Abstract
Interferon regulatory factor 8 (IRF8), also known as interferon consensus sequence-binding protein (ICSBP), is a transcription factor of the IRF family. IRF8 plays a key role in normal B cell differentiation, a cellular process that is intrinsically associated with Epstein-Barr virus (EBV) reactivation. However, whether IRF8 regulates EBV lytic replication remains unknown. In this study, we utilized a CRISPR/Cas9 genomic editing approach to deplete IRF8 and found that IRF8 depletion dramatically inhibits the reactivation of EBV upon lytic induction. We demonstrated that IRF8 depletion suppresses the expression of a group of genes involved in apoptosis and thus inhibits apoptosis induction upon lytic induction by B cell receptor (BCR) stimulation or chemical induction. The protein levels of caspase-1, caspase-3 and caspase-8 all dramatically decreased in IRF8-depleted cells, which led to reduced caspase activation and the stabilization of KAP1, PAX5 and DNMT3A upon BCR stimulation. Interestingly, caspase inhibition blocked the degradation of KAP1, PAX5 and DNMT3A, suppressed EBV lytic gene expression and viral DNA replication upon lytic induction, suggesting that the reduced caspase expression in IRF8-depleted cells contributes to the suppression of EBV lytic replication. We further demonstrated that IRF8 directly regulates CASP1 (caspase-1) gene expression through targeting its gene promoter and knockdown of caspase-1 abrogates EBV reactivation upon lytic induction, partially through the stabilization of KAP1. Together our study suggested that, by modulating the activation of caspases and the subsequent cleavage of KAP1 upon lytic induction, IRF8 plays a critical role in EBV lytic reactivation.
Author summary
Infection with Epstein-Barr virus (EBV) is closely associated with human cancers of both B cell and epithelial cell origin. The EBV life cycle is tightly regulated by both viral and cellular factors. Here, we demonstrate that interferon regulatory factor 8 (IRF8) is required for EBV lytic replication. Mechanistically, IRF8 directly regulates caspase-1 expression and hence caspase activation upon B cell receptor (BCR) stimulation and chemical induction, which leads to the cleavage and de-stabilization of several host factors suppressing lytic replication, including KAP1. Caspase-1 depletion blocks EBV reactivation while KAP1 depletion facilitates reactivation in caspase-1 depleted cells. These results together establish a IRF8/caspase-1/KAP1 axis important for EBV reactivation.
Introduction
Epstein-Barr virus (EBV), a ubiquitous human gammaherpesvirus, is associated with malignant diseases, including Burkitt’s lymphoma, Hodgkin’s lymphoma, nasopharyngeal carcinoma, and NK/T cell lymphoma [1]. The genome of EBV is approximately 170 kb in length and encodes more than 80 genes. EBV infects both B lymphocytes and some epithelial cells and the life cycle of EBV is divided into latent or lytic phases. In the lytic phase, EBV expresses all lytic genes and progeny virus particles are packaged and released from the cell [2]. The reactivation of EBV from latent to lytic phase can be triggered by expression of two viral immediate-early gene products, ZTA (also called BZLF1 or Z) and RTA (also known as BRLF1 or R). A series of cellular factors have been shown to regulate ZTA and RTA gene expression and to affect ZTA/RTA transcriptional activity [3,4,5,6,7,8,9,10,11,12,13,14,15,16]. B cell receptor (BCR) activation is a philologically relevant stimulus for triggering EBV reactivation from latency since this occurs not only in tumor cell lines but also in freshly isolated B cells from patients [17,18].
The interferon regulatory factor (IRF) family members (IRF1-9) are transcription factors for interferon (IFN) and IFN-inducible genes [19,20]. Members of the IRF family also play a vital role in regulation of immunity and oncogenesis [21]. Previous studies showed that several IRFs are implicated in the life cycles of herpesviruses, including EBV. For examples, IRF1, IRF2, IRF4, IRF5 and IRF7 are involved in EBV latency and virus-mediated cell transformation [22,23,24,25,26]. IRF4 synergizes with RTA encoded by murine γ-herpesvirsus-68 to facilitate viral M1 gene expression [27]. IRF3 and IRF7-mediated antiviral responses are counteracted by EBV encoded proteins [28,29,30].
IRF8, also known as IFN consensus sequence-binding protein (ICSBP), is a unique transcription factor of the IRF family because it is expressed predominately in hematopoietic cells [31]. Similar to other IRFs, IRF8 contains a DNA binding domain (DBD) and interacts with other proteins (such as PU.1, IRF1, IRF2 or IRF4) through the IRF association domain (IAD). In addition, IRF8 can be tyrosine phosphorylated [32,33,34,35], SUMOylated [36] and ubiquitinated [37,38]. The DBD, IAD and post-translational modifications of IRF8 all contribute to its transcription-regulatory activities [36,39,40,41]. Phosphorylation and dephosphorylation can alter the function of IRF8 in innate immune responses and leukemia pathogenesis [34,42]. SUMO conjugation-deconjugation switches IRF8’s function as a repressor or a activator [36]. IRF8 is ubiquitinated by an E3 ligase TRIM21, which alters IRF8’s ability in IL12p40 transcription [30,37]. Knockdown of IRF8 inhibits the growth of diffuse large B-cell lymphoma [43]. IRF8 is required for apoptotic induction in myeloid cells [44]. Recently, an important study established a role for IRF4 and IRF8 in EBV-mediated B-cell transformation [45]. EBV EBNA3C, which is expressed in cells of type III latency, interacts with and stabilizes IRF4. EBNA3C coordinates with IRF4 to downregulate IRF8, which is critical for apoptosis inhibition and thus the survival of EBV-transformed cells [45]. However, in EBV-positive B cells of type I latency, EBNA3C is not expressed and IRF4 protein level is very low while IRF8 is highly expressed [46]. Despite the high expression of IRF8 in B cells of type I EBV latency, the contribution of IRF8 to EBV lytic replication remains unknown.
Driven by these facts, we explored the role of IRF8 in the EBV lytic cycle. We demonstrated that IRF8 positively regulates EBV lytic replication through regulating caspases expression and hence caspase activation upon lytic induction and caspase activation facilitates the degradation of cellular factors that limit EBV lytic replication.
Results
IRF8 depletion suppresses EBV lytic replication
The previous research on IRF8 and EBV latency [45] and the high expression of IRF8 in EBV-positive B cells of type I latency prompted us to test whether and how IRF8 regulates EBV lytic replication. Here we first utilized an Akata (EBV+) cell line, a Burkitt’s lymphoma cell line of type I latency, as a model system to investigate the role of IRF8 in the EBV lytic cycle. Because Akata (EBV+) cells express surface immunoglobulin receptors of the G (κ) class (IgG) and anti-IgG cross-linking mediated BCR activation can serve as a physiologically relevant stimulus for EBV lytic reactivation [18], these cells are well-suited for investigating the contribution of cellular factors in EBV lytic replication [13,47].
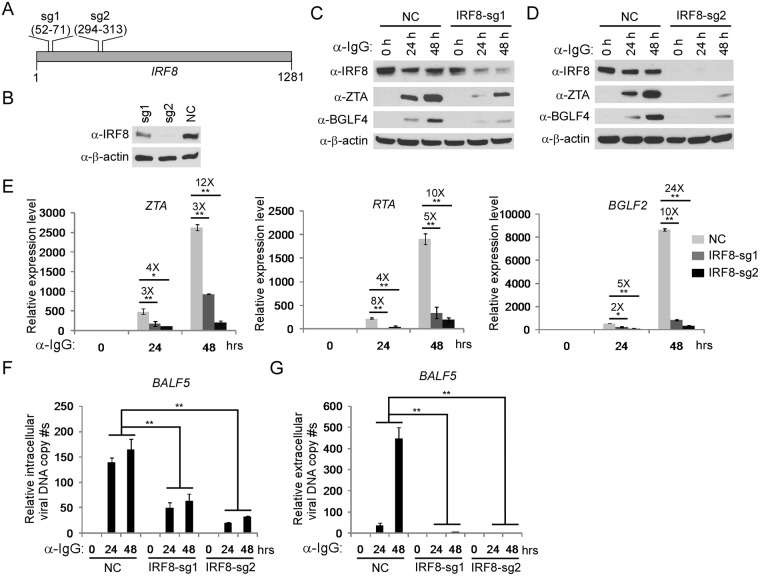
To demonstrate whether IRF8 regulates EBV lytic replication, we utilized CRISPR/Cas9 technology to knockdown endogenous IRF8 in Akata (EBV+) B cells. We designed two sgRNAs and used a lenti-viral system to establish two IRF8-depleted pool cell lines (Fig 1A). To ensure the reproducibility of our results, at least three independent lentiviral infections were performed. The infection efficiency was approximately 20% and the experiments were performed after one to two weeks selection with puromycin when all living cells were puromycin-resistant. Compared with non-targeting control (NC), the sgRNA sg1 partially knocked down the protein expression of IRF8, while sg2 efficiently depleted IRF8 (Fig 1B). To further confirm the correct targeting of IRF8 by CRISPR/Cas9, we sequenced the genomic DNA spanning the CRISPR/Cas9 targeting region of the IRF8-sg1 and IRF8-sg2 cell lines and we found that 10 out of 22 clones for sg1 and 9 out of 14 clones for sg2 contain frame shifts (S1 Fig). To evaluate the effects of IRF8 depletion on EBV lytic replication, we triggered EBV lytic replication by anti-IgG mediated BCR cross-linking. We found that the accumulation of the EBV lytic proteins ZTA and BGLF4 was suppressed in the two IRF8-depleted cell lines upon lytic induction and that the higher IRF8 knockdown efficiency correlated with lower ZTA and BGLF4 expression (Fig 1C and 1D).
Fig 1. IRF8 depletion inhibits the reactivation of EBV in Akata (EBV+) cells.
A. The locations of two sgRNAs (sg1 and sg2) used for IRF8 depletion. B. Western blot was performed to check the knockdown efficiency of IRF8 by sg1 and sg2 compared with the non-targeting control sgRNA (NC). C-G.IRF8-depleted (sg1 and sg2) and control (NC) Akata (EBV+) cells were either untreated (0 hr) or treated with anti-IgG for 24 and 48 hrs to induce lytic replication. The cell pellets and supernatant was harvested 24 and 48 hrs after anti-IgG stimulation. Protein extracts were analyzed by western blot using antibodies against IRF8 and EBV immediate-early (ZTA) and early (BGLF4) proteins (C and D). RT-qPCR showing the suppression of EBV immediate-early (ZTA and RTA) and late (BGLF2) genes expression upon IRF8 depletion (sg1 and sg2) (E). qPCR showing the reduction of intracellular viral DNA (F) and extracellular virion-associated DNA (G) copy numbers upon IRF8 depletion. The EBV genome copy number was measured by qPCR using primers specific to EBV BALF5. The intracellular EBV copy number was normalized by qPCR using specific primers to β-actin. Data are presented as means ± standard deviations (n = 3). * p<0.05 and ** p<0.01.
We then examined the level of lytic RNA transcripts in these cell lines. As expected, knockdown of IRF8 dramatically suppressed the expression of immediate early (ZTA and RTA) and late (BGLF2) genes (Fig 1E). To test whether IRF8 plays a role in EBV replication, we measured both intracellular and extracellular EBV genome copies following lytic induction. We found that both intracellular (Fig 1F) and extracellular (Fig 1G) viral DNA copies were significantly reduced upon IRF8 depletion. These results suggested that IRF8 acts as a key positive regulator during EBV lytic reactivation.
To further demonstrate that the observed phenotype was not due to off-target effects, we reconstituted IRF8 back into the IRF8-depleted (sg2) cells. We found that IRF8 restoration facilitated EBV ZTA and RTA protein expression compared with IRF8-depleted cells upon IgG cross-linking (S2A Fig, lanes 2–3 vs 5–6). Moreover, EBV DNA replication was also dramatically enhanced upon IRF8 reconstitution (S2B Fig, lanes 2–3 vs 5–6). Together these results suggest that IRF8 promotes EBV replication upon lytic induction.
IRF8-dependent caspase activation is required for EBV reactivation
As a transcription factor, IRF8 may also regulate EBV replication through altering cellular processes. To provide insight into IRF8-regulated cellular events, we performed RNA-Seq analysis for the control and IRF8-depleted cells generated from three different lentiviral transductions. Totally we identified 253 differentially expressed genes (S1 Table). Among these genes, 196 genes were down-regulated and 57 genes were up-regulated upon IRF8 depletion (Fig 2A). Gene Ontology (GO) analysis plus manual curation of these differentially regulated genes revealed that 19 genes involved in “positive regulation of apoptosis” were significantly enriched. Interestingly, all of these genes involved in apoptosis were down-regulated in IRF8-depleted cells (Fig 2A, red dots and Fig 2B). To validate our RNA-seq results, we selected 8 genes and analyzed their expression by RT-qPCR for both IRF8-sg1 and IRF8-sg2 cells. The down-regulation was confirmed for all those genes tested, including caspase-1 (CASP1) (Figs 2B and S3A). Consistent with the reduced mRNA expression, caspase-1 protein level was reduced in IRF8-depleted cells (Figs 2C and S3B, lane 1 vs 4). The down-regulation of apoptosis related genes suggested that IRF8 depletion may suppress apoptosis induction during EBV lytic replication upon BCR activation. To test this possibility, we monitored the cleavage of PARP and global caspase substrates containing a cleavage motif [DE(T/S/A)D]. We found that IRF8 depletion suppressed protein cleavage upon BCR activation (Figs 2C and S3B, lanes 2–3 vs 5–6).
Fig 2. IRF8 depletion suppresses the expression of genes involved in apoptosis.
A. Schematic representation of RNA-seq analyses of Akata (EBV+) cells carrying control (NC) or IRF8-sg2 sgRNAs, RNAs were extracted from cells derived from three distinct lentiviral transductions. Using 2-fold change as a cutoff, 196 and 57 genes were down- or up-regulated upon IRF8 depletion, respectively. Gene Ontology analysis showing that 19 genes involved in “positive regulation of apoptosis” (red dots) were down-regulated by IRF8 depletion. B. Fold changes of the 19 apoptosis-related genes and the validation of 8 of them by RT-qPCR analysis of RNAs from cells derived from three distinct lentiviral transductions. C. IRF8 depletion (sg2) suppresses caspase-1 expression and the generation of cleaved caspase substrates upon lytic induction by anti-IgG cross-linking. Western blot analysis of protein extracts from Fig 1D using antibodies against caspase-1, PARP, and cleaved caspase substrates (Peptides containing [DE(T/S/A)D] motif) as indicated.
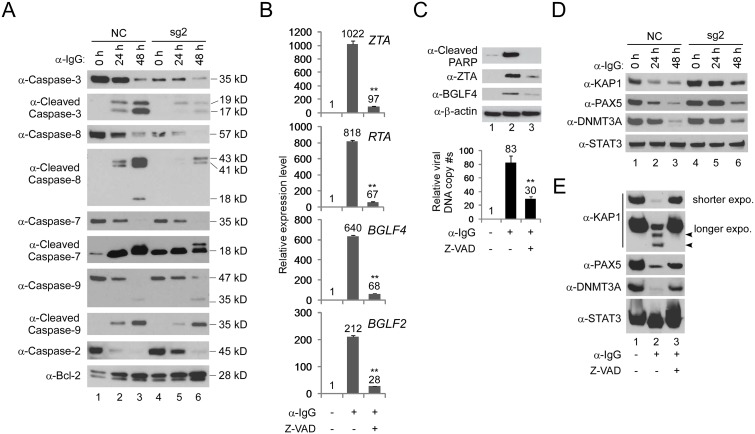
IRF8 has been shown to positively regulate the apoptosis of myeloid cells and nonhematopoietic tumor cells [44,48,49,50]. The dramatic down-regulation of caspase-mediated protein cleavage upon IRF8 depletion suggested that IRF8 may regulate the activation of caspases. To test this possibility, we monitored the level of individual caspases and their cleaved products. Strikingly, we found that the IRF8 depletion markedly reduced the levels of caspase-3 and caspase-8 and consequently the generation of active cleaved products was also suppressed upon BCR activation. In contrast, the protein levels of caspase-2, caspase-7 and caspase-9 and their cleavage were less affected by IRF8 depletion (Figs 3A and S3C). In addition, the level of Bcl-2, an anti-apoptosis protein, increased in IRF8-depleted cells (Figs 3A and S3C, Bcl-2 blot, lanes 1–3 vs 4–6), which further contributed to IRF8-dependent inhibition of apoptosis. Except for caspase-1, the gene expression levels of other caspases, including caspase-3 and caspase-8, were not regulated by IRF8 depletion according to our RNA-seq analysis (S4 Fig and S1 Table), suggesting that IRF8 may control caspase-3 and caspase-8 protein levels through modulation of translation or protein stability rather than transcription.
Fig 3. IRF8 depletion suppresses caspase activation and caspase activation is required for EBV lytic replication.
A. IRF8 depletion suppresses caspase activation. Western blot analysis of protein extracts from Fig 1D using antibodies against caspase-3, cleaved caspase-3, caspase-8, cleaved caspase-8, caspase-7, cleaved caspase-7, caspase-9, cleaved caspass-9, caspase-2 and Bcl-2 as indicated. B. Caspase inhibition suppresses EBV lytic gene expression. Akata (EBV+) cells were untreated or pre-treated with pan-caspase inhibitor (Z-VAD-FMK) for 1 hr and then anti-IgG was added for 48 hrs. RNA was extracted and EBV lytic gene expression was analyzed by RT-qPCR. Data are presented as means ± standard deviations of triplicate assays. ** p<0.01 (compared with the second bar). C. Caspase inhibition suppresses EBV DNA replication. Protein extracts from cells treated as Panel B were analyzed by western blot using antibodies against cleaved-PARP, EBV ZTA and BGLF4 as indicated. β-actin was used as loading controls. Genomic DNA was extracted and relative EBV DNA copy numbers was measured by qPCR using primers specific to EBV BALF5. The EBV copy number was normalized by qPCR using specific primers to β-actin. Data are presented as means ± standard deviations of triplicate assays. ** p<0.01 (compared with the second bar). D. IRF8 depletion suppresses the degradation of KAP1, PAX5 and DNMT3A upon lytic induction. Western blot analysis of protein extracts from Fig 1D using antibodies against KAP1, PAX5, DNMT3A and STAT3 as indicated. E. Caspase inhibition restores the expression of KAP1, PAX5 and DNMT3A. Protein extracts from Panel C were analyzed by western blot using antibodies against KAP1, PAX5, DNMT3A and STAT3 as indicated. The longer exposure of KAP1 blot revealed two cleaved KAP1 products upon lytic induction (lane 2, arrow heads).
Because caspase activation upon apoptotic induction can facilitate EBV lytic reactivation in other EBV-positive cell lines [51,52], we reasoned that IRF8 facilitates EBV reactivation in the Akata (EBV+) cells through caspase activation. To test this hypothesis, we pretreated the Akata (EBV+) cells with a pan-caspase inhibitor Z-VAD-FMK and then induced EBV lytic reactivation by anti-IgG cross-linking of the BCR. Caspase inhibition strongly suppressed the expression immediate-early (ZTA and RTA), early (BGLF4) and late (BGLF2) gene expression (Fig 3B). Consistently, the EBV ZTA and BGLF4 protein expression and viral DNA replication were also blocked by caspase inhibition (Fig 3C).
The switch from EBV latency to lytic reactivation is negatively regulated by a number of cellular factors [53]. Because caspase activation can lead to the cleavage of many cellular proteins [54,55,56], we hypothesized that those factors normally suppressing EBV lytic replication are destabilized by caspase activation upon BCR stimulation. To test this hypothesis, we monitored the levels of several proteins, including KAP1 [12,57,58,59], PAX5 [8,60,61,62], DNMT3A [63] and STAT3[64,65,66,67,68], whose functions have been shown to maintain herpesviruses latency and suppress lytic replication/reactivation. We found that the protein levels of KAP1, PAX5 and DNMT3A, but not that of STAT3, were dramatically reduced upon lytic induction (Figs 3D and S3C, lanes 1–3) while IRF8 depletion suppressed the down-regulation of KAP1, PAX5 and DNMT3A (Figs 3D and S3C, lanes 4–6). To further test whether caspase activation plays a role in the de-stabilization of KAP1, PAX5 and DNMT3A, we monitored their protein levels in Akata (EBV+) cells when caspases are inhibited and lytic replication is triggered by BCR stimulation. Interestingly, pretreatment of the cells with a pan-caspase inhibitor Z-VAD-FMK restored their expression (Fig 3E). For KAP1, in addition to the reduced protein level, we also noticed the generation of two potential cleaved fragments upon BCR activation, which is also blocked by caspase inhibition (Fig 3E, KAP1, longer exposure). Taken together, these results suggested caspase activation-mediated de-stabilization of cellular restriction factors contributes to EBV lytic replication.
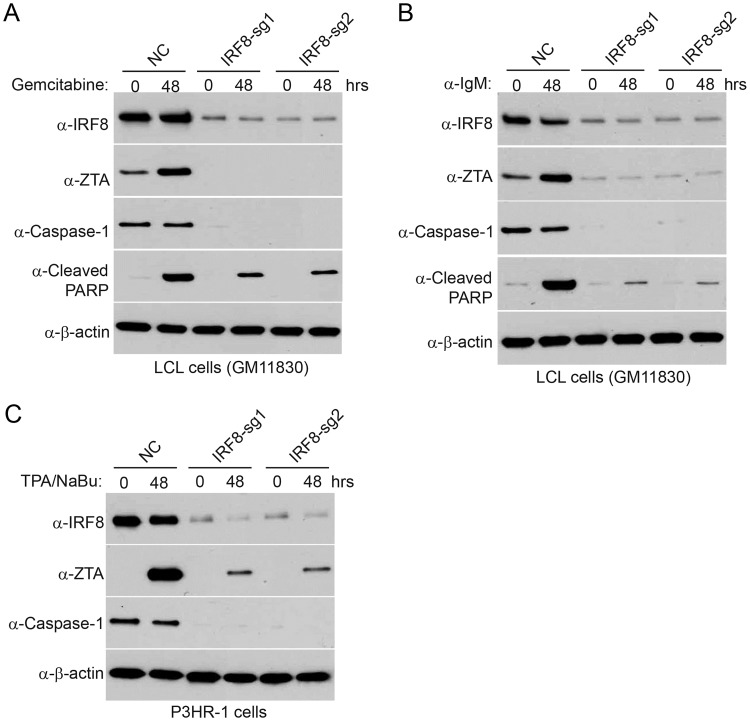
To demonstrate the effect of IRF8 in additional EBV-positive cell lines, we depleted IRF8 in two additional cell lines, P3HR-1 and an EBV transformed lymphoblastoid cell line (LCL). We observed universal lower reactivation for EBV in IRF8-depleted cells treated with either gemcitabine, anti-IgM (for LCL cells) or TPA/sodium butyrate (for P3HR-1 cells) (Fig 4), reinforcing that IRF8 plays a key role in EBV reactivation.
Fig 4. IRF8 depletion suppresses EBV reactivation in LCL and P3HR-1 cells upon lytic induction.
A and B. Control (NC) and IRF8-depleted (sg1 and sg2) LCL cells were either untreated (0 hr) or treated with 1 μg/mL gemcitabine (A) or 20 μg/mL α-IgM (B) for 48 hrs to induce lytic replication. Western blot analyses showing IRF8, ZTA, caspase-1 and cleaved-PARP level as indicated. C. Control (NC) and IRF8-depleted (sg1 and sg2) P3HR-1 cells were either untreated (0 hr) or treated with TPA (20 ng/ml)/sodium butyrate (NaBu, 3 mM) for 48 hrs to induce lytic replication. Western blot analyses showing IRF8, ZTA and caspase-1 level as indicated.
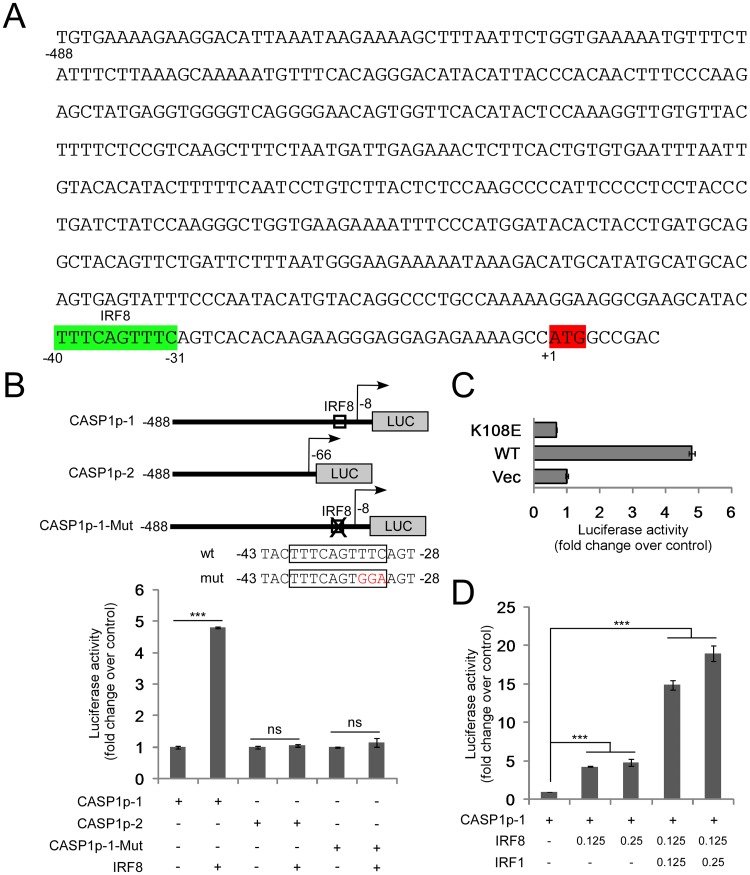
IRF8 regulates CASP1 (caspase-1) promoter activity
Based on our RNA-seq results, only CASP1 (caspase-1) gene was regulated by IRF8 at the RNA level (S4 Fig). Previous studies using ChIP-seq showed that IRF8 could bind to the promoter regions of both human and mouse CASP1 at a conserved consensus site, -40 to -31 bp upstream of the start codon of human CASP1 (Fig 5A) [69,70]. However, it is not clear whether IRF8 directly regulates CASP1 expression. We hypothesized that IRF8, as a transcription activator, directly regulates CASP1 gene expression through binding to its promoter. To test our hypothesis, we constructed luciferase reporter plasmids, which contain the CASP1 promoter with or without the putative IRF8 binding site (Fig 5B). The luciferase reporter assay showed that IRF8 activated the wild-type CASP1 promoter but not the truncated version without the IRF8 binding site (Fig 5B). To confirm our results, we mutated the conserved IRF8 binding site and found that IRF8 failed to activate the mutated reporter (Fig 5B). To further validate our results, we constructed a DNA-binding deficient IRF8 mutant (K108E) [71] and tested whether it can block the activation of CASP1 promoter. Compared with wild-type IRF8, the DNA-binding deficient mutant (K108E) lost the ability to regulate the CASP1 promoter (Fig 5C). In conclusion, our results demonstrated that IRF8 enhances CASP1 gene expression through regulation of its promoter. A previous study showed that IRF1 can also regulate CASP1 gene promoter [72]. Therefore, we tested whether IRF1 could cooperate with IRF8 to further enhance the CASP1 promoter activity. The luciferase reporter assay demonstrated that IRF1 synergized with IRF8 to further enhance CASP1 promoter activity (Fig 5D).
Fig 5. IRF8 regulates CASP1 promoter activities.
A. Schematic representation of the promoter of human CASP1. IRF8 consensus binding site is highlighted in green. The ATG of CASP1 is highlighted in red. B. The pGL2-CASP1p constructs (with or without IRF8 consensus site) and the IRF8 consensus site mutated construct were co-transfected into 293T cells with either vector control or IRF8 expression vectors. Luciferase assays were performed 36 hrs post-transfection. The value of cells transfected with empty vectors was set as 1. The results were presented as mean ± standard deviation of triplicate assays. C. The pGL2-CASP1p1 construct was co-transfected into 293T cells with either vector control, wild-type IRF8 (WT) or IRF8 DNA binding mutant (K108E) expression vectors and luciferase assays were performed 36 hrs post-transfection. The value of cells transfected with empty vectors was set as 1. The results were presented as mean ± standard deviation of triplicate assays. D. The pGL2-CASP1p1 construct was co-transfected into 293T cells with either vector control or IRF8 and IRF1 expression vectors and luciferase assays were performed 36 hrs post-transfection. The value of cells transfected with empty vectors was set as 1. The results were presented as mean ± standard deviation of triplicate assays. *** p<0.001.
To further prove whether IRF8/IRF1 bind to CASP1 promoter in B cells, we performed ChIP experiments using chromatin prepared from EBV-postive Akata, LCL and P3HR-1 cells. Our results showed that IRF8/IRF1 indeed bind to the promoter region of CASP1 for all these cells (S5A Fig), suggesting that they directly regulate CASP1 expression in vivo. To demonstrate physiological relevance of IRF8/IRF1 activation of CASP1 promoter observed in 293T cells, we performed luciferase assay using Akata cells. Similarly, we found that IRF8 and IRF1 triggered a strong activation of CASP1 promoter while the IRF8 DNA binding deficient mutant (K108E) failed to activate the promoter (S5B Fig).
Our RNA-seq analysis showed that both IRF1 and IRF8 are expressed in the Akata (EBV+) cells, with IRF8 level approximately 6-fold higher than that of IRF1 (S6 Fig). Based on the luciferase assay, IRF8, together with its closely related family member IRF1, plays an effective role on regulating CASP1 expression.
Caspase-1 depletion abrogates EBV lytic replication
The control of caspase-1 expression by IRF8 promoted us to test whether caspase-1 contributes to EBV reactivation upon lytic induction. To answer this question, we utilized a similar CRISPR/Cas9 approach to deplete endogenous CASP1 in Akata (EBV+) B cells. To offset the potential off-target effect, we designed two sgRNAs to establish CASP1-depleted cell lines by three distinct lentiviral infections (Fig 6A). To further confirm the correct targeting of CASP1 by CRISPR/Cas9, we also sequenced the genomic DNA spanning the CRISPR/Cas9 targeting region of the CASP1-sg1 and CASP1-sg2 cell lines. The sequencing results showed that frame shifts were introduced in 8 out of 13 clones for CASP1-sg1 and 12 out of 14 clones for CASP1-sg2 (S7 Fig). To evaluate the effects of caspase-1 depletion on EBV lytic reactivation, we triggered EBV reactivation by anti-IgG mediated BCR cross-linking. We found that the accumulation of the EBV lytic proteins ZTA and RTA was dramatically suppressed in the two CASP1-depleted cell lines upon BCR activation (Fig 6B). We also examined the level of lytic RNA transcripts in these cell lines. As expected, knockdown of CASP1 dramatically suppressed the expression of immediate early (ZTA and RTA) and late (BGLF2) genes (Fig 6C). To test whether caspase-1 plays a role in EBV replication, we measured intracellular EBV genome copies following lytic induction. Compared with control, the intracellular viral DNA copies were significantly reduced upon caspase-1 depletion (Fig 6D), suggesting that caspase-1 is required for EBV reactivation.
Fig 6. CASP1 depletion inhibits the reactivation of EBV in Akata (EBV+) cells.
A. The locations of two sgRNAs (sg1 and sg2) used for CASP1 depletion. B-D. CASP1-depleted (sg1 and sg2) and control (NC) Akata (EBV+) cells were either untreated (0 hr) or treated with anti-IgG for 24 and 48 hrs to induce lytic replication. The cell pellets were harvested 24 and 48 hrs after anti-IgG stimulation. Protein extracts were analyzed by western blot using antibodies against CASP1 and EBV immediate-early (ZTA and RTA) proteins and β-actin (B). RT-qPCR showing the suppression of EBV immediate-early (ZTA and RTA) and late (BGLF2) genes expression upon CASP1 depletion (sg1 and sg2) (C). qPCR showing the reduction of intracellular viral DNA copy numbers upon CASP1 depletion (D). The EBV genome copy number was measured by qPCR using primers specific to EBV BALF5. The intracellular EBV copy number was normalized by qPCR using specific primers to β-actin. Data are presented as means ± standard deviations (n = 3). ** p<0.01.
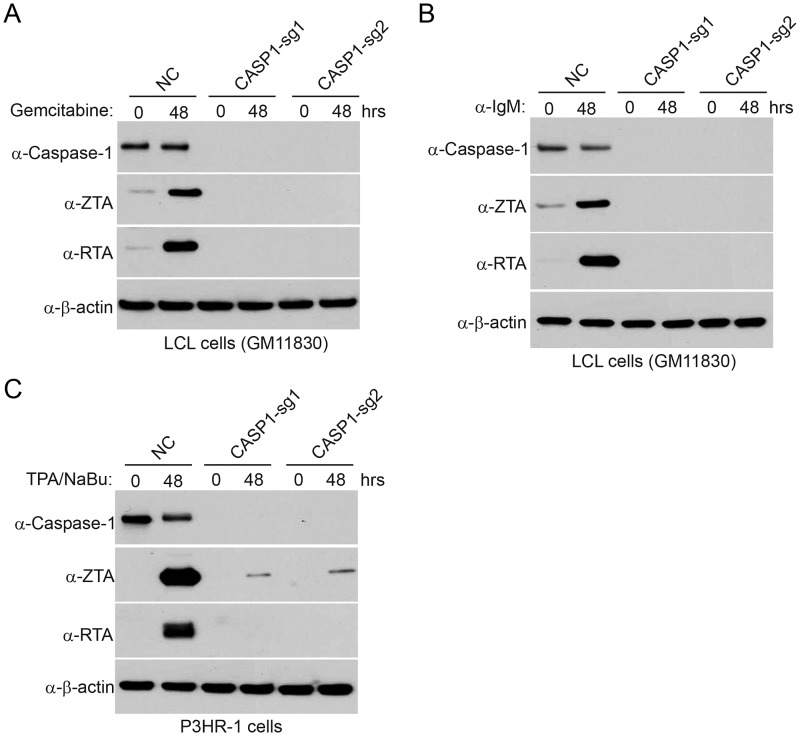
To demonstrate the effect of caspase-1 in broader settings, we also depleted CASP1 in P3HR-1 and EBV transformed LCL cells. We found that CASP1-depletion suppresses EBV reactivation treated with either gemcitabine, anti-IgM (for LCL) or TPA/sodium butyrate (for P3HR-1) (Fig 7), suggesting that IRF8/caspase-1 axis contributes to EBV reactivation upon lytic induction.
Fig 7. CASP1 depletion suppresses EBV reactivation in LCL and P3HR-1 cells upon lytic induction.
A and B. Control (NC) and CASP1-depleted (sg1 and sg2) LCL cells were either untreated (0 hr) or treated with 1 μg/mL gemcitabine (A) or 20 μg/mL α-IgM (B) for 48 hrs to induce lytic replication. Western blot analyses showing caspase-1, ZTA and RTA level as indicated. C. Control (NC) and CASP1-depleted (sg1 and sg2) P3HR-1 cells were either untreated (0 hr) or treated with TPA (20 ng/ml)/sodium butyrate (NaBu, 3 mM) for 48 hrs to induce lytic replication. Western blot analyses showing caspase-1, ZTA and RTA level as indicated.
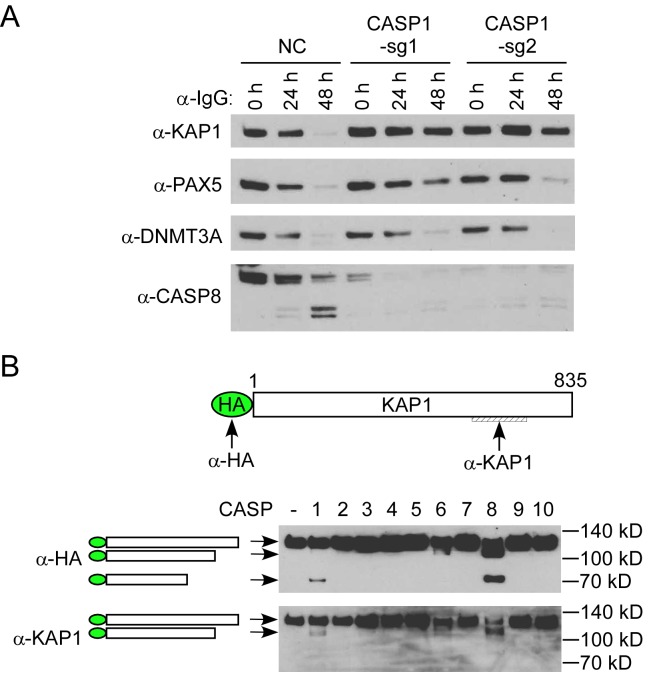
Caspase-1 promotes EBV reactivation partially through KAP1 cleavage
IRF8 can affect the degradation of KAP1, PAX5 and DNMT3A through caspase activation (Figs 3D and S3C). To test whether caspase-1 could affect their degradation, we monitored the protein stability when caspase-1 was depleted and lytic reactivation was induced by BCR activation. Interestingly, we found that the degradation of KAP1, but not PAX5 and DNMT3A, was blocked in caspase-1-depleted cells (Fig 8A). Based on these results, we reasoned that KAP1 might be cleaved by caspase-1. To prove this, we performed an in vitro cleavage assay using individual recombinant caspases and KAP1. To facilitate the detection of cleaved KAP1 fragments, we utilized an N-terminally HA-tagged KAP1 construct and immunoprecipitated the KAP1 protein from transfected 293T cells using HA magnetic beads. HA-KAP1 was eluted for the in vitro cleavage assay. Anti-HA and anti-KAP1 antibodies recognize N- and C-terminal of KAP1 respectively (Fig 8B), which facilitates the detection of cleaved fragments. Interestingly, we found that caspase-1, as well as caspase-8 can cleave KAP1 in vitro (Fig 8B). We also checked the expression of caspase-8 (CASP8) and found that the caspase-8 protein level (Fig 8A) but not its mRNA level (S8 Fig) was also reduced in caspase-1-depleted cells. These results together suggested that KAP1 cleavage is regulated by caspase-1 and -8 in Akata (EBV+) cells upon lytic induction. Because KAP1 depletion has been shown to facilitate EBV, Kaposi’s sarcoma-associated herpesvirus (KSHV) and human cytomegalovirus reactivation [12,57,58,59], we reasoned that the cleavage of KAP1 by caspase-1 and -8 should promote viral reactivation.
Fig 8. Caspase-1 promotes EBV reactivation partially through KAP1 cleavage.
A. Caspase-1 depletion suppresses KAP1 degradation. Protein extracts form Fig 5B were analyzed by western blot using antibodies against KAP1, PAX5, DNMT3A and Caspase-8 (CASP8). B. Caspase-1 and -8 cleave KAP1 in vitro. HA-KAP1 and the antibody recognition sites are labeled as indicated. HA-tagged KAP1 was immuoprecipitated from transfected 293T cells using HA magnetic beads. The beads-bound HA-KAP1 was incubated with individual recombinant caspase for 2 hrs at 37°C. WB was performed using either anti-HA or anti-KAP1 antibodies. The relative positions of cleaved fragments were labeled as indicated.
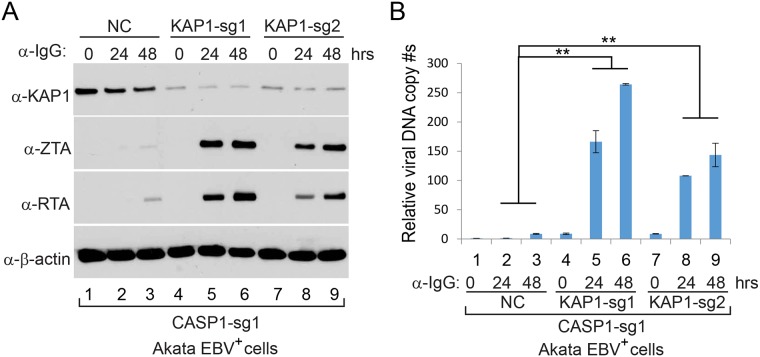
To prove our prediction, we further depleted KAP1 in CASP1-depleted (sg1) Akata cells by CRISPR/Cas9 genomic editing approach. As expected, KAP1-depletion in CASP1-depleted cells restored EBV reactivation upon BCR activation (Fig 9). Taken together, our results suggested that KAP1 is one of the important downstream targets of caspase-1 critical for EBV reactivation.
Fig 9. KAP1 depletion facilitates EBV reactivation upon lytic induction.
A. Control (NC) and KAP1-depleted (sg1 and sg2) Akata (EBV+)-CASP1-sg1 cells were untreated (0 hr) or treated with α-IgG (1:200) for 24 and 48 hrs to induce lytic replication. Western blot analyses showing KAP1, ZTA and RTA level as indicated. β-actin blot was included as loading controls. B. Intracellular viral DNA from cells treated as in (A) was measured by qPCR using primers to EBV BALF5. The value of NC control at 0 hr (lane 1) was set as 1. Data are presented as means ± standard deviations of triplicate assays. ** p<0.01.
Discussion
In this study, we discovered that the cellular factor IRF8 facilitates EBV lytic replication by promoting caspase expression and their activation upon lytic inducition. The IRF family proteins have been shown to play an important role in immunity, cell growth, differentiation and oncogenesis [19]. In contrast to the positive role of IRF8 in EBV lytic replication observed in our study, most of the IRFs contribute to anti-viral immunity and block the infection or lytic reactivation of herpesviruses. For example, it was reported that IRF1 restricts gammaherpesvirus replication through IFN-mediated suppression of viral replication [73,74,75,76]. IRF2 also suppresses gammaherpesvirus replication and reactivation by inhibiting the M2 gene promoter [77]. Herpesviruses have evolved strategies to block IRF3 mediated anti-viral signaling [30,78]. IRF5 or IRF7-mediaed suppression of KSHV replication is counteracted by virally encoded proteins [79,80,81]. While IRF4 has been implicated in suppressing KSHV replication [82,83,84], it has been shown that IRF4 promotes gammaherpesvirus-68 replication through enhancing viral promoter activation [27,85,86]. Our identification of IRF8 as a positive regulator for EBV reactivation provides another example of IRFs in promoting herpesvirus lytic replication.
IRF8 is a unique member of the IRF family. It is highly expressed in B cells [87] and plays a critical role in B cell biology [88]. A recent study showed that IRF8 regulates EBV latency and the apoptosis of EBV-positive B cells [45]. However, the contribution of IRF8 to EBV lytic replication remained unclear prior to our study.
Using a CRISPR/Cas9 genomic editing method, we for the first time demonstrated that IRF8 depletion dramatically suppresses the reactivation of EBV (Figs 1 and 4). IRF8 positively regulates apoptosis in different types of cells, including B cells [44,48,49,50,89]. Our RNA-seq and western blot analyses showed that IRF8 modulates caspase activation during EBV lytic replication (Figs 2 and 3). Especially, IRF8 binds to and enhances CASP1 gene promoter activity (Fig 5) and caspase-1 expression is critical for EBV reactivation (Figs 6 and 7), partially through KAP1 cleavage (Figs 8 and 9). The regulation of caspase-1 by IRF8 may also contribute to subsequent BPLF1 cleavage, which has been shown to facilitate EBV DNA replication [90]. In addition, the cleavage of other cellular [56,91,92,93,94] or potentially viral proteins by caspase-1 and other caspases could also contribute to EBV reactivation. In addition to caspase cleavage of BPLF1, caspase-3 was reported cleave LMP1 in Hela cells while the functional importance is not clear [95]. Using bioinformatic tools PeptideCutter and GraBCas [96,97], we also predicted the potential caspase cleavage sites for EBV proteins and found that many other viral proteins, such as BCRF1/vIL10, may also be potentially cleaved by caspases (S2 Table). Further detailed studies are required to prove their cleavage and the subsequent functional importance during EBV reactivation.
Several studies showed that EBV lytic reactivation is closely associated with apoptosis and that caspase activation promotes EBV lytic replication in EBV-transformed LCLs and EBV-infected gastric cancer (AGS) cells [51,52]. However, the underlying mechanisms for caspase activation in EBV lytic replication were not clear. Here we provide evidence that caspase activation-induces de-stabilization of cellular factors KAP1, PAX5 and DNMT3A contributes to efficient EBV replication (Fig 3). KAP1 is a corepressor that inhibits the reactivation of multiple herpesviruses [12,57,58,98,99]. Although phosphorylation of KAP1 overcomes KAP1-mediated inhibition, our study suggested that caspase-1/-8-mediated cleavage provides another means to antagonize KAP1-mediated inhibition (Fig 8). PAX5 is a B-cell-specific transcription factor that promotes EBV latency and suppresses lytic reactivation [8,60,61,62]. A previous study suggested that the lytic triggers TPA and sodium butyrate facilitate PAX5 destabilization through down-regulation of its mRNA expression [8] and BCR stimulation of B cells also decreases the level of PAX5 mRNA [100]. Our demonstration of caspase activation in PAX5 degradation provides an additional layer of regulation of PAX5 during EBV lytic replication. The de novo DNA methyltransferase DNMT3A contribute to γ-herpesvirus latency by suppressing viral lytic gene promoters through methylation [63]. It is conceivable that the down-regulation of DNMT3A by caspase activation would facilitate viral lytic replication.
Recent studies suggested that not only the decrease of IRF8 but also the increase of IRF4 is required for B cell differentiation, and that the IRF4/IRF8 ratios provide the differential signal for plasmablast versus germinal center plasma cell fate [70,88]. In Akata (EBV+) B cells, the expression of IRF4 is very low revealed by RNA-Seq (S6 Fig) and IRF4 protein is not detectable by western blot analysis [46]. Therefore, in the absence of IRF4, IRF8 depletion may not be sufficient to trigger B cell differentiation.
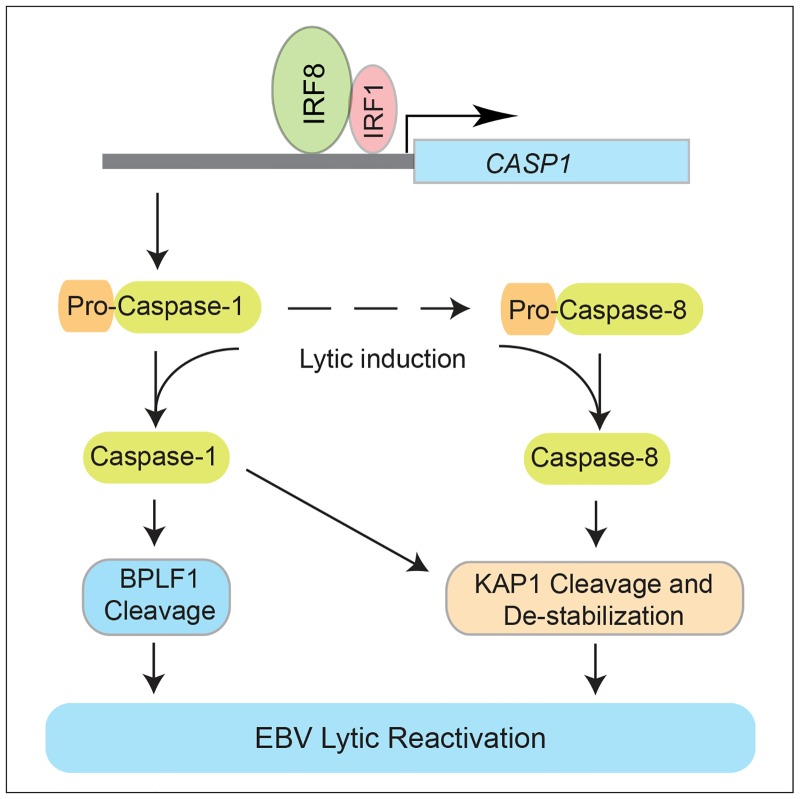
Although IRF8 normally suppresses B cell differentiation to plasma cells [101], a process that positively contributes to EBV reactivation [7], the results of our current work and the studies of others support a model in which IRF8 facilitates the reactivation of EBV upon lytic induction (Fig 10). IRF8 plays a key role in maintaining caspase-1 expression, a cellular protease critical for EBV reactivation upon lytic induction. Caspase-1 activation can trigger the specific cleavage of EBV BPLF1 for efficient viral DNA replication [90]. The activation of caspase-1 and caspase-8 can lead to the cleavage and destabilization of KAP1 and thus enhanced EBV replication.
Fig 10. Hypothesized model by which IRF8 contributes to EBV lytic replication.
IRF8 regulates the protein levels of caspase-1 and caspase-8. BCR stimulation triggers the activation of caspases and subsequent BPLF1 cleavage and the destabilization of KAP1, which leads to enhanced viral gene expression and DNA replication.
As a positive regulator of interferon signaling, IRF8 might also function as an anti-viral factor [102,103,104] by promoting interferon signaling during primary EBV infection, which could then limit viral lytic infection and facilitate the establishment of latency. Future studies are required to examine this possibility.
In summary, our study suggests that IRF8 positively regulates EBV lytic replication upon lytic induction. These findings provide valuable insights into our understanding of IRF8 and caspase activation in EBV lytic replication, which lays the foundation for developing novel therapeutic strategies against EBV-associated malignancies.
Materials and methods
Cell culture and reagents
Akata (EBV+) cells (gifts from Diane Hayward, Johns Hopkins University) were grown in RPMI 1640 media supplemented with 10% FBS (Cat# 26140079, Thermo Fisher Scientific) in 5% CO2 at 37°C [105,106]. The P3HR-1 cell (ATCC, HTB-62) was purchased from ATCC. The EBV-transformed lymphoblast cell lines (LCL, GM11830) was purchased from the Coriell Institute for Medical Research (Camden, NJ). The P3HR-1 cell was grown in RPMI 1640 media supplemented with 10% FBS. The LCL cell was cultured in RPMI 1640 media supplemented with 15% FBS. 293T cells (a gift from Diane Hayward, Johns Hopkins University) were grown in DMEM media supplemented with 10% FBS. The pan-caspase inhibitor (Z-VAD-FMK, Cat# A1902) was purchased from ApexBio.
Plasmids, cloning, and site-directed mutagenesis
Plasmid DNA was purified on miniprep columns according to the manufacturer’s protocol (Qiagen). pCMV3-N-FLAG and pCMV3-N-FLAG-IRF8 were obtained from Sino biological. pcDNA3.1-V5-His and pSG5 were obtained from Invitrogen and Stratagene, respectively. T vector pMD19 was bought from Clontech. pSG5-HA-KAP1 expression vector (pGL190) was a gift from Diane Hayward (Johns Hopkins) and contain the corresponding open reading frames in a derivative of pSG5 (Stratagene) [107]. The IRF1 ORF was cloned from Akata (EBV+) cDNA into pMD19 (Clontech) by PCR using the following primer sets: forward (5’-ATGCCCATCACTCGGATGC-3’) and reverse (5’-CTACGGTGCACAGGGAATGG-3’). IRF1 was then subcloned into pcDNA3.1-V5-His (Invitrogen) by using Gibson assembly and the following two primer sets: primer set-1, forward (5’-CCAGTGTGGTGGAATTGCCCTTGCTATGCCCATCACTCGGATGCGC-3’) and reverse (5’-CATTTTACCAACAGTACCGGAATGCCAAGCTTCGGTGCACAGGGAATGGCCTG-3’); primer set-2, forward (5’-CAGGCCATTCCCTGTGCACCGAAGCTTGGCATTCCGGTACTGTTGGTAAAATG-3’) and reverse (5’-GCGCATCCGAGTGATGGGCATAGCAAGGGCAATTCCACCACACTGG-3’). The pGL2-CASP1p1 (−488 to −8 relative to the CASP1 ORF) and pGL2-CASP1p2 (−488 to -66) luciferase reporter plasmids were constructed into the pGL2-basic vector (Promega) by using the Gibson assembly and the following two primer sets for pGL2-CASP1p1: primer set-1, forward (5’-GCTCTTACGCGTGCTAGCTCGAGTGTGAAAAGAAGGACATTAAATAAGAA-3’) and reverse (5’-CAACAGTACCGGAATGCCAAGCTTCTCTCCTCCCTTCTTGTGTGAC-3’); primer set-2, forward (5’-GTCACACAAGAAGGGAGGAGAGAAGCTTGGCATTCCGGTACTGTTG-3’) and reverse (5’-TTCTTATTTAATGTCCTTCTTTTCACACTCGAGCTAGCACGCGTAAGAGC-3’); and the following two primer sets for pGL2-CASP1p2: primer set-1, forward (5’-GCTCTTACGCGTGCTAGCTCGAGTGTGAAAAGAAGGACATTAAATAAGAA-3’) and reverse (5’-CAACAGTACCGGAATGCCAAGCTTGGGCCTGTACATGTATTGGGAAATACTCAC-3’); primer set-2, forward (5’-GTGAGTATTTCCCAATACATGTACAGGCCCAAGCTTGGCATTCCGGTACTGTTG-3’) and reverse (5’-TTCTTATTTAATGTCCTTCTTTTCACACTCGAGCTAGCACGCGTAAGAGC-3’).
Plasmids pCMV3-N-FLAG-IRF8(K108E) and pGL2-CASP1p1-mut (IRF8 binding site mutation) were constructed by using QuikChange II site-directed mutagenesis kit (Agilent Technologies, Santa Clara, CA, USA) and the following primer sets: IRF8(K108E) forward (5’-GGACATTTCCGAGCCATACGAGGTTTACCGAATTGTTCCTG-3’) and reverse (5’-CAGGAACAATTCGGTAAACCTCGTATGGCTCGGAAATGTCC-3’); CASP1p1-mut forward (5’-CCAAAAAGGAAGGCGAAGCATACTTTCAGTGGAAGTCACACAAGAAGGGAGGAGAGAAGCTTG -3’) and reverse (5’-CAAGCTTCTCTCCTCCCTTCTTGTGTGACTTCCACTGAAAGTATGCTTCGCCTTCCTTTTTGG -3’) DNA sequences in all these plasmids were authenticated by automatic sequencing.
IRF8, CASP1 and KAP1 depletion by CRISPR/Cas9 genomic editing
To deplete IRF8 or CASP1, two different sgRNAs targeting human IRF8 or CASP1 were designed and cloned into lentiCRISPR v2 vector (a gift from Feng Zhang; Addgene plasmid # 52961) [108]. Packaging 293T cells were transfected with IRF8 or CASP1 sgRNAs or negative controls (non-targeting sgRNA-NC) and helper vectors (pMD2.G and psPAX2; gifts from Didier Trono; Addgene plasmid #s 12259 and 12260) using Lipofectamine 2000 reagent (Cat# 11668019, Life Technologies). Medium containing lentiviral particles and 8 μg/mL polybrene (Sigma-Aldrich, St. Louis) was used to infect Akata (EBV+) cells. Infected cells were selected in medium containing 2 μg/mL puromycin.
To deplete KAP1, two different sgRNAs targeting human KAP1 were designed and cloned into lentiCRISPR v2-Blast vector (a gift from Mohan Babu, Addgene plasmid #83480). Packaging 293T cells were transfected with KAP1 sgRNAs or negative controls (non-targeting sgRNA-NC) and helper vectors (pMD2.G and psPAX2) using Lipofectamine 2000 reagent. Medium containing lentiviral particles and 8 μg/mL polybrene were used to infect caspase-1 knockout cell lines. Infected cells were selected in medium containing 10 μg/mL blasticidin.
The target guides sequences are as follows: IRF8-sg1: forward (5’-CACCGATTGACAGTAGCATGTATCC-3’) and reverse (5’-AAACGGATACATGCTACTGTCAATC-3’); IRF8-sg2: forward (5’-CACCGCGGAAATGTCCAGTTGGGAC-3’) and reverse (5’-AAACGTCCCAACTGGACATTTCCGC-3’); CASP1-sg1: forward (5’-CACCGGACAGTATTCCTAGAAGAAC-3’) and reverse (5’-AAACGTTCTTCTAGGAATACTGTCC-3’); CASP1-sg2: forward (5’-CACCGTTATCCGTTCCATGGGTGA-3’) and reverse (5’-AAACTCACCCATGGAACGGATAAC-3’); sgRNA-NC: forward (5’-CACCGTGAGGATCATGTCGAGCGCC-3’) and reverse (5’-AAACGGCGCTCGACATGATCCTCAC-3’); KAP1-sg1: forward (5’-CACCGGCGGGTGAAGTACACCAAGG-3’) and reverse (5’-AAACCCTTGGTGTACTTCACCCGCC-3’); KAP1-sg2: forward (5’-CACCGAGTCTCGGGATGGTGAACGT-3’) and reverse (5’-AAACACGTTCACCATCCCGAGACTC-3’).
Sequencing of CRISPR targeting region
IRF8 or CASP1 knockdown efficiency was confirmed using western blot analysis and Sanger sequencing. In details, the PAM region (containing the target site of sgRNA) was amplified from DNA mixture extracted from three biological IRF8-sg1, IRF8-sg2, CASP1-sg1 and CASP1-sg2 pool cells, respectively by using Wizard Genomic DNA Purification Kit (Fisher). The primer sets used for cloning are as follows: IRF8-sg1: forward (5’-AATGGTGGTCGGCGGCTTC-3’) and reverse (5’-AATGGAGGCATCCACTTCCTGATT-3’); IRF8-sg2: forward (5’-GCCTGGGCAGTTTTTAAAGGGAAG-3’) and reverse (5’-TCGGTAAACTTTGTATGGCTCGGAAA-3’); CASP1-sg1: forward (5’-TCAATTCTGTTCCCCCTTTTCAAT-3’) and reverse (5’-AGGCTTGTGCTGCATGACTCTTAT-3’); CASP1-sg2: forward (5’-TGGGCTATTTCTGCTTCATTACTTT-3’) and reverse (5’-CCTTTCGGAATAACGGAGTCAATC-3’). The PCR amplicons were subcloned into pMD19 vectors (Clontech) and more than 10 clones were randomly chosen for sequencing.
RNA-seq analysis
Total RNA from three biological replicates (cells derived from three distinct lentivrial transductions) was extracted using ISOLATE II RNA Mini Kit (Bioline). The library construction, cluster generation and HiSeq (Illumina) sequencing were performed with by the Genomics Sequencing Core of the Department of Environmental Health (University of Cincinnati) following the previous reported methods [109]. Raw fastq data were analyzed by using Galaxy (https://usegalaxy.org/). Human genome (hg38) was used as the reference genome. Differential gene expression between IRF8-depleted (IRF8-sg2) and control (NC) cells was analyzed by using DESeq2 [110]. The differentially expressed genes were selected based on a false-discovery rate–adjusted q-value (q< 0.05). Genes with more than 2-fold change were selected for further analysis. RNA-seq raw data have been submitted to National Center for Biotechnology Information (NCBI) Sequence Read Archive (SRA; accession numbers: SRP107862) with access URL https://www.ncbi.nlm.nih.gov/Traces/study/?acc=SRP107862.
Chromatin-immunoprecipitation (ChIP)
2x107 Akata (EBV+), LCL and P3HR-1 cells were cross-linked individually in 1% (w/v) formaldehyde (Sigma) for 5 min at room temperature and the cross-linking reaction was quenched by addition of glycine to a final concentration of 0.125M. Cells were washed twice with cold PBS and lysed in 1 ml of cell lysis buffer (10 mM Tris-HCl [pH 8.0], 10 mM NaCl, 0.2% [v/v] NP40, 10 mM Sodium butyrate, 50 μg/ml PMSF) with fresh added complete protease inhibitor on ice for 10 min. After centrifuge at 2,500 rpm at 4°C for 5 min, the supernatant was discarded and the nuclei were resuspended in 1.2 ml nuclei lysis buffer (50 mM Tris-HCl [pH 8.1], 10 mM EDTA, 1% [w/v] SDS, 10 mM Sodium butyrate, 50 μg/ml PMSF) with fresh added complete protease inhibitor on ice for 10 min. Then sonication was performed with a Diagenode Bioruptor 300. After extract clearing by centrifugation, supernatants were diluted 1:10 in dilution buffer (20 mM Tris-HCl [pH 8.1], 150 mM NaCl, 2 mM EDTA, 1% [v/v] Triton X-100, 0.01% [w/v] SDS, 10 mM Sodium butyrate 50 μg/ml PMSF) with fresh added complete protease inhibitor. Aliquots of each input chromatin lysate were reserved for PCR analysis. 1 ml of diluted chromatin lysate was incubated with ChIP-grade antibodies with rotation at 4°C overnight. Primary antibodies used were anti-IRF8 (Santa Cruz, Cat # sc-6058X), normal goat IgG (Santa Cruz, Cat # sc-2028), anti-IRF1 (abcam, Cat # ab26109), and normal rabbit IgG (Santa Cruz, Cat # sc-2027). 25 μl Protein A/G magnetic beads (life technologies, 10002D and 10004D) were added to each 1 ml ChIP and incubated for 2 hour at 4°C with rotation. Next, magnetic beads were pelleted with magnetic separation rack and washed once with cold low salt wash buffer (20 mM Tris-HCl [pH8.1], 2 mM EDTA, 150 mMNaCl, 1% [v/v] Triton X-100, 0.1% [w/v] SDS), once with high salt wash buffer (identical to low salt wash buffer, except 500 mM NaCl), once with LiCl wash buffer (10 mM Tris-HCl [pH8.1], 1 mM EDTA, 0.25 M LiCl, 1% [v/v] NP40, 1% Deoxycholic acid), and finally twice with TE buffer (10 mM Tris-HCl [pH8.1], 1 mM EDTA). Samples were then resuspended in 150 μl of elution buffer (0.1 M NaHCO3, 1% [w/v] SDS) and rotated for 20 min at room temperature. Two rounds of elution of protein-DNA complexes were pooled. Reversal of cross-linking was accomplished by incubation of pooled eluates at 65°C for 4 hours after addition of NaCl to final concentration of 200mM and 100 ug/ml Proteinase K. DNA was purified by phenol-chloroform extraction followed by isopropanol-sodium acetate precipitation and then resuspended in 100 μl nuclease-free water and quantified using regular PCR. Purified input chromatin lysate was used in PCR reactions for standardization. ChIP primers used to amplify the CASP1 promoter are: forward (5’-TACACTACCTGATGCAGGCTA-3’) and reverse (5’-TGAAACTGAAAGTATGCTTCG-3’).
Reverse transcription and quantitative PCR (RT-qPCR)
Total RNA was extracted using ISOLATE II RNA Mini Kit (Bioline). Reverse transcription was carried out by using High Capacity cDNA Reverse Transcription Kit (Invitrogen). Quantitative PCR (qPCR) was performed using an ABI Prism 7000 Sequence Detector with SYBR Green. The PCR reactions were set up in a 96-well optical plate in duplicate by adding the following reagents into each well: 2 μl of cDNA, 10 μl of SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA); the final concentrations of primers were 0.3 μmol/L in a final volume of 20 μl. The PCR amplification protocol was initiated at 50°C for 2 min followed by 10 min at 95°C and 40 PCR cycles consisting of 15 seconds at 95°C followed by 60°C for 1 min. All samples were tested with the reference gene β-actin for data normalization to correct for variations in RNA quality and quantity. The specificity of amplification of targets with high Ct values was confirmed by analysis of the temperature dissociation curves. Primers used for measuring gene transcriptional level: RTA and β-actin primers were described previously [13]; ZTA primers are forward 5’-AGGCCAGCTCACTGCCTATC-3’ and reverse 5’-TGATTCTGGGTTATGTCTGA-3’; BGLF2 primers are forward 5’-ATCTGGCACCTGTCCTTGTC-3’ and reverse5’-GGGACCTCTTTCCCATTAGC-3’; BGLF4 primers are forward 5’-GGCAATAGAGGCGATAGAGC-3’ and reverse 5’-TGGTCCTGACTGATTATGGG-3’; CASP1 primers are forward 5’-ATAGCTGGGTTGTCCTGCAC-3’ and reverse 5’-GCCAAATTTGCATCACATACA-3’; AIM2 primers are forward 5’-TAGCGCCTCACGTGTGTTAG-3’ and reverse 5’-TTGAAGCGTGTTGATCTTCG-3’; IFNB1 primers are forward 5’-CAGGAGAGCAATTTGGAGGA-3’ and reverse 5’-CTTTCGAAGCCTTTGCTCTG-3’; SLAMF7 primers are forward 5’-GAACCGACCAGCTCTTTCAC-3’ and reverse 5’-AATATGGCTGGTTCCCCAAC-3’; SULF1 primers are forward 5’-ATCCTGGTTGAATAATCAATCTCT-3’ and reverse 5’-ATGCAGGTTCTTCAAGGCAG-3’; TNFSF10 primers are forward 5’-AGCAATGCCACTTTTGGAGT-3’ and reverse 5’-TTCACAGTGCTCCTGCAGTC-3’; MX1 primers are forward 5’-GATGATCAAAGGGATGTGGC-3’ and reverse 5’-AGCTCGGCAACAGACTCTTC-3’; DAPL1 primers are forward 5’-TGCCCTGAATGACGCACTG-3’ and reverse 5’-GTGGGTTTTTGATGCGCCAT-3’; CASP8 primers are forward 5’-TGTCCAGTTGTTCCCCAATA-3’ and reverse 5’-GGTCACTTGAACCTTGGGAA-3’.
IRF8 reconstitution
The pLX304 vector was a gift from David Root (Addgene plasmid # 25890). The V5-tagged pLX304-IRF8 was purchased from DNASU Plasmid Repository. To prepare lentiviruses, 293T cells were transfected with empty vector or pLX304 containing the gene of IRF8 and the help vectors (pMD2.G and psPAX2) using Lipofectamine 2000 reagent. The supernatants were harvested at 48 h after transfection. The medium containing lentiviral particles and 8 μg/mL polybrene were used to infect IRF8-depleted (sg2) cell lines. Infected cells were selected in medium containing 10 μg/mL blasticidin.
Luciferase reporter assay
Luciferase assay was performed as previously described [16]. Briefly, 293T cells were co-transfected with the firefly luciferase reporter vectors along with IRF8 (WT or K108E mutant), IRF1, and renilla expression plasmids using Lipofectamine 2000 reagent (Cat# 11668019, Life Technologies). The Akata (EBV+) cell was transfected using electroporation method. For plasmid transfection, 10 μg each of plasmid were mixed with 5x106 cells in a 4-mm cuvette. Electroporation was performed at 970 μF and 0.2 V with a Gene pulser Xcell system (Bio-Rad). The cells were transferred to new plates contain 10 ml pre-warmed fresh medium. At thirty-six hours post-transfection, cell extracts were prepared and assayed with the dual-luciferase assay kit from Promega (Cat #E1960, Madison, WI, USA). Each condition was performed in triplicate.
Lytic induction and measurement of viral DNA copy number
Akata (EBV+) cells were treated with 50 μg/ml of goat anti-human IgG (MP Biomedicals) for 24 and 48 h to induce the EBV lytic cycle. For caspase inhibition assay, Akata (EBV+) cells were untreated or pretreated with pan-caspase inhibitor for 1 hr and then treated with anti-IgG (1:200, Cat# 55087, MP Biomedicals) for additional 48 hrs. EBV reactivation in P3HR-1 cells was triggered by addition of TPA (20 ng/ml) and sodium butyrate (3 mM; Millipore, Cat# 19–137). The EBV lytic replication in LCL cells was induced by addition of gemcitabine (1 μg/mL; Fisher Scientific, Cat# NC9325685). To induce the BCR activation, the LCL cells were treated with anti-IgM antibody (20 μg/mL, Cat# 2020–01, Southern Biotech) for 0 to 48 hrs.
To measure EBV replication, intracellular viral DNA and virion-associated DNA present in culture supernatant were determined by qPCR analysis [13]. Total genomic DNA was extracted by using Wizard Genomic DNA Purification Kit (Promega, Madison, WI, USA). For extracellular viral DNA extraction, the supernatant (120 μl) was treated with 4 μl RQ1 DNase (Promega) for 1 h at 37°C, and reactions were stopped by adding 20 μl of stop buffer and incubation at 65°C for 10 min; 12.5 μl proteinase K (20 mg/ml, Invitrogen) and 25 μl 10% (wt/vol) SDS then were added to the reaction mixtures, which were incubated for 1 h at 65°C. DNA was purified by phenol-chloroform extraction followed by isopropanol-sodium acetate precipitation and then resuspended in 100 μl nuclease-free water. qPCR was performed as mentioned above. Relative levels of viral DNA were normalized to supernatant viral DNA without lytic induction. The BALF5 primers used for quantitating EBV copy numbers were described previously [13,105]. The reference gene β-actin was used for data normalization.
In vitro caspase cleavage assay
In vitro cleavage assay was performed as previously described [94]. Briefly, HA-tagged KAP1 was immunoprecipitated from transfected 293T cells using HA magnetic beads. The beads-bound HA-KAP1 and individual active caspases (active human caspases group IV; ApexBio, Cat# K2060) were incubated in caspase assay buffer (50 mM HEPES, pH7.2, 50 mM NaCl, 0.1% Chaps, 10 mM EDTA, 5% Glycerol and 10mM DTT) at 37°C for 2 hrs. Reactions were stopped by boiling in 2× SDS sample buffer and samples were analyzed by western blot.
Immunoblot analysis
Cell lysates were harvested in lysis buffer including protease inhibitors (Roche) as described previously[106]. Protein concentration was determined using the Bradford assay (Biorad), and proteins were separated in SDS 4–20% polyacrylamide gels and then transferred onto a PVDF membrane. Membranes were blocked in TBS containing 5% milk, and 0.1% Tween 20 solution. Membranes were then incubated in the following primary antibodies: mouse anti-ZTA (Argene, Cat # 11–007, 1:5,000), mouse anti-RTA (Argene, 1:1,000), mouse anti-BGLF4 antibody (1:1,000) [111], anti-β-actin (Sigma, Cat # A5441, 1:5,000), anti-IRF8 (CST, Cat #5628, 1:1,000), anti-PARP (CST, Cat #9532, 1:1,000), anti-Cleaved PARP (CST, Cat #5625, 1:1,000), anti-Cleaved Caspase Substrates (CST, Cat #8698, 1:1,000), anti-Caspase-1 (CST, Cat #3866, 1:1,000), anti-Caspase-2 (CST, Cat #2224, 1:1,000), anti-Caspase-3 (Santa Cruz, Cat #sc-7148, 1:1,000), anti-Cleaved Caspase-3 (CST, Cat #9664, 1:1,000), anti-Caspase-7 (CST, Cat #12827, 1:1,000), anti-Cleaved Caspase-7 (CST, Cat #8438, 1:1,000), anti-Caspase-8 (CST, Cat #9746, 1:1,000), anti-Cleaved Caspase-8 (CST, Cat #9496, 1:1,000), anti-Caspase-9 (CST, Cat #9508, 1:1,000), anti-Bcl-2 (Bethyl, Cat #A303-675A, 1:1,000), anti-KAP1 (CST, Cat #4123, 1:1,000), anti-PAX5 (CST, Cat #8970, 1:1,000), anti-DNMT3A (Bethyl, Cat #A304-278A, 1:1,000), anti-STAT3 (CST, Cat #9139, 1:1,000), and anti-HA (CST, Cat #14031S, 1:1,000). The secondary antibodies used were horseradish peroxidase (HRP)-labeled goat anti-mouse antibody (Fisher Scientific, 1:5,000) and HRP-labeled anti-rabbit antibody (Fisher scientific, 1:5,000).
Bioinformatics analysis
Potential caspase cleavage sites were searched for all the EBV protein sequences using PeptideCutter (http://web.expasy.org/peptide_cutter/) and the GraBCas software [96,97].
Statistical analysis
All numerical data were presented as mean ± standard deviation of triplicate assays. The statistical significances were determined using Student’s two-tail t-test, where p<0.05 was considered statistically significant.
Supporting information
A. The transcription level of all the genes identified in IRF8-sg2 and NC cell lines. B. Differentially expressed genes between IRF8-sg2 and NC cell lines.
(XLSX)
(XLSX)
The sequencing of IRF8-depleted cell lines showing that 10 out of 22 clones for sg1 and 9 out of 14 clones for sg2 contain frame shifts. The PAM sequences were highlighted by red and the guide RNA sequences were shown in bold. WT: wild-type; “+” or “-” followed by numbers indicates the number of base pair inserted or deleted; “S” followed by numbers indicates the number of site mutations; “×” followed by numbers indicates the number of clones obtained in the sequencing.
(TIF)
A. Akata (EBV+) IRF8-sg2 cells were used to establish IRF8-expressing stable cell lines using a pLX-IRF8 lentiviral construct. Western blot analyses showing IRF8, ZTA, RTA and BGLF4 expression level in different cell lines upon IgG cross-linking as indicated. B. Intracellular viral DNA from cells treated as in (A) was measured by qPCR using primers to EBV BALF5. The value of vector control at 0 hr (lane 4) was set as 1. Data are presented as means ± standard deviations of triplicate assays. ** p<0.01.
(TIF)
A. RT-qPCR validation of the 8 apoptosis-related genes in IRF8-sg1 cells. B and C. IRF8 depletion (sg1) suppresses caspase-1 expression and the generation of cleaved caspase substrates upon lytic induction by anti-IgG cross-linking. Western blot analysis of protein extracts from Fig 1C using antibodies against caspase-1, PARP, and cleaved caspase substrates as indicated in panel (B). Western blot analysis of protein extracts from Fig 1C using antibodies against caspase-3, cleaved caspase-3, caspase-8, cleaved caspase-8, caspase-7, cleaved caspase-7, caspase-9, cleaved caspass-9, caspase-2, Bcl2, KAP1, PAX5, DNMT3A and STAT3 as indicated in panel (C).
(TIF)
RPKM, Reads Per Kilobase of transcript per Million mapped reads.
(TIF)
A. ChIP-PCR analysis using three EBV-positive cells [Akata (EBV+), P3HR-1 and LCLs] showing IRF8/IRF1 binding to CASP1 promoter. ChIP by a nonspecific IgG was include as negative controls. B. The pGL2-CASP1p-1-Luc constructs were co-transfected into Akata (EBV+) cells with either 10 ug of IRF8, IRF1 or IRF8-K108E expression vectors. Luciferase assays were performed 36 hrs post-transfection. The value of cells transfected with an empty vector was set as 1. The results were presented as mean ± standard deviation of triplicate assays. ** p<0.01, *** p<0.001.
(TIF)
RPKM, Reads Per Kilobase of transcript per Million mapped reads.
(TIF)
The sequencing of CASP1-depleted cell lines showing that 8 out of 13 clones for CASP1-sg1 and 12 out of 14 clones for CASP1-sg2 contain frame shifts. The PAM sequences were highlighted by red and the guide RNA sequences were shown in bold. WT: wild-type; “+” or “-” followed by numbers indicates the number of base pair inserted or deleted; “S” followed by numbers indicates the number of site mutations; “×” followed by numbers indicates the number of clones obtained in the sequencing.
(TIF)
qPCR analysis showing that CASP8 mRNA level was slightly increased by CASP1 depletion. The value was normalized by qPCR using specific primers to β-actin. Data are presented as means ± standard deviations of triplicate assays.
(TIF)
Acknowledgments
We thank Diane Hayward and Iain Morgan for comments and suggestions for the article. We thank Diane Hayward for providing cell lines and EBV ZTA/RTA and KAP1 constructs. We thank Shannon Kenney for providing us the Hela-B95-8 cell line and Mei-Ru Chen for anti-BGLF4 antibody. We thank Feng Zhang for sharing the lentiCRISPR v2 plasmid (Addgene plasmid # 52961) and Didier Trono for providing the pMD2.G and psPAX2 plasmids (Addgene plasmid #s 12259 and 12260). We also thank David Root for providing the pLX304 vector (Addgene plasmid # 25890) and Mohan Babu for lentiCRISPR v2-Blast vector (Addgene plasmid #83480).
Data Availability
RNA-seq raw data have been submitted to National Center for Biotechnology Information (NCBI) Sequence Read Archive (SRA; accession numbers: SRP107862) with access URL https://www.ncbi.nlm.nih.gov/Traces/study/?acc=SRP107862.
Funding Statement
This work was supported by NIH K99AI104828/R00AI104828 to RL. The work was also partly supported by Institutional Research Grant IRG-14-192-40 from the American Cancer Society. RL received support from the VCU Philips Institute for Oral Health Research and the VCU NCI Designated Massey Cancer Center (NIH P30 CA016059) (http://grants.nih.gov/grants/oer.htm). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Young LS, Yap LF, Murray PG (2016) Epstein-Barr virus: more than 50 years old and still providing surprises. Nature Reviews Cancer 16: 789–802. doi: 10.1038/nrc.2016.92 [DOI] [PubMed] [Google Scholar]
- 2.Hammerschmidt W, Sugden B (2013) Replication of Epstein–Barr Viral DNA. Cold Spring Harbor perspectives in biology 5: a013029 doi: 10.1101/cshperspect.a013029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zalani S, Holley-Guthrie E, Kenney S (1995) The Zif268 cellular transcription factor activates expression of the Epstein-Barr virus immediate-early BRLF1 promoter. J Virol 69: 3816–3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu FY, Wang SE, Chen H, Wang L, Hayward SD, et al. (2004) CCAAT/enhancer binding protein alpha binds to the Epstein-Barr virus (EBV) ZTA protein through oligomeric interactions and contributes to cooperative transcriptional activation of the ZTA promoter through direct binding to the ZII and ZIIIB motifs during induction of the EBV lytic cycle. J Virol 78: 4847–4865. doi: 10.1128/JVI.78.9.4847-4865.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson AR, Kwek SS, Kenney SC (2012) The B-cell specific transcription factor, Oct-2, promotes Epstein-Barr virus latency by inhibiting the viral immediate-early protein, BZLF1. PLoS Pathog 8: e1002516 doi: 10.1371/journal.ppat.1002516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson AR, Kwek SS, Hagemeier SR, Wille CK, Kenney SC (2011) Cellular transcription factor Oct-1 interacts with the Epstein-Barr virus BRLF1 protein to promote disruption of viral latency. J Virol 85: 8940–8953. doi: 10.1128/JVI.00569-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reusch JA, Nawandar DM, Wright KL, Kenney SC, Mertz JE (2015) Cellular differentiation regulator BLIMP1 induces Epstein-Barr virus lytic reactivation in epithelial and B cells by activating transcription from both the R and Z promoters. J Virol 89: 1731–1743. doi: 10.1128/JVI.02781-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raver RM, Panfil AR, Hagemeier SR, Kenney SC (2013) The B-cell-specific transcription factor and master regulator Pax5 promotes Epstein-Barr virus latency by negatively regulating the viral immediate early protein BZLF1. J Virol 87: 8053–8063. doi: 10.1128/JVI.00546-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nawandar DM, Wang A, Makielski K, Lee D, Ma S, et al. (2015) Differentiation-Dependent KLF4 Expression Promotes Lytic Epstein-Barr Virus Infection in Epithelial Cells. PLoS Pathog 11: e1005195 doi: 10.1371/journal.ppat.1005195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nawandar DM, Ohashi M, Djavadian R, Barlow E, Makielski K, et al. (2017) Differentiation-Dependent LMP1 Expression Is Required for Efficient Lytic Epstein-Barr Virus Reactivation in Epithelial Cells. J Virol 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murata T, Narita Y, Sugimoto A, Kawashima D, Kanda T, et al. (2013) Contribution of myocyte enhancer factor 2 family transcription factors to BZLF1 expression in Epstein-Barr virus reactivation from latency. J Virol 87: 10148–10162. doi: 10.1128/JVI.01002-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Burton EM, Bhaduri-McIntosh S (2017) Chloroquine triggers Epstein-Barr virus replication through phosphorylation of KAP1/TRIM28 in Burkitt lymphoma cells. PLoS Pathog 13: e1006249 doi: 10.1371/journal.ppat.1006249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li R, Zhu J, Xie Z, Liao G, Liu J, et al. (2011) Conserved herpesvirus kinases target the DNA damage response pathway and TIP60 histone acetyltransferase to promote virus replication. Cell Host Microbe 10: 390–400. doi: 10.1016/j.chom.2011.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kraus RJ, Perrigoue JG, Mertz JE (2003) ZEB negatively regulates the lytic-switch BZLF1 gene promoter of Epstein-Barr virus. J Virol 77: 199–207. doi: 10.1128/JVI.77.1.199-207.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iempridee T, Reusch JA, Riching A, Johannsen EC, Dovat S, et al. (2014) Epstein-Barr virus utilizes Ikaros in regulating its latent-lytic switch in B cells. J Virol 88: 4811–4827. doi: 10.1128/JVI.03706-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang J, Liao G, Chen H, Wu FY, Hutt-Fletcher L, et al. (2006) Contribution of C/EBP proteins to Epstein-Barr virus lytic gene expression and replication in epithelial cells. J Virol 80: 1098–1109. doi: 10.1128/JVI.80.3.1098-1109.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kosowicz JG, Lee J, Peiffer B, Guo Z, Chen J, et al. (2017) Drug Modulators of B Cell Signaling Pathways and Epstein-Barr Virus Lytic Activation. J Virol 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takada K (1984) Cross-linking of cell surface immunoglobulins induces Epstein-Barr virus in Burkitt lymphoma lines. Int J Cancer 33: 27–32. [DOI] [PubMed] [Google Scholar]
- 19.Tamura T, Yanai H, Savitsky D, Taniguchi T (2008) The IRF family transcription factors in immunity and oncogenesis. Annu Rev Immunol 26: 535–584. doi: 10.1146/annurev.immunol.26.021607.090400 [DOI] [PubMed] [Google Scholar]
- 20.Mamane Y, Heylbroeck C, Génin P, Algarté M, Servant MJ, et al. (1999) Interferon regulatory factors: the next generation. Gene 237: 1–14. [DOI] [PubMed] [Google Scholar]
- 21.Savitsky D, Tamura T, Yanai H, Taniguchi T (2010) Regulation of immunity and oncogenesis by the IRF transcription factor family. Cancer immunology, immunotherapy 59: 489–510. doi: 10.1007/s00262-009-0804-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schaefer BC, Paulson E, Strominger JL, Speck SH (1997) Constitutive activation of Epstein-Barr virus (EBV) nuclear antigen 1 gene transcription by IRF1 and IRF2 during restricted EBV latency. Molecular and cellular biology 17: 873–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ning S, Huye LE, Pagano JS (2005) Interferon regulatory factor 5 represses expression of the Epstein-Barr virus oncoprotein LMP1: braking of the IRF7/LMP1 regulatory circuit. Journal of virology 79: 11671–11676. doi: 10.1128/JVI.79.18.11671-11676.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu D, Meyer F, Ehlers E, Blasnitz L, Zhang L (2011) Interferon regulatory factor 4 (IRF-4) targets IRF-5 to regulate Epstein-Barr virus transformation. Journal of Biological Chemistry 286: 18261–18267. doi: 10.1074/jbc.M110.210542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu D, Zhao L, Del Valle L, Miklossy J, Zhang L (2008) Interferon regulatory factor 4 is involved in Epstein-Barr virus-mediated transformation of human B lymphocytes. Journal of virology 82: 6251–6258. doi: 10.1128/JVI.00163-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang L, Pagano JS (1999) Interferon regulatory factor 2 represses the Epstein-Barr virus BamHI Q latency promoter in type III latency. Molecular and cellular biology 19: 3216–3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Flaherty BM, Soni T, Wakeman BS, Speck SH (2014) The murine gammaherpesvirus immediate-early Rta synergizes with IRF4, targeting expression of the viral M1 superantigen to plasma cells. PLoS Pathog 10: e1004302 doi: 10.1371/journal.ppat.1004302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bentz GL, Liu R, Hahn AM, Shackelford J, Pagano JS (2010) Epstein–Barr virus BRLF1 inhibits transcription of IRF3 and IRF7 and suppresses induction of interferon-β. Virology 402: 121–128. doi: 10.1016/j.virol.2010.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hahn AM, Huye LE, Ning S, Webster-Cyriaque J, Pagano JS (2005) Interferon regulatory factor 7 is negatively regulated by the Epstein-Barr virus immediate-early gene, BZLF-1. Journal of virology 79: 10040–10052. doi: 10.1128/JVI.79.15.10040-10052.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang J-T, Doong S-L, Teng S-C, Lee C-P, Tsai C-H, et al. (2009) Epstein-Barr virus BGLF4 kinase suppresses the interferon regulatory factor 3 signaling pathway. Journal of virology 83: 1856–1869. doi: 10.1128/JVI.01099-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee CH, Melchers M, Wang H, Torrey TA, Slota R, et al. (2006) Regulation of the germinal center gene program by interferon (IFN) regulatory factor 8/IFN consensus sequence-binding protein. The Journal of experimental medicine 203: 63–72. doi: 10.1084/jem.20051450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang W, Horvath E, Eklund EA (2007) PU. 1, interferon regulatory factor (IRF) 2, and the interferon consensus sequence-binding protein (ICSBP/IRF8) cooperate to activate NF1 transcription in differentiating myeloid cells. Journal of Biological Chemistry 282: 6629–6643. doi: 10.1074/jbc.M607760200 [DOI] [PubMed] [Google Scholar]
- 33.Huang W, Zhu C, Wang H, Horvath E, Eklund EA (2008) The interferon consensus sequence-binding protein (ICSBP/IRF8) represses PTPN13 gene transcription in differentiating myeloid cells. Journal of Biological Chemistry 283: 7921–7935. doi: 10.1074/jbc.M706710200 [DOI] [PubMed] [Google Scholar]
- 34.Kautz B, Kakar R, David E, Eklund EA (2001) SHP1 Protein-tyrosine Phosphatase Inhibits gp91PHOXand p67PHOX Expression by Inhibiting Interaction of PU. 1, IRF1, Interferon Consensus Sequence-binding Protein, and CREB-binding Protein with Homologous Cis Elements in the CYBB andNCF2 Genes. Journal of Biological Chemistry 276: 37868–37878. doi: 10.1074/jbc.M103381200 [DOI] [PubMed] [Google Scholar]
- 35.Unlu S, Kumar A, Waterman WR, Tsukada J, Wang KZ, et al. (2007) Phosphorylation of IRF8 in a pre-associated complex with Spi-1/PU. 1 and non-phosphorylated Stat1 is critical for LPS induction of the IL1B gene. Molecular immunology 44: 3364–3379. doi: 10.1016/j.molimm.2007.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chang T-H, Xu S, Tailor P, Kanno T, Ozato K (2012) The small ubiquitin-like modifier-deconjugating enzyme sentrin-specific peptidase 1 switches IFN regulatory factor 8 from a repressor to an activator during macrophage activation. The Journal of Immunology 189: 3548–3556. doi: 10.4049/jimmunol.1201104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim JY, Ozato K (2009) The sequestosome 1/p62 attenuates cytokine gene expression in activated macrophages by inhibiting IFN regulatory factor 8 and TNF receptor-associated factor 6/NF-κB activity. The Journal of Immunology 182: 2131–2140. doi: 10.4049/jimmunol.0802755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kong HJ, Anderson DE, Lee CH, Jang MK, Tamura T, et al. (2007) Cutting edge: autoantigen Ro52 is an interferon inducible E3 ligase that ubiquitinates IRF-8 and enhances cytokine expression in macrophages. The Journal of Immunology 179: 26–30. [DOI] [PubMed] [Google Scholar]
- 39.Tamura T, Nagamura-Inoue T, Shmeltzer Z, Kuwata T, Ozato K (2000) ICSBP directs bipotential myeloid progenitor cells to differentiate into mature macrophages. Immunity 13: 155–165. [DOI] [PubMed] [Google Scholar]
- 40.Tsujimura H, Tamura T, Gongora C, Aliberti J, e Sousa CR, et al. (2003) ICSBP/IRF-8 retrovirus transduction rescues dendritic cell development in vitro. Blood 101: 961–969. doi: 10.1182/blood-2002-05-1327 [DOI] [PubMed] [Google Scholar]
- 41.White CL, Kessler PM, Dickerman BK, Ozato K, Sen GC (2016) Interferon Regulatory Factor 8 (IRF8) Impairs Induction of Interferon Induced with Tetratricopeptide Repeat Motif (IFIT) Gene Family Members. Journal of Biological Chemistry 291: 13535–13545. doi: 10.1074/jbc.M115.705467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fragale A, Stellacci E, Ilari R, Remoli AL, Lanciotti A, et al. (2011) Critical role of IRF-8 in negative regulation of TLR3 expression by Src homology 2 domain-containing protein tyrosine phosphatase-2 activity in human myeloid dendritic cells. The Journal of Immunology 186: 1951–1962. doi: 10.4049/jimmunol.1000918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu Y, Jiang L, Fang J, Fang R, Morse HC III, et al. (2015) Loss of IRF8 Inhibits the Growth of Diffuse Large B-cell Lymphoma. Journal of Cancer 6: 953 doi: 10.7150/jca.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gabriele L, Phung J, Fukumoto J, Segal D, Wang IM, et al. (1999) Regulation of apoptosis in myeloid cells by interferon consensus sequence-binding protein. J Exp Med 190: 411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banerjee S, Lu J, Cai Q, Saha A, Jha HC, et al. (2013) The EBV latent antigen 3C inhibits apoptosis through targeted regulation of interferon regulatory factors 4 and 8. PLoS Pathog 9: e1003314 doi: 10.1371/journal.ppat.1003314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang L, Yao ZQ, Moorman JP, Xu Y, Ning S (2014) Gene expression profiling identifies IRF4-associated molecular signatures in hematological malignancies. PloS one 9: e106788 doi: 10.1371/journal.pone.0106788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lupey-Green LN, Moquin SA, Martin KA, McDevitt SM, Hulse M, et al. (2017) PARP1 restricts Epstein Barr Virus lytic reactivation by binding the BZLF1 promoter. Virology 507: 220–230. doi: 10.1016/j.virol.2017.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu X, Yang D, Zimmerman M, Liu F, Yang J, et al. (2011) IRF8 regulates acid ceramidase expression to mediate apoptosis and suppresses myelogeneous leukemia. Cancer Res 71: 2882–2891. doi: 10.1158/0008-5472.CAN-10-2493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang D, Thangaraju M, Browning DD, Dong Z, Korchin B, et al. (2007) IFN regulatory factor 8 mediates apoptosis in nonhemopoietic tumor cells via regulation of Fas expression. J Immunol 179: 4775–4782. [DOI] [PubMed] [Google Scholar]
- 50.Yang D, Wang S, Brooks C, Dong Z, Schoenlein PV, et al. (2009) IFN regulatory factor 8 sensitizes soft tissue sarcoma cells to death receptor-initiated apoptosis via repression of FLICE-like protein expression. Cancer Res 69: 1080–1088. doi: 10.1158/0008-5472.CAN-08-2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prasad A, Remick J, Zeichner SL (2013) Activation of human herpesvirus replication by apoptosis. J Virol 87: 10641–10650. doi: 10.1128/JVI.01178-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim H, Choi H, Lee SK (2015) Epstein-Barr Virus MicroRNA miR-BART20-5p Suppresses Lytic Induction by Inhibiting BAD-Mediated caspase-3-Dependent Apoptosis. J Virol 90: 1359–1368. doi: 10.1128/JVI.02794-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kenney SC, Mertz JE (2014) Regulation of the latent-lytic switch in Epstein-Barr virus. Semin Cancer Biol 26: 60–68. doi: 10.1016/j.semcancer.2014.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shimbo K, Hsu GW, Nguyen H, Mahrus S, Trinidad JC, et al. (2012) Quantitative profiling of caspase-cleaved substrates reveals different drug-induced and cell-type patterns in apoptosis. Proc Natl Acad Sci U S A 109: 12432–12437. doi: 10.1073/pnas.1208616109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Julien O, Zhuang M, Wiita AP, O’Donoghue AJ, Knudsen GM, et al. (2016) Quantitative MS-based enzymology of caspases reveals distinct protein substrate specificities, hierarchies, and cellular roles. Proc Natl Acad Sci U S A 113: E2001–2010. doi: 10.1073/pnas.1524900113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Julien O, Wells JA (2017) Caspases and their substrates. Cell Death Differ 24: 1380–1389. doi: 10.1038/cdd.2017.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gjyshi O, Roy A, Dutta S, Veettil MV, Dutta D, et al. (2015) Activated Nrf2 Interacts with Kaposi’s Sarcoma-Associated Herpesvirus Latency Protein LANA-1 and Host Protein KAP1 To Mediate Global Lytic Gene Repression. J Virol 89: 7874–7892. doi: 10.1128/JVI.00895-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rauwel B, Jang SM, Cassano M, Kapopoulou A, Barde I, et al. (2015) Release of human cytomegalovirus from latency by a KAP1/TRIM28 phosphorylation switch. Elife 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sun R, Liang D, Gao Y, Lan K (2014) Kaposi’s sarcoma-associated herpesvirus-encoded LANA interacts with host KAP1 to facilitate establishment of viral latency. J Virol 88: 7331–7344. doi: 10.1128/JVI.00596-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee N, Yario TA, Gao JS, Steitz JA (2016) EBV noncoding RNA EBER2 interacts with host RNA-binding proteins to regulate viral gene expression. Proc Natl Acad Sci U S A 113: 3221–3226. doi: 10.1073/pnas.1601773113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee N, Moss WN, Yario TA, Steitz JA (2015) EBV noncoding RNA binds nascent RNA to drive host PAX5 to viral DNA. Cell 160: 607–618. doi: 10.1016/j.cell.2015.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Arvey A, Tempera I, Tsai K, Chen HS, Tikhmyanova N, et al. (2012) An atlas of the Epstein-Barr virus transcriptome and epigenome reveals host-virus regulatory interactions. Cell Host Microbe 12: 233–245. doi: 10.1016/j.chom.2012.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gray KS, Forrest JC, Speck SH (2010) The de novo methyltransferases DNMT3a and DNMT3b target the murine gammaherpesvirus immediate-early gene 50 promoter during establishment of latency. J Virol 84: 4946–4959. doi: 10.1128/JVI.00060-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li X, Bhaduri-McIntosh S (2016) A Central Role for STAT3 in Gammaherpesvirus-Life Cycle and -Diseases. Front Microbiol 7: 1052 doi: 10.3389/fmicb.2016.01052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.King CA, Li X, Barbachano-Guerrero A, Bhaduri-McIntosh S (2015) STAT3 Regulates Lytic Activation of Kaposi’s Sarcoma-Associated Herpesvirus. J Virol 89: 11347–11355. doi: 10.1128/JVI.02008-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Koganti S, Clark C, Zhi J, Li X, Chen EI, et al. (2015) Cellular STAT3 functions via PCBP2 to restrain Epstein-Barr Virus lytic activation in B lymphocytes. J Virol 89: 5002–5011. doi: 10.1128/JVI.00121-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hill ER, Koganti S, Zhi J, Megyola C, Freeman AF, et al. (2013) Signal transducer and activator of transcription 3 limits Epstein-Barr virus lytic activation in B lymphocytes. J Virol 87: 11438–11446. doi: 10.1128/JVI.01762-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Daigle D, Megyola C, El-Guindy A, Gradoville L, Tuck D, et al. (2010) Upregulation of STAT3 marks Burkitt lymphoma cells refractory to Epstein-Barr virus lytic cycle induction by HDAC inhibitors. J Virol 84: 993–1004. doi: 10.1128/JVI.01745-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shin DM, Lee CH, Morse HC 3rd (2011) IRF8 governs expression of genes involved in innate and adaptive immunity in human and mouse germinal center B cells. PLoS One 6: e27384 doi: 10.1371/journal.pone.0027384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sciammas R, Shaffer AL, Schatz JH, Zhao H, Staudt LM, et al. (2006) Graded expression of interferon regulatory factor-4 coordinates isotype switching with plasma cell differentiation. Immunity 25: 225–236. doi: 10.1016/j.immuni.2006.07.009 [DOI] [PubMed] [Google Scholar]
- 71.Salem S, Langlais D, Lefebvre F, Bourque G, Bigley V, et al. (2014) Functional characterization of the human dendritic cell immunodeficiency associated with the IRF8(K108E) mutation. Blood 124: 1894–1904. doi: 10.1182/blood-2014-04-570879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Calattini S, Sereti I, Scheinberg P, Kimura H, Childs RW, et al. (2010) Detection of EBV genomes in plasmablasts/plasma cells and non-B cells in the blood of most patients with EBV lymphoproliferative disorders by using Immuno-FISH. Blood 116: 4546–4559. doi: 10.1182/blood-2010-05-285452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mboko WP, Rekow MM, Ledwith MP, Lange PT, Schmitz KE, et al. (2017) Interferon Regulatory Factor 1 and Type I Interferon Cooperate To Control Acute Gammaherpesvirus Infection. J Virol 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mboko WP, Olteanu H, Ray A, Xin G, Darrah EJ, et al. (2015) Tumor Suppressor Interferon-Regulatory Factor 1 Counteracts the Germinal Center Reaction Driven by a Cancer-Associated Gammaherpesvirus. J Virol 90: 2818–2829. doi: 10.1128/JVI.02774-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mboko WP, Mounce BC, Emmer J, Darrah E, Patel SB, et al. (2014) Interferon regulatory factor 1 restricts gammaherpesvirus replication in primary immune cells. J Virol 88: 6993–7004. doi: 10.1128/JVI.00638-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dutia BM, Allen DJ, Dyson H, Nash AA (1999) Type I interferons and IRF-1 play a critical role in the control of a gammaherpesvirus infection. Virology 261: 173–179. doi: 10.1006/viro.1999.9834 [DOI] [PubMed] [Google Scholar]
- 77.Mandal P, Krueger BE, Oldenburg D, Andry KA, Beard RS, et al. (2011) A gammaherpesvirus cooperates with interferon-alpha/beta-induced IRF2 to halt viral replication, control reactivation, and minimize host lethality. PLoS Pathog 7: e1002371 doi: 10.1371/journal.ppat.1002371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hwang S, Kim KS, Flano E, Wu TT, Tong LM, et al. (2009) Conserved herpesviral kinase promotes viral persistence by inhibiting the IRF-3-mediated type I interferon response. Cell Host Microbe 5: 166–178. doi: 10.1016/j.chom.2008.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bi X, Yang L, Mancl ME, Barnes BJ (2011) Modulation of interferon regulatory factor 5 activities by the Kaposi sarcoma-associated herpesvirus-encoded viral interferon regulatory factor 3 contributes to immune evasion and lytic induction. J Interferon Cytokine Res 31: 373–382. doi: 10.1089/jir.2010.0084 [DOI] [PubMed] [Google Scholar]
- 80.Liang Q, Fu B, Wu F, Li X, Yuan Y, et al. (2012) ORF45 of Kaposi’s sarcoma-associated herpesvirus inhibits phosphorylation of interferon regulatory factor 7 by IKKepsilon and TBK1 as an alternative substrate. J Virol 86: 10162–10172. doi: 10.1128/JVI.05224-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hwang SW, Kim D, Jung JU, Lee HR (2017) KSHV-encoded viral interferon regulatory factor 4 (vIRF4) interacts with IRF7 and inhibits interferon alpha production. Biochem Biophys Res Commun 486: 700–705. doi: 10.1016/j.bbrc.2017.03.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Forero A, McCormick KD, Jenkins FJ, Sarkar SN (2014) Downregulation of IRF4 induces lytic reactivation of KSHV in primary effusion lymphoma cells. Virology 458–459: 4–10. doi: 10.1016/j.virol.2014.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee HR, Doganay S, Chung B, Toth Z, Brulois K, et al. (2014) Kaposi’s sarcoma-associated herpesvirus viral interferon regulatory factor 4 (vIRF4) targets expression of cellular IRF4 and the Myc gene to facilitate lytic replication. J Virol 88: 2183–2194. doi: 10.1128/JVI.02106-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Forero A, Moore PS, Sarkar SN (2013) Role of IRF4 in IFN-stimulated gene induction and maintenance of Kaposi sarcoma-associated herpesvirus latency in primary effusion lymphoma cells. J Immunol 191: 1476–1485. doi: 10.4049/jimmunol.1202514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Matar CG, Rangaswamy US, Wakeman BS, Iwakoshi N, Speck SH (2014) Murine gammaherpesvirus 68 reactivation from B cells requires IRF4 but not XBP-1. J Virol 88: 11600–11610. doi: 10.1128/JVI.01876-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rangaswamy US, Speck SH (2014) Murine gammaherpesvirus M2 protein induction of IRF4 via the NFAT pathway leads to IL-10 expression in B cells. PLoS Pathog 10: e1003858 doi: 10.1371/journal.ppat.1003858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ersing I, Nobre L, Wang LW, Soday L, Ma Y, et al. (2017) A Temporal Proteomic Map of Epstein-Barr Virus Lytic Replication in B Cells. Cell Rep 19: 1479–1493. doi: 10.1016/j.celrep.2017.04.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xu H, Chaudhri VK, Wu Z, Biliouris K, Dienger-Stambaugh K, et al. (2015) Regulation of bifurcating B cell trajectories by mutual antagonism between transcription factors IRF4 and IRF8. Nat Immunol 16: 1274–1281. doi: 10.1038/ni.3287 [DOI] [PubMed] [Google Scholar]
- 89.Pathak S, Ma S, Shukla V, Lu R (2013) A role for IRF8 in B cell anergy. J Immunol 191: 6222–6230. doi: 10.4049/jimmunol.1301169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gastaldello S, Chen X, Callegari S, Masucci MG (2013) Caspase-1 promotes Epstein-Barr virus replication by targeting the large tegument protein deneddylase to the nucleus of productively infected cells. PLoS Pathog 9: e1003664 doi: 10.1371/journal.ppat.1003664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Agard NJ, Maltby D, Wells JA (2010) Inflammatory stimuli regulate caspase substrate profiles. Mol Cell Proteomics 9: 880–893. doi: 10.1074/mcp.M900528-MCP200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.De Leo A, Chen HS, Hu CA, Lieberman PM (2017) Deregulation of KSHV latency conformation by ER-stress and caspase-dependent RAD21-cleavage. PLoS Pathog 13: e1006596 doi: 10.1371/journal.ppat.1006596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Denes A, Lopez-Castejon G, Brough D (2012) Caspase-1: is IL-1 just the tip of the ICEberg? Cell Death Dis 3: e338 doi: 10.1038/cddis.2012.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang K, Lv D-W, Li R (2017) B Cell Receptor Activation and Chemical Induction Trigger Caspase-Mediated Cleavage of PIAS1 to Facilitate Epstein-Barr Virus Reactivation. Cell Rep 21: 3445–3457. doi: 10.1016/j.celrep.2017.11.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Togi S, Hatano Y, Muromoto R, Kawanishi E, Ikeda O, et al. (2016) Caspase-dependent cleavage regulates protein levels of Epstein-Barr virus-derived latent membrane protein 1. FEBS Lett 590: 808–818. doi: 10.1002/1873-3468.12119 [DOI] [PubMed] [Google Scholar]
- 96.Backes C, Kuentzer J, Lenhof HP, Comtesse N, Meese E (2005) GraBCas: a bioinformatics tool for score-based prediction of Caspase- and Granzyme B-cleavage sites in protein sequences. Nucleic Acids Res 33: W208–213. doi: 10.1093/nar/gki433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wilkins MR, Gasteiger E, Bairoch A, Sanchez JC, Williams KL, et al. (1999) Protein identification and analysis tools in the ExPASy server. Methods Mol Biol 112: 531–552. [DOI] [PubMed] [Google Scholar]
- 98.Zhang L, Zhu C, Guo Y, Wei F, Lu J, et al. (2014) Inhibition of KAP1 enhances hypoxia-induced Kaposi’s sarcoma-associated herpesvirus reactivation through RBP-Jkappa. J Virol 88: 6873–6884. doi: 10.1128/JVI.00283-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liao G, Huang J, Fixman ED, Hayward SD (2005) The Epstein-Barr virus replication protein BBLF2/3 provides an origin-tethering function through interaction with the zinc finger DNA binding protein ZBRK1 and the KAP-1 corepressor. J Virol 79: 245–256. doi: 10.1128/JVI.79.1.245-256.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hauser J, Verma-Gaur J, Wallenius A, Grundstrom T (2009) Initiation of antigen receptor-dependent differentiation into plasma cells by calmodulin inhibition of E2A. J Immunol 183: 1179–1187. doi: 10.4049/jimmunol.0900455 [DOI] [PubMed] [Google Scholar]
- 101.Carotta S, Willis SN, Hasbold J, Inouye M, Pang SH, et al. (2014) The transcription factors IRF8 and PU.1 negatively regulate plasma cell differentiation. J Exp Med 211: 2169–2181. doi: 10.1084/jem.20140425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sun L, St Leger AJ, Yu CR, He C, Mahdi RM, et al. (2016) Interferon Regulator Factor 8 (IRF8) Limits Ocular Pathology during HSV-1 Infection by Restraining the Activation and Expansion of CD8+ T Cells. PLoS One 11: e0155420 doi: 10.1371/journal.pone.0155420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ayithan N, Bradfute SB, Anthony SM, Stuthman KS, Bavari S, et al. (2015) Virus-like particles activate type I interferon pathways to facilitate post-exposure protection against Ebola virus infection. PLoS One 10: e0118345 doi: 10.1371/journal.pone.0118345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tussiwand R, Everts B, Grajales-Reyes GE, Kretzer NM, Iwata A, et al. (2015) Klf4 expression in conventional dendritic cells is required for T helper 2 cell responses. Immunity 42: 916–928. doi: 10.1016/j.immuni.2015.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li R, Liao G, Nirujogi RS, Pinto SM, Shaw PG, et al. (2015) Phosphoproteomic profiling reveals Epstein-Barr virus protein kinase integration of DNA damage response and mitotic signaling. PLoS Pathog 11: e1005346 doi: 10.1371/journal.ppat.1005346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lv D-W, Zhong J, Zhang K, Pandey A, Li R (2017) Understanding Epstein-Barr Virus Life Cycle with Proteomics: A Temporal Analysis of Ubiquitination During Virus Reactivation. OMICS: A Journal of Integrative Biology 21: 27–37. doi: 10.1089/omi.2016.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sarisky RT, Gao Z, Lieberman PM, Fixman ED, Hayward GS, et al. (1996) A replication function associated with the activation domain of the Epstein-Barr virus Zta transactivator. Journal of virology 70: 8340–8347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sanjana NE, Shalem O, Zhang F (2014) Improved vectors and genome-wide libraries for CRISPR screening. Nature methods 11: 783–784. doi: 10.1038/nmeth.3047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Carreira VS, Fan Y, Kurita H, Wang Q, Ko CI, et al. (2015) Disruption of Ah Receptor Signaling during Mouse Development Leads to Abnormal Cardiac Structure and Function in the Adult. PLoS One 10: e0142440 doi: 10.1371/journal.pone.0142440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Love MI, Huber W, Anders S (2014) Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15: 550 doi: 10.1186/s13059-014-0550-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wang J-T, Yang P-W, Lee C-P, Han C-H, Tsai C-H, et al. (2005) Detection of Epstein–Barr virus BGLF4 protein kinase in virus replication compartments and virus particles. Journal of general virology 86: 3215–3225. doi: 10.1099/vir.0.81313-0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. The transcription level of all the genes identified in IRF8-sg2 and NC cell lines. B. Differentially expressed genes between IRF8-sg2 and NC cell lines.
(XLSX)
(XLSX)
The sequencing of IRF8-depleted cell lines showing that 10 out of 22 clones for sg1 and 9 out of 14 clones for sg2 contain frame shifts. The PAM sequences were highlighted by red and the guide RNA sequences were shown in bold. WT: wild-type; “+” or “-” followed by numbers indicates the number of base pair inserted or deleted; “S” followed by numbers indicates the number of site mutations; “×” followed by numbers indicates the number of clones obtained in the sequencing.
(TIF)
A. Akata (EBV+) IRF8-sg2 cells were used to establish IRF8-expressing stable cell lines using a pLX-IRF8 lentiviral construct. Western blot analyses showing IRF8, ZTA, RTA and BGLF4 expression level in different cell lines upon IgG cross-linking as indicated. B. Intracellular viral DNA from cells treated as in (A) was measured by qPCR using primers to EBV BALF5. The value of vector control at 0 hr (lane 4) was set as 1. Data are presented as means ± standard deviations of triplicate assays. ** p<0.01.
(TIF)
A. RT-qPCR validation of the 8 apoptosis-related genes in IRF8-sg1 cells. B and C. IRF8 depletion (sg1) suppresses caspase-1 expression and the generation of cleaved caspase substrates upon lytic induction by anti-IgG cross-linking. Western blot analysis of protein extracts from Fig 1C using antibodies against caspase-1, PARP, and cleaved caspase substrates as indicated in panel (B). Western blot analysis of protein extracts from Fig 1C using antibodies against caspase-3, cleaved caspase-3, caspase-8, cleaved caspase-8, caspase-7, cleaved caspase-7, caspase-9, cleaved caspass-9, caspase-2, Bcl2, KAP1, PAX5, DNMT3A and STAT3 as indicated in panel (C).
(TIF)
RPKM, Reads Per Kilobase of transcript per Million mapped reads.
(TIF)
A. ChIP-PCR analysis using three EBV-positive cells [Akata (EBV+), P3HR-1 and LCLs] showing IRF8/IRF1 binding to CASP1 promoter. ChIP by a nonspecific IgG was include as negative controls. B. The pGL2-CASP1p-1-Luc constructs were co-transfected into Akata (EBV+) cells with either 10 ug of IRF8, IRF1 or IRF8-K108E expression vectors. Luciferase assays were performed 36 hrs post-transfection. The value of cells transfected with an empty vector was set as 1. The results were presented as mean ± standard deviation of triplicate assays. ** p<0.01, *** p<0.001.
(TIF)
RPKM, Reads Per Kilobase of transcript per Million mapped reads.
(TIF)
The sequencing of CASP1-depleted cell lines showing that 8 out of 13 clones for CASP1-sg1 and 12 out of 14 clones for CASP1-sg2 contain frame shifts. The PAM sequences were highlighted by red and the guide RNA sequences were shown in bold. WT: wild-type; “+” or “-” followed by numbers indicates the number of base pair inserted or deleted; “S” followed by numbers indicates the number of site mutations; “×” followed by numbers indicates the number of clones obtained in the sequencing.
(TIF)
qPCR analysis showing that CASP8 mRNA level was slightly increased by CASP1 depletion. The value was normalized by qPCR using specific primers to β-actin. Data are presented as means ± standard deviations of triplicate assays.
(TIF)
Data Availability Statement
RNA-seq raw data have been submitted to National Center for Biotechnology Information (NCBI) Sequence Read Archive (SRA; accession numbers: SRP107862) with access URL https://www.ncbi.nlm.nih.gov/Traces/study/?acc=SRP107862.