Abstract
Dislocation of the sternoclavicular joint is a rare injury and typically requires high-energy forces applied through the joint. Initial treatment is dependent on the direction of dislocation, with acute reduction indicated for posterior dislocations presenting with signs of tracheal, esophageal, or neurovascular compression. Although most patients do well with conservative treatment after the initial trauma, some can have persistent pain and scapular dyskinesia due to instability or locked dislocation of the sternoclavicular joint. Stabilization of the sternoclavicular joint with reconstruction may be indicated for those with persistent symptoms despite a trial of steroid injections and physical therapy. In this report and video, we present a figure-of-8 reconstruction technique to reduce and stabilize a posterior dislocation of the sternoclavicular joint using a gracilis autograft. Ultimately, this reconstruction technique can be performed in a safe, efficient, and reliable manner when appropriate surgical steps are followed.
The sternoclavicular joint (SCJ) is a pivotal articulation for movement of the shoulder girdle. It translates anteriorly and posteriorly for clavicular protraction and retraction, superior and inferiorly for elevation, and may rotate by as much as 40° around its longitudinal axis during combined movements.1 Although less than half of the medial clavicular surface articulates with the corresponding articular facet on the sternum, the SCJ is remarkably stable because of the interclavicular ligament, costoclavicular ligament, the intra-articular meniscal band, and joint capsule.
Dislocation of the SCJ is a rare injury and typically requires high-energy forces applied directly or indirectly to the joint. Although anterior sternoclavicular dislocations are more common because of the strength of the posterior joint capsule, posterior sternoclavicular dislocations tend to be more morbid because of the risk of tracheal, esophageal, or neurovascular compression. Even after appropriate treatment of the initial dislocation, patients can occasionally have persistent SCJ instability that may present as pain and scapular dyskinesia.1 Moreover, those with locked SCJ dislocations may complain of shoulder stiffness as a result of limited mobility of the medial clavicular hinge. SCJ reconstruction to reduce and stabilize the joint may be indicated for those with persistent symptoms despite a trial of conservative treatment.
Several different techniques for SCJ reconstruction have been described. These procedures require sound knowledge of neighboring anatomy, including the subclavian vessels and supraclavicular brachial plexus posterolaterally and the trachea and esophagus posteromedially, to avoid damaging these structures. We describe a figure-of-8 reconstruction technique using gracilis autograft for a patient with a chronic locked posterior SCJ dislocation (Fig 1).
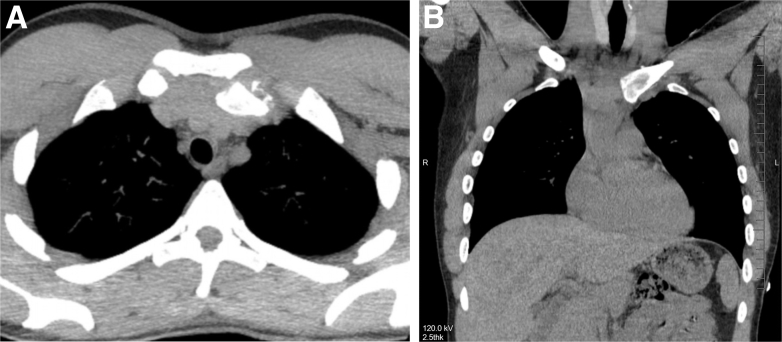
Fig 1.
Axial (A) and coronal (B) computed tomography images show a chronic left sternoclavicular joint dislocation that is locked posteriorly.
Technique
Patient Positioning and Gracilis Harvest
The patient is placed in a beach-chair position with the shoulder, entire length of the clavicle, and SCJ exposed. The arm may be placed in an arm holder or on top of a padded Mayo stand based on surgeon preference. The ipsilateral lower leg is also prepped and draped (Fig 2A). The gracilis is harvested using standard technique.2 Briefly, a 2-cm vertical incision is made at the level of the pes anserinus insertion. The sartorius fascia is incised and elevated, exposing the tendons on the undersurface. The gracilis tendon is isolated using a right-angled clamp and harvested with an open-ended tendon stripper. Typically, a minimum graft length of 16 cm is necessary to provide enough tendon overlap to the figure-of-8 configuration and apply tension to the limbs. The graft is then taken to the back table and cleared of all muscle tissue with a large periosteal elevator or ruler. Larger tendons may require trimming to allow for easy passage of the graft through a 4.8-mm-diameter tunnel. A no. 2 FiberWire (Arthrex, Naples, FL) locking whipstitch suture is placed in a small portion of both free ends of the tendon to allow for ease of passage and tensioning (Fig 2B). The graft is then stored in a saline-soaked gauze wrap until later passage.
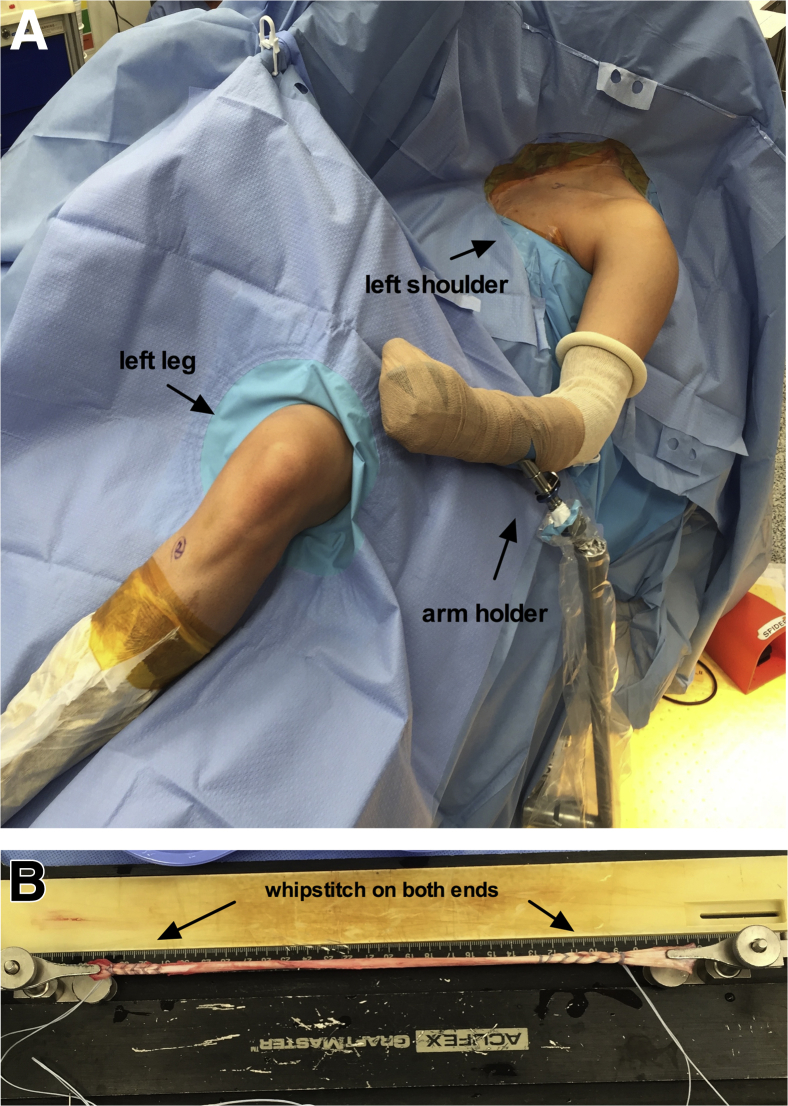
Fig 2.
Patient positioning and graft preparation. (A) The patient is placed in a beach-chair position with the left shoulder, entire length of the clavicle, and sternoclavicular joint exposed. The left lower leg is also prepped and draped for gracilis harvest. (B) The gracilis graft is prepared with a no. 2 FiberWire locking whipstitch suture on each end to allow for ease of passage and tensioning. The graft should pass easily through a 4.8-mm-diameter tunnel.
Sternoclavicular Joint Reconstruction
A 10-cm transverse skin incision is made centered over the SCJ and taken down through the subcutaneous tissues. The medial edge of the clavicle and manubrium are exposed subperiosteally. In chronic injuries, abundant callus and scar tissue may be present. This callus and scar, which can be adherent to the underlying brachiocephalic trunk and other posterior structures, should be gently detached to facilitate reduction of the joint (Fig 3A). Care is taken to ensure that dissection around the medial clavicle is performed in a subperiosteal fashion to protect the underlying neurovascular structures (Table 1). A bone clamp can be placed around the midclavicle to elevate the articulating end away from the posterior structures to remove the callus (Video 1). To fully reduce the SCJ, a small portion (5 mm) of the medial clavicle may require resection. After callus and scar removal, the joint is identified, and the intra-articular disc is removed.
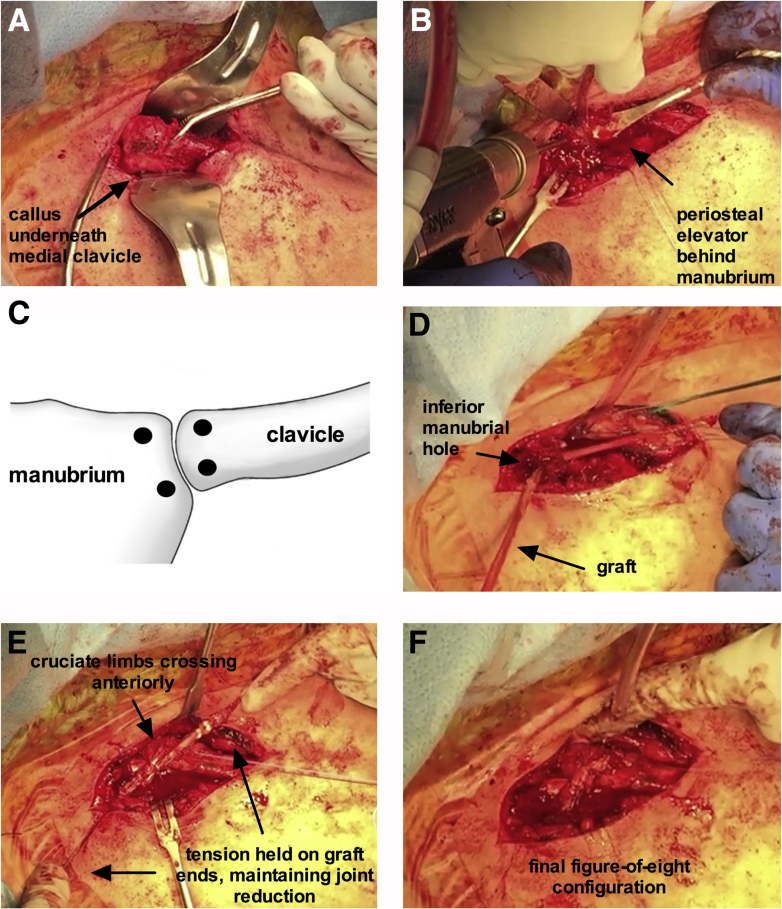
Fig 3.
Steps for left sternoclavicular joint reconstruction with the patient in the beach-chair position. (A) After careful subperiosteal dissection of the sternoclavicular joint, abundant callus inferior to the medial edge of the clavicle is encountered. Reduction was only possible after removal of this callus and scar tissue. (B) A large periosteal elevator is placed behind the manubrium when drilling to protect the underlying structures. (C) A total of 4 bone tunnels are drilled (2 each in the manubrium and clavicle). (D) The gracilis autograft is first passed from anterior to posterior through the inferior manubrial hole. (E) After passage through all 4 holes, the limbs of the graft are crossed over anterior to the joint and tension to the graft ends is applied, maintaining reduction of the joint. (F) After securing the graft to itself, the excess ends of the graft are cut.
Table 1.
Pearls and Pitfalls of Figure-of-8 Reconstruction Technique
|
|
Adequate reduction of the joint should be achievable before proceeding with drilling of the bone tunnels. Prior to drilling, a large periosteal elevator is placed directly beneath the manubrium and clavicle to protect from penetrating into posterior structures (Fig 3B, Video 1). First, 2 parallel 4.8-mm-diameter bone tunnels are drilled along the articulating edge of the manubrium from anterior to posterior. Care should be taken to avoid entering the joint. This process is repeated along the articulating edge of the medial clavicle (Fig 2C). After drilling, a small curette is used to clear bony debris and chamfer the edges of the tunnels to ease passage of the graft. Shuttling sutures (No. 0 Vicryl; Ethicon, Somerville, NJ]) are placed in each bone tunnel matching the direction of graft passage (Fig 4) and temporarily held with clamps.
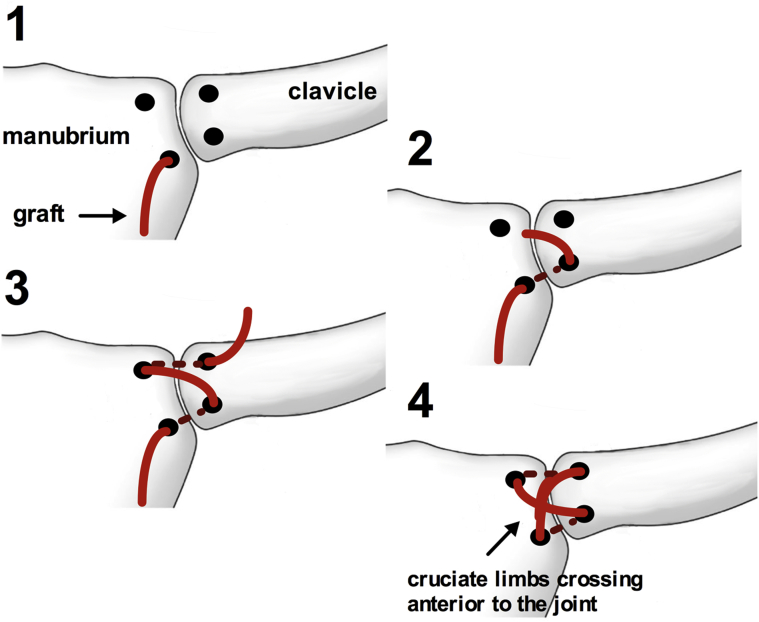
Fig 4.
Steps for graft passage to create figure-of-8 configuration for a left sternoclavicular joint reconstruction. The graft (red) is first passed from anterior to posterior through the inferior manubrial hole (step 1) and then posterior to anterior through the inferior clavicular hole (step 2). The graft is then crossed over the joint anteriorly and passed from anterior to posterior through the superior manubrial hole (step 3) and then from posterior to anterior through the superior clavicular hole (step 4). The cruciate limbs should both cross anterior to the sternoclavicular joint.
The graft is then taken from the back table and passed in a figure-of-8 pattern, with the cruciate limbs crossing over the joint anteriorly (Figs 3E and 4). First, using the shuttling sutures, the graft is passed from anterior to posterior through the inferior manubrial hole and then from posterior to anterior through the inferior clavicular hole. The graft is then crossed over the joint anteriorly and passed from anterior to posterior through the superior manubrial hole. Lastly, the graft is passed from posterior to anterior through the superior clavicular hole (Fig 4). The graft should slide freely through all the bone tunnels. The 2 free limbs of the graft are crossed anteriorly over the SCJ. Using the traction sutures at each end of the tendon, tension is held on the crossed graft (Fig 3E, Video 1); if the graft is able to slide freely through all 4 tunnels, the SCJ should reduce with this maneuver. Although an assistant is holding traction on the graft ends to maintain reduction of the joint, numerous no. 2 Ethibond sutures are placed in an interrupted fashion between different limbs of the figure-of-8 to secure the graft to itself (Fig 3F, Video 1). After ensuring adequate stability of the joint and graft tension, the free ends of the tendon are cut. The reconstructed SCJ is once again inspected before irrigation and wound closure in layers.
Rehabilitation
Postoperatively, the patient's arm is immobilized in a sling for a minimum of 4 weeks with pendulum exercises permitted. After 4 weeks, active-assisted motion is progressed with initial maximal abduction to 90°. Range of motion and weight bearing is then progressed according to clinical course. Return to high-level activities and athletics is initiated on an individual patient basis but typically is avoided for a minimum of 12 weeks after surgery.
Discussion
The myriad of techniques described for SCJ reconstruction likely indicates the lack of consensus on the optimal treatment. Although the current literature is limited to small case series because of the rarity of the injury and success of conservative treatment, the results of a few SCJ reconstruction techniques have been reported and deserve mention. Lyons and Rockwood3 reported 14 major vascular injuries resulting in 8 deaths due to the migration of smooth and threaded pins used to stabilize 21 anterior SCJ dislocations. As a result, pin transfixation across the SCJ is absolutely contraindicated because of the potential for catastrophic complications. Other authors have described techniques that reconstruct the costoclavicular ligament because of reports of better outcomes when this ligament is intact after medial clavicle resection.4, 5 We perform our technique because of biomechanical evidence that the figure-of-8 reconstruction confers superior stability compared with other techniques, particularly in the posterior direction.6 Additionally, we prefer using autologous tendon rather than allograft to reduce the risk of infection, maximize healing potential, and facilitate long-term tissue integration (Table 2). Recently, Kusnezov et al.7 reported a faster return to full duty in young active military service members who underwent figure-of-8 autograft reconstruction compared with those who underwent allograft reconstruction. Ultimately, this reconstruction technique can be performed in a safe, efficient, and reliable manner when appropriate surgical steps are followed.
Table 2.
Advantages and Disadvantages of Figure-of-8 Reconstruction Technique
|
|
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.S.D. is a consultant for Arthrex, Conmed Linvatec, and Ossur and receives royalties from Wolters Kluwer Health. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Figure-of-8 reconstruction technique for a chronic left posterior sternoclavicular joint dislocation. After gracilis harvest, the sternoclavicular joint is exposed and reduced. Two bone tunnels are drilled in the manubrium and clavicle each, and the graft is passed through in a figure-of-8 fashion and secured.
References
- 1.Sewell M.D., Al-Hadithy N., Le Leu A., Lambert S.M. Instability of the sternoclavicular joint: Current concepts in classification, treatment and outcomes. Bone Joint J Br. 2013;95:721–731. doi: 10.1302/0301-620X.95B6.31064. [DOI] [PubMed] [Google Scholar]
- 2.Kern M., Love D., Cotter E.J., Postma W. Quadruple-bundle semitendinosus-gracilis graft technique for all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1317–e1320. doi: 10.1016/j.eats.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lyons F.A., Rockwood C.A., Jr. Migration of pins used in operations on the shoulder. J Bone Joint Surg Am. 1990;72:1262–1267. [PubMed] [Google Scholar]
- 4.Booth C.M., Roper B.A. Chronic dislocation of the sternoclavicular joint: An operative repair. Clin Orthop Relat Res. 1979;140:17–20. [PubMed] [Google Scholar]
- 5.Morell D.J., Thyagarajan D.S. Sternoclavicular joint dislocation and its management: A review of the literature. World J Orthop. 2016;7:244–250. doi: 10.5312/wjo.v7.i4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spencer E.E., Jr., Kuhn J.E. Biomechanical analysis of reconstructions for sternoclavicular joint instability. J Bone Joint Surg Am. 2004;86:98–105. doi: 10.2106/00004623-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Kusnezov N., Dunn J.C., DeLong J.M., Waterman B.R. Sternoclavicular reconstruction in the young active patient: Risk factor analysis and clinical outcomes at short-term follow-up. J Orthop Trauma. 2016;30:e111–e117. doi: 10.1097/BOT.0000000000000483. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure-of-8 reconstruction technique for a chronic left posterior sternoclavicular joint dislocation. After gracilis harvest, the sternoclavicular joint is exposed and reduced. Two bone tunnels are drilled in the manubrium and clavicle each, and the graft is passed through in a figure-of-8 fashion and secured.