Abstract
People affected by rare diseases often have limited coping resources and sometimes face stigma. They build communities with others who share their conditions, but not all members may benefit from these communities. This study investigated how adults with a rare genetic health condition (Alpha-1 antitrypsin deficiency; AATD) think about both the Alpha-1 community and public stigma about AATD, and how these cognitions were associated with their communication responses and well-being. The results showed that people with AATD encountered stigmatization from various sources, including family, employers, healthcare providers, and insurance companies. Stronger public stigma predicted more secrecy, more stress, and less available support. Stronger group identification with the Alpha-1 community predicted less secrecy; stronger group activism predicted more available support and more communication to challenge stigmatizers. Post-hoc analyses showed significant interactions between public stigma and group cognitions on communication to challenge stigmatizers. Practical implications for bolstering communities to improve the well-being of people with rare diseases were discussed.
Keywords: support communities, public stigma, coping, activism, group identification
Approximately 25 million people in the United States are affected by one of 7,000 rare diseases, many of which have a genetic component (Valdez, Ouyang, & Bolen, 2016). These people encounter difficulty in coping with their illness; one source of difficulty is that resources often are scarce for rare diseases, because they do not attract the attention of researchers, clinicians, pharmaceutical companies, and policy makers (Valdez et al., 2016). People living with rare diseases often build communities with others who share their condition. The Rare Diseases Act passed by the US Congress in 2002 identified disease-based support groups as a key area of investment. By 2015, the National Institutes of Health (NIH) had documented over 1,400 disease-based communities in the US that support people with rare diseases and their families.
The resources for coping with rare diseases may be further depleted when the diseases or their causes are stigmatized (Smith, Parrott, & Wienke, 2016). People with rare, genetic health conditions have reported being socially excluded by friends and relatives (Klitzman & Sweeney, 2011) and denied employment and insurance coverage (Klitzman, 2010). As people believe that the general public will devalue and discriminate against them based on their health condition (i.e., public stigma), they may engage in strategies to limit their risk of experiencing rejection, such as keeping their health condition secret (Link, Cullen, Struening, Shrout, & Dohrenwend, 1989). It is unclear how effectively health communities mitigate the negative effects (e.g., stress) of public stigma.
We investigated a community consisting of people with a rare, genetic condition—Alpha-1 antitrypsin deficiency (AATD). Drawing from the group cognition model (Correll & Park, 2005), we examined how public stigma and social cognitions about the Alpha-1 community (i.e., identification and activism) are associated with stress, communicative response (i.e., secrecy and challenge), and available support. The findings can offer evidence-based guidance to strengthen support communities, which can play a critical role in mobilizing actions toward finding effective treatments for rare conditions and advocating for social equality.
AATD and Health-Related Stigma
AATD is an under-recognized genetic disorder that predisposes people to adult-onset diseases such as chronic obstructive pulmonary disease, emphysema, cirrhosis, and lung or liver cancer (Stoller & Aboussouan, 2011). The diseases are caused by the abnormal production of a protein, alpha-1 antitrypsin (AAT), which leaves the lungs and liver inadequately protected from damage. Of the estimated 33,000 to 70,000 Americans affected by severe deficiency of the protein, fewer than 10% are currently receiving clinical treatments such as intravenous augmentation therapy (Stoller & Aboussouan, 2011).
Under-recognition of AATD has severely constrained the resources available for affected people and their family to receive interventions that may favorably influence disease outcomes. For example, people with AATD have reported seeing multiple health providers with relevant symptoms before getting tested for the abnormal protein or its genetic predictors (Stoller, Smith, Yang, & Spray, 1994), thereby delaying treatments that could slow the diseases. Treatment costs more in later than early stages of the disease progression; thus, delayed diagnoses increase the economic burden for the affected people and their family (Valdez et al., 2016). Access to effective and affordable treatment options is also compromised because underdiagnoses reduce drug manufacturers’ motivation to fund research and development into commercially viable medicines (Trouiller et al., 2002).
Health-related stigma presents another obstacle for people with AATD. Stigma is “a simplified, standardized image of the disgrace of certain people that is held in common by the community at large” (Smith, 2007, p. 464). Stigma is not an objective characteristic of a particular health condition, but a social construction with many dimensions (Berger, Ferrans, & Lashley, 2001). Within this study, we focused on what Corrigan (2004) called public stigma, which highlights stigmatized people’s beliefs about the negative stereotypes about and reactions to a group that have diffused among the general public (Corrigan, 2004). Put differently, public stigma is “the extent to which individuals believe that ‘most people’ (the community at large) will devalue and discriminate” against a person living with AATD (Link et al., 1989, p. 403).
Stigma can be induced by one’s possession of a visible, repulsive mark recognized by the community at large (Smith, 2007). People with problematic alleles in the SERPINA1 gene are at risk for AATD. A gene has two alleles; the SERPINA1 gene has been identified with several types of alleles, which confer different risk for AATD. The M allele, for example, is associated with normal levels of AAT; a person with MM in the SERPINA1 gene is considered normal. Problematic alleles such as Z and S lead to a deficiency of AAT (Stoller & Aboussouan, 2011). People with two problematic alleles (e.g., ZZ) have a higher likelihood of exhibiting symptoms than people with only one problematic allele (e.g., MZ; Stoller & Aboussouan, 2011). AATD-related symptoms, such as dyspnea and wheezing, have noted stigmas (Berger, Kapella, & Larson, 2011). For example, people were excluded from social activities because other interactants considered their persistent cough irritating and their copious sputum disgusting (Berger et al., 2011). Family members were embarrassed by and blamed patients for their using inhalers in public, and people with AATD reported experiencing relational conflicts and rejection from dating partners (Klitzman & Sweeney, 2011).
AATD is associated with the first documented case of stigma related to one’s genetic condition (Jones & Sarata, 2008). Despite the enactment of the Genetic Insurance Nondiscrimination Act, stigma against people with AATD may still exist through issues it does not address, such as denial of life insurance or lack of workplace accommodation (Klitzman, 2010). For example, a company may refuse to limit an AATD carrier’s exposure to environmental irritants, which could accelerate the disease progression (Klitzman, 2010). In this scenario, employees with AATD must choose between putting their personal health at great risk or quitting their jobs and incurring loss of income and benefits. Given that people with AATD may encounter various stigmatization related to their health condition, we asked:
RQ1: What characterizes the memorable events people with AATD recall as being stigmatizing?
Secrecy, Support Availability, and Stress
Health-related stigma is linked to many negative outcomes. We focused on secrecy, support availability, and stress, as they may influence the resources for people to cope with diseases and health-related stigmatization (Link et al., 1989).
Secrecy
Stronger public stigma may be associated with more secrecy due to fear of being rejected, which limits opportunities to gain informational, instrumental, and emotional support from confidants (Greene, 2009). Secrecy refers to the concealment of information that would categorize a person in a stigmatized group (Link et al., 1989). For example, husbands who perceived infertility stigma were more likely to avoid disclosing information about their own or their wives’ infertility treatment to their social networks (Steuber & Solomon, 2011).
Support availability
Broadly defined, support availability refers to the perception that one or more people are ready and able to provide assistance or that the available support is adequate (Burleson & MacGeorge, 2002). The definitions are related. Wright (2000) reported that the size of a person’s support network was positively associated with both the number of hours a person spends communicating with online support groups and the number of messages a person receives within the group. People with more supporters available to them may be better able to receive higher quality support to meet their needs.
In this study, we defined support availability as a person’s estimate of the number of providers who can complete supportive tasks should the need arise (Link et al., 1989). We focused on the perceived number of available support providers for two reasons. First, judging the quality of the support provided presumes that someone is available to provide support. Stigmatized peoples’ social networks may become smaller, as they attempt to avoid experiencing rejection or as the public pulls away from them (Link et al., 1989). In the context of mental illness, public stigma has been associated with less support availability in cross sectional studies (e.g., Link et al., 1989), and significant continued shrinking in longitudinal studies (e.g., Perry & Pescosolido, 2012). Second, the optimal matching model (Cutrona & Russell, 1990) suggested that no single provider is beneficial for all supportive tasks. A person who gives good advice about disease management may not be helpful in offering insurance-related advice. A social network may become so small that no one is perceived as available to provide a certain type of support, leaving stigmatized people unable to meet their needs. With multiple support providers, if one provider is not available, a person can seek out additional providers to meet the need.
Stress
Stronger public stigma may be also related to a greater level of stress, as the threats imposed by potential stigmatization exceed the affected person’s coping resources (Wright & Rains, 2013). Indeed, the strong link between anticipating and experiencing stigmatization and stress is one of the mechanisms by which stigma speeds disease progression and increases mortality (Link & Phelan, 2006). We hypothesized:
H1: Stronger public stigma about AATD predicts (a) more secrecy, (b) lower perceived support availability, and (c) greater perceived stress.
Alpha-1 Community and Group Cognition Model
Past decades have witnessed an increasing number of support groups that are “formed for the specific purposes of providing mutual aid among members who share a common dilemma” (Cline, 1999, p. 516). The increasing prevalence of support groups is driven by societal changes such as overburdened healthcare system, complexity and uncertainty about health conditions (Cline, 1999), and stigma against the affected people and their support networks (Link et al., 1989); people with AATD face these same challenges.
A robust Alpha-1 community consisting of patients, their close contacts, clinicians, and researchers has been created to bring attention to the under-recognized condition and respond to social pressures (Walsh, 2013). The Alpha-1 community originated in 1987 when NIH recruited people with AATD through 37 clinical centers around the nation. Participants in this recruitment event described meeting other people with similar conditions as “an epiphany” (p. 58) and “like finding a long lost relative” (p.57) who could truly empathize, not just sympathize, with their illness experience (Walsh, 2013). The community now has over 80 affiliated support groups. Community activities include multiple education days each year across the country, a national conference, support group meetings, and a research registry. Numerous publications, including a community-wide magazine, educational brochures, newsletters, and a reference guide (available in nine languages), were developed to provide affected people with practical advice, personal stories, and updates on the advocacy events (Walsh, 2013). Through these activities and outlets, the community offered a platform for people affected by AATD to exchange information, share experience, and bond as a community.
Existing research shows that support groups have positive effects on health and well-being. The results of several meta-analyses on the effectiveness of group psychotherapy found that face-to-face support groups alleviated disease symptoms (Barkowski et al., 2016), increased satisfaction with group experience (Barlow, Burlingame, Nebeker, & Anderson, 2000), and led to general health improvements (Burlingame, Fuhriman, & Mosier, 2003). The benefits of participating in support groups were also observed in computer-mediated support groups, with at least one meta-analysis reporting that people who enrolled in internet-based groups perceived greater social support, experienced less depression, had a higher quality of life, and reported more self-efficacy to manage their health conditions at the conclusion of the interventions than at the beginning of program (Rains & Young, 2009). Scholars often highlight groups’ supportive communication climate, in which members with similar challenges seek information, validate experience, express emotions, expand support network, and develop new identities (Cline, 1999).
However, not all members benefit from participation in support groups to the same extent, and support groups may even produce negative consequences for some participants. Past research revealed that the extent to which people benefit from support groups depends on individual characteristics and features of health conditions (e.g., Gottlieb & Wachala, 2007). One less studied mechanism is the role of participants’ cognitions about their groups (Cline, 1999). There are pragmatic reasons for understanding how participants’ cognitions influence support outcomes. Support group leaders can promote communication activities that improve group cognitions associated with favorable outcomes such as confidence in challenging stigmatization, while modifying cognitions that prevent people benefiting from participation in support groups. The group cognition model (GCM; Correll & Park, 2005) may offer insights.
Group Cognition Model
According to the GCM, the extent to which people benefit from participation in support groups is affected by whether they assess the group as a resource or a threat (Barreto, 2014; Correll & Park, 2005). The assessment is informed by two social cognitions: group identification (Correll & Park, 2005) and group activism (Corrigan, Faber, Rashid, & Leary, 1999).
Group identification refers to how attached people feel to a particular group and focuses on whether the group serves as a source of a person’s identity (Correll & Park, 2005). Stronger identification with a support group has been associated with less secrecy and less stress (Rüsch et al., 2009). Indeed, studies showed that information seeking and exchange appears more frequently than secrecy in both online (Wright, 1999) and face-to-face support groups (Dennis, Kunkel, & Keyton, 2008). People who identify with the support group may view it as a safe forum to disclose information and seek support that can be offered only by those with a similar health condition. Furthermore, the likelihood of disclosure depends on a discloser’s assessment of receivers: people are more likely to disclose if they expect positive reactions and outcomes from the receivers (Greene, 2009). Group identification may lead to positive assessments of receivers, thereby promoting disclosure. As information exchange increases, people may find that their coping resources begin to outweigh the demands imposed by stressors and experience less stress. We hypothesized:
H2: Greater identification with Alpha-1 community is associated with a) less secrecy and b) less perceived stress.
The extant literature suggests that group activism is conceptualized as both a behavioral (Brashers, Haas, Klingle, & Neidig, 2000) and a cognitive construct (Corrigan et al., 1999). As a behavioral construct, group activism refers to “persuasive communication behaviors of a collective that are intended to serve the common interest” (Brashers et al., 2000, p. 375), such as demonstrating, protesting, and lobbying (Zoller, 2005). Group activism orients people toward taking actions for the shared interests of the group to which they belong, and differs from self-advocacy, where the primary purpose of action is to serve individual interests (Brashers et al., 2000). As a cognitive construct, group activism describes the extent to which people are confident that the group has the capacity to attain their goals (Corrigan et al., 1999). It reflects one’s belief in the group’s capacity to change the status quo that is perceived to obstruct the well-being of the group and its members. In this study, we explored group activism as a cognitive construct, referring to the extent to which people with AATD believe that the Alpha-1 community, when working together, can achieve their goals.
Stronger group activism has been linked to more support and lower stress. In the context of mental health, people with stronger perceptions of their support group as active received more emotional, material, and informational support (Corrigan et al., 1999), and have reported less stress (Rüsch et al., 2009). Stronger group activism may also be associated with communicative behavior to challenge stigmatization. Challenging takes the forms of providing information in the hope of generating acceptance and averting social rejection or expressing disagreement when stigmatization occurs (Link, Struening, Neese-Todd, Asmussen, & Phelan, 2002). People challenge stigmatizers when they believe that they do not deserve devaluation (Meisenbach, 2010); group activism may allow stigmatized people to avoid internalizing public stigma, and empower them to fight back. We hypothesized:
H3: Stronger group activism about the Alpha-1 community is associated with a) higher perceived support availability, b) less perceived stress, and c) more communication to challenge stigmatizers.
Genetic Essentialism
Genetic health conditions invite considerations of genetic essentialism, which may be associated with both public stigma and group identification. In general, essentialism “guides our perceptions by allowing us to sort characteristics into groups and act based on our beliefs about the essence of a category” (Parrott, Smith, Hong, & Worthington, 2015, p. 533). Genetic essentialism places primacy on genes as determining one’s personality, behavior, health, and life course. Essentialist beliefs related to genes and health include the belief that the presence of a problematic allele in a gene means someone will develop a disease (Parrott & Smith, 2014). Stronger genetic essentialism may be associated with more social divisions, as the belief provides a rationale for justifying people as inherently different. As it increases divisions, genetic essentialism may be positively associated with stigma beliefs about AATD. Genetic essentialism may also facilitate identification with genetic-based groups, as it provides a profound basis for similarity. Genetic essentialism, then, may not only facilitate considering groups based on shared genes, but also tie one’s inherent place and self-definition to the genetic-health group. We hypothesized:
H4: Stronger genetic essentialism is associated with a) stronger public stigma about AATD and b) stronger group identification with the Alpha-1 community.
Method
Participants and Procedures
Participants were recruited through the Alpha-1 Research Registry at the Medical University of South Carolina (MUSC) in May, 2015. The study was approved by institutional review boards at MUSC and the authors’ university. The registry included 4,927 members; 2,288 members were 21 years old or older, willing to be contacted for research, preferred to be contacted by email, and provided working emails. The recruitment invitations and a link to an online survey were e-mailed to registered members of any phenotype who were 21 years of age or older. The survey included different sections for married and unmarried members. After agreeing to the consent form, participants were asked, “What is your relationship status?” If participants were single, committed, separated, divorced or widowed, they were directed to the questionnaire for unmarried adults; these were the sample for this study. Relative to married adults, a robust disease-based community may be particularly important for unmarried adults with AATD because they cannot obtain support from marital relationships.
Of 2,288 invitations, 433 registry members responded to married or unmarried versions of the survey (18.9%). This response rate approximated average e-mail survey response rates without follow-up e-mail (Yun & Trumbo, 2000). A total of 137 registry members completed the survey for unmarried adults, and the rest of participants completed the survey for married adults. Responses of 3 unmarried participants were dropped due to significant number of missing values (≥ 50%). The final sample included 134 unmarried adults.
Of 134 unmarried participants, 53% had alleles leading to severe deficiency (e.g., ZZ), and 45% had alleles leading to mild deficiency (e.g., MZ). Most were White (97%), which reflects the biology of Alpha-1 (de Serres, Blanco, & Fernandez-Bustillo, 2010). The registry members were mostly female (81.2%). They varied in relationship status (44.8% single, 39.6% divorced, 9.7% widowed, 6% separated) and employment status (51.9% employed). The participants varied in whether they had experienced symptoms associated with Alpha-1 (67.9%), experienced stigmatization due to their genetic condition (21.6%), or attended an Alpha-1 education day at least once (28%). Average age of participants was 53 years (SD=15.01, Median=55, Minimum=23, Maximum=81).
Measures
A confirmatory factor analysis with maximum likelihood estimation was employed to test the scales for public stigma, genetic essentialism, group identification, group activism, secrecy, challenging, perceived stress, and perceived support availability. All factors were allowed to covary, but error terms were not. The criteria for model fit suggested by Holbert and Stephenson (2002) were used for a sample size smaller than 250. The model showed reasonable fit: χ2(df=874, N=134) = 1469.35, p <.05, SRMR=.08, RMSEA=.07 (90% CI: .065, .078).
Public stigma
Twelve items adapted from Link et al. (1989) were used to assess participants’ perceptions of public stereotypes about and reactions to their genetic condition (e.g., Most people will think less of a person diagnosed with a genetic disorder). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.94), with higher scores indicating stronger public stigma about AATD.
Genetic essentialism
Four items (Parrott, Kahl, Ndiaye, & Traeder, 2012) were used to assess participants’ essentialist beliefs about genes (e.g., Genetics play a bigger role in whether you will get liver disease than your lifestyle). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.86), with higher scores indicating more essentialist views of genes’ influence on health.
Group identification
Five items adapted from Spencer-Rogers, Williams, Hamilton, Peng, and Wang (2007) were used to assess the participants’ identification with the Alpha-1 community (e.g., Do you feel like a member of an Alpha-1 community?). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.86), with higher scores indicating stronger identification with Alpha-1 community.
Group activism
Five items adapted from Rogers and colleagues’ (1997) empowerment scale assessed participants’ belief that the Alpha-1 community had the capacity to achieve goals (e.g., By working together, people associated with Alpha-1 can have an effect on the health industry). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.85), with higher scores indicating stronger group activism.
Secrecy
Five items adapted from Link et al. (1989) assessed the extent to which participants’ concealed information about their health condition to avoid stigmatization (e.g., In view of society’s attitudes toward people with genetic disorders, I keep my Alpha-1 test results secret). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.80), with higher scores indicating more secrecy.
Challenging
Five items adapted from Link et al. (2002) assessed participants’ intentions to use communication to confront stigmatizers (e.g., If I thought someone was treating people living with Alpha-1 unfairly, I would try to challenge him/her). Responses (1=strongly disagree, 5=strongly agree) were averaged into one score (α=.85), with higher scores indicating stronger intention to challenge stigmatization.
Perceived stress
Five items from Cohen, Carmack, and Mermelstein (1983) were used to assess the extent to which participants appraised their life as stressful (e.g., Felt difficulties were piling up so high that you could not overcome them). Responses (1= never, 5= frequently) were averaged into one score (α=.92), with higher scores indicating more stress.
Perceived support availability
Three items from Link et al. (1989) were used to assess participants’ perceived number of people to whom they can go for support. These items covered different kinds of supportive tasks such as decision making (e.g., provided you advice when making important decisions) and emotional support (e.g., discussed your personal worries with you). Responses (1= no one, 5= more than 10 people) were averaged into one score (α=.84), with higher scores indicating higher perceived support availability.
Stigmatization experience
Two open-ended questions explored stigmatization experience. Participants were first asked whether they have experienced stigmatization due to AATD. If they answered yes, they were instructed to think about their last experience and describe what happened, who was involved, and how they felt.
Coding
Of 134 participants, 27 answered yes when asked if they had experienced stigmatization. These participants also offered descriptions about their stigmatization experience. Responses were examined with a content analysis. Two coders first unitized each participant’s description (κ=.94). Each unit represents an independent descriptor of participants’ experience, concerns and feelings about stigmatization related to their genetic condition. For example, a response that “my son was angry, refused to get tested, and had an argument with me” was coded as three separate units. Disagreements were discussed by the coders until they reached a consensus. Participants, on average, wrote 5 units (SD = 2.40). The second author read through comments and identified three themes: rejection from family members, friends, and romantic partners; employers’ and health care providers’ discrimination and contempt; and negative judgments that reveal the inaccurate beliefs about AATD. Next, each response was coded by the first author and another coder blind to the research question. A theme was coded ‘one’ if a participant’s response included at least one unit relating to that theme. A theme was coded ‘zero’ if no units were associated with it. For training, a random sample (~20%) was selected, and the coders discussed how each comment could be coded based on the existing categories. After that, each coder independently coded the rest of the open-ended responses, and intercoder reliability indexes were calculated, ranging from .76 to .92. Disagreements were resolved through discussions.
Results
Stigmatization Experience
RQ1 explored the memorable events that people with AATD reported as being stigmatizing. Among 27 participants who reported stigmatization, 48% lived with alleles leading to severe deficiency (e.g., ZZ). About 80% of the sub-sample were female, and 48% were employed. Participants of this sub-sample were, on average, 52 years old (SD = 13.91). The most frequent theme was memorable experiences of rejection from family members, friends, and romantic partners (59%), followed by experiences linked to employers’ and health care providers’ discrimination and contempt (44%). The prevalence of each theme was comparable to that found in studies examining stigmatization against people with other genetic disorders such as Huntington’s disease (Otlowski, Taylor, & Bombard, 2012). About 37% of the participants described experiences with blame and other negative judgments that reveal the inaccuracy of others’ beliefs.
Participants experienced rejection from family members, friends, and romantic partners, including divorce, after getting the test results. One participant reported that her husband decided to leave her because “having a handicapped spouse was not in his wishes for his life.” In another participant’s words,
This was very hard for me because it makes me worried that I will never be able to find a husband/boyfriend who will be ok and accepting of my disease. It is disheartening that this is something that I will never be able to change. It is hard being judged and looked at like I am a broken toy and having people look at my disease and not who I am as a person.
Participants reported that blood relatives reacted to the news of Alpha-1 test results with anger, denial, and attempts to shame and guilt the participant for disclosing the news. A participant reported that family members ignored his advice to get tested for Alpha-1 and called him “a hypochondriac.” Another participant wrote, “My brother was teasing me about it - saying that I wouldn’t be any help (when moving heavy objects in the garage) because I can’t breathe.”
Participants also reported discrimination and contempt from employers and health care providers in relation to their genetic condition, as well as being denied health insurance coverage. Discrimination often occurred in the context of physical activity. For example, one participant reported that his doctor disallowed his deployment with his military unit, even though the participant was able to physically outperform more than 90% of his military unit, and had approval from other health care professionals. Another participant said, “I am not invited to events requiring physical activity. People assume I am sick and can’t do physical activity. People assume I will die sooner rather than later.” Participants experienced contempt when their employers and health care providers did not take their conditions seriously. For example, a participant asked employers to clean the office because dust may accelerate the disease progression. The employers refused the request, and did not think that Alpha-1 was a real disease. The participant was later excluded from all conversation with management about the working environment, and felt “frustrated, angry, and at times humiliated.” Some employers even blamed the people with AATD for their own sufferings—according to one participant, some health professionals dismissed the health condition, and even flat out said that “it’s an excuse to be lazy, and they are just depressed.” In the participant’s words, “Doctors just nod at me like oh here we go, another nut!”
The last theme involved experiences of negative judgements that reveal the inaccuracy of others’ beliefs about AATD. Some participants were told that the condition was a result of sinning against the divine, or that it was actually alcohol abuse. The alternative etiology of alcohol abuse also appeared in misattributing a child’s disease to maltreatment by the parent, instead of to a genetic condition over which the parent had no control. As a participant wrote, “Having a very young child with end stage liver disease, I was frequently criticized and asked how I could give such a young child alcohol.” The participant was also told that the mother must have drunk alcohol while pregnant and that this was irresponsible parenting. Another participant reported being judged negatively because people misunderstood AATD as a contagious disease. Misunderstanding AATD’s etiology also appeared in reports of participants being kept away from their children. One participant said, “Some people would rather make accusations than research the issue.”
Stigma can also occur within a disease community. One participant stated,
It seems that anyone who doesn’t have the ZZ combinations are treated as less and if you don’t have a Z allele at all you’re intentionally excluded. It’s even worse if you’re young or mostly healthy. I have the unfortunate combination of being an SS, young, and mostly healthy. This brands me as an outcast and I’m looked down on and treated as less of an alpha, or not even an alpha at all.
Hypotheses Testing
Descriptive statistics of the variables and their correlations appear in Table 1. H1 focused on the deleterious effects of public stigma on secrecy, perceived support availability, and perceived stress. Stronger public stigma about AATD was associated with more secrecy about genetic test results, lower perceived support availability, and greater perceived stress. H2 and H3 focused on the effects of group cognitions on perceived support availability, perceived stress, and communicative responses to public stigma. Stronger identification with the Alpha-1 community was associated with less secrecy. However, group identification was not associated with perceived stress. Stronger group activism was associated with higher perceived support availability, and more communication to challenge stigmatizers. Group activism was not associated with perceived stress. H4 explored the role of genetic essentialism in public stigma and group cognitions. The results revealed that genetic essentialism was positively associated with public stigma about AATD, and identification with the Alpha-1 community.
Table 1.
Descriptive statistics and zero-order correlations (N = 134)
| M | SD | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Perceived stress | 2.72 | .90 | 1–4.8 | |||||||
| 2. Support availability | 3.05 | .83 | 1–5 | −.21* | ||||||
| 3. Secrecy | 2.41 | .82 | 1–4.4 | .31* | −.26* | |||||
| 4. Challenge | 4.03 | .61 | 1–5 | −.09 | .12 | −.09 | ||||
| 5. Public Stigma | 2.55 | .84 | 1–4.9 | .40* | −.32* | .52* | .05 | |||
| 6. Essentialism | 2.76 | .83 | 1–5 | .16 | −.25* | .01 | .13 | .28* | ||
| 7. Identification | 3.16 | .90 | 1–5 | −.04 | .10 | −.20* | .28* | −.02 | .22* | |
| 8. Group activism | 4.07 | .70 | 1.2–5 | −.16 | .27* | −.15 | .33* | −.05 | −.03 | .39* |
p< .05
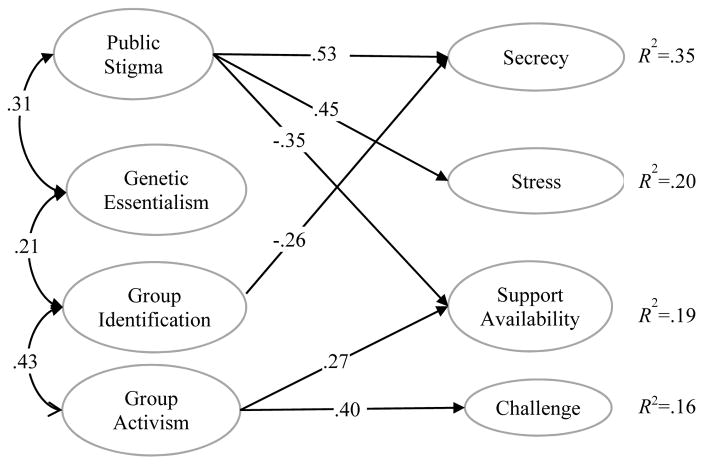
Bivariate correlations may be created spuriously given the associations among stigma beliefs, genetic essentialism, and group cognitions. A structural equation model was run to test the hypotheses. Following Holbert and Stephenson (2002), the correlations in the measurement model were replaced with hypothesized structural paths. The model showed reasonable fit: χ2(df=891, N=134)=1493.94, p<.01, SRMR=.08, RMSEA=.07 (90% CI .06, .08). Not all of the hypothesized paths were statistically significant. Perceived stress was associated with neither identification with Alpha-1 community (β=.04, p=.65) nor group activism (β= −.16, p=.10). These paths were dropped, and the model was run again. The model showed the same goodness of fit: χ2(df=893, N=134)=1485.55, p<.01, SRMR=.086, RMSEA=.07 (90% CI .06, .08). The remaining parameter estimates were significant at p<.05. Results appear in Figure 1. The findings showed that stronger public stigma about AATD and less identification with the Alpha-1 community predicted more secrecy. Furthermore, genetic essentialism was positively associated with public stigma and group identification. Weaker public stigma and stronger group identification predicted higher perceived support availability. Stronger public stigma predicted greater perceived stress. Finally, stronger group activism predicted more communication to challenge stigmatization and stronger identification with the Alpha-1 community. These findings were robust after controlling for demographic variables including sex, age, and phenotypes that may determine the level of deficiency.
Figure 1.
Revised structural equation model. Standardized regression weights appear on the paths; correlations appear on the undirected paths. All parameters were significant at p<.05
Post-Hoc Tests of Moderations
The literature review highlighted the way that people respond to gene-related stigmatization depends on how they perceive public stigma and the support community to which they belong. The results showed that public stigma and group identification predicted secrecy, while group activism was linked to communication to challenge stigmatizers. Using Hayes’ (2013) PROCESS macro for SPSS, we further explored whether group cognitions moderated the relationships between public stigma and communication responses. After controlling for the level of deficiency, sex, and age, the analyses revealed a significant public stigma × group activism interaction (B=0.17, 95% CI: [.02, .32]) on communication to challenge stigmatizers, R2change=.03. Specifically, public stigma was positively associated with communication to challenge stigmatizers when people perceived high group activism (one SD above the mean; B=0.17, 95% CI: [.01, .33]), but not when they perceived group activism as moderate (at the mean; B=0.05, 95% CI: [−.07, .17]) to low (one SD below the mean; B=−0.07, 95% CI: [−.22, .09]). The interaction between public stigma and group identification on communication to challenge stigmatizers was also significant (B=0.14, 95% CI: [.02, .26]), after controlling for the level of deficiency, sex, and age, R2change=.04. Specifically, public stigma was positively associated with communication to challenge stigmatization when people had a strong identification with the Alpha-1 community (B=.16, 95% CI: [.001, .32]), but not when group identification was moderate (B=.04, 95% CI: [−.09, .16]) to low (B=−.09, 95% CI: [−.25, .08]). No significant interactions between public stigma and group cognitions were found for secrecy.
Discussion
The goal of the current study was to investigate how group cognitions about the Alpha-1 community and public stigma were linked to communicative and well-being outcomes of people identified with genes putting them at risk for developing AATD. The key findings, implications for health practitioners, limitations, and directions for future study are discussed next.
Communicative Responses to Public Stigma
Recent advances in communication scholarship have identified strategies people use to respond to public stigma (Meisenbach, 2010). The current study extended the prior research by providing empirical evidence on how public stigma and group cognitions may motivate people to keep stigmatizing conditions secret or use communication to challenge stigmatizers. Results showed that more secrecy was associated with greater public stigma, and stronger genetic essentialist beliefs related to a heightened sense of public stigma. The broader finding was consistent with previous research on other health conditions, including HIV (Smith, Rossetto, & Peterson, 2008), infertility (Steuber & Solomon, 2011), and mental illnesses (Link et al., 1989). It seems likely that fear of negative judgements and the loss of opportunities may make secrecy an appealing strategy in response to stigma. The association between public stigma and secrecy in the current study (r=.52) appears to be stronger than the association reported in the context of HIV (e.g., r=.35 in Berger et al., 2001; |r|=.19 in Smith et al.’s [2008] meta-analysis). This suggests that fear of public stigma may be a particularly strong motive for people with AATD to keep the condition secret. Beliefs that gene determine one’s life course may make genes a core attribute with high salience for affected individuals. For people with rare health conditions such as AATD, secrecy is particularly problematic because it impairs their ability to receive timely treatment and support from network members. While stigma may impede disclosure, the negative association between group identification and secrecy suggested that the sense of attachment to a community of similar others may promote disclosure. The positive relationship between group identification and genetic essentialism reveals a complex dialectic associated with these beliefs: a tension between public stigma and more secrecy versus group identification and less secrecy. A community of similar others may function as a social safety net, where people identifying with the community anticipate fewer risks of devaluation and discrimination.
Consistent with the GCM, group activism was positively associated with communication to challenge stigmatization. Stigma profoundly reduces the value and the power of a social group (Goffman, 1963). Group activism enhances the beliefs that the existing power relationship poses an unfair burden on the well-being of the subordinates and that people can change the status quo by working as a united group (Zoller, 2005). People who perceive stronger activism may be more confident in the legitimacy and efficacy of using communication to challenge stigmatizers, and hence are more likely to use it. Indeed, the significant interactions between group cognitions and public stigma suggested that stigmatized people may be motivated to challenge unfair treatment if they strongly identify with a community of similar others or if they believe in the community’s capacity to achieve goals.
Perceived Stress and Support Availability
Public stigma was associated with a number of factors that may deplete the already-limited resources for people with AATD to cope with illness. As expected, stronger public stigma was associated with higher perceived stress. Notably, essentialist beliefs that contribute to this public stigma may be a harbinger for such stress. The memorable stigmatizing events reported by a sub-group of participants ranged from healthcare to organizational settings and included various manifestations, such as expression of contempt, discrimination, relationship deterioration, and the denial of access to instrumental support.
Neither group identification nor activism was associated with perceived stress. We reasoned that group identification and activism may motivate people to view others with similar conditions as valuable resources, thereby elevating their perceptions of the available coping resources in response to stressors. The current finding may indicate that the support associated with group identification and activism does not match with the unique demands of a stigma-related stressor. For example, perceived stress may not be alleviated much if a person with AATD needs instrumental support to cover the cost of augmentation therapy but receives esteem support from the community through group identification (Rüsch et al., 2009).
Perceived support availability was negatively associated with public stigma, suggesting a further deleterious outcome linked to the arousal of public stigma aligned with genetic essentialist beliefs. The association between stigma and support availability was consistent with a meta-analysis in the context of HIV (Smith et al., 2008), where a moderate, negative correlation was observed (r=−.34). As noted by Smith and colleagues (2008), the operationalization of social support varied among studies, which may account for the heterogeneity in stigma-social support association. The current study focused on one dimension of perceived support: the number of available support providers for a given task. Future studies would benefit from examining the relationship between stigma and other dimensions such as validation, satisfaction, and quality of social support.
Practical Implications
The findings have practical implications for strengthening health communities that garner resources for people with rare health conditions such as AATD. First, enhancing group cognitions such as identification and activism is critical to promote information exchange, enhance perceived support availability, and increase communication to challenge stigmatization. Communication is integral to cultivating strong identification and activism associated with support groups (Cline, 1999). In the case of rare health conditions, communication that enhances genetic essentialist beliefs may prompt identification with groups based on genetic status and promote less secrecy. Communication that creates or intensifies genetic essentialist beliefs, however, risks alerting one to public stigma associated with genetic status. Storytelling is a useful means to enhance group cognitions because it facilitates collective interpretations of illness experience that help create shared norms and values and coordinate the efforts to defend the rights of the group (Cline, 1999). In practice, for example, the monthly magazine of Alpha-1 community has devoted a section specifically for patients’ narratives about their own journey in coping with illness and published stories on how people with AATD and their support network members reached out to policy makers to advocate for relevant bills and appropriations (e.g., “Alphas and caregivers pack FDA” in Alpha-1-to-One magazine, 2015, Volume 13, Issue 3, pp. 6–7). Support group leaders may consider offering platforms and facilitating dialogue that increase members’ identification and activism.
Group identification may not always relate to positive outcomes, as suggested by an incident in which people with alleles leading to mild deficiency reported within-community stigmatization by those with alleles leading to more severe genetic variants. Communicative practices strengthening group identification may unexpectedly create or strengthen the boundaries between insiders and outsiders, which may induce systematic devaluation of a subgroup within the community.
In general, genetic essentialism has been described as an inaccurate belief on the relationship between genes and health, and has been linked a series of problematic outcomes, such as a sense of fatalism and lack of control over health, and limiting personal actions to contour the expression of genes for health (Parrott & Smith, 2014). The finding that genetic essentialism was positively related to group identification is a novel insight into the ramifications of these beliefs. Essentialism’s link to lower perceived support availability and stronger stigma beliefs aligns with prior recommendations to communicate about genes and health in ways that limit genetic essentialism. We echo the advice of Dennis and colleagues (2008), who recommended that community leaders ensure not only that group members have equal opportunities to disclose, but also that members, regardless of backgrounds, are not judged by others.
The current findings also highlight the importance of efficacy information as group members attempt to challenge the status quo. Members may experience increased confidence in challenging social injustice via group activism, but they might not be equipped with efficacious knowledge on how to act. ACT UP (the AIDS Coalition to Unleash Power) is a good example of a disease-based activism group that not only inspires people living with AIDS to challenge stigmatizing beliefs and practices about the disease, but also develops materials to teach members to engage in confrontation and education. For example, ACT UP specifically advised members to learn about the disease by starting a scientific club to discuss what they read and share what they learned before approaching to others. In another document, the organization offered a list of direct actions targeted to change public beliefs about HIV and rated the actions based on the level of social risks (Brashers et al., 2000). Support group leaders may consider including effective and implementable communication strategies in their programs.
Limitations and Future Directions
Several scholars have defined stigma as a multi-dimensional construct (e.g., Berger et al., 2001). In Berger and colleagues’ (2001) conceptualization, for example, stigma involved one’s awareness of actual or potential social disqualification, limited opportunities, and negative change in self-image; it was operationalized as a combination of negative social consequences, disclosure concerns, negative self-image, and concerns about public attitudes. The present study focused on stigmatized people’s concerns about the public’s devaluing and discriminatory reactions (Corrigan, 2004), and cannot speak to other facets of stigma such as the extent to which people with AATD internalize public devaluing and discriminatory conceptions as part of their self-image. It is possible that the development of negative self-image linked to AATD may in part explain why public stigma was negatively associated with lower perceived support availability, with one study finding that negative self-image mediated the relationship between mental illness patients’ public stigma against counseling and their attitudes toward seeking support (Vogel, Wade, & Hackler, 2007). Without direct measures on internalized stigma, the current study is limited in addressing participants’ feelings and the consequences of other people knowing their disease status.
Our cross-sectional data cannot offer causal insights into the relationships among the variables of interest. For example, although perceived support availability was tested as a dependent variable, it is possible that greater perceptions of support availability lead to a reduced perception of stigma. As noted by one reviewer, it is also possible that communication with similar others increases one’s identification with the community.
Another limitation is that recruiting participants from the research registry may introduce selection bias. It is likely that people who participated in the registry have higher group activism and lower perceived stigma than those who did not participate in the community. Indeed, the means for group activism and intention to challenge stigmatization were both around four on five-point scales, while means for stigma were lower than the mid-point of the scale.
Finally, the present study did not have data on the members’ participation in different support groups within the community. The Alpha-1 community involves various groups that offer social support, such as virtual support groups, face-to-face meetings, national conferences, regional education days, and events for support leaders. Each group and the means of support has unique strengths. For example, computer-mediated support may be particularly useful in garnering support from weak ties (i.e., individuals without a close personal relationship; Wright & Rains, 2013). Future research would benefit from investigating participants’ affiliations with different support groups and how participants’ group cognitions and well-being outcomes vary as a function of group characteristics.
Conclusions
People with rare diseases such as AATD have difficulty garnering resources critical for their health and well-being. Public stigma was related to a number of factors that deplete already-limited resources. People with rare health conditions often build communities with others who share their conditions. The results of this study provided evidence that group cognitions were associated with communication strategies in response to public stigma. While some scholars hold a pessimistic view that “the actions of single individuals are very unlikely to change the power difference between stigmatized and stigmatizing groups” (Link, Phelan, & Hatzenbuehler, 2014, p. 60), we remain optimistic about the potential for designing communication interventions to enhance beliefs about an active, united support group in alleviating the deleterious effects of stigma.
Acknowledgments
This project was supported by the National Human Genome Research under Award number R21HG007111 and by the National Institute on Drug Abuse under Award number P50-DA010075-16. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Amanda Applegate for her feedback on an earlier version of this paper, two anonymous reviewers for their constructive comments, and Xuan Ma for her assistance with coding. We are grateful to the members of the Alpha-1 Research Registry for sharing their thoughts and experience with us.
Contributor Information
Xun Zhu, Communication Arts & Sciences, Pennsylvania State University, 316 Sparks Building, University Park, PA 16802.
Rachel A. Smith, Communication Arts & Sciences, Pennsylvania State University, 216 Sparks Building, University Park, PA 16802, (814) 865-4201
Roxanne L. Parrott, Communication Arts & Sciences and Health Policy & Administration, Pennsylvania State University
References
- Barkowski S, Schwartze D, Strauss B, Burlingame GM, Barth J, Rosendahl J. Efficacy of group psychotherapy for social anxiety disorder: A meta-analysis of randomized-controlled trials. Journal of Anxiety Disorders. 2016;39:44–64. doi: 10.1016/j.janxdis.2016.02.005. [DOI] [PubMed] [Google Scholar]
- Barlow SH, Burlingame GM, Nebeker RS, Anderson E. Meta-analysis of medical self-help groups. International Journal of Group Psychotherapy. 2000;50:53–69. doi: 10.1080/00207284.2000.11490981. Retrieved from http://www.tandfonline.com/loi/ujgp20#.VwQlz_krKUk. [DOI] [PubMed] [Google Scholar]
- Barreto M. Experiencing and coping with social stigma. In: Mikulincer M, Shaver PR, Dovidio JF, Simpson JA, editors. APA handbook of personality and social psychology, volume 2: Group processes. Washington, DC: American Psychological Association; 2014. pp. 473–506. [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Berger BE, Kapella MC, Larson JL. The experience of stigma in chronic obstructive pulmonary disease. Western Journal of Nursing Research. 2011;33:916–932. doi: 10.1177/0193945910384602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brashers E, Haas M, Klingle S, Neidig L. Collective AIDS activism and individuals’ perceived self-advocacy in physician-patient communication. Human Communication Research. 2000;26:372–402. doi: 10.1093/hcr/26.3.372. [DOI] [Google Scholar]
- Burleson BR, MacGeorge EL. Supportive communication. In: Knapp ML, Daly JA, editors. Handbook of Interpersonal Communication. 3. Thousand Oaks, CA: Sage; 2002. pp. 374–424. [Google Scholar]
- Burlingame GM, Fuhriman A, Mosier J. The differential effectiveness of group psychotherapy: A meta-analytic perspective. Group Dynamics: Theory, Research, and Practice. 2003;7:3–12. doi: 10.1037/1089-2699.7.1.3. [DOI] [Google Scholar]
- Cline RJW. Communication in support groups. In: Frey LR, Gouran DS, Poole MS, editors. The handbook of group communication theory and research. Thousand Oaks, CA: Sage; 1999. pp. 516–538. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:386–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Correll J, Park B. A model of the ingroup as a social resource. Personality and Social Psychology Review. 2005;9:341–359. doi: 10.1207/s15327957pspr0904_4. [DOI] [PubMed] [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. American Psychologist. 2004;59:614–625. doi: 10.1037/0003-066x.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Faber D, Rashid F, Leary M. The construct validity of empowerment among consumers of mental health services. Schizophrenia Research. 1999;38:77–84. doi: 10.1016/s0920-9964(98)00180-7. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002;9:35–53. doi: 10.1093/clipsy.9.1.35. [DOI] [Google Scholar]
- Cutrona CE, Russell DW. Type of social support and specific stress: Toward a theory of optimal matching. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: An interactional view. Oxford: John Wiley & Sons; 1990. pp. 319–366. [Google Scholar]
- de Serres FJ, Blanco I, Fernandez-Bustillo E. Ethnic differences in alpha-1 antitrypsin deficiency in the United States of America. Therapeutic Advances in Respiratory Disease. 2010;4:63–70. doi: 10.1177/1753465810365158. [DOI] [PubMed] [Google Scholar]
- Dennis MR, Kunkel A, Keyton J. Problematic integration theory, appraisal theory, and the Bosom Buddies breast cancer support group. Journal of Applied Communication Research. 2008;36:415–436. doi: 10.1080/00909880802094315. [DOI] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall; 1963. [Google Scholar]
- Gottlieb BH, Wachala ED. Cancer support groups: a critical review of empirical studies. Psycho-Oncology. 2007;16:379–400. doi: 10.1002/pon.1078. [DOI] [PubMed] [Google Scholar]
- Greene K. An integrated model of health disclosure decision making. In: Afifi TD, Afifi WA, editors. Uncertainty and information regulation in interpersonal contexts: Theories and applications. New York, NY: Routledge; 2009. pp. 226–253. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- Holbert RL, Stephenson MT. Structural equation modeling in the communication sciences, 1995–2000. Human Communication Research. 2002;28:531–551. doi: 10.1093/hcr/28.4.531. [DOI] [Google Scholar]
- Jones NL, Sarata AK. Report for Congress. Genetic information: Legal issues relating to discrimination and privacy. 2008 Retrieved from http://biotech.law.lsu.edu/crs/R-L30006_20080310.pdf.
- Klitzman R. Views of discrimination among individuals confronting genetic disease. Journal of Genetic Counseling. 2010;19:68–83. doi: 10.1007/s10897-009-9262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman RL, Sweeney MM. “In sickness and in health”? Disclosures of genetic risks in dating. Journal of Genetic Counseling. 2011;20:98–112. doi: 10.1007/s10897-010-9331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review. 1989;54:400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- Link BG, Phelan J. Stigma and its public health consequences. Lancet. 2006;367:528–529. doi: 10.1016/s0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC, Hatzenbuehler ML. Stigma and social inequality. In: McLeod JD, Lawler E, Schwalbe M, editors. Handbook of the social psychology of inequality. Dordrech, Netherlands: Springer; 2014. pp. 49–64. [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. On describing and seeking to change the experience of stigma. Psychiatric Rehabilitation Skills. 2002;6:201–231. doi: 10.1080/10973430208408433. [DOI] [Google Scholar]
- Meisenbach R. Stigma management communication: A theory and agenda for applied research on how individuals manage moments of stigmatized identity. Journal of Applied Communication Research. 2010;38:268–292. doi: 10.1080/00909882.2010.490841. [DOI] [Google Scholar]
- National Institutes of Health. Contact Information for Rare Disease Advocacy Organizations. 2015 Retrieved from https://rarediseases.info.nih.gov/resources/5/support-for-patients-and-families#category15.
- Otlowski M, Taylor S, Bombard Y. Genetic discrimination: International perspectives. Annual Review of Genomics and Human Genetics. 2012;13:433–454. doi: 10.1146/annurev-genom-090711-163800. [DOI] [PubMed] [Google Scholar]
- Parrott R, Kahl M, Ndiaye K, Traeder T. Health communication, genetic determinism, and perceived control: The role of beliefs about disease susceptibility and severity versus disease essentialism. Journal of Health Communication. 2012;17:762–768. doi: 10.1080/10810730.2012.677301. [DOI] [PubMed] [Google Scholar]
- Parrott RL, Smith RA. Defining genes using “blueprint” versus “instruction” metaphors: Effects for genetic determinism, response efficacy, and perceived control. Health Communication. 2014;29:137–146. doi: 10.1080/10410236.2012.729181. [DOI] [PubMed] [Google Scholar]
- Parrott RL, Smith RA, Hong SJ, Worthington A. Congruence-incongruence patterns in alpha-1 antitrypsin deficiency couples’ genetic determinist beliefs and perceived control over genes: Implications for clinical and public health genomic communication. Journal of Genetic Counseling. 2015;24:532–540. doi: 10.1007/s10897-014-9786-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BL, Pescosolido BA. Social network dynamics and biographical disruption: The case of “First-timers” with mental illness. American Journal of Sociology. 2012;118:134–175. doi: 10.1086/666377. [DOI] [Google Scholar]
- Rains S, Young V. A meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Human Communication Research. 2009;35:309–336. doi: 10.1111/j.1468-2958.2009.01353.x. [DOI] [Google Scholar]
- Rogers E, Chamberlin J, Ellison M, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatric Services. 1997;48:1042–1047. doi: 10.1176/ps.48.8.1042. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Corrigan PW, Wassel A, Michaels P, Olschewski M, Wilkniss S, Batia K. Ingroup perception and responses to stigma among persons with mental illness. Acta Psychiatrica Scandinavica. 2009;120:320–328. doi: 10.1111/j.1600-0447.2009.01403.x. [DOI] [PubMed] [Google Scholar]
- Smith RA. Language of the lost: An explication of stigma communication. Communication Theory. 2007;17:462–485. doi: 10.1111/j.1468-2885.2007.00307.x. [DOI] [Google Scholar]
- Smith RA, Parrott RL, Wienke SE. Keeping secrets or educating others: A dyadic analysis of group entitativity’s influence on spouses’ label management connected to AATD. Health Communication. 2016;31:150–160. doi: 10.1080/1041023-6.2014.940671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RA, Rossetto K, Peterson BL. A meta-analysis of perceived stigma, disclosure of one’s HIV+ status, and perceived social support. AIDS Care. 2008;20:1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- Spencer-Rodgers J, Williams MJ, Hamilton DL, Peng K, Wang L. Culture and group perception: Dispositional and stereotypic inferences about novel and national groups. Journal of Personality and Social Psychology. 2007;93:525–543. doi: 10.1037/0022-3514.93.4.525. [DOI] [PubMed] [Google Scholar]
- Steuber KR, Solomon DH. Relational uncertainty, partner interference, and privacy boundary turbulence: Explaining spousal discrepancies in infertility disclosures. Journal of Social and Personal Relationships. 2011;29:3–27. doi: 10.1177/0265407511406896. [DOI] [Google Scholar]
- Stoller J, Aboussouan L. A review of α1-antitrypsin deficiency. American Journal of Respiratory and Critical Care Medicine. 2011;185:246–259. doi: 10.1164/rccm.201108-1428CI. [DOI] [PubMed] [Google Scholar]
- Stoller JK, Smith P, Yang P, Spray J. Physical and social impact of alpha 1-antitrypsin deficiency: Results of a survey. Cleveland Clinic journal of medicine. 1994;61:461–467. doi: 10.3949/ccjm.61.6.461. [DOI] [PubMed] [Google Scholar]
- Trouiller P, Olliaro P, Torreele E, Orbinski J, Laing R, Ford N. Drug development for neglected diseases: A deficient market and a public-health policy failure. The Lancet. 2002;359:2188–2194. doi: 10.1016/s0140-6736(02)09096-7. [DOI] [PubMed] [Google Scholar]
- Valdez R, Ouyang L, Bolen J. Public health and rare diseases: Oxymoron no more. Preventing Chronic Disease. 2016;13:E05. doi: 10.5888/pcd13.150491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, Hackler AH. Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology. 2007;54:40–50. doi: 10.1037/0022-0167.54.1.40. [DOI] [Google Scholar]
- Walsh JW. How patients learned to control their own future. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2013;10:57–59. doi: 10.3109/15412555.2013.763783. [DOI] [PubMed] [Google Scholar]
- Wright KB. Computer-mediated support groups: An examination of relationships among social support, perceived stress, and coping strategies. Communication Quarterly. 1999;47:402–414. doi: 10.1080/01463379909385570. [DOI] [Google Scholar]
- Wright K. Perceptions of on-line support providers: An examination of perceived homophily, source credibility, communication and social support within on-line support groups. Communication Quarterly. 2000;48:44–59. doi: 10.1080/01463370009385579. [DOI] [Google Scholar]
- Wright K, Rains S. Weak-tie support network preference, health-related stigma, and health outcomes in computer-mediated support groups. Journal of Applied Communication Research. 2013;41:309–324. doi: 10.1080/00909882.2013.792435. [DOI] [Google Scholar]
- Yun GW, Trumbo CW. Comparative response to a survey executed by post, email, and web form. Journal of Computer-Mediated Communication. 2000;6 Retrieved from http://jcmc.indiana.edu/vol6/issue1/yun.html. [Google Scholar]
- Zoller HM. Health activism: Communication theory and action for social change. Communication Theory. 2005;15:341–364. doi: 10.1093/ct/15.4.341. [DOI] [Google Scholar]