Abstract
Background
Studies on postpartum depression (PPD) in China have focused primarily on women of Han ethnicity, whereas work on other ethnic groups has proven limited. This study explored the ethnic differences of associated social-demographic and obstetric factors for PPD between Han-majority and Kazak-minority women in northwestern China.
Methods
Han and Kazak women who received routine examinations at four hospitals in a multi-ethnic area of China six weeks after childbirth between March 2016 and December 2016 were included in the study. Data on the women’s socio-demographic characteristics, obstetric factors, and possible depression at six weeks after childbirth were collected. We examined the associated factors of PPD using multivariable logistic regression analyses by ethnic group.
Results
The overall incidence of PPD was 14.6% (184/1,263) at six weeks after childbirth. PPD was detected more frequently among Kazak (16.1%) than Han women (13.1%). Kazak women exhibited a higher risk of PPD (adjusted OR = 1.561, 95% CI [1.108–2.198], P = 0.011). Urinary incontinence (UI) represented a significant risk factor of PPD for Kazak compared with Han women (OR = 1.720, 95% CI [1.056–2.804], P = 0.003). In contrast, the presence of the mother-in-law as a caregiver after childbirth demonstrated a positive association with PPD among Han (OR = 2.600, 95% CI [1.499–4.512], P = 0.001), but not with Kazak women.
Conclusions
Kazak women were more likely to develop PPD than Han women, even after controlling for confounders. Moreover, distinct risk factors for PPD existed for Han and Kazak women. Future research that explores the relationships between Han women and their mothers-in-law as well as Kazak women’s attitudes toward UI could help us further understand PPD in these populations.
Keywords: Postpartum depression, Health status disparities, Urinary incontinence, Risk factors, Race
Introduction
Postpartum depression (PPD) is a common psychological problem that affects as many as 13–19% of women (O’Hara & McCabe, 2013). Generally, PPD occurs within the first four weeks after delivery (Gao et al., 2016), causing significant distress for the parents and adverse effects on the healthy development of their offspring. The pathogenesis of PPD is unknown, but psycho-social predictors, such as depression history, antenatal depression or anxiety, poor social support, marital dissatisfaction, and stressful life events, have been widely demonstrated by multiple meta-analyses (Beck, 2001; Robertson et al., 2004; O’Hara & Swain, 1996), while the contribution of social-demographic and obstetric factors differs by ethnicity and culture (Liu & Tronick, 2013; Wei et al., 2008).
Most research in China has focused on the largest ethnic group in China—the Han—whereas studies devoted to other ethnic groups are limited (Yan et al., 2015; Yang et al., 2015). Xinjiang, an area that is less developed in comparison to the Central and Eastern regions, is located in the northwest corner of China. The region is populated by a variety of ethnicities. The Kazaks, one of the largest minorities, has a population of 1.25 million (approximately 6.5% of the total population in Xinjiang province) according to the 2010 census; and the proportion for Kazaks is 6.5% (8.74 million) (Li et al., 2015). A considerable number of Kazaks are nomadic. Consequently, they have less access to medical resources. Postpartum mental health of Kazak women had not been documented.
This study was designed to observe and compare the incidence of and social-demographic and obstetric factors associated with PPD among Han and Kazak women. We hypothesized that social-demographic and obstetric factors are related to the development of PPD. The purpose of this study was to add information to the data on the risk profile of PPD by considering different ethnicities and cultures. In addition, we expected to alert scholars and medical practitioners to the health of minority females in Xinjiang, China, an economically underdeveloped region.
Materials and Methods
Ethics statement
Ethics approval for the study was granted by the Ethics Committee of the First Affiliated Hospital of Medicine College, Shihezi University (2015-134-01). All participants provided written informed consent.
Estimation of sample size
Since the effect size of the difference between the PPD incidents of Han and Kazak ethnicity was unavailable in existing literature, the estimation of sample size was based on the standard practice of 1 variable per 10 events criterion for a binary logistic regression analysis (Rao, 2005). We took two steps to decide which risk factors to include in the present study. The first step was based on a comprehensive review of the literature (Fritel et al., 2016; Klainin & Arthur, 2009; Liu & Tronick, 2013; Templeton et al., 2003; Zaidi et al., 2017). Then, a focus group discussion with one obstetrician, two midwives, two practice nurses, and one psychiatrist was undertaken to explore their opinions based on the literature. We expected a total number of 16 possible candidate predictors for PPD based on the literature review conducted and consultation with clinical experts, which were age, race/ethnicity, religion, income, employment, parity, level of education, smoking, drinking, previous pregnancy loss, unplanned pregnancy, mode of delivery, infant gender, infant feeding, postpartum urinary incontinence (UI), and type of caregiver after childbirth. As no previous work in Kazak women had been undertaken, the estimate for the incidence of PPD was based on previous research among Chinese women, which is approximately 15% (Wan et al., 2009), the estimated sample size was 16 × 10/15% = 1,067. Considering the possibility of a negative response rate of 20%, the estimate of a final sample size was 1,334. To examine differences in incidence and associated factors of PPD between the Han and Kazak women, the study sample sought to represent an equal number of Han and Kazak participants.
Participants
Purposive convenience sampling was employed to recruit participants. Women who visited obstetric clinics of four hospitals in Xinjiang province at six weeks postpartum were recruited consecutively between March 2016 and December 2016, with no compensation or honoraria. One of the four clinics was located in an area inhabited primarily by Hans, two of four clinics were located in an area inhabited by an approximately equal number of Han and Kazak women, and the remaining clinic was located in an area inhabited mainly by Kazaks. Access to medical care did not differ for the women with different lifestyles and cultural practices. Han and Kazak women were approached in the clinic waiting room by trained investigators. If interested, they were offered verbal and written information about the study. Women who provided written informed consent and were able to easily communicate with the investigators were asked to attend a face-to-face interview at the clinic immediately before or after their scheduled check. Women with a family history of mental illness or who had experienced mental disorders before or during pregnancy were excluded. A woman was deemed to have experienced a mental disorder if her answer was affirmative to one or both of the following questions: Have you ever seen a psychiatrist or psychologist before or during pregnancy? Have you ever taken antidepressants, anxiolytics or benzodiazepines before or during pregnancy? Women who provided incomplete/missing information, such refusal to give a response to one or more of the interviewer’s question, or did not remain throughout the duration of the investigation, were excluded.
Data collection
An interview was conducted to obtain socio-demographic characteristics (ethnicity, age, religious faith, education, employment situation, household income per month, type of caregivers following childbirth, whether or not the pregnancy was planned), health-related behaviors (history of smoking and drinking), and obstetric factors (parity, previous pregnancy loss, mode of delivery on this occasion, infant gender, infant feeding, experience or not of UI after childbirth), and PPD. Most of the research was conducted by nurses whose mother tongue was Chinese. For the small number of Kazak women who could not understand and/or speak Chinese, assistance was provided by Kazak nurses.
Definitions and descriptions of variables
The data collected on the different variables relied primarily on self-reported responses. Religious faith was defined as following or believing in the basic tenets of a major religion, such as Islam, Buddhism, or Christianity. Participants could choose between (1) religious faith and (2) no religious belief. Education level was separated into either (1) primary school or less or, (2) middle school or above. Participants were asked if they had steady employment or not. Steady employment was defined as full-time work eight months or more a year. Possible responses to the question about monthly household income was either 2,000 yuan (300 USD) or more or less than 2,000 yuan (300 USD). History of smoking was defined as more than one cigarette daily for more than six months and drinking was defined as equal or more than 50 ml daily or 500 ml weekly for more than 6 months. Previous pregnancy loss was defined as having a lost or terminated pregnancy, including miscarriage, induced abortion, or stillbirth. The existence of UI was self-reported involuntary urinary leakage after childbirth.
Postpartum depression was determined by the Chinese translation of the Edinburgh Postnatal Depression Scale (EPDS). The scale is comprised of 10 questions that help to identify common symptoms of depression. Each item had four grades that were scored from 0 to 3 according to the severity of symptoms; The total score ranged from 0 to 30. An EPDS score of 13 or above indicated PPD; the scale demonstrated good reliability among Chinese women (validity, 0.79; Cronbach’s α coefficient, 0.87) (Heh, 2001).
Data analysis
The distributions of associated risk factors were calculated as means for age and as proportions for the other variables. Characteristics were further stratified and tested for differences by ethnic group using the two-sided Student’s t-test for age, and the χ2 test for the rest variables. The statistical models assumed that the errors were a binomial distribution, and that significance could be determined by using a likelihood ratio. Multivariable logistic regression analysis of maximum likelihood estimation (forward stepwise) with PPD as a dependent variable, was performed to analyze the main effect of ethnicity after adjusting for potential confounders addressed in this study. To evaluate the associated factors of PPD for different ethnic groups, we estimated the factors’ effects on PPD using multivariable logistic regression stratified by ethnicity. Statistical processing was conducted using SPSS 13.0. A P-value of 0.05 or less was considered to be statistically significant.
Results
Social-demographic and obstetric characteristics of the women
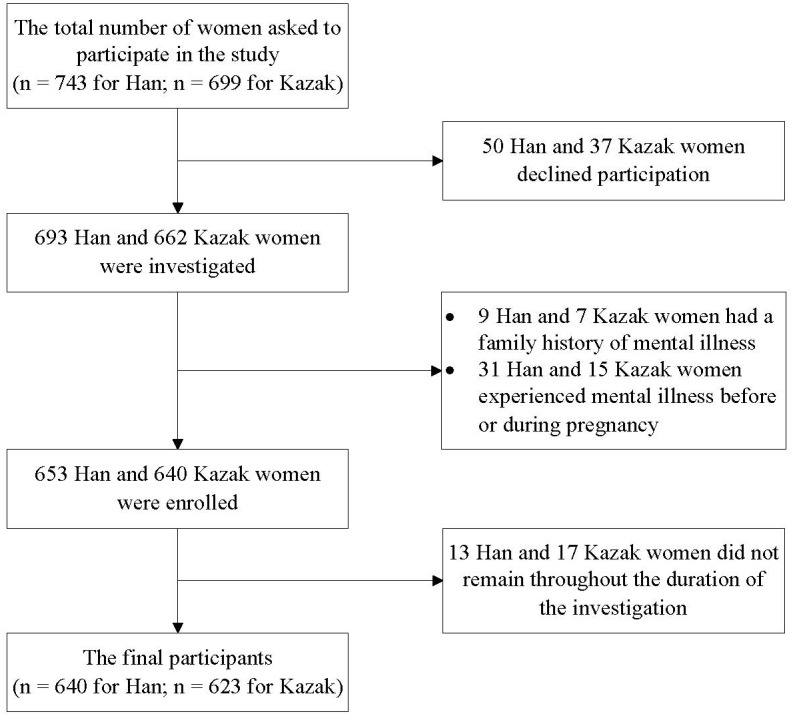
A total of 1,442 women were invited to participate. Of those women, 87 (6.0%) declined to participate. The percentage that declined did not vary by ethnic group (50 women (6.7%) for Han and 37 women (5.3%) for Kazak, P > 0.05). Of the 1,355 women interviewed, 16 (1.2%) of them had a family history (nine women (1.3%) for Han and seven women (1.1%) for Kazak, P = 0.681); 46 (3.4%) of them experienced mental illness before or during pregnancy (31 women (4.5%) for Han and 15 women (2.3%) for Kazak, P = 0.025). An additional 30 (2.3%) women were excluded because they did not remain throughout the duration of the investigation. A total of 1,263 women (640 Han and 623 Kazak) were ultimately included in the study. They had a mean age of 28.32 (±5.00) years. The recruitment process is illustrated in Fig. 1.
Figure 1. The flowchart of recruitment of women for this study.
A significantly higher percentage of the Kazak were religious compared to the Han women (99.0% vs. 8.4%). The percentage of women with a middle school or above education, steady employment, and a monthly household income of more than 2,000 yuan (300 USD)/month was lower among the Kazak (26.0%, 21.7%, and 34.5%, respectively) than the Han (33.9%, 58.1%, and 92.2%, respectively). More Han women were nulliparous (67.2%), preferred cesarean section (48.9%), and received care from their mothers-in-law after childbirth (48.8%), compared to Kazak women (31.9%, 34.2%, and 24.6%, respectively) (Table 1).
Table 1. Comparisons of socio-demographic and obstetric variables by ethnicity.
| Overall (n= 1,263) | Han women (n = 640) | Kazak women (n = 623) | t/χ2 | P | |
|---|---|---|---|---|---|
| Age (y) (mean ± SD) | 28.32 ± 5.00 | 27.98 ± 4.99 | 28.68 ± 4.99 | 2.467b | 0.014 |
| Religion (yes) n (%) | 671 (53.1) | 54 (8.4) | 617 (99.0) | 1040.586c | <0.001 |
| None/primary education n (%) | 678 (53.7) | 217 (33.9) | 461 (74.0) | 204.066c | <0.001 |
| Stable employment n (%) | 507 (40.1) | 372 (58.1) | 135 (21.7) | 174.611c | <0.001 |
| Household income ≤ 2,000 yuan (300 USD)/month n (%) | 458 (36.3) | 50 (7.8) | 408 (65.5) | 454.377c | <0.001 |
| Smoking history n (%) | 54 (4.3) | 20 (3.1) | 34 (5.5) | 4.196c | 0.041 |
| Drinking history n (%) | 79 (6.3) | 60 (9.4) | 19 (3.0) | 21.540c | <0.001 |
| Previous pregnancy loss n (%) | 314 (24.9) | 154 (24.1) | 160 (25.7) | 0.443c | 0.506 |
| Multiparous n (%) | 634 (50.2) | 210 (32.8) | 424 (68.1) | 156.868c | <0.001 |
| Unplanned pregnancy n (%) | 265 (21.0) | 144 (22.5) | 121 (19.4) | 1.804c | 0.179 |
| Cesarean section n (%) | 526 (41.6) | 313 (48.9) | 213 (34.2) | 28.135c | <0.001 |
| Female infant n (%) | 576 (45.6) | 300 (46.9) | 276 (44.3) | 0.843c | 0.359 |
| Mother-in-law as caregiver after childbirthan (%) | 465 (36.8) | 312 (48.8) | 153 (24.6) | 79.421c | <0.001 |
| Breast-feeding n (%) | 960 (76.0) | 444 (69.4) | 516 (82.8) | 31.319c | <0.001 |
| Postpartum UI n (%) | 315 (24.9) | 150 (23.4) | 165 (26.5) | 1.566c | 0.211 |
| PPD n (%) | 184 (14.6) | 84 (13.1) | 100 (16.1) | 2.172c | 0.141 |
Notes.
All other caregivers as the reference category.
t.
χ2.
- UI
- urinary incontinence
- PPD
- postpartum depression
Multivariable logistic regression analysis for the association of ethnicity and PPD
The overall incidence of PPD was 14.6% (184/1,263) at six weeks after childbirth. PPD was detected more frequently among Kazak women (16.1%) than Han women (13.1%). Kazak women exhibited a higher risk of PPD than Han women (OR = 1.561, 95% CI [1.108–2.198], P = 0.011) after controlling for previous pregnancy loss, unplanned pregnancy, mother-in-law as a caregiver after childbirth, infant gender, and postpartum UI (Table 2).
Table 2. Multivariable logistic regression analysis of the risk factors for PPD.
| β coefficient | P | OR | 95% CI | |
|---|---|---|---|---|
| Kazaka | 0.445 | 0.011 | 1.561b | 1.108–2.198 |
| Previous pregnancy loss | 0.661 | <0.001 | 1.937 | 1.362–2.755 |
| Unplanned pregnancy | 0.792 | <0.001 | 2.207 | 1.549–3.146 |
| Mother-in-law as caregiver after childbirth | 0.653 | <0.001 | 1.921 | 1.343–2.746 |
| Female infant | 0.605 | 0.001 | 1.832 | 1.302–2.578 |
| Postpartum UI | 0.386 | 0.037 | 1.471 | 1.024–2.115 |
Notes.
Han as the reference category.
Adjusted for previous pregnancy loss, unplanned pregnancy, caregiver after childbirth, infant gender, and urinary incontinence.
- PPD
- postpartum depression
- OR
- odds ratio
- CI
- confidence interval
- UI
- urinary incontinence
Multivariable analyses of the associated factors of PPD by ethnic group
Significant risk factors for PPD were previous pregnancy loss, unplanned pregnancy, and female infant. For both ethnic groups they were not different. However, the mother-in-law as a caregiver after childbirth was strongly associated with PPD for the Han women but not for the Kazak women (OR = 2.600, 95% CI [1.499–4.512], P = 0.001). In contrast, postpartum UI was a significant risk factor for PPD for the Kazak women yet not for the Han women (OR = 1.720, 95% CI [1.056–2.804], P = 0.003) (Table 3).
Table 3. Multivariable logistic regression analyses of the risk factors for PPD stratified by ethnic group.
| Han women | Kazak women | |||||||
|---|---|---|---|---|---|---|---|---|
| β coefficient | P | OR | 95% CI | β coefficient | P | OR | 95% CI | |
| Mother-in-law as caregiver after childbirth | 0.956 | 0.001 | 2.600 | 1.499–4.512 | – | – | – | – |
| Previous pregnancy loss | 0.609 | 0.021 | 1.839 | 1.096–3.087 | 0.635 | 0.010 | 1.888 | 1.163–3.063 |
| Unplanned pregnancy | 0.818 | 0.001 | 2.267 | 1.368–3.756 | 0.646 | 0.011 | 1.907 | 1.158–3.142 |
| Female infant | 0.547 | 0.043 | 1.728 | 1.018–2.933 | 0.661 | 0.004 | 1.936 | 1.236–3.033 |
| Postpartum UI | – | – | – | – | 0.542 | 0.030 | 1.720 | 1.056–2.804 |
| Intercept | −3.160 | −2.505 | ||||||
Notes.
- PPD
- postpartum depression
- OR
- odds ratio
- CI
- confidence interval
- UI
- urinary incontinence
Discussion
The present study represents the first work to investigate and compare the incidence and associated risk factors for PPD among Han and Kazak women in a less-developed region in northwestern China. The incidence of PPD among Han women was consistent with results from an epidemiological survey conducted in Mainland China (Wan et al., 2009) and a literature review of studies conducted in Asian countries that revealed a range from 3.5% to 63.3% (Klainin & Arthur, 2009). PPD among Kazak women in Xinjiang, China has never been documented. Therefore, this work provides an important reference for future research. In summary, this study demonstrated that (1) Kazak women were more likely to develop PPD than Han women, even after controlling for confounders; (2) there was a significant association between postpartum UI and PPD among Kazak but not among Han women; (3) mothers-in-law as caregivers after childbirth was positively associated with PPD among Han but not among Kazak women; and (4) common risk factors for PPD (previous pregnancy loss, unplanned pregnancy, and giving birth to a female infant) existed among both ethnic groups. As this was an exploratory study and there was uncertainty around the sample size estimation, we conducted a post-hoc power analysis. Based on the observed data, with an adjusted OR of 1.561 for Kazaks (compared to Hans) and a sample size of 1,263 observations (of which 51% are Hans and 49% are Kazaks), an 82% power is achieved at a 0.05 significance level to detect the association of Kazak ethnicity and PPD.
The current study suggests that UI has a differential impact on PPD risk by ethnic group. Kazak women who experienced postpartum UI had a higher risk of PPD. UI is a worldwide health problem, which adversely impacts quality of life of women (Padmanabhan & Dmochowski, 2014). Pregnancy and birth are known risk factors for the development of UI. The prevalence of postpartum UI is high, affecting as much as 33% of all women (Thom & Rortveit, 2010). Although previous studies have reported a correlation between UI and PPD (Fritel et al., 2016; Hullfish et al., 2007), a better understanding of the differences among ethnic groups with regard to the association of PPD and UI merits further exploration.
The presence of mothers-in-law as caregivers after delivery was found as a risk factor for PPD among the Han, but not among Kazak women. The custom of “doing the month” in China means that females stay at home, do not eat cold foods, and avoid a cool/wet environment in the first month after delivery. It is the family’s responsibility to not only care for the child, but for the new mother as well. Since husbands frequently return to work, the caregiver during “the month” is usually the woman’s mother or mother-in-law. The conflict between mothers-in-law and daughters-in-law is deep-rooted in China. A study by Chi et al. (2016) found that only 14.7% of females felt very satisfied in their relationships with their mothers-in-law. A study in Taiwan, China demonstrated that mothers-in-law produced a negative impact on females during the month (Heh, Coombes & Bartlett, 2004). This study also indicated that Han women who were cared for by mothers-in-law during the month after delivery were 2.54 times more likely to have PPD as compared to those who were cared for by others. The same association did not exist among the Kazak women. We found that both Han and Kazak women share the custom of doing the month. The difference is that almost half of the Han women stay at their home, and are cared for by their mothers-in-law during the month. Because Kazak women traditionally stay at their parents’ home during the month, less than a quarter of the Kazak women in our study were taken care of by their mothers-in-law following childbirth. Therefore, the same negative effects of mother-in-law caregiving would not be observed.
Despite the fact that different associated risk factors were found, risk factors that have been accepted in literature also existed in both ethnic groups, which is previous pregnancy loss, unplanned pregnancy, and giving birth to a female infant. This study confirmed the finding that previous pregnancy loss is an independent risk factor for PPD (Giannandrea et al., 2013). Previous studies also found that in economically underdeveloped countries or regions, unplanned pregnancy represents a risk factor for PPD (De Castro et al., 2015; Lara, Navarrete & Nieto, 2016), as well as women who delivered female infants were more likely to suffer from PPD (Xie et al., 2011). That association between female infant and PPD might best be explained by the prevalent desire for male offspring, and the negative reactions of family members toward the birth of a female infant, although this association was not found in a region with a relatively developed economy in China (Wan et al., 2009).
Limitations
Several limitations to this study should be noted. First, the screening tool for PPD used in this study was EPDS. Although the Chinese version of this scale has demonstrated good reliability and validity (Heh, 2001), a few Kazak women participants did not understand Chinese and the evaluation was completed with the assistance of Kazak nurses. This may have caused language bias. Second, these findings are not representative of all Han and Kazak women in Xinjiang province, since the purposive convenience sampling method was adopted to recruit equal numbers in each ethnic group. The results could have suffered from selection bias, particularly as those Kazak women who lived in remote areas and did not attend the routine consulting six weeks after childbirth were not included in the study. Finally, the study only included variables regarding socio-demographic and obstetric predictors, interaction of those variables and psychosocial factors could be ignored. Therefore, the results presented here should be interpreted with consideration of these circumstances.
Implications
The incidence of, and factors associated with, PPD among Han women are well-demonstrated in the literature. However, little is known about the situation in women of ethnic minority in China. Despite the limitations mentioned above, this study has addressed a gap in the literature, and has important implications for future research in related fields. First, given the fact that participants were not randomly selected, replication studies with efforts to minimize the selection bias are encouraged to further validate the results obtained from this study. Moreover, since information about the psycho-social predictors was not collected in this study, the association between ethnicity and PPD requires further examination to provide a comprehensive risk profile. To date, no psychometric instrument has been developed adapted for the Kazak population; studies with qualitative design could be alternative solutions to overcome the lack of validated tools. Beyond that, further research is needed to expand the qualitative aspects of the relationships between mothers-in-law and Han women, or Kazak women’s attitudes about UI. Finally, future research should direct attention to the translation of health-related assessment tools for ethnic minorities in China, thereby providing better medical services for these populations.
Conclusions
Kazak women were more likely to develop PPD than Han women, even after controlling for confounders. The risk factors for PPD identified were not the same between the different ethnic groups. Future research that explores the relationships between Han women and their mothers-in-law as well as Kazak women’s attitudes toward UI could further understanding about PPD in these populations.
Supplemental Information
Acknowledgments
The authors would like to thank Ainipa Ali, Gulijianati Abulikemu, Azhi Wen, and Gulizhipaxi Mi for assistance with interviewing Kazak women who could not understand and/or speak Chinese.
Funding Statement
This work was supported by the Sanming project of medicine in Shenzhen, China (No. SZSM201612018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Ling Chen conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables.
Li Ding conceived and designed the experiments, performed the experiments, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Ming Qi performed the experiments, contributed reagents/materials/analysis tools, wrote the paper.
Chao Jiang and Xin-min Mao performed the experiments, reviewed drafts of the paper.
Wen-Zhi Cai conceived and designed the experiments, analyzed the data, reviewed drafts of the paper.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Ethics approval for the study was granted by the Ethics Committee of the First Affiliated Hospital of Medicine College, Shihezi University (2015-134-01).
References
- Beck (2001).Beck CT. Predictors of postpartum depression: an update. Nursing Research. 2001;50:275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Chi et al. (2016).Chi X, Zhang P, Wu H, Wang J. Screening for postpartum depression and associated factors among women in China: a cross-sectional study. Frontiers in Psychology. 2016;7 doi: 10.3389/fpsyg.2016.01668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Castro et al. (2015).De Castro F, Place JM, Billings DL, Rivera L, Frongillo EA. Risk profiles associated with postnatal depressive symptoms among women in a public sector hospital in Mexico: the role of sociodemographic and psychosocial factors. Archives of Women’s Mental Health. 2015;18:463–471. doi: 10.1007/s00737-014-0472-1. [DOI] [PubMed] [Google Scholar]
- Fritel et al. (2016).Fritel X, Tsegan YE, Pierre F, Saurel-Cubizolles MJ, Group EM-CCS Association of postpartum depressive symptoms and urinary incontinence. A cohort study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2016;198:62–67. doi: 10.1016/j.ejogrb.2015.12.028. [DOI] [PubMed] [Google Scholar]
- Gao et al. (2016).Gao X, Wang J, Yao H, Cai Y, Cheng R. Serum BDNF concentration after delivery is associated with development of postpartum depression: a 3-month follow up study. Journal of Affective Disorders. 2016;200:25–30. doi: 10.1016/j.jad.2016.04.002. [DOI] [PubMed] [Google Scholar]
- Giannandrea et al. (2013).Giannandrea SA, Cerulli C, Anson E, Chaudron LH. Increased risk for postpartum psychiatric disorders among women with past pregnancy loss. Journal of Women’s Health. 2013;22:760–768. doi: 10.1089/jwh.2012.4011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heh (2001).Heh SS. Validation of the Chinese version of the Edinburgh postnatal depression scale: detecting postnatal depression in Taiwanese women. Hu Li Yan Jiu Nursing Research. 2001;9:105–113. [PubMed] [Google Scholar]
- Heh, Coombes & Bartlett (2004).Heh SS, Coombes L, Bartlett H. The association between depressive symptoms and social support in Taiwanese women during the month. International Journal of Nursing Studies. 2004;41:573–579. doi: 10.1016/j.ijnurstu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Hullfish et al. (2007).Hullfish KL, Fenner DE, Sorser SA, Visger J, Clayton A, Steers WD. Postpartum depression, urge urinary incontinence, and overactive bladder syndrome: is there an association? International Urogynecology Journal and Pelvic Floor Dysfunction. 2007;18:1121–1126. doi: 10.1007/s00192-007-0313-0. [DOI] [PubMed] [Google Scholar]
- Klainin & Arthur (2009).Klainin P, Arthur DG. Postpartum depression in Asian cultures: a literature review. International Journal of Nursing Studies. 2009;46:1355–1373. doi: 10.1016/j.ijnurstu.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Lara, Navarrete & Nieto (2016).Lara MA, Navarrete L, Nieto L. Prenatal predictors of postpartum depression and postpartum depressive symptoms in Mexican mothers: a longitudinal study. Archives of Women’s Mental Health. 2016;19:825–834. doi: 10.1007/s00737-016-0623-7. [DOI] [PubMed] [Google Scholar]
- Li et al. (2015).Li S, Zhang L, Liu Y, Qi Q. Changing spatial pattern of population of Xinjiang’s major ethnic groups, 1982–2010. Population Research. 2015;39:78–86. (In Chinese) [Google Scholar]
- Liu & Tronick (2013).Liu CH, Tronick E. Rates and predictors of postpartum depression by race and ethnicity: results from the 2004 to 2007 New York City PRAMS survey (Pregnancy Risk Assessment Monitoring System) Maternal and Child Health Journal. 2013;17:1599–1610. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- O’Hara & McCabe (2013).O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- O’Hara & Swain (1996).O’Hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry. 1996;8:37–54. doi: 10.3109/09540269609037816. [DOI] [Google Scholar]
- Padmanabhan & Dmochowski (2014).Padmanabhan P, Dmochowski R. Urinary incontinence in women: a comprehensive review of the pathophysiology, diagnosis and treatment. Minerva Ginecologica. 2014;66:469–478. [PubMed] [Google Scholar]
- Rao (2005).Rao SJ. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Journal of the American Statistical Association. 2005;98:257–258. [Google Scholar]
- Robertson et al. (2004).Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. General Hospital Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Templeton et al. (2003).Templeton L, Velleman R, Persaud A, Milner P. The experiences of postnatal depression in women from black and minority ethnic communities in Wiltshire, UK. Ethnicity and Health. 2003;8:207–221. doi: 10.1080/1355785032000136425. [DOI] [PubMed] [Google Scholar]
- Thom & Rortveit (2010).Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstetricia Et Gynecologica ScandInavica. 2010;89:1511–1522. doi: 10.3109/00016349.2010.526188. [DOI] [PubMed] [Google Scholar]
- Wan et al. (2009).Wan EY, Moyer CA, Harlow SD, Fan Z, Jie Y, Yang H. Postpartum depression and traditional postpartum care in China: role of zuoyuezi. International Journal of Gynaecology and Obstetrics. 2009;104:209–213. doi: 10.1016/j.ijgo.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Wei et al. (2008).Wei G, Greaver LB, Marson SM, Herndon CH, Rogers J. Postpartum depression: racial differences and ethnic disparities in a tri-racial and bi-ethnic population. Maternal and Child Health Journal. 2008;12:699–707. doi: 10.1007/s10995-007-0287-z. [DOI] [PubMed] [Google Scholar]
- Xie et al. (2011).Xie RH, Liao S, Xie H, Guo Y, Walker M, Wen SW. Infant sex, family support and postpartum depression in a Chinese cohort. Journal of Epidemiology and Community Health. 2011;65:722–726. doi: 10.1136/jech.2009.096651. [DOI] [PubMed] [Google Scholar]
- Yan et al. (2015).Yan X, Lu J, Shi S, Wang X, Zhao R, Yan Y, Chen G. Development and psychometric testing of the Chinese Postnatal Risk Factors Questionnaire (CPRFQ) for postpartum depression. Archives of Women’s Mental Health. 2015;18:229–237. doi: 10.1007/s00737-014-0451-6. [DOI] [PubMed] [Google Scholar]
- Yang et al. (2015).Yang F, Gardner Jr CO, Bigdeli T, Gao J, Zhang Z, Tao M, Liu Y, Li Y, Wang G, Shi J, Gao C, Zhang K, Li K, Wang X, Liu L, Sun J, Du B, Shi S, Zhang J, Wu W, Wang X, Shen J, Liu T, Gu D, Liang W, Deng H, Pan J, Yang L, Jian H, Jiang G, Meng H, Miao G, Li Y, Hu C, Huang G, Zhang Y, Chen Y, Ha B, Gao S, Fang X, Mei Q, Hong X, Yang D, Liu T, Fengyu Y, Zhong H, Sang H, Chen G, Cai M, Song Y, Dong J, Shen Z, Zhang W, Wang X, Pan R, Liu X, Li Y, Liu Z, Zhang Q, Li G, Flint J, Kendler KS. Clinical features of and risk factors for major depression with history of postpartum episodes in Han Chinese women: a retrospective study. Journal of Affective Disorders. 2015;183:339–346. doi: 10.1016/j.jad.2015.05.033. [DOI] [PubMed] [Google Scholar]
- Zaidi et al. (2017).Zaidi F, Nigam A, Anjum R, Agarwalla R. Postpartum depression in women: a risk factor analysis. Journal of Clinical and Diagnostic Research. 2017;11:QC13–QC16. doi: 10.7860/JCDR/2017/25480.10479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


