Abstract
We sought to examine if self-reported oral health conditions regarding difficulty eating tough foods, dry mouth, choking, number of teeth and denture use are associated with incident falls. Our study was based on panel data from the Japan Gerontological Evaluation Study conducted in 2010 and 2013 using self-administered questionnaires. Data from 19,995 male and 20,858 female community-dwelling older people aged ≥65 years without a history of falls within the previous year in 2010 were analyzed. Multilevel logistic regression models were used to determine the association between poor oral health in 2010 and multiple incident falls in 2013 after adjusting for possible confounders and considering differences in municipalities. The percentage of males and females who reported falls in 2013 were 2.4% and 2.1%, respectively. After adjusting for age, educational attainment, equivalized income, depression, self-rated health, instrumental activities of daily living, body mass index, present illness related to falls, social participation, walking in min/day, alcohol drinking status, and municipality population density, dry mouth in males (odds ratio [OR] = 1.41; 95% confidence interval [CI]: 1.12–1.77) and choking in females (OR = 1.64; 95% CI: 1.27–2.11) were significantly associated with incident falls. Difficulty eating tough foods in both sexes and choking in males were marginally associated with incident falls (p<0.1). Females having 10–19 teeth without dentures (OR = 1.63; 95% CI: 1.14–2.31), ≤9 teeth with dentures (OR = 1.36; 95% CI: 1.03–1.80), and ≤9 without dentures (OR = 1.46; 95% CI: 1.02–2.08) were significantly associated with incident falls compared with those having ≥20 teeth, respectively. These findings suggest that poor oral function, having fewer teeth, and not using dentures are predictors of incident falls. Further studies are needed to determine whether improving oral health can reduce the risk of falls.
Introduction
As the world’s population continues to age, falls are becoming an increasingly major public health problem. In England, it has been reported that approximately 28–35% of older people aged ≥65 years experienced a fall in the previous year [1,2]. Injuries from falls can range from light bruises to hip fractures, and can even result in death [3]. At least 10% of fallers in the U.S. experienced serious injuries [4]. In addition, falls and fractures account for 12.2% of all causes leading to the need for long-term care among older people in Japan [5].
It is therefore important to identify risk factors for falls. Although little can be done about biological risk factors such as age, sex, and chronic illness, behavioral risk factors such as lack of exercise and medication use can be modified by interventions and changes in individual behavior [6]. One recent study revealed that having a low number of teeth and not using dentures were associated with a higher frequency of falls [7]. A longitudinal study involving 4,425 community-dwelling older people showed that those having ≤19 teeth without dentures had a significantly higher risk for incident falls than those having ≥20 teeth [7].
However, the association between oral function and falls remains controversial. One cross-sectional study involving 87 older people showed an association between a decrease in occlusal function and postural instability [8]. Another longitudinal study involving 348 older people showed that occlusal disharmony is a risk factor for a decrease in balance function [9]. A cross-sectional study involving 34 frail older people showed that lower occlusal force was associated with a higher risk of falls, as assessed using a 21-item fall risk index [10]. On the other hand, a longitudinal study found no significant associations between self-reported chewing ability and incident falls [7].
Swallowing is another oral function closely linked to chewing ability because it follows mastication and bolus formation. Saliva production also contributes to mastication, bolus formation, and swallowing [11]. Questions regarding three oral functions, difficulty eating tough foods, dry mouth and choking are included on the basic screening checklist for frail older people in the Japanese long-term care insurance system [12]. A cross-sectional study reported that these questions were significantly associated with falls [13]; however, their temporal relationship remains unknown. If a decline in oral function is found to precede falls, it could become an accurate predictor of falls and be useful for collaborating oral health and fall prevention in older people from the perspective of health policy.
Therefore, the present study investigated the association between oral function and incident falls using longitudinal data from community-dwelling older people. In addition, it has been suggested that falls show regional differences [14], so the association between number of teeth and/or denture use and incident falls was also investigated to verify the reproducibility of the results of a previous study [7] using a large sample and multilevel logistic regression models.
Materials and methods
Study population
Data from a longitudinal study, collected as part of the Japan Gerontological Evaluation Study (JAGES) project, an ongoing Japanese prospective cohort study [15,16], were used for the present study. The JAGES aims to investigate factors associated with the loss of healthy years, such as functional decline, cognitive impairment, and death among non-institutionalized older people. The JAGES sample was restricted to those who did not already have physical or cognitive disability at baseline, which was defined as not receiving long-term public care insurance benefits and having self-reported dependence in walking, toileting, and bathing.
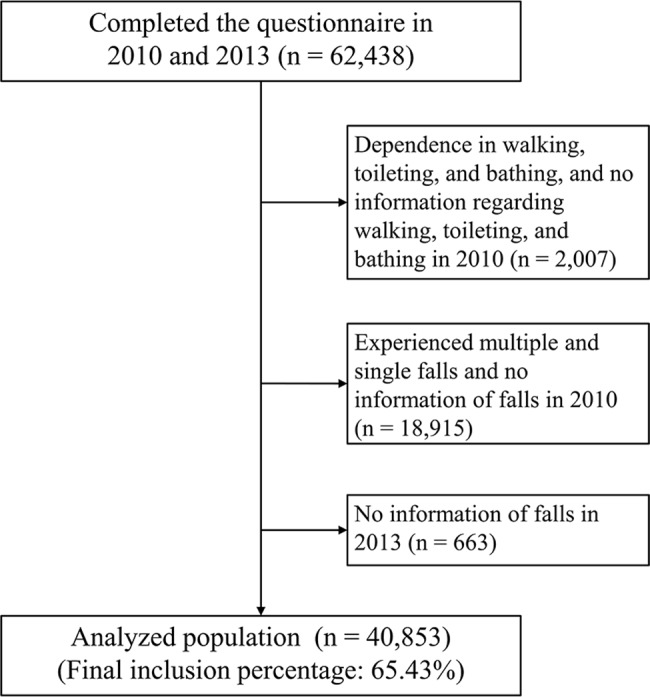
Our analyses used the panel data from two surveys. The baseline survey was conducted between August 2010 and January 2012 among 141,452 people aged ≥65 years. Self-administered questionnaires were mailed to the entire population of 10 municipalities, and randomly to selected residents in 14 municipalities based on the official residential registers obtained from the respective municipal governments. A total of 92,272 people responded to the questionnaires (response rate: 65.2%). A follow-up survey using self-administered questionnaires was conducted between October 2013 and December 2013 on the same respondents in the same municipalities. Collectively, 62,438 individuals completed both the 2010 and 2013 questionnaires. Data from 40,853 respondents (19,995 males and 20,858 females) were used for the analyses after excluding those from 2,007 who already had self-reported dependence in walking, toileting, and bathing at baseline, 16,240 who had experienced single or multiple falls at baseline, 2,675 who provided no information on falls at baseline, and 663 who provided no information on falls at follow-up (Fig 1. Flow chart of the participant selection process). The JAGES protocol was reviewed and approved by the Nihon Fukushi University Ethics Committee (No. 10–05), and the Ethical Committee of Kanagawa Dental University (No. 466) approved the analysis of data in the present study.
Fig 1. Flow chart of the participant selection process.
Outcome variables
The incidence of falls was determined by asking, “How many times have you fallen within the past year?”, with possible answers of “multiple times”, “once”, or “none”. Multiple falls was utilized as an outcome after combining the last two categories because previous studies have shown that single fallers are more similar to nonfallers than to recurrent fallers on a range of medical, physical, and psychological risk factors [17–19].
Oral health variables
Oral function, including difficulty eating tough foods, dry mouth, and choking, and dental status were assessed using self-administered questionnaires. Difficulty eating tough foods, dry mouth, and choking were determined by asking, “Do you have any difficulties eating tough foods now compared with 6 months ago?”, “Do you often have dry mouth?”, and “Have you recently choked on your tea or soup?”, respectively, with possible answers dichotomized into yes and no, as utilized in a basic checklist for nursing care prevention in the Japanese long-term care insurance system [12]. Dental status was categorized as follows: having ≥20 teeth, having 10–19 teeth with dentures, having 10–19 teeth without dentures, having ≤9 teeth with dentures, and having ≤9 teeth without dentures.
Covariates
Factors associated with falls, including age [7,20,21], educational attainment [7,22], equivalized income [22,23], depression [7,21], self-rated health [7,24], instrumental activities of daily living (IADL) [13], body mass index (BMI) [24], present illness related to falls [20,21], social participation [22], walking in min/day [22], alcohol drinking status [25] and population density [22], were used as covariates. Age was categorized as follows: 65–69, 70–74, 75–79, 80–84 or ≥85 years. Educational attainment was categorized as follows: ≤9, 10–12, or ≥13 years. Equivalized income was calculated by dividing household income by the square root of the number of household members, and was categorized as follows: ≤1,999,999 JPY (1 USD = 100 JPY), 2,000,000–3,999,999 JPY, or ≥4,000,000 JPY. Depression was assessed using the Japanese short version of the Geriatric Depression Scale-15 [26], and was grouped into three categories: 0–4 (no), 5–9 (mild), or 10–15 (moderate to severe). Self-rated health was determined by asking, “How is your health at present?”, with answers categorized as follows: “excellent”, “good”, “fair”, or “poor”. IADL was assessed using the Tokyo Metropolitan Institute of Gerontology Index of Competence (TMIG-IC) questionnaire [27], and categorized as follows: independence (13 points) or dependence (≤12 points). BMI was categorized into three groups: <18.5, 18.5–24.9, or ≥25.0. Self-reported current medical treatment for stroke, osteoporosis, joint disease/neuralgia, injury/fracture, impaired vision and/or impaired hearing was used as a variable for present illness related to falls and categorized into two groups: yes or no. Social participation was determined by asking, “Do you belong to the following organization or group?” in relation to the following types of community organizations: neighborhood/senior association, citizen/firefighting club, religious group, political group/organization, industrial or trade association, volunteer group, citizen/consumer group, hobby group, and sports club/group. Answers were categorized into two groups: participation (yes) or nonparticipation (no). Walking in min/day was categorized as follows: ≥90 min, 60–89 min, 30–59 min, or <30 min. Alcohol drinking status was categorized as follows: current, former, or never drinker. Municipality population density was categorized as follows: metropolitan (density over 4,000 people per km2), urban (density between 1,500 and 4,000 people per km2), semi-urban (density between 1,000 and 1,499 people per km2), and rural (density below 1,000 people per km2).
Statistical analysis
Categorical variables that included missing values were recorded by reassigning missing values to separate “data missing” categories to maximize the number of participants included in the statistical analysis and thereby maximize statistical power. In the follow-up survey, incident falls was defined as a history of multiple falls. First, univariate associations between incident falls and oral health variables and covariates in males and females were examined. Then, two-level (first level: individuals; second level: municipality) logistic regression models with random intercepts and fixed slopes were used for males and females separately to calculate multilevel odds ratios (ORs) and 95% confidence intervals (CIs) for incident falls at follow-up. In the first model, univariate ORs and 95% CIs were calculated for each oral health variable. In the second model, multilevel ORs and 95% CIs were calculated for each oral health variable after adjusting for age. In the third model, multilevel ORs and 95% CIs were calculated for each oral health variable after adjusting for all covariates, i.e., age, educational attainment, equivalized income, depression, self-rated health, IADL, BMI, present illness related to falls, social participation, walking in min/day and alcohol drinking status, as individual-level variables, and population density as a municipality-level variable. In the fourth model, difficulty eating tough foods, dry mouth, and choking were simultaneously added after adjusting for all covariates. In the fifth model, all oral health variables were simultaneously added after adjusting for all covariates and checking the multicollinearity among the oral health variables. All statistical analyses were performed using MLwiN 2.36 (Centre for Multilevel Modelling, University of Bristol, Bristol, UK) and IBM SPSS Statistics (version 23.0; IBM Co., New York, NY, USA).
Results
The number (%) of males and females who reported having multiple falls in the follow-up survey were 475 (2.4%) and 430 (2.1%), respectively. Table 1 shows the rates of males and female fallers at follow-up according to oral health variables and covariates. In both sexes, participants with difficulty eating tough foods, dry mouth, choking, poor dental status, older age, low educational attainment, low equivalized income, depression, poor self-rated health, low IADL, low BMI, present illness related to falls, social nonparticipation, <30 min walking/day, status as a former drinker and living in rural areas were more likely to report the occurrence of incident falls.
Table 1. Univariate associations of oral health variable and covariates with incident falls in males and females.
| Males | Females | ||||||
|---|---|---|---|---|---|---|---|
| Total | Fallers | Total | Fallers | ||||
| n | n | % | n | n | % | ||
| Oral health variables | |||||||
| Difficulty eating tough foods | No | 14749 | 295 | 2.00 | 15786 | 270 | 1.71 |
| Yes | 4261 | 155 | 3.64 | 4179 | 135 | 3.23 | |
| Data missing | 985 | 25 | 2.54 | 893 | 25 | 2.80 | |
| Dry mouth | No | 15793 | 322 | 2.04 | 16480 | 296 | 1.80 |
| Yes | 3061 | 124 | 4.05 | 3195 | 105 | 3.29 | |
| Data missing | 1141 | 29 | 2.54 | 1183 | 29 | 2.45 | |
| Choking | No | 16668 | 360 | 2.16 | 17539 | 310 | 1.77 |
| Yes | 2302 | 93 | 4.04 | 2377 | 90 | 3.79 | |
| Data missing | 1025 | 22 | 2.15 | 942 | 30 | 3.18 | |
| Dental status | ≥20 teeth | 7965 | 130 | 1.63 | 7973 | 105 | 1.32 |
| 10–19 teeth with dentures | 3280 | 71 | 2.16 | 3101 | 56 | 1.81 | |
| 10–19 teeth without dentures | 1707 | 41 | 2.40 | 1891 | 48 | 2.54 | |
| ≤9 teeth with dentures | 4379 | 129 | 2.95 | 4601 | 134 | 2.91 | |
| ≤9 teeth without dentures | 1712 | 64 | 3.74 | 1659 | 52 | 3.13 | |
| Data missing | 952 | 40 | 4.20 | 1633 | 35 | 2.14 | |
| Covariates | |||||||
| Age (years) | 65–69 | 7381 | 100 | 1.35 | 7523 | 78 | 1.04 |
| 70–74 | 6224 | 122 | 1.96 | 6571 | 134 | 2.04 | |
| 75–79 | 4074 | 126 | 3.09 | 4278 | 121 | 2.83 | |
| 80–84 | 1822 | 85 | 4.67 | 1874 | 70 | 3.74 | |
| ≥85 | 494 | 42 | 8.50 | 612 | 27 | 4.41 | |
| Educational attainment (years) | ≤9 | 7694 | 237 | 3.08 | 9603 | 218 | 2.27 |
| 10–12 | 6857 | 137 | 2.00 | 7720 | 140 | 1.81 | |
| ≥13 | 4867 | 75 | 1.54 | 2798 | 41 | 1.47 | |
| Data missing | 577 | 26 | 4.51 | 737 | 31 | 4.21 | |
| Equivalized income (10,000 yen) | Low (≤199) | 7738 | 215 | 2.78 | 8227 | 168 | 2.04 |
| Middle (200–399) | 7937 | 138 | 1.74 | 6668 | 117 | 1.75 | |
| High (≥400) | 2219 | 45 | 2.03 | 1923 | 29 | 1.51 | |
| Data missing | 2101 | 77 | 3.66 | 4040 | 116 | 2.87 | |
| Depression | No | 13791 | 262 | 1.90 | 13397 | 212 | 1.58 |
| Mild | 2997 | 110 | 3.67 | 2945 | 84 | 2.85 | |
| Moderate to severe | 799 | 48 | 6.01 | 719 | 33 | 4.59 | |
| Data missing | 2408 | 55 | 2.28 | 3797 | 101 | 2.66 | |
| Self-rated health | Excellent | 3081 | 40 | 1.30 | 2887 | 32 | 1.11 |
| Good | 14137 | 296 | 2.09 | 15269 | 286 | 1.87 | |
| Fair | 2345 | 114 | 4.86 | 2228 | 92 | 4.13 | |
| Poor | 295 | 19 | 6.44 | 224 | 18 | 8.04 | |
| Data missing | 137 | 6 | 4.38 | 250 | 2 | 0.80 | |
| IADL | Independence (13) | 7012 | 134 | 1.91 | 10672 | 152 | 1.42 |
| Dependence (≤12) | 11209 | 289 | 2.58 | 8157 | 210 | 2.57 | |
| Data missing | 1774 | 52 | 2.93 | 2029 | 68 | 3.35 | |
| Body mass index | <18.5 | 826 | 28 | 3.39 | 1609 | 35 | 2.18 |
| 18.5–24.9 | 13835 | 319 | 2.31 | 14222 | 248 | 1.74 | |
| ≥25 | 4640 | 102 | 2.20 | 4026 | 110 | 2.73 | |
| Data missing | 694 | 26 | 3.75 | 1001 | 37 | 3.70 | |
| Present illness related to falls* | No | 10612 | 231 | 2.18 | 9167 | 155 | 1.69 |
| Yes | 3979 | 150 | 3.77 | 6322 | 204 | 3.23 | |
| Data missing | 5404 | 94 | 1.74 | 5369 | 71 | 1.32 | |
| Social participation | No | 3280 | 100 | 3.05 | 3191 | 94 | 2.95 |
| Yes | 14476 | 293 | 2.02 | 14703 | 258 | 1.75 | |
| Data missing | 2239 | 82 | 3.66 | 2964 | 78 | 2.63 | |
| Walking in min/day | ≥90 | 3760 | 73 | 1.94 | 3433 | 58 | 1.69 |
| 60–89 | 3634 | 74 | 2.04 | 3199 | 52 | 1.63 | |
| 30–59 | 6999 | 156 | 2.23 | 7415 | 149 | 2.01 | |
| <30 | 5319 | 164 | 3.08 | 5976 | 144 | 2.41 | |
| Data missing | 283 | 8 | 2.83 | 835 | 27 | 3.23 | |
| Alcohol drinking status | Never drinker | 6471 | 169 | 2.61 | 16205 | 341 | 2.10 |
| Former drinker | 985 | 27 | 2.74 | 179 | 9 | 5.03 | |
| Current drinker | 11582 | 255 | 2.20 | 3447 | 54 | 1.57 | |
| Data missing | 957 | 24 | 2.51 | 1027 | 26 | 2.53 | |
| Population density (person per square kilometers) |
Metropolitan (≥4,000) | 5340 | 109 | 2.04 | 5536 | 86 | 1.55 |
| Urban (1,500–3,999) | 5079 | 104 | 2.05 | 4913 | 79 | 1.61 | |
| Semiurban (1,000–1,499) | 4505 | 117 | 2.60 | 4673 | 97 | 2.08 | |
| Rural (≤999) | 5071 | 145 | 2.86 | 5736 | 168 | 2.93 | |
*Stroke, osteoporosis, joint disease/neuralgia, injury/fracture, impaired vision and/or impaired hearing.
Table 2 shows the ORs (95% CIs) for male fallers according to oral health variables in the five multilevel logistic regression models. In Models 1 and 2, all oral health variables were significantly associated with incident falls. In Model 3, the associations between falls and difficulty eating tough foods, dry mouth, and choking remained significant; however, no significant associations were found between dental status and incident falls. In Models 4 and 5, three kinds of difficulties in oral function were associated with incident falls, although the statistical significance was marginal for difficulty eating tough foods in Model 5 and choking in Models 4 and 5 (p<0.10). In Model 5, dry mouth had a significantly high OR (1.41; 95% CI: 1.12–1.77); however, no significant association was observed between dental status and incident falls.
Table 2. Odds ratios and their 95% confidence intervals of oral health variables in the adjusted multilevel logistic regression models in males.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||||||
| Low | High | Low | High | Low | High | Low | High | Low | High | ||||||||||||
| Difficulty eating tough foods (reference: No) |
Yes | 1.86 | 1.52 | 2.26 | <0.001 | 1.70 | 1.39 | 2.07 | <0.001 | 1.33 | 1.08 | 1.64 | 0.007 | 1.27 | 1.03 | 1.56 | 0.028 | 1.23 | 0.99 | 1.52 | 0.060 |
| Data missing | 1.30 | 0.85 | 1.97 | 0.222 | 1.18 | 0.78 | 1.79 | 0.441 | 1.02 | 0.53 | 1.98 | 0.945 | 2.12 | 0.86 | 5.21 | 0.103 | 1.98 | 0.80 | 4.89 | 0.139 | |
| Dry mouth (reference: No) |
Yes | 2.03 | 1.64 | 2.51 | <0.001 | 1.90 | 1.53 | 2.35 | <0.001 | 1.49 | 1.19 | 1.86 | <0.001 | 1.41 | 1.12 | 1.77 | 0.003 | 1.41 | 1.12 | 1.77 | 0.003 |
| Data missing | 1.27 | 0.86 | 1.87 | 0.233 | 1.15 | 0.78 | 1.69 | 0.491 | 0.89 | 0.51 | 1.55 | 0.684 | 1.05 | 0.52 | 2.10 | 0.898 | 1.04 | 0.52 | 2.09 | 0.909 | |
| Choking (reference: No) |
Yes | 1.91 | 1.51 | 2.41 | <0.001 | 1.67 | 1.32 | 2.11 | <0.001 | 1.37 | 1.07 | 1.74 | 0.012 | 1.24 | 0.97 | 1.59 | 0.092 | 1.24 | 0.97 | 1.59 | 0.089 |
| Data missing | 1.01 | 0.65 | 1.56 | 0.982 | 0.92 | 0.59 | 1.43 | 0.718 | 0.62 | 0.32 | 1.20 | 0.157 | 0.37 | 0.13 | 1.04 | 0.058 | 0.38 | 0.13 | 1.06 | 0.065 | |
| Dental status (reference: ≥20 teeth) |
10–19 teeth with dentures |
1.33 | 0.99 | 1.79 | 0.056 | 1.26 | 0.94 | 1.69 | 0.219 | 1.18 | 0.88 | 1.59 | 0.265 | 1.12 | 0.83 | 1.51 | 0.465 | ||||
| 10–19 teeth without dentures |
1.47 | 1.03 | 2.10 | 0.035 | 1.37 | 0.96 | 1.96 | 0.087 | 1.16 | 0.81 | 1.67 | 0.410 | 1.13 | 0.79 | 1.63 | 0.504 | |||||
| ≤9 teeth with dentures |
1.81 | 1.41 | 2.32 | <0.001 | 1.39 | 1.08 | 1.80 | 0.011 | 1.18 | 0.91 | 1.53 | 0.203 | 1.12 | 0.86 | 1.46 | 0.401 | |||||
| ≤9 teeth without dentures |
2.30 | 1.69 | 3.12 | <0.001 | 1.75 | 1.28 | 2.38 | <0.001 | 1.36 | 0.99 | 1.87 | 0.059 | 1.29 | 0.93 | 1.78 | 0.125 | |||||
| Data missing | 2.71 | 1.88 | 3.91 | <0.001 | 2.03 | 1.40 | 2.93 | <0.001 | 1.52 | 1.03 | 2.24 | 0.033 | 1.46 | 0.99 | 2.16 | 0.057 | |||||
Model 1: Univariate analysis
Model 2: Age-adjusted analysis
Model 3: Educational attainment, equivalized income, depression, self-rated health, IADL, body mass index, present illness related falls, social participation, walking in min/day, alcohol drinking status and population density were added to model 2. Oral health variables were not simultaneously included.
Model 4: Adjusted variables in model 3 and oral health variables were simultaneously included.
Model 5: All variables are included into the same model.
Table 3 shows the ORs (95% CIs) for female fallers according to oral health variables in the five multilevel logistic regression models. In Models 1–3, all oral health variables were significantly associated with incident falls. In Model 4, difficulty eating tough foods and choking were significantly associated with incident falls; however, no significant association was observed for dry mouth. In Model 5, choking had a significantly high OR (1.64; 95% CI: 1.27–2.11); however, no significant association was found between dry mouth and incident falls. The statistical significance for difficulty eating tough foods was marginal (p<0.10). Furthermore, compared with females having ≥20 teeth, those having 10–19 teeth without dentures, ≤9 teeth with dentures, and ≤9 without dentures had significantly increased risk for incident falls, at 1.63-fold (95% CI: 1.14–2.31), 1.36-fold (95% CI: 1.03–1.80), and 1.46-fold (95% CI: 1.02–2.08), respectively.
Table 3. Odds ratios and their 95% confidence intervals of oral health variables in the adjusted multilevel logistic regression models in females.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |||||||
| Low | High | Low | High | Low | High | Low | High | Low | High | ||||||||||||
| Difficulty eating tough foods (reference: No) |
Yes | 1.92 | 1.55 | 2.37 | <0.001 | 1.73 | 1.39 | 2.14 | <0.001 | 1.41 | 1.13 | 1.75 | 0.002 | 1.32 | 1.06 | 1.65 | 0.015 | 1.25 | 0.99 | 1.57 | 0.058 |
| Data missing | 1.66 | 1.09 | 2.52 | 0.018 | 1.55 | 1.02 | 2.36 | 0.042 | 1.23 | 0.70 | 2.18 | 0.467 | 1.13 | 0.52 | 2.43 | 0.762 | 1.14 | 0.52 | 2.46 | 0.748 | |
| Dry mouth (reference: No) |
Yes | 1.90 | 1.52 | 2.39 | <0.001 | 1.75 | 1.39 | 2.20 | <0.001 | 1.38 | 1.08 | 1.75 | 0.009 | 1.21 | 0.95 | 1.54 | 0.130 | 1.21 | 0.95 | 1.54 | 0.132 |
| Data missing | 1.37 | 0.93 | 2.02 | 0.115 | 1.26 | 0.85 | 1.87 | 0.246 | 0.93 | 0.57 | 1.51 | 0.756 | 0.60 | 0.30 | 1.17 | 0.135 | 0.61 | 0.31 | 1.20 | 0.149 | |
| Choking (reference: No) |
Yes | 2.23 | 1.75 | 2.83 | <0.001 | 2.06 | 1.61 | 2.62 | <0.001 | 1.73 | 1.35 | 2.21 | <0.001 | 1.63 | 1.26 | 2.09 | <0.001 | 1.64 | 1.27 | 2.11 | <0.001 |
| Data missing | 1.83 | 1.25 | 2.69 | 0.002 | 1.72 | 1.17 | 2.53 | 0.006 | 1.55 | 0.92 | 2.59 | 0.097 | 2.07 | 1.04 | 4.12 | 0.037 | 2.07 | 1.04 | 4.13 | 0.038 | |
| Dental status (reference: ≥20 teeth) |
10–19 teeth with dentures |
1.36 | 0.98 | 1.89 | 0.069 | 1.29 | 0.92 | 1.79 | 0.135 | 1.25 | 0.90 | 1.74 | 0.181 | 1.19 | 0.85 | 1.66 | 0.310 | ||||
| 10–19 teeth without dentures |
1.92 | 1.36 | 2.71 | <0.001 | 1.83 | 1.29 | 2.60 | 0.001 | 1.68 | 1.18 | 2.38 | 0.004 | 1.63 | 1.14 | 2.31 | 0.007 | |||||
| ≤9 teeth with dentures |
2.18 | 1.68 | 2.83 | <0.001 | 1.69 | 1.29 | 2.22 | <0.001 | 1.46 | 1.11 | 1.91 | 0.006 | 1.36 | 1.03 | 1.80 | 0.030 | |||||
| ≤9 teeth without dentures |
2.30 | 1.64 | 3.24 | <0.001 | 1.76 | 1.25 | 2.50 | 0.001 | 1.55 | 1.09 | 2.21 | 0.014 | 1.46 | 1.02 | 2.08 | 0.038 | |||||
| Data missing | 1.60 | 1.08 | 2.36 | 0.019 | 1.22 | 0.82 | 1.81 | 0.325 | 0.97 | 0.65 | 1.45 | 0.875 | 0.91 | 0.61 | 1.38 | 0.670 | |||||
Model 1: Univariate analysis
Model 2: Age-adjusted analysis
Model 3: Educational attainment, equivalized income, depression, self-rated health, IADL, body mass index, present illness related falls, social participation, walking in min/day, alcohol drinking status and population density were added to model 2. Oral health variables were not simultaneously included.
Model 4: Adjusted variables in model 3 and oral health variables were simultaneously included.
Model 5: All variables are included into the same model.
Discussion
The results of the present study suggest that older people reporting poor oral function, including difficulty eating tough foods, dry mouth, and choking, are more likely to experience falls. These results agree with those from a previous cross-sectional study showing associations between the three questions and falls [13], and further clarify the temporal relationship between poor oral function and incident falls. In the Japanese long-term care insurance system, three questions are used to screen subjects with poor oral function and encourage participation in care prevention services [12]. The results from the present study suggest that the integration of these questions into those regarding fall risk could improve the accuracy of the assessments. Further studies are needed to determine whether improvement of oral function may reduce the risk of falls.
Several possible explanations for the association between poor oral function and incident falls can be envisaged. First, there may be other underlying factors between poor oral health and incident falls, although some adjustments for possible confounders have already been made. For example, some medications are associated with dry mouth [28], and patients treated with such medications are more likely to experience falls [6]. The variable, self-reported present illnesses related to dry mouth, which includes cancer, heart disease, hypertension, diabetes, obesity, hyperlipidemia, respiratory illness, gastrointestinal illness, mental illness, urinary disease and sleep disorder [28], was added to Models 3–5 in consideration of the effects of medication on the association between dry mouth and falls; however, no significant changes were observed in the ORs for dry mouth (data not shown). Further studies using patients’ medication data are necessary to examine the possibility of residual confounders.
Neuromuscular disorders may also represent an underlying factor because they can cause symptoms such as swallowing disorders [29] and an increased risk of falls [6]. To address this issue, two variables of physical activity, ascertained by asking the participants “Do you go upstairs without holding on to the handrail or the wall?” and “Do you get up out of a chair without holding anything?”, with possible answers dichotomized into yes and no [22], were added to Models 3–5. No significant changes were observed in the ORs for difficulty eating tough foods or choking (data not shown); however, further studies using data regarding neuromuscular conditions are needed to address the possibility of residual confounders.
Second, a decline in oral function may be part of a self-perpetuating cycle of frailty [30], which could in turn increase the risk of falls. Several studies have reported associations between chewing ability and physical fitness, such as lower extremity dynamic strength and equilibrium [31], which is a primary cause of falls [32]. One review showed that swallowing or chewing problems and poor oral intake were associated with an increased likelihood of weight loss [33]. We were unable to consider all potential confounders regarding general frailty because the present study was observational. Although further studies are necessary to examine the causal associations between incident falls and dry mouth and choking, the findings suggest that these indicators could be used as predictors.
Another possibility is that poor oral function could increase the degree of risk factors for falls, such as depression. One recent longitudinal study reported that older people who experienced more difficulty chewing tough foods developed depressive symptoms [16], which is a risk factor for incident falls [7,21]. However, depression was adjusted as a covariate in the present study, so other pathways may be involved.
In another previous study, analyses were not conducted separately by sex because of the relatively small sample size [7]. Balance performance in females was worse than that in males among older people [34, 35], suggesting that the effects of dental status on incident falls may be significant in females, but not in males. The ORs for females having 10–19 teeth without dentures, but not for those having 10–19 teeth with dentures, were significantly high. These results agree with those of a previous study [7], even though in that study, 10–19 teeth and ≤9 teeth were combined in the same category.
The ORs for three oral function variables in Model 4 were lower than were those in Model 3, indicating an association between these variables. In addition, the ORs for difficulty eating tough foods and dental status in Model 5 were lower than were those in Model 3, indicating an association. From the results of present study, we could not conclude whether oral function and dental status were the cause of falls, or whether they were mediators between systemic conditions and falls. However, our results do show that poor oral function and dental status significantly increased the risk of falls, even after adjusting for variables in relation to systemic conditions. Therefore, we consider that in addition to the effect of systemic conditions, oral function and dental status, especially occlusion, exert a direct effect on incident falls. One possible explanation for the mechanism between falls and occlusion is the effect of jaw position on body posture [36]. Proprioceptive receptors of the masticatory muscular system and dentoalveolar ligaments provide sensory afferent input [37]; hence, poor dental occlusion may decrease that proprioception, thereby interfering with the stability of head posture and increasing the risk of falls. In fact, one longitudinal study showed that partial or complete loss of dental occlusion was associated with a decline in lower extremity dynamic strength and balance function [9], and a clinical study showed that denture use improves balance and control in older people [38].
The primary strength of this study was its large sample size, population-based sampling, and control for numerous confounding factors. In addition, a wide range of municipalities was surveyed to consider regional differences in incident falls [14].
This study did have several limitations. First, oral health status was based on self- rather than clinical assessments. However, the validity and reliability of self-assessed oral health status has been established and widely used in epidemiological studies [39]. Furthermore, the validity of our questionnaire for dental status has been confirmed [40]. Second, self-reported falls may not be completely factual. However, the associations between falls and demographic factors and other covariates were in the generally expected direction, suggesting that there may be sufficient value in these outcomes.
Conclusions
This longitudinal study using data from community-dwelling older people showed that poor oral function, including difficulty eating tough foods, dry mouth, and choking, was associated with incident falls. Moreover, having fewer teeth and not using dentures were independent predictors of falls in older females. Further studies are needed to determine whether improvement of oral health can reduce the risk of falls.
Acknowledgments
This study used data from the Japan Gerontological Evaluation Study (JAGES), which was supported by the Ministry of Education, Culture, Sports, Science and Technology-Japan (MEXT)-Supported Program for the Strategic Research Foundation at Private Universities (2009–2013), Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Numbers (22330172, 22390400, 23243070, 23590786, 23790710, 24390469, 24530698, 24683018, 25253052, 25870573, 25870881, 26285138, 26882010, 15H01972, 15H05059), Health Labour Sciences Research Grants (H22-Choju-Shitei-008, H24-Junkanki [Seishu]-Ippan-007, H24-Chikyukibo-Ippan-009, H24-Choju-Wakate-009, H25-Kenki-Wakate-015, H25-Choju-Ippan-003, H26-Irryo-Shitei-003 [Fukkou], H26-Choju-Ippan-006, H27-Ninchisyou-Ippan-001), Research and Development Grants for Longevity Science from the Japan Agency for Medical Research and Development (AMED), Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology (24–17, 24–23), and the Japan Foundation For Aging And Health (J09KF00804).
Data Availability
All data used are from the JAGES study and are not third-party data. All enquiries are to be addressed at the JAGES data management committee via e-mail: dataadmin.ml@jages.net. All JAGES datasets have ethical or legal restrictions for public deposition due to inclusion of sensitive information from the human participants. Following the regulation of local governments which cooperated on our survey, the JAGES data management committee has imposed the restrictions upon the data.
Funding Statement
This study was supported by the Ministry of Education, Culture, Sports, Science and Technology-Japan (MEXT)-Supported Program for the Strategic Research Foundation at Private Universities (2009-2013), Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Numbers (22330172, 22390400, 23243070, 23590786, 23790710, 24390469, 24530698, 24683018, 25253052, 25870573, 25870881, 26285138, 26882010, 15H01972, 15H05059), Health Labour Sciences Research Grants (H22-Choju-Shitei-008, H24-Junkanki [Seishu]-Ippan-007, H24-Chikyukibo-Ippan-009, H24-Choju-Wakate-009, H25-Kenki-Wakate-015, H25-Choju-Ippan-003, H26-Irryo-Shitei-003 [Fukkou], H26-Choju-Ippan-006, H27-Ninchisyou-Ippan-001), Research and Development Grants for Longevity Science from the Japan Agency for Medical Research and Development (AMED), Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology (24-17, 24-23), and the Japan Foundation For Aging And Health (J09KF00804). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing. 1981;10: 141–146. [DOI] [PubMed] [Google Scholar]
- 2.Blake AJ, Morgan K, Bendall MJ, Dallosso H, Ebrahim SB, Arie TH, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988; 17: 365–372. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43: 1214–1221. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337: 1279–1284. doi: 10.1056/NEJM199710303371806 [DOI] [PubMed] [Google Scholar]
- 5.Cabinet Office, Government of Japan. Annual Report on the Aging Society: 2015. In Japanese. Available: http://www8.cao.go.jp/kourei/whitepaper/w-2015/html/zenbun/index.html. Accessed 25 July 2017.
- 6.World Health Organization. WHO global report on falls prevention in older age. Available: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf. Accessed 25 July 2017.
- 7.Yamamoto T, Kondo K, Misawa J, Hirai H, Nakade M, Aida J, et al. Dental status and incident falls among older Japanese: a prospective cohort study. BMJ Open. 2012;31: 2 doi: 10.1136/bmjopen-2012-001262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song-Yu X, Rodis OM, Ogata S, Can-Hu J, Nishimura M, Matsumura S. Postural stability and occlusal status among Japanese elderly. Gerodontology. 2012;29: e988–997. doi: 10.1111/j.1741-2358.2011.00596.x [DOI] [PubMed] [Google Scholar]
- 9.Okuyama N, Yamaga T, Yoshihara A, Nohno K, Yoshitake Y, Kimura Y, et al. Influence of dental occlusion on physical fitness decline in a healthy Japanese elderly population. Arch Gerontol Geriatr. 2011;52: 172–176. doi: 10.1016/j.archger.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 10.Yamashita Y, Kogo H, Otao H, Hirao A, Mizota K. The relationship between the Fall Risk Index-21(FRI-21) and occlusal force in the frail elderly. Japanese Journal of Health Promotion and Physical Therapy. 2015;5(1): 9–14 (In Japanese) [Google Scholar]
- 11.Pedersen AM, Bardow A, Jensen SB, Nauntofte B. Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis. 2002;8: 117–129. [DOI] [PubMed] [Google Scholar]
- 12.Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15: 518–519. doi: 10.1111/ggi.12397 [DOI] [PubMed] [Google Scholar]
- 13.Masumoto T, Yamada Y, Yamada M, Nakaya T, Miyake M, Watanabe Y, et al. Fall risk factors and sex differences among community-dwelling elderly individuals in Japan. A Kameoka study. Japanese Society of Public Health. 2015;62: 390–401. (In Japanese) doi: 10.11236/jph.62.8_390 [DOI] [PubMed] [Google Scholar]
- 14.Hayashi T, Kondo K, Yamada M, Matsumoto D. Are there any areas where are few fallers? A study of regional differences and related factors: JAGES project. Journal of Health and Welfare Statistics. 2014;61(7): 1–7. (Author’s translation) (In Japanese) [Google Scholar]
- 15.Koyama S, Aida J, Saito M, Kondo N, Sato Y, Matsuyama Y, et al. Community social capital and tooth loss in Japanese older people: a longitudinal cohort study. BMJ Open. 2016;6: e010768 doi: 10.1136/bmjopen-2015-010768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto T, Aida J, Kondo K, Fuchida S, Tani Y, Saito M, et al. Oral Health and Incident Depressive Symptoms: JAGES Project Longitudinal Study in Older Japanese. J Am Geriatr Soc. 2017;65: 1079–1084. doi: 10.1111/jgs.14777 [DOI] [PubMed] [Google Scholar]
- 17.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261: 2663–2668. [PubMed] [Google Scholar]
- 18.Lord SR, Clark RD, Webster IW. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39: 1194–1200. [DOI] [PubMed] [Google Scholar]
- 19.Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46: 58–64. [DOI] [PubMed] [Google Scholar]
- 20.Ueno M, Kawai S, Mino T, Kamoshita H. Systematic review of fall-related factors among the house-dwelling elderly in Japan. Nihon Ronen Igakkai Zasshi. 2006;43(1): 92–101. (In Japanese) [DOI] [PubMed] [Google Scholar]
- 21.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319: 1701–1707. doi: 10.1056/NEJM198812293192604 [DOI] [PubMed] [Google Scholar]
- 22.Hayashi T, Kondo K, Suzuki K, Yamada M, Matsumoto D. Factors associated with falls in community-dwelling older people with focus on participation in sport organizations: the Japan Gerontological Evaluation Study Project. Biomed Res Int. 2014;2014: 537614 doi: 10.1155/2014/537614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsuda R. Life-style choices and falls In: Kondo K, editor. Health Inequalities in Japan: An Empirical Study of Older People. Melbourne, Australia: Trans Pacific Press; 2010. pp. 37–50. [Google Scholar]
- 24.Grundstrom AC, Guse CE, Layde PM. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch Gerontol Geriatr. 2012;54: 421–428. doi: 10.1016/j.archger.2011.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, et al. The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110: 108–116. doi: 10.1016/j.drugalcdep.2010.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol. 1991;4: 173–178. [DOI] [PubMed] [Google Scholar]
- 27.Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of Competence. Arch Gerontol Geriatr. 1991;13: 103–116. [DOI] [PubMed] [Google Scholar]
- 28.Villa A, Wolff A, Narayana N, Dawes C, Aframian DJ, Lynge Pedersen AM, et al. World Workshop on Oral Medicine VI: a systematic review of medication-induced salivary gland dysfunction. Oral Dis. 2016;22: 365–382. doi: 10.1111/odi.12402 [DOI] [PubMed] [Google Scholar]
- 29.Schindler JS1, Kelly JH. Swallowing disorders in the elderly. Laryngoscope. 2002;112: 589–602. doi: 10.1097/00005537-200204000-00001 [DOI] [PubMed] [Google Scholar]
- 30.Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women's Health and Aging Study II. J Gerontol A Biol Sci Med Sci. 2008;63: 984–990. [DOI] [PubMed] [Google Scholar]
- 31.Takata Y, Ansai T, Awano S, Hamasaki T, Yoshitake Y, Kimura Y, et al. Relationship of physical fitness to chewing in an 80-year-old population. Oral Dis. 2004;10: 44–49. [DOI] [PubMed] [Google Scholar]
- 32.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52: 1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x [DOI] [PubMed] [Google Scholar]
- 33.Tamura BK, Bell CL, Masaki KH, Amella EJ. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: a systematic review of the literature. J Am Med Dir Assoc. 2013;14: 649–655. doi: 10.1016/j.jamda.2013.02.022 [DOI] [PubMed] [Google Scholar]
- 34.Kim JW, Eom GM, Kim CS, Kim DH, Lee JH, Park BK, et al. Sex differences in the postural sway characteristics of young and elderly subjects during quiet natural standing. Geriatr Gerontol Int. 2010;10: 191–198. doi: 10.1111/j.1447-0594.2009.00582.x [DOI] [PubMed] [Google Scholar]
- 35.Kim JW, Kwon Y, Ho Y, Jeon HM, Bang MJ, Jun JH, et al. Age-gender differences in the postural sway during squat and stand-up movement. Biomed Mater Eng. 2014;24: 2707–2713. doi: 10.3233/BME-141088 [DOI] [PubMed] [Google Scholar]
- 36.Bracco P, Deregibus A, Piscetta R. Effects of different jaw relations on postural stability in human subjects. Neurosci Lett. 2004;356: 228–230. doi: 10.1016/j.neulet.2003.11.055 [DOI] [PubMed] [Google Scholar]
- 37.Gangloff P, Louis JP, Perrin PP. Dental occlusion modifies gaze and posture stabilization in human subjects. Neurosci Lett. 2000;293: 203–206. [DOI] [PubMed] [Google Scholar]
- 38.Okubo M, Fujinami Y, Minakuchi S: Effect of complete dentures on body balance during standing and walking in elderly people. J Prosthodont Res. 2010;54: 42–47. doi: 10.1016/j.jpor.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 39.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62: 122–128. [DOI] [PubMed] [Google Scholar]
- 40.Yamamoto T, Kondo K, Fuchida S, Aida J, Nakade M, Hirata Y. Validity of self-reported oral health variables: Aichi Gerontological Evaluation Study (AGES) project. Health Sci Health Care. 2012;12(1): 4–12. (In Japanese) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used are from the JAGES study and are not third-party data. All enquiries are to be addressed at the JAGES data management committee via e-mail: dataadmin.ml@jages.net. All JAGES datasets have ethical or legal restrictions for public deposition due to inclusion of sensitive information from the human participants. Following the regulation of local governments which cooperated on our survey, the JAGES data management committee has imposed the restrictions upon the data.


