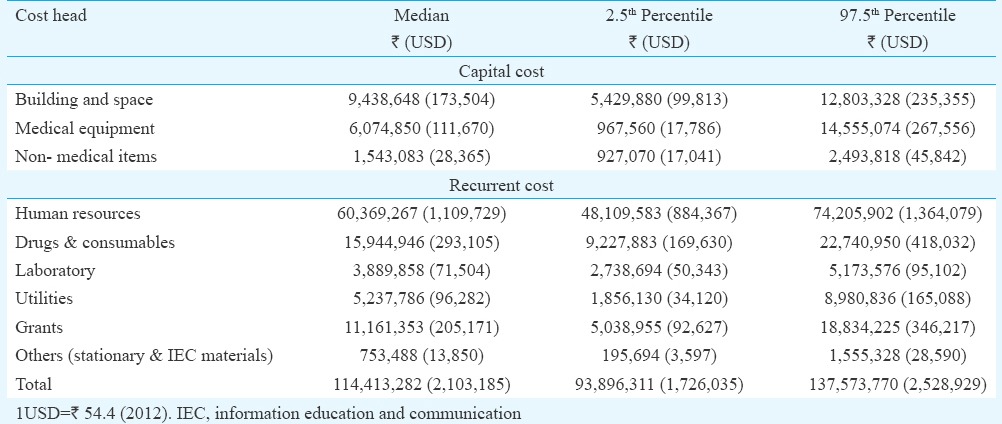
Figure.
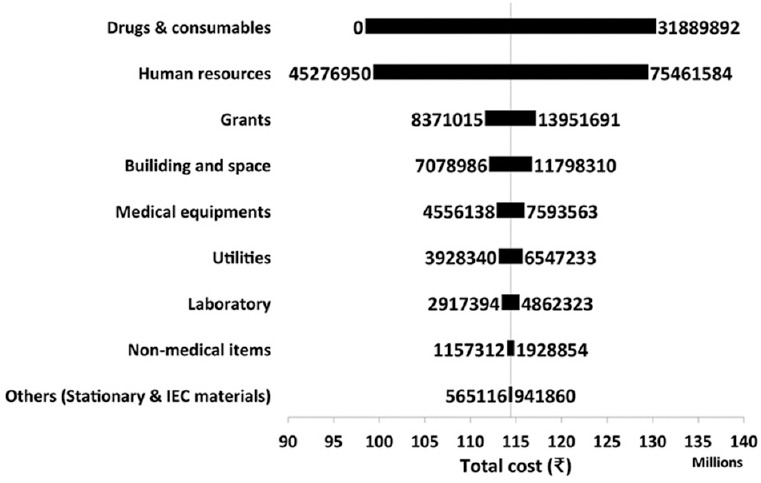
Sensitivity of estimated annual cost to variation in prices of resources.
Unit costs: The cost of providing services at district hospital was  844 (665-1074) per bed-day hospitalization,
844 (665-1074) per bed-day hospitalization,  3481 (1169-5681) per surgery and
3481 (1169-5681) per surgery and  170 (128-222) per outpatient visit (Table III). The standardized unit costs were
170 (128-222) per outpatient visit (Table III). The standardized unit costs were  834 per bed-day,
834 per bed-day,  3439 per case operated and
3439 per case operated and  168 per outpatient visit at 100 per cent capacity utilization (Table III). The variation in costs between hospitals is shown in Table IV. There was also a significant variation among the various specialties for unit cost of outpatient and inpatient services. In case of inpatient admission, the cost ranged from
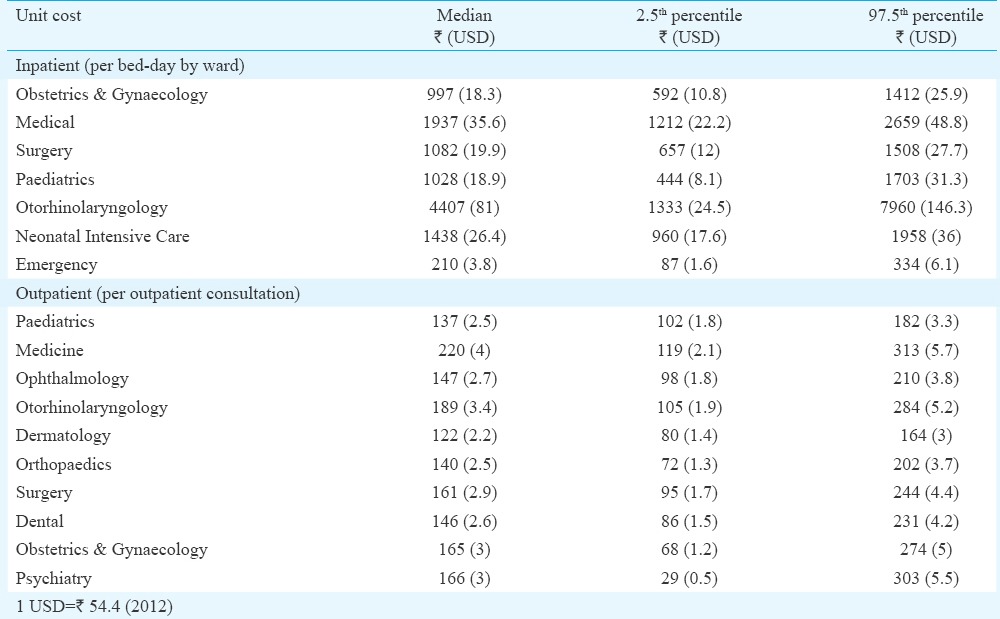
168 per outpatient visit at 100 per cent capacity utilization (Table III). The variation in costs between hospitals is shown in Table IV. There was also a significant variation among the various specialties for unit cost of outpatient and inpatient services. In case of inpatient admission, the cost ranged from  210 per bed-day in emergency ward and
210 per bed-day in emergency ward and  4407 per bed-day in otorhinolaryngology. In case of an outpatient consultation, the unit cost ranged from
4407 per bed-day in otorhinolaryngology. In case of an outpatient consultation, the unit cost ranged from  122 in dermatology to
122 in dermatology to  220 in medicine (Table V).
220 in medicine (Table V).
Table III.
Unit cost of provision of health care services delivered at public sector district hospitals in India
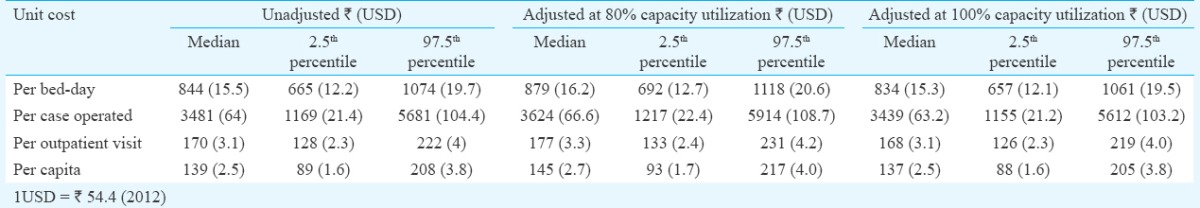
Table IV.
Hospital-wise unit cost of provision of healthcare services in India
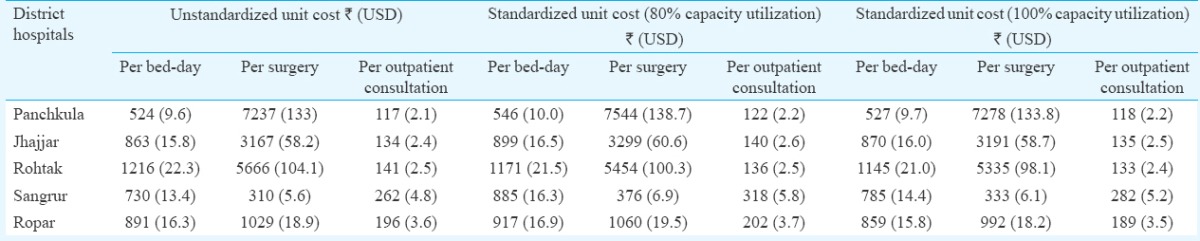
Table V.
Specialty-wise unit cost for outpatient consultation and inpatient bed-day in public sector district hospitals of north India
Per-capita costs: At the population level, per-capita cost of providing secondary care health care services in India through public sector district hospitals in north India was  139 (2.5th - 97.5th percentile 89-208) (Table III).
139 (2.5th - 97.5th percentile 89-208) (Table III).
Discussion
District hospitals in public sector form the core facility for provision of secondary health services in India. While detailed analysis of cost of provision of primary health care services through community health workers is available13,14, the evidence base for cost of provision of secondary-level health care through district hospitals is weak.
Our estimates of unit costs for inpatient bed-day, operating cost and outpatient visit were comparable to that reported earlier8. Adjusting for inflation over the intervening years at the rate of 8.23 per cent from the year of reporting, the cost of outpatient consultation was reported to be USD 2.45 by Chatterjee et al8 and USD 3.6 by WHO-CHOICE study for South East Asia Region4. In the WHO-CHOICE, inpatient unit costs are estimated per hospital bed-day and represent only the ‘hotel’ component of hospital costs i.e. excluding the cost of drugs and diagnostic tests but including costs such as personnel, capital and food costs. Similarly, outpatient unit costs represent the estimated cost per outpatient visit and include all cost components, except drugs and diagnostics. Human resources, and drugs and consumables accounted for 53 and 14 per cent, respectively, of the overall costs in our study, similar to 52.6 and 21.8 per cent observed in PHC, and 58.9 and 11.3 per cent respectively in CHC, in our earlier study15. Mahapatra and Berman16 found the cost of inpatient care as USD 17.4 per bed-day. However, this study was undertaken in 1989-1990 and many changes in health care delivery infrastructure, prices, patient profile and treatment-seeking behaviour have taken place since then. In terms of cost of specialities, our estimates for newborn intensive care ( 1438 per bed-day) were similar to
1438 per bed-day) were similar to  889 reported in 2010 in our previous study which included four Special Newborn Care Units in district hospitals covering three Indian States6. This could be due to the different setting in which the study was undertaken.
889 reported in 2010 in our previous study which included four Special Newborn Care Units in district hospitals covering three Indian States6. This could be due to the different setting in which the study was undertaken.
Significant variation in cost among various specialities was observed in our study. Fixed allocation of number of beds to various specialities despite a low bed occupancy rate could explain the high costs of otorhinolaryngology. In the outpatient medicine department, in addition to higher resource allocation, it served as first point of contact for all patients prior to being referred to any speciality which could explain higher unit cost. The unit costs in dermatology outpatient department were particularly low. This could be attributed to higher patient loads. Many studies have shown beneficial effects of interventions on increasing the public sector utilization of maternal health care services17,18,19.
The required cost of universal health care (UHC) delivery through the existing mix of public and private health institutions has been reported to be  1713 (USD 38, 95% CI USD 18-73) per person per annum in India20. In this context, the present study's per-capita cost of
1713 (USD 38, 95% CI USD 18-73) per person per annum in India20. In this context, the present study's per-capita cost of  139 for the provision of curative care in district hospitals showed that investment in public facilities for provision of curative care should be increased if India envisages achieving UHC20,21. In per capita terms, the public expenditure on health in the country has nearly doubled in the period from
139 for the provision of curative care in district hospitals showed that investment in public facilities for provision of curative care should be increased if India envisages achieving UHC20,21. In per capita terms, the public expenditure on health in the country has nearly doubled in the period from  263 in 2004-2005 to
263 in 2004-2005 to  486 in 2010-2011 in constant terms (2004-2005 prices) and
486 in 2010-2011 in constant terms (2004-2005 prices) and  960 per-capita in real terms (no adjustment)22. However, this increase has mostly occurred for reproductive and child health services under the National Health Mission (NHM). Hence, there is a need for a broader focus of investment in health care which involves a comprehensive primary care which is well integrated with secondary care.
960 per-capita in real terms (no adjustment)22. However, this increase has mostly occurred for reproductive and child health services under the National Health Mission (NHM). Hence, there is a need for a broader focus of investment in health care which involves a comprehensive primary care which is well integrated with secondary care.
Our study findings point to an imperative need to improve hospital efficiency. Two factors appear important in explaining inefficiencies. First, majority of the supply-side health system spending occurs on account of paying salaries. Moreover, little is left to meet other recurrent resource needs which are required for service delivery, for example, drugs and diagnostics23. As a result, there is a need to reorient health system spending by ensuring a minimum threshold spending on drugs. Evidence from Tamil Nadu and Bihar suggested that improving access to medicines in public sector facilities improved the patient attendance in public sector facilities significantly24. On the contrary, findings from a recent study show that the only about half of the essential medicines are available in public sector hospitals in Punjab and Haryana25.
The capital cost accounted for just about one-sixth of the total cost of care8,26,27. However, there is a significant variation in capital cost among different hospitals, ranging from  3.4 to 29.3 million, which is associated with scale of operation. This implies that increases in service utilization will have to be matched with commensurate increase in capital infrastructure.
3.4 to 29.3 million, which is associated with scale of operation. This implies that increases in service utilization will have to be matched with commensurate increase in capital infrastructure.
Findings of our study could be used to revise the existing estimates and pay providers under these schemes, and estimates on cost could be used to undertake further analysis. These could help in doing cost-effectiveness analysis of various health services28.
Our study had certain limitations. First, there are wide variations in health care delivery infrastructure in various parts of India. Hence, it is recommended to undertake a study with a bigger and more representative sample from multiple States of India to generalize the findings. Second, we did not undertake a time-motion study to assess time contribution of staff performing multiple tasks. However, omission of a detailed time-motion study and application of methods used in our study have been justified in other studies6,13,14. Third, it was important to highlight that for a number of services, resources were available at pooled hospital level only. We used standard apportioning techniques which are recommended elsewhere10. Hospital management information system systems should provide disaggregated data to help determine specific speciality costs in a more robust manner in future studies. Fourth, our estimates of cost are reflective of the current level of infrastructure and services delivered. However, these may not be completely representative of costs in an ideal scenario as envisaged by the Indian Public Health Standards2. For example, the overall number of human resources and the mix of staff were not exactly as per recommendations. Similarly, these hospitals may not have had the desired set of all medicines available throughout the year. In a study done during the similar period, it was reported that 47.8 per cent of the basket of medicines were available in public sector district hospitals in Punjab25. In another study from Punjab State, a shortage of medicines was pointed out which led to high out-of-pocket (OOP) expenditures for patients29. Our estimates on cost of care have not accounted for the OOP expenditures which people incur in public sector hospitals. However, there is abundant evidence available on the extent of OOP in public sector hospitals of north India29,30,31,32.
In conclusion, our study provided detailed estimates of cost of provision of secondary-level health care services delivered through public sector district hospitals in north India. These estimates can be used for evidence-based scale-up of curative secondary care services and refining provider payment rates under health insurance schemes. Our study estimates on cost can be used for further economic research such as undertaking cost-effectiveness analysis of secondary health care services, disease-specific health accounts and benefit-incidence analysis to evaluate the distributional benefits of public subsidy.
Acknowledgment
Authors acknowledge Post Graduate Institute of Medical Education and Research, Chandigarh, India, for financial support.
Footnotes
Conflicts of Interest: None.
References
- 1.Rural Health Statistics 2012. New Delhi: Ministry of Health and Family Welfare Government of India; 2013. [Google Scholar]
- 2.New Delhi: Ministry of Health and Family Welfare, Government of India; 2012. Indian Public Health Standards (IPHS) Guidelines for District Hospitals (101 to 500 Bedded) Revised 2012. [Google Scholar]
- 3.New Delhi: PHFI; 2011. Public Health Foundation of India. A Critical Assessment of the Existing Health Insurance Models in India. [Google Scholar]
- 4.Geneva: WHO; 2005. [accessed on December 7, 2015]. World Health Organization. CHOosing Interventions that are Cost-Effective (WHO-CHOICE): Results for Unit Costs for Patient Services for 14 GBD Regions. Available from: http://www.who.int/choice/costs/unit_regions/en/ [Google Scholar]
- 5.Krishnan A, Arora NK, Pandav CS, Kapoor SK. Cost of curative pediatric services in a public sector setting. Indian J Pediatr. 2005;72:657–60. doi: 10.1007/BF02724072. [DOI] [PubMed] [Google Scholar]
- 6.Prinja S, Manchanda N, Mohan P, Gupta G, Sethy G, Sen A, et al. Cost of neonatal intensive care delivered through district level public hospitals in India. Indian Pediatr. 2013;50:839–46. doi: 10.1007/s13312-013-0234-6. [DOI] [PubMed] [Google Scholar]
- 7.Prinja S, Manchanda N, Aggarwal AK, Kaur M, Jeet G, Kumar R. Cost & efficiency evaluation of a publicly financed & publicly delivered referral transport service model in three districts of Haryana State, India. Indian J Med Res. 2013;138:1003–11. [PMC free article] [PubMed] [Google Scholar]
- 8.Chatterjee S, Levin C, Laxminarayan R. Unit cost of medical services at different hospitals in India. PLoS One. 2013;8:e69728. doi: 10.1371/journal.pone.0069728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Rural Health Mission, Government of India. State PIP Budget 2012-13. [accessed on April 30, 2014]. Available from: http://www.nrhm.gov.in/nrhm-in-state/state-program-implementation-plans-pips.html .
- 10.Fox-Rushby J, Cairns J. Economic evaluation. London: Oxford University Press; 2006. [Google Scholar]
- 11.Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: Bottom-up and top-down. Health Econ. 2009;18:1188–201. doi: 10.1002/hec.1422. [DOI] [PubMed] [Google Scholar]
- 12.Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach. Med Decis Making. 1985;5:157–77. doi: 10.1177/0272989X8500500205. [DOI] [PubMed] [Google Scholar]
- 13.Prinja S, Jeet G, Verma R, Kumar D, Bahuguna P, Kaur M, et al. Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS One. 2014;9:e91781. doi: 10.1371/journal.pone.0091781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prinja S, Mazumder S, Taneja S, Bahuguna P, Bhandari N, Mohan P, et al. Cost of delivering child health care through community level health workers: How much extra does IMNCI program cost? J Trop Pediatr. 2013;59:489–95. doi: 10.1093/tropej/fmt057. [DOI] [PubMed] [Google Scholar]
- 15.Prinja S, Gupta A, Verma R, Bahuguna P, Kumar D, Kaur M, et al. Cost of delivering health care services in public sector primary and community health centres in north India. PloS One. 2016;11:e0160986. doi: 10.1371/journal.pone.0160986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahapatra P, Berman P. Resource allocation for public hospitals in Andhra Pradesh, India. Health Policy Plan. 1995;10:29–39. doi: 10.1093/heapol/10.1.29. [DOI] [PubMed] [Google Scholar]
- 17.Prinja S, Jeet G, Kaur M, Aggarwal AK, Manchanda N, Kumar R. Impact of referral transport system on institutional deliveries in Haryana, India. Indian J Med Res. 2014;139:883–91. [PMC free article] [PubMed] [Google Scholar]
- 18.Tripathi N, Saini SK, Prinja S. Impact of Janani Shishu Suraksha Karyakram on out-of-pocket expenditure among urban slum dwellers in Northern India. Indian Pediatr. 2014;51:475–7. doi: 10.1007/s13312-014-0430-z. [DOI] [PubMed] [Google Scholar]
- 19.Prinja S, Bahuguna P, Gupta R, Sharma A, Rana SK, Kumar R. Coverage and financial risk protection for institutional delivery: How universal is provision of maternal health care in India? PLoS One. 2015;10:e0137315. doi: 10.1371/journal.pone.0137315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal health care in India: A model based estimate. PLoS One. 2012;7:e30362. doi: 10.1371/journal.pone.0030362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prinja S, Gupta R, Bahuguna P, Sharma A, Kumar Aggarwal A, Phogat A, et al. A composite indicator to measure universal health care coverage in India: Way forward for post-2015 health system performance monitoring framework. Health Policy Plan. 2017;32:43–56. doi: 10.1093/heapol/czw097. [DOI] [PubMed] [Google Scholar]
- 22.Choudhury M, Nath H. An Estimate of Public Expenditure on Health in India. New Delhi: National Institute of Public Finance and Policy; 2013. [Google Scholar]
- 23.Kumar R, Tripathy JP, Singh N, Kaur M, Prinja S, Lakshmi PVM, et al. Rapid assessment of health services in Punjab using a mixed method approach. Indian J Community Health. 2015;27:197–203. [Google Scholar]
- 24.Chokshi M, Farooqui HH, Selvaraj S, Kumar P. A cross-sectional survey of the models in Bihar and Tamil Nadu, India for pooled procurement of medicines. WHO South East Asia J Public Health. 2015;4:78–85. doi: 10.4103/2224-3151.206625. [DOI] [PubMed] [Google Scholar]
- 25.Prinja S, Bahuguna P, Tripathy JP, Kumar R. Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacol Toxicol. 2015;16:43. doi: 10.1186/s40360-015-0043-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prinja S, Bahuguna P, Duseja A, Kaur M, Chawla YK. Cost of intensive care treatment for liver disorders at tertiary care level in India. PharmacoEconomics-Open. 2017:1–12. doi: 10.1007/s41669-017-0041-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sangwan A, Prinja S, Aggarwal S, Jagnoor J, Bahuguna P, Ivers R. Cost of Trauma Care in Secondary-and Tertiary-Care Public Sector Hospitals in North India. Appl Health Econ Health Policy. 2017:1–12. doi: 10.1007/s40258-017-0329-7. [DOI] [PubMed] [Google Scholar]
- 28.Prinja S, Bahuguna P, Faujdar DS, Jyani G, Srinivasan R, Ghoshal S, et al. Cost-effectiveness of human papillomavirus vaccination for adolescent girls in Punjab state: Implications for India's universal immunization program. Cancer. 2017;123:3253–60. doi: 10.1002/cncr.30734. [DOI] [PubMed] [Google Scholar]
- 29.Prinja S, Kanavos P, Kumar R. Health care inequities in north India: Role of public sector in universalizing health care. Indian J Med Res. 2012;136:421–31. [PMC free article] [PubMed] [Google Scholar]
- 30.Prinja S, Aggarwal AK, Kumar R, Kanavos P. User charges in health care: Evidence of effect on service utilization & equity from North India. Indian J Med Res. 2012;136:868–76. [PMC free article] [PubMed] [Google Scholar]
- 31.Balasubramanian D, Prinja S, Aggarwal AK. Effect of user charges on secondary level surgical care utilization and out-of-pocket expenditures in Haryana State, India. PLoS One. 2015;10:e0125202. doi: 10.1371/journal.pone.0125202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.New Delhi: NSSO, Ministry of Statistics and Program Implementation; 2015. National Sample Survey Organization. Social Consumption in India: Health NSS 71st Round (January-June 2014) [Google Scholar]


