Abstract
High tibial osteotomy (HTO) is a valid treatment option for young active patients with medial tibiofemoral osteoarthrosis (OA) and varus deformity. Sometimes medial OA is combined with symptomatic anterior cruciate ligament (ACL) deficiency. Although isolated HTO (with possible delayed ACL reconstruction) might be indicated in the older population, young active patients may require combined HTO and ACL reconstruction. In addition, an abnormally increased tibial slope may predispose to ACL reconstruction failure and should be addressed for a successful ACL revision. The combination of HTO and ACL reconstruction produces good results, with resumption of normal daily activities, as well as recreational sports, and does not seem to increase the risk of complications compared with isolated HTO. The purpose of this Technical Note is to describe our indications, planning, and technique for opening wedge HTO fixed with a spacer plate and anatomic soft-tissue (autograft or allograft) ACL reconstruction, with proximal extracortical suspension and distal interference screw fixation.
High tibial osteotomy (HTO) is a valid treatment option for young (<60 years of age) active patients with medial tibiofemoral osteoarthrosis (OA) and varus deformity.1 Sometimes medial OA is combined with symptomatic anterior cruciate ligament (ACL) deficiency, and the surgeon has to address both problems. In addition, the natural history of a chronic ACL tear is cartilage wear of the posteromedial tibial plateau with progression to varus deformity. In the later stages, a slackening of the lateral and posterolateral ligamentous structures results in a varus thrust (double varus) or varus recurvatum thrust (triple varus).2
Recently, there has been increasing interest regarding the role of tibial slope in knee stability. An abnormally increased tibial slope may predispose to ACL reconstruction failure and should be addressed for a successful ACL revision.
In these scenarios, concurrent HTO and ACL reconstruction or revision can be indicated. The purpose of this Technical Note is to describe our indications (Table 1) and technique (Video 1) for combined opening wedge HTO and ACL reconstruction.
Table 1.
Indications for Combined HTO and ACL Reconstruction or Revision and Isolated HTO (With Possible Delayed ACL Reconstruction)
| Combined HTO and ACL reconstruction or revision |
| Medial-compartment OA (Ahlbäck grades 1-3) + varus malalignment + ACL tear (with symptomatic anteroposterior instability) |
| Medial-compartment OA (Ahlbäck grades 1-3) + varus malalignment + failed ACL reconstruction |
| Failed ACL reconstruction because of increased tibial slope |
| Double or triple varus and ACL tear (with symptomatic anteroposterior instability) |
| Varus malalignment + ACL tear + chondral or meniscal injuries (requiring cartilage repair or meniscal transplant) |
| Isolated HTO (with possible delayed ACL reconstruction) |
| Longstanding ACL deficiency + double or triple varus |
| Longstanding ACL deficiency + varus malalignment + symptomatic medial-compartment OA |
| Longstanding ACL deficiency + double or triple varus + symptomatic medial-compartment OA |
ACL, anterior cruciate ligament; HTO, high tibial osteotomy; OA, osteoarthrosis.
Surgical Technique
Preoperative Planning
Long-leg radiographs with anteroposterior and lateral views are required for planning. In the case of medial OA, HTO is planned with a slight valgus overcorrection (3°-5°) (Fig 1).1 In this scenario the mechanical axis should pass through a point located at 62.5% of the width of the tibial plateau from medial to lateral. In young active patients a correction to neutral alignment (50% of tibial plateau) is planned.3 The tibial slope is assessed on lateral views. A normal slope varies from 0° to 18°.4 When exceeding 10°, the slope should be decreased to reduce tension to the reconstructed ACL. Even though bone block autograft or allograft (i.e., bone–patellar tendon–bone) can be used for ACL reconstruction or revision, we recommend soft-tissue autograft (i.e., hamstring) or allograft (i.e., tibialis anterior) to overcome the possible complication of graft-tunnel mismatch.
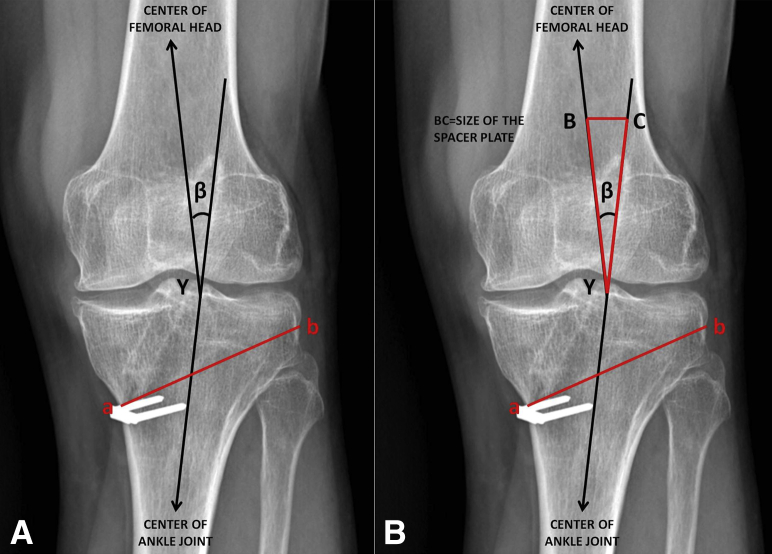
Fig 1.
Planning of opening wedge high tibial osteotomy (left knee, anteroposterior view). (A) Opening wedge high tibial osteotomy is planned with a line from point Y (62.5% or 50% of the width of the tibial plateau) to the center of the femoral head, as well as another line connecting Y with the center of the ankle joint. The angle between these 2 lines is the angle of correction (β). The osteotomy line (ab) is defined from medial (around 4 cm below the joint line) to lateral (around 1 cm below the lateral joint line). (B) The distance “ab” is transferred to both rays (YB and YC) of angle β from vertex Y. Segment BC is equal to the opening of the osteotomy and the size of the tooth of the spacer plate.
Patient Positioning
Intravenous antibiotic prophylaxis is administered. The patient is positioned supine on a radiolucent table, under regional or general anesthesia, with a tourniquet at the proximal thigh. A lateral post is placed at the level of the tourniquet. Positioning should allow for knee hyperflexion if inside-out transportal femoral tunnel drilling is planned.
Graft Harvesting
A 7- to 8-cm vertical incision is performed medially, midway between the tibial tubercle and posteromedial tibial cortex, starting 1 cm distal to the joint line. When autologous hamstring graft is used, the sartorial fascia is incised; the gracilis tendon proximally and the semitendinosus distally are identified. All the vincula of the tendons are carefully released. A tendon stripper (ConMed Linvatec, Largo, FL) is then used to harvest the tendons (Fig 2). When allograft is used, surgery begins with the next step, comprising arthroscopy, knee balancing, and femoral tunnel drilling.
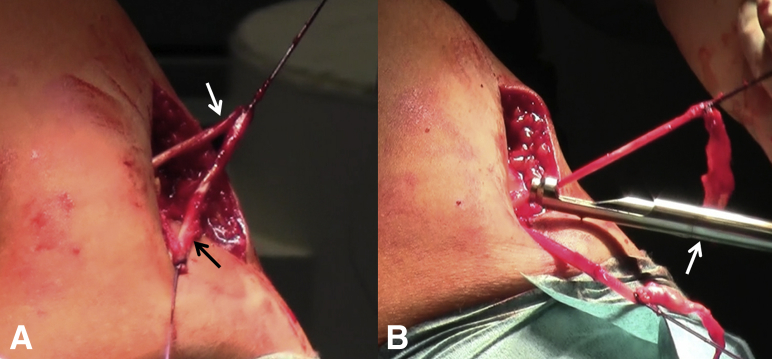
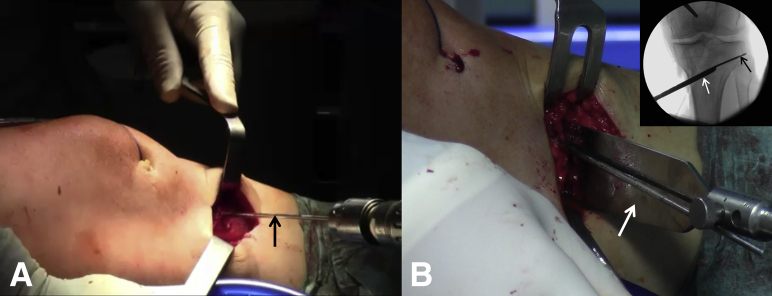
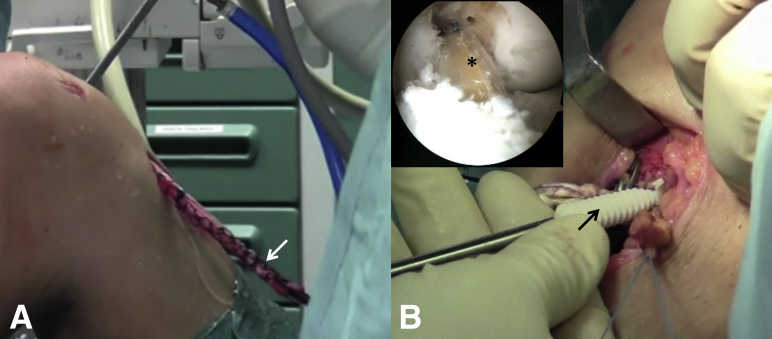
Fig 2.
Surgical technique (left knee, medial view). (A) With a vertical incision, performed midway between the tibial tubercle and posteromedial tibial cortex, the gracilis tendon proximally (white arrow) and the semitendinosus distally (black arrow) are identified. (B) Once all the vincula of the tendons are released, a tendon stripper (arrow) is used to harvest the tendons.
Arthroscopy, Knee Balancing, and Femoral Tunnel Drilling
Arthroscopy is performed through standard anteromedial (AM) and anterolateral portals. Complete knee balancing is performed, and concomitant meniscal and chondral injuries are treated. The ACL stump is removed, when present, and the medial wall of the lateral femoral condyle is carefully debrided. In some cases osteophytes are seen in the intercondylar notch, and these need to be removed with a shaver or acromioplasty burr to avoid roof impingement with the ACL. Any technique for femoral tunnel drilling can be used, except transtibial drilling. Our preferred technique is inside-out transportal femoral tunnel drilling, although this may vary in the case of revision ACL, depending on the previous femoral tunnel position. The femoral tunnel intra-articular aperture is determined (usually the AM bundle or the midpoint between the AM and posterolateral bundles) with a femoral offset guide (ConMed Linvatec) and a guidewire (Fig 3). Femoral tunnel preparation proceeds according to the preferred femoral fixation device. An extracortical suspension technique is our preferred fixation method (EndoButton; Smith & Nephew, Andover, MA). With this technique, a 4.5-mm cannulated reamer is used to create a full tunnel (Smith & Nephew), over the guidewire. The guidewire is removed, the tunnel measured, and the guidewire repositioned. A half tunnel of the desired length (usually 25 mm) is then created with a cannulated reamer (same size as graft diameter). A shuttle suture is left in the femoral tunnel, exiting from the lateral thigh and the AM portal (Fig 4).
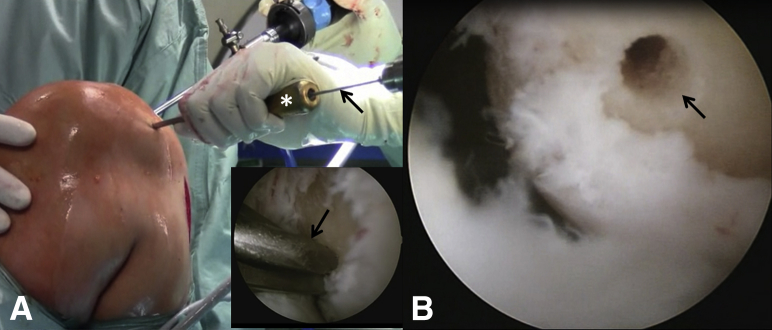
Fig 3.
Surgical technique (left knee, medial view). (A) With the knee hyperflexed, the anatomic position of the femoral tunnel is determined with a femoral offset guide (asterisk) and a guidewire (arrows). An arthroscopic view is shown in the inset. (B) Arthroscopic view from anteromedial portal. It should be noted that the tunnel is placed at the level of the anteromedial bundle femoral insertion (arrow).
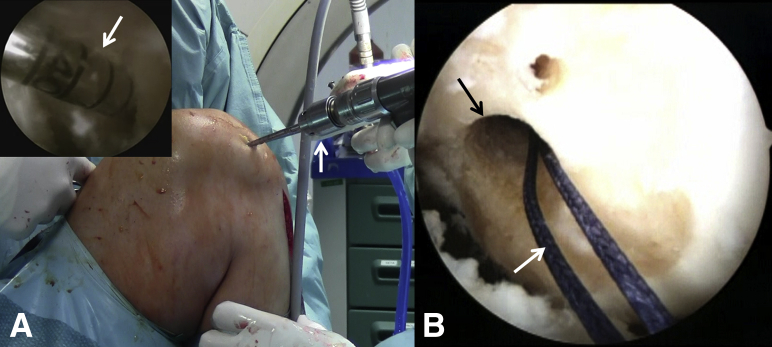
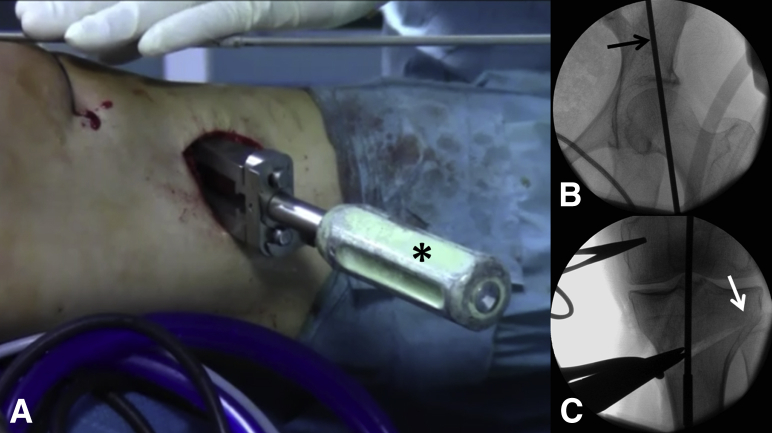
Fig 4.
Surgical technique (left knee, medial view). (A) With the knee hyperflexed, the femoral tunnel is drilled using cannulated reamers (arrows) with an inside-out technique. An arthroscopic view is shown in the inset. Because an extracortical suspension device is used in this case for anterior cruciate ligament proximal fixation, first a 4.5-mm full femoral tunnel and then a half tunnel of the same diameter as the graft are drilled. (B) A shuttle suture (white arrow) is positioned in the femoral tunnel (black arrow).
Opening Wedge High Tibial Osteotomy
A guidewire is positioned under fluoroscopic guidance from medial to lateral and from distal to proximal, starting around 4 cm below the medial joint line, aiming at the tip of the fibular head (around 1 cm below the lateral joint line) (Fig 5). The distal insertion of the superficial medial collateral ligament is partially detached. The patellar tendon and the posterior neurovascular structures are protected with blunt retractors throughout the whole procedure. A 3-cm-wide, thin oscillating saw is used to cut the medial, anterior, and posteromedial cortices distal to the guidewire. The osteotomy should be parallel to the tibial slope (with 10° of anteroposterior inclination). Wide thin osteotomes are used to complete the osteotomy, preserving a lateral cortical hinge (Fig 5). With this goal, the blade of the osteotome should be advanced up to around 1 cm from the lateral tibial cortex; this distance should be less than the distance from the lateral joint line and the blade of the osteotome to avoid intra-articular migration of the osteotomy. The mobility of the osteotomy is checked by using a gentle valgus force or by pulling the handle of the last osteotome distally. If the osteotomy does not open, the surgeon should verify that the cut of the anterior and posterior cortices is complete. Graduated osteotomy wedges are then inserted up to the planned opening. With fluoroscopy, a long alignment rod is placed from the center of the femoral head to the center of the ankle to check the mechanical axis at the level of the knee (Fig 6). When the desired alignment is achieved, plating can be performed. Our favorite fixation device is a short locking spacer plate (plate and HTO instrumentation from Arthrex, Naples, FL). The plate is generally positioned in a more posterior position compared with HTO for isolated medial OA. This has the advantages of (1) decreasing the tibial slope and protecting the ACL graft from excessive tension and (2) leaving more room on the AM tibia for tibial tunnel drilling. All screws are positioned except for the proximal anterior cancellous screw. This will be placed after tibial tunnel drilling.
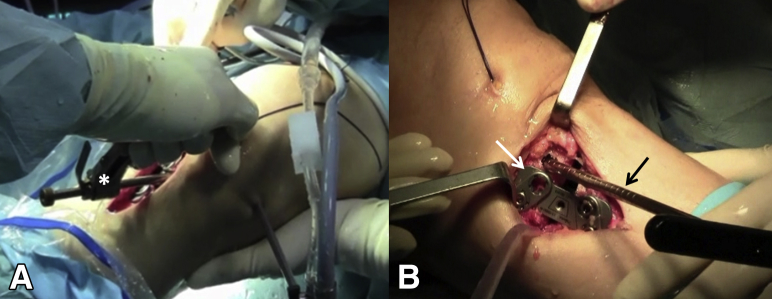
Fig 5.
Surgical technique (left knee, medial view). (A) A guidewire (arrow) is positioned under fluoroscopic guidance from medial to lateral and from distal to proximal, starting around 4 cm below the medial joint line, aiming at the tip of the fibular head (around 1 cm below the lateral joint line). (B) The osteotomy is created distal to the guidewire, first with an oscillating saw and then with graduated osteotomes (white arrow). This is performed under fluoroscopic guidance. The inset shows an anteroposterior view of the guidewire (black arrow) and osteotome (white arrow).
Fig 6.
Surgical technique (left knee, medial view). (A) Graduated osteotomy wedges (asterisk) are inserted up to the planned opening. (B, C) With fluoroscopy, a long alignment rod (black arrow) is placed from the center of the femoral head (B) to the center of the ankle to check the mechanical axis at the level of the knee (C). One should note that a lateral bone hinge (white arrow) should be preserved. When the desired alignment is achieved, plating can be performed.
Tibial Tunnel Drilling
Under arthroscopic visualization, a tibial guide (Smith & Nephew) is positioned on the anatomic tibial footprint of the ACL. The distal tibial aperture of the tunnel should be right anterior to the plate on the proximal tibial fragment (Fig 7). With a tibial guide, a guidewire is drilled into the proximal tibia. A cannulated reamer (same size as graft) is then used to create the tunnel. A metal bone tunnel dilator (same diameter as reamer) is inserted in the tibial tunnel and left in place (Fig 7).
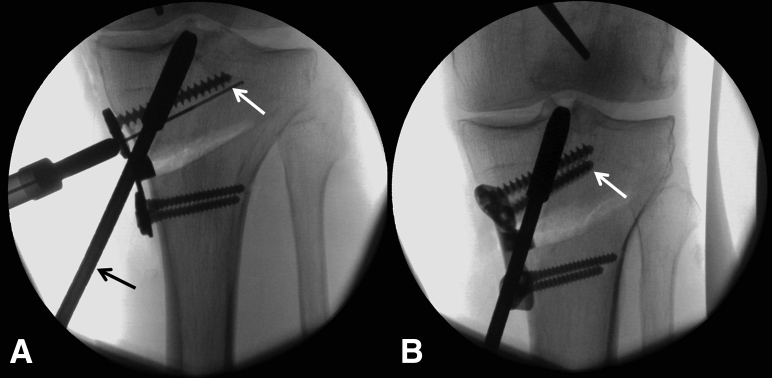
Fig 7.
Surgical technique (left knee, medial view). Once plating is performed and all screws (except for the proximal anterior screw) are placed, the tibial tunnel can be drilled. (A) Under arthroscopic visualization, a tibial guide (asterisk) is positioned on the anatomic tibial footprint of the anterior cruciate ligament. The distal tibial aperture of the tunnel should be right anterior to the plate on the proximal tibial fragment. A guidewire and a cannulated reamer (same size as graft) are then used to create the tunnel. (B) A metal bone tunnel dilator (black arrow) is inserted in the tibial tunnel and left in place. It should be noted that the proximal anterior screw is not in place (white arrow) at this point.
Completion of Osteotomy Fixation
To avoid interference between the tibial tunnel and the proximal anterior cancellous screw, this is placed with the metal dilator into the tibial tunnel (Fig 8). Once all the screws are in place, the dilator can be removed. An arthroscopic grasper is then inserted in the tibial tunnel, and the shuttle suture (previously positioned in the femoral tunnel in the step comprising arthroscopy, knee balancing, and femoral tunnel drilling) is retrieved from the AM tibia.
Fig 8.
Surgical technique (anteroposterior fluoroscopic views of left knee). (A) To avoid interference between the tibial tunnel and the proximal anterior cancellous screw, this is placed with the metal dilator (black arrow) into the tibial tunnel. The bone screw depth gauge is shown (white arrow). (B) The last cancellous screw (arrow) is shown in place.
ACL Graft Fixation
The sutures of the cortical suspension device are pulled into the joint with the shuttle suture. The graft is pulled into the joint and fixed proximally by flipping the button (EndoButton) on the lateral femoral cortex. The graft is tensioned by moving the knee through full range of motion for about 10 cycles. Tibial fixation is achieved at 20° of flexion with an interference screw (1 or 2 mm larger than the tibial tunnel, depending on the bone quality; DePuy Synthes, Raynham, MA) (Fig 9). The arming sutures of the graft's tails are tied to the plate for additional fixation. For osteotomies with an opening of less than 10 mm, no bone grafting is necessary. For larger corrections, allograft bone wedges are used to augment the gap. Technical tips are summarized in Table 2.
Fig 9.
Surgical technique (left knee, medial view). (A) The graft (arrow) is pulled into the joint and fixed proximally by flipping the button of the cortical suspension device on the lateral femoral cortex. (B) After the surgeon checks the correct position (asterisk) of the graft (an arthroscopic view of the neo-ligament from the anteromedial portal is shown the inset), tibial fixation is achieved at 20° of flexion with an interference screw (arrow).
Table 2.
Technical Tips and Rationale for Tips in Combined HTO and ACL Reconstruction or Revision
| Surgical Step | Technical Tip | Rationale |
|---|---|---|
| Graft choice | Use soft-tissue autograft (i.e., hamstring) or allograft (i.e., tibialis anterior). | Avoid possible graft-tunnel mismatch intraoperatively. |
| Arthroscopy and femoral tunnel drilling | Perform arthroscopy and femoral tunnel drilling before HTO. | Avoid stress and hyperflexion of the knee after HTO, with the risk of loss of correction. |
| HTO | Before HTO, protect the patellar tendon with a blunt retractor and the posterior neurovascular structures with a blunt Hohmann retractor. | Avoid damage to these structures. |
| Preserve a cortical lateral hinge. Bear in mind that the osteotomes should be advanced up to 1 cm of distance from the lateral tibial cortex, and note that this distance should be less than the distance from the tip of the osteotome to the lateral articular surface. | Avoid lateral hinge disruption (with mediolateral displacement of the fragments) or intra-articular migration of the osteotomy. | |
| After completion of the HTO, check the mobility of the osteotomy site by using a gentle valgus force or by pulling the handle of the last osteotome distally. If the osteotomy does not open, verify that the cut of the anterior and posterior cortices is complete. | Avoid intra-articular or distal migration of the osteotomy. | |
| Note that the plate is generally positioned in a more posterior position compared with HTO for isolated medial OA. | (1) Decrease the tibial slope, protecting the ACL graft from excessive tension. (2) Leave more room on the anteromedial tibia for tibial tunnel drilling. | |
| During plating, note that all screws are positioned except for the proximal anterior cancellous screw. Place this after tibial tunnel drilling. | Avoid interference between the tibial tunnel and the proximal anterior cancellous screw. | |
| Tibial tunnel drilling | After tibial tunnel drilling, insert a metal bone tunnel dilator in the tunnel during positioning of the proximal anterior cancellous screw. | Avoid interference between the tibial tunnel and the proximal anterior cancellous screw. |
ACL, anterior cruciate ligament; HTO, high tibial osteotomy; OA, osteoarthrosis.
Postoperative Regimen
Immediate full range-of-motion exercises are allowed. The patient is kept partially weight bearing in a hinged knee brace for 6 weeks. At 6 weeks, after radiographic confirmation of bone healing, weight bearing is allowed, the brace is discontinued, and the rehabilitation protocol proceeds as in standard ACL reconstruction.
Discussion
The combination of HTO and ACL reconstruction has the obvious advantage of a single surgical procedure together with a faster recovery compared with a staged procedure and produces good results in active patients with symptomatic ACL deficiency, medial OA, and varus malalignment (Table 3).5 Resumption of normal daily activities and recreational sports can be expected.5 With opening wedge HTO, the surgeon is able to correct the coronal and sagittal (tibial slope) alignment. Reducing the tibial slope during surgery seems to have a key role in protecting the ACL graft, and this is essential in the case of ACL revision, when ACL failure is caused by an abnormally increased tibial slope.6 Moreover, closing wedge HTO combined with ACL reconstruction is a valid alternative option, with the potential advantage of a reduced risk of nonunion. Closing wedge HTO usually results in a decreased tibial slope, but the amount of correction is more difficult to fine-tune. In addition, closing wedge HTO is a more complex procedure entailing common peroneal nerve dissection and proximal tibiofibular joint disruption or fibular osteotomy.
Table 3.
Advantages and Disadvantages of Combined HTO and ACL Reconstruction or Revision
| Advantages |
| Reliability |
| No graft-tunnel mismatch |
| Single surgical procedure |
| Non-interference between tibial tunnel and osteotomy screws |
| Fine-tuning of tibial slope |
| Reduced costs compared with staged procedure |
| Disadvantages |
| Long learning curve |
| Longer rehabilitation |
| Increased costs compared with isolated osteotomy |
ACL, anterior cruciate ligament; HTO, high tibial osteotomy.
Although the combination of ACL reconstruction and HTO is more technically demanding and seems at higher risk of complications compared with a staged procedure, it has been shown to have a similar rate of complications to that of isolated HTO.7 In older, less demanding patients (Table 1), isolated HTO (with possible delayed ACL reconstruction) can produce satisfactory outcomes.8
Footnotes
The authors report the following potential conflict of interest or source of funding: R.R. receives support from the following: part of the teaching program for Zimmer-Biomet and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Our technique for combined anterior cruciate ligament reconstruction and high tibial osteotomy is described. This technique is for opening wedge high tibial osteotomy fixed with a spacer plate and anatomic soft-tissue (autograft or allograft) anterior cruciate ligament reconstruction, with proximal extracortical suspension and distal interference screw fixation. Radiographs and surgical images of a left knee are shown. The patient is positioned supine with the possibility of fully extending and flexing the knee. The camera is positioned on the right side of the patient (pointing to the medial aspect of the knee).
References
- 1.Bonasia D.E., Dettoni F., Sito G. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: Prognostic factors. Am J Sports Med. 2014;42:690–698. doi: 10.1177/0363546513516577. [DOI] [PubMed] [Google Scholar]
- 2.Noyes F.R., Barber-Westin S.D., Hewett T.E. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28:282–296. doi: 10.1177/03635465000280030201. [DOI] [PubMed] [Google Scholar]
- 3.Naudie D.D., Amendola A., Fowler P.J. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32:60–70. doi: 10.1177/0363546503258907. [DOI] [PubMed] [Google Scholar]
- 4.Genin P., Weill G., Julliard R. The tibial slope: Proposal for a measurement method. J Radiol. 1993;74:27–33. [PubMed] [Google Scholar]
- 5.Li Y., Zhang H., Zhang J., Li X., Song G., Feng H. Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: A systematic review. Arthroscopy. 2015;31:507–519. doi: 10.1016/j.arthro.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 6.Arun G.R., Kumaraswamy V., Rajan D. Long-term follow up of single-stage anterior cruciate ligament reconstruction and high tibial osteotomy and its relation with posterior tibial slope. Arch Orthop Trauma Surg. 2016;136:505–511. doi: 10.1007/s00402-015-2385-5. [DOI] [PubMed] [Google Scholar]
- 7.Willey M., Wolf B.R., Kocaglu B., Amendola A. Complications associated with realignment osteotomy of the knee performed simultaneously with additional reconstructive procedures. Iowa Orthop J. 2010;30:55–60. [PMC free article] [PubMed] [Google Scholar]
- 8.Mehl J., Paul J., Feucht M.J. ACL deficiency and varus osteoarthritis: High tibial osteotomy alone or combined with ACL reconstruction? Arch Orthop Trauma Surg. 2017;137:233–240. doi: 10.1007/s00402-016-2604-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Our technique for combined anterior cruciate ligament reconstruction and high tibial osteotomy is described. This technique is for opening wedge high tibial osteotomy fixed with a spacer plate and anatomic soft-tissue (autograft or allograft) anterior cruciate ligament reconstruction, with proximal extracortical suspension and distal interference screw fixation. Radiographs and surgical images of a left knee are shown. The patient is positioned supine with the possibility of fully extending and flexing the knee. The camera is positioned on the right side of the patient (pointing to the medial aspect of the knee).