Abstract
The use, timing, and priority of angioembolization in the management of bleeding pelvic fractures remain ambiguous. The most common vessels for angioembolization are, in decreasing order, the internal iliac artery and its branches, the superior gluteal artery, the obturator artery, and the internal pudendal artery. Technical success rates for this treatment option range from 74% to 100%. The fracture patterns most commonly requiring angioembolization are the Young and Burgess lateral compression and anterior-posterior compression types and Tile type C. Mortality rates after angioembolization of 16% to 50% have been reported, but deaths are usually related to concomitant injuries. The sensitivity and specificity of contrast-enhanced CT in detecting the need for angioembolization range from 60% to 90% and 92% to 100%, respectively. Angioembolization can be effective in the management of bleeding pelvic fractures, but as with any treatment, the risks of complications must be considered. Availability of angioembolization and institutional expertise/preference for the alternative strategy of pelvic packing influence its use.
Keywords: external fixation, mortality, pelvic angiography, pelvic binder, pelvic embolization, pelvic fracture, pelvic hemorrhage
Pelvic fractures in trauma patients can be associated with substantial hemorrhage, leading to mortality rates as high as 50%.1 Several methods, such as external fixation, pelvic packing, placement of pelvic binders, and circumferential sheet wrapping, can be used to stabilize bleeding from pelvic fractures.2-4 Although approximately 85% of bleeding associated with pelvic fractures is from veins or bones,1,5 arterial injury also poses an immediate threat.6 Ligation of the internal iliac artery during laparotomy was previously used to control pelvic arterial hemorrhage. However, this method has proven ineffective because of the rich collateral blood supply to the pelvis.7 Because of the need for an effective means of controlling arterial hemorrhage and in response to technologic advancement, the use of angioembolization has increased.
Despite the publication of research on angioembolization for the management of pelvic hemorrhage as early as 1972,8 ambiguity persists regarding its use.7 We reviewed the available literature on angioembolization for the management of hemorrhage associated with pelvic fracture to assess indications for the procedure, including relationship to fracture type and CT findings; utilization, success, and mortality rates; the most commonly embolized vessels; effects of the time from injury to embolization; and complications. We found 26 studies, published from 1989 to 2013, concerning pelvic fracture and angiography.2,5-7,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30 Of these, 24 studies reported on 15,633 patients with pelvic trauma admitted to treating hospitals. Appendix 1 (Supplemental Digital Content 1, Utilization, Success Rates, and Mortality Rates of Angiography and Embolization in Pelvic Fracture Patients, http://links.lww.com/JAAOS/A75) provides data from these studies. Because the studies had different research aims, not all of the desired data elements were clearly stated in each article. Therefore, we organized the data with the aim of obtaining accurate representations of overall patient populations and ratios.
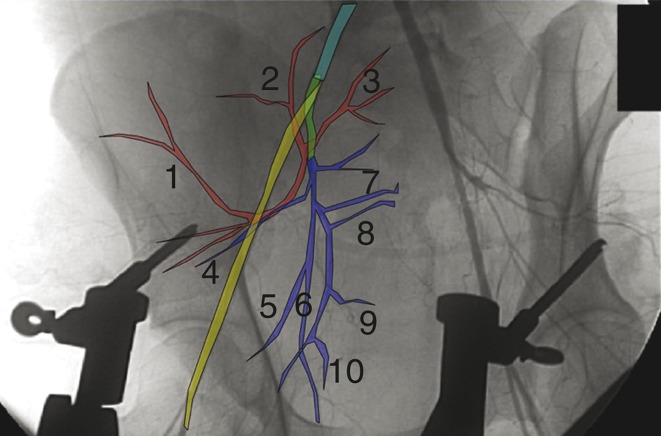
Anatomy of the Pelvic Arterial System
The common iliac arteries begin at the terminus of the aorta. The external iliac artery forms when the common iliac artery bifurcates and continues as the femoral artery at the inguinal ligament. The other branch is the internal iliac artery, which supplies the walls and viscera of the pelvis, the buttocks, the reproductive organs, and the medial compartment of the thigh. It is a short, thick vessel, smaller than the external iliac artery, and is approximately 3 to 4 cm in length. As it passes downward to the upper margin of the greater sciatic foramen, it divides into two large trunks, the anterior and posterior divisions. The posterior division gives rise to the superior gluteal, iliolumbar, and lateral sacral arteries. The anterior division gives rise to the obturator, inferior gluteal, umbilical, uterine (in women), vaginal (in women), inferior vesical, medial rectal, and internal pudendal arteries. These branches have some variability (Figure 1).
Figure 1.
Diagram depicting the pelvic arterial system, overlaid on a pelvic angiogram. The common iliac artery is shown in aqua; the external iliac artery, in yellow; the internal iliac artery, in green; the posterior branch of the internal iliac artery, in red; and the anterior branch of the internal iliac artery, in blue. Smaller vessels include the superior gluteal artery (1), iliolumbar artery (2), lateral sacral artery (3), inferior gluteal artery (4), umbilical artery (5), obturator artery (6), internal pudendal artery (7), medial rectal artery (8), uterine artery or ductus deferens (9), and superior vesical artery (10).
Indication for Angiography and Embolization
The use of angiography depends on several factors, including the patient’s clinical scenario, vital signs, and continued need for resuscitation; angiographer availability; and physician experience.31 Although many institutions have similar algorithms and guidelines for the use of angiography, no standard protocol has been established.
The basic indication for angiography is the suspicion of an injured pelvic artery that is actively bleeding. However, complex clinical situations can lead to a dilemma in assessing whether a patient has pelvic arterial bleeding. For example, hemodynamic instability has been shown to be present in up to 25% of patients admitted with anterior-posterior compression (APC) type I and II pelvic fractures, making the source of blood loss less clear.2 Screening of a patient with pelvic trauma on arrival to the emergency department involves assessing vital signs to determine whether the patient is experiencing hemorrhagic shock without obvious bleeding from other sources. These patients have often sustained high-impact trauma and can have associated injuries that could be a source of bleeding.9 In multiple studies, the indication for angiography was not specifically mentioned or was stated simply as clinical suspicion of bleeding.3-5,10,11,31-33 As in the treatment of any patient showing signs of shock, immediate actions are to secure the airway and start resuscitation. A patient’s failure to respond to the use of resuscitative fluids is an indication for investigation of possible hemorrhage.7,12,34 Miller et al13 found that an inadequate response to initial resuscitation is 100% sensitive and 30% specific in predicting the presence of arterial bleeding on angiography.
Some surgeons use hemodynamic instability on presentation (defined as systolic arterial pressure <90 mm Hg after an infusion of 2 L of lactated Ringer solution and the initiation of transfusion of packed red blood cells) as an indication to immediately perform angiography with embolization.14 Other surgeons attempt to stabilize the pelvic fracture with an external fixator, sheets, or a pelvic binder to reduce pelvic volume and stabilize clot formation.15,31 A study of pressure-volume relationships in cadavers by Grimm et al35 showed that pressures of only 10 mm Hg are required for tamponade of venous bleeding in the pelvis. They showed that sufficient retroperitoneal pressures would be reached without the use of external fixation. Even with external fixation, the pelvis is not a closed space, especially when it has been violated by trauma, allowing the bleeding to extend beyond its normal boundaries within the pelvis.16 Miller et al13 recommended sending patients directly to angiography, stating that external fixation would have delayed effective control of arterial hemorrhage in 7 of 16 patients (44%) in their study. However, this opinion is not universally accepted.
Patients who are nonresponsive to resuscitation are usually investigated with Focused Assessment with Sonography for Trauma (FAST),13,17,18 diagnostic peritoneal lavage (DPL), or CT and are treated with a binder, laparotomy, external fixation, or pelvic packing before the decision to perform angiography is made. A positive FAST or DPL examination should be followed by laparotomy when indicated for further investigation of abdominal injury and hemorrhage. When laparotomy is indicated, several authors prefer to stabilize the pelvis with an external fixator or a C-clamp and then proceed to pelvic packing.24,36-38 This strategy has been shown to reduce the need for angiography, reduce the need for blood transfusion, and possibly decrease mortality.24,36-38
Negative FAST and DPL examinations draw suspicion to the pelvis as the source of bleeding. The current controversy regarding treatment in patients with pelvic hemorrhage and negative DPL or FAST results is whether to stabilize the pelvis with a binder or sheet and proceed to angiography6,10,17,20 or to stabilize the pelvis surgically with external fixation or a C-clamp and use pelvic packing.36,37 Pelvic stabilization using binders or sheets is quick and effective, and it reduces the time to angiography. Depending on institutional preferences and resources, the order of angiography versus pelvic fixation or stabilization and pelvic packing after negative FAST or DPL results may vary.20 Pelvic packing can reduce the need for angiography and embolization, and it may improve survival.19 Compared with angiography, pelvic packing is a relatively invasive procedure that requires specific expertise, may not be completely effective in controlling bleeding from large-bore arteries, and requires an additional surgical procedure for removal of the packs 24 to 48 hours after the initial procedure.
A well-accepted indication for embolization after angiography is the presence of active arterial bleeding, seen as a contrast blush on angiography.5 Hak et al33 recommend embolization if visual evidence of arterial injury is observed to avoid the risk of delayed hemorrhage, which can result in pseudoaneurysm, arteriovenous fistula, pelvic hematoma, and vessel truncation.18,20
Pelvic Fracture Type as an Indication for Angiography
The Pennal as well as the Young and Burgess classifications of pelvic fractures are based on the mechanism of injury.34 The main fracture types are APC, lateral compression (LC), vertical shear (VS), and combined mechanism (CM). The LC and APC types are subdivided into three grades of increasing severity. Pattern types APC II and III, LC III, VS, and CM, which are indicative of major ligamentous disruption, are associated with higher transfusion requirements, the presence of pelvic arterial injury, and the incidence of pelvic hemorrhage.6,9-11,20,21,33-35 El-Haj et al5 found that patients with fracture types APC II and III, followed by LC II and III, were most likely to have major arterial bleeding requiring embolization, but they found no statistically significant difference between pelvic fracture types in terms of bleeding observed on angiography. Other studies also did not demonstrate a notable correlation between this classification and arterial bleeding.2,5,9,14,17,20 Conversely, Costantini et al2 showed that APC injuries were least likely to have a positive angiogram, compared with other fracture types.
The Tile classification for pelvic fractures includes type A (stable), type B (rotationally unstable, vertically stable), and type C (rotationally and vertically unstable). Hauschild et al9 showed no statistically significant correlation between embolization and Tile classification. Although Takahira et al23 found that 60% of their patients with embolization had Tile type C fractures, this study focused only on embolization resulting in gluteal necrosis, for which the authors had a small sample size (five patients). Barentsz et al21 showed that 14 of 19 of their patients (74%) with type C fractures required embolization, and all 3 of the patients who died in their study had Tile type C fractures. Other authors concluded that severe pelvic bleeding with damage to the trunk of the internal iliac artery is more likely in patients with high-energy type C fractures than in patients with other fracture types.18
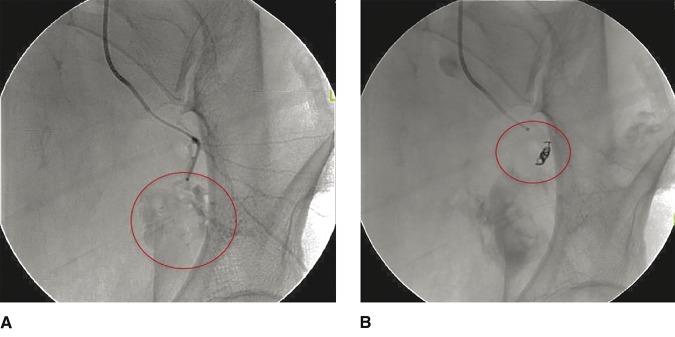
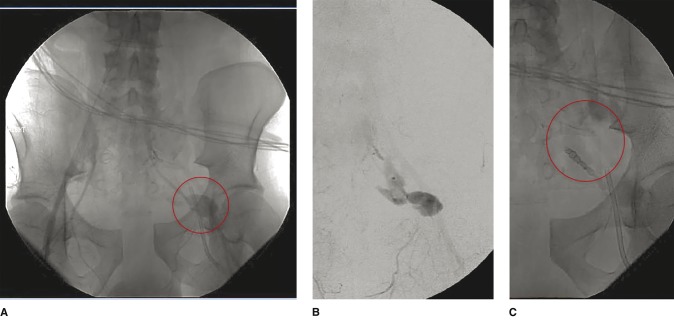
Fractures through the sciatic notch are thought to be associated with a high rate of arterial injury because of the proximity of the superior gluteal artery (SGA)13,25 (Figure 2). Diastasis of the pubic symphysis may also indicate an increased likelihood of arterial damage.10 However, multiple studies of patients with unspecified fracture types have shown discrepancies in findings of association between pelvic fracture and hemorrhage.2,9,17,39 Exsanguinating hemorrhage can occur in patients with seemingly low-risk patterns, such as APC type I. Hemorrhage from the SGA has been described in the absence of pelvic fracture.13 Hence, obtaining an arteriogram on the basis of pelvic fracture alone would result in a low yield of vessels requiring embolization.14,16
Figure 2.
A, Angiogram showing posterior branch/superior gluteal artery extravasation (circled) in a 47-year-old woman who sustained a Young and Burgess lateral compression type III pelvic injury in a motor vehicle accident. B, Angiogram showing successful embolization (circled).
In the compiled data from 16 studies, 478 fractures in patients who underwent angiography were classified by fracture type according to the Young and Burgess classification2,5,6,9,10,13,14,16,17,20,21,23,24,25,26,27 (Appendix 2, Supplemental Digital Content 2, Pelvic Fracture Types Associated With Angiography or Angioembolization, http://links.lww.com/JAAOS/A76). Of these, the most common fracture type was LC, with 228 fractures (47.7%), followed by APC (159 fractures [33.3%]), CM (59 fractures [12.3%]), and VS (32 fractures [6.7%]). Among the 86 fractures classified according to the Tile classification, type C was the most common, with 64 fractures (74.4%), followed by type B (15 fractures [17.4%]) and type A (7 fractures [8.1%]). Among the 76 patients who underwent embolization and were classified using the Young and Burgess classification, type LC was the most common fracture pattern, with 42 fractures (55.3%), followed by APC (22 fractures [28.9%]), VS (7 fractures [9.2%]), and CM (5 fractures [6.6%]). Among the 81 fractures classified according to the Tile classification, type C was the most common pattern (61 fractures [75.3%]), followed by type B (14 fractures [17.3%]) and type A (6 fractures [7.4%]). Select studies classifying patients who underwent pelvic angiography or angioembolization by fracture type are shown in Appendix 2 (Supplemental Digital Content 2, Pelvic Fracture Types Associated With Angiography or Angioembolization, http://links.lww.com/JAAOS/A76). Although basing the decision to perform angiography on pelvic fracture type alone is not recommended, these data show that the Young and Burgess LC and APC and the Tile type C fracture types most often required angioembolization, compared with other fracture types.
Use of CT to Predict the Need for Angiography
Contrast-enhanced CT can be useful in predicting the need for angiography.31 The indication to proceed to angiography can be either extravasation of contrast from vessels or the presence of pelvic hematoma in a patient who is hemodynamically unstable and has a pelvic injury. The sensitivity and specificity of CT in predicting the need for angioembolization range from 60% to 90% and from 92% to 100%, respectively.13,14,21,26,35 However, in a study by Costantini et al,2 only 4 of 17 patients with positive angiography findings had positive findings on contrast-enhanced CT, yielding a sensitivity of 23.5%. A positive finding of contrast extravasation on CT has been shown to have enormous value in management, whereas a negative test likelihood ratio is considered intermediate in magnitude.25 Using the patient’s hemodynamic status and response to resuscitation in addition to the results of contrast-enhanced CT is helpful in predicting the need for angiography.13 Patients with a positive blush on CT in the clinical context of hemodynamic instability and a pelvic injury are likely to require embolization. However, care must be taken to avoid delaying angiography when the suspicion of hemorrhage is high. Thus, the utilization of CT, as with many techniques in trauma management, depends on its availability.13
Angiography and Embolization Utilization, Success, and Mortality Rates
In 24 studies that we reviewed, accounting for a total of 15,633 patients with pelvic fractures, the need for angiography ranged from 0.34% to 48.6%.2,5-7,9,10,11,12,13,14,15,16,17,18,20,21,22,23,24,25,26,27,28,29 In these studies, 13.1% to 100% of the patients who had an angiogram proceeded to embolization. Despite the wide range of angioembolization rates in these studies, a common finding is a high success rate of embolization, ranging from 74% to 100%. However, the studies did not all use the same definition of success. In one study, technical success was defined as a procedure that went as planned and in which a flow of contrast was no longer visualized distal to the embolized segment.21 The 74% success rate referred to the authors’ definition of treatment success, meaning that the patient was no longer hemodynamically unstable after the procedure, despite 100% technical success. In that study, treatment failed in five patients: two required additional surgeries for other injuries, two died from hypovolemic shock, and one died from cerebral herniation.21 The treatment success rate, although still high, was lower than the 93% treatment success rate reported by Velmahos et al.22
The need for repeat angiography is described in three studies, with rates ranging from 2.2% to 34%.10,16,22 The need for repeat embolization ranged from 11.3% to 40.0%.10,16,22 Gourlay et al10 reported that the source of bleeding on repeat angiogram occurred at a new bleeding site in 68% of patients, at a previously embolized site in 18%, and at both new and previously embolized sites in 14%. Hamill et al16 reported that the source of bleeding on repeat angiogram was from a new site in all patients. One explanation is distal dislodgement of gelatin sponge material, leaving the bleeding site unoccluded. However, one study showed no significant association between the type of material used and the need for repeat embolization.40 Dislodgement of material would not explain bleeding at a new site, as reported in most cases. Bleeding from a new site may be attributable to insufficient resuscitation or a transient vasospasm during the initial angiogram.40 Patients with repeat positive angiographies were more likely to have multiple injuries with more severe hemorrhage, compared with those who did not have repeated positive angiographies.40 Gourlay et al10 identified hypotension, pubic symphysis disruption, a transfusion rate >2 U of blood per hour, and the presence of more than two pelvic arterial injuries on initial angiogram as statistically significant predictors of recurrent arterial hemorrhage. They recommended that the arterial sheath be left in these patients for 48 to 72 hours. Close surveillance of these patients is necessary, and the threshold for repeat angiography should be low.31
In patients who underwent embolization, mortality rates were as high as 88.9%.7 However, determining the presence of a statistically significant correlation between embolization and mortality is difficult because of the high rate of additional life-threatening injuries.18 Takahira et al23 reported a mortality rate of 60%, but their study included only patients who had gluteal muscle necrosis, all of whom had substantial high-energy trauma with multiple injuries. Evers et al7 reported a mortality rate of 88.9%, relating it to a long mean time to embolization (>4 hours), which can lead to a prolonged low flow state, multisystem organ failure, and sepsis.
The highest mortality rates are also from the earliest reports, suggesting improvement in outcomes with more modern resources, technology, and awareness of the indications for angioembolization. Despite the reports showing high mortality rates, success rates remain high, showing that angioembolization is an effective strategy for controlling hemorrhage, although these patients often have other complex injuries that affect morbidity and mortality.
Selection of Vessels for Embolization
The most commonly reported vessels for embolization, in decreasing order, are the internal iliac artery, at 67.2%; unnamed branches of the internal iliac artery, at 17.0%; the SGA, at 4.4%; the obturator artery, at 4.1%; and the internal pudendal artery, at 3.2%. Additional embolized vessels included the lateral sacral artery, iliolumbar artery, branches of the external iliac artery, the inferior gluteal artery, the gluteal branch of the internal iliac artery, the inferior rectal artery, and the external iliac artery (Figures 2 through 5). Of the vessels listed in Appendix 3 (Supplemental Digital Content 3, Vessels Embolized in Patients Undergoing Pelvic Angioembolization, http://links.lww.com/JAAOS/A77), bilateral embolization occurred in 58 patients with the internal iliac artery (Figure 3), in 3 patients with unnamed branches of the internal iliac artery, and in 2 patients with the internal pudendal artery (Supplemental Digital Content 3, Vessels Embolized in Patients Undergoing Pelvic Angioembolization).
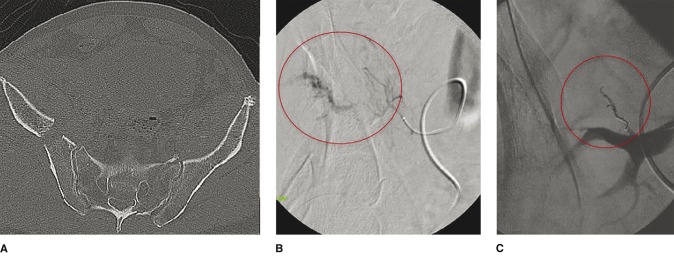
Figure 5.
Axial pelvic CT (A) and aortopelvic angiogram (B) showing bleeding off the posterior division of the right internal iliac artery in an 81-year-old man who sustained a hemodynamically unstable Young and Burgess lateral compression type III pelvic injury in a fall from a roof. The patient was treated initially with a pelvic binder. C, Angiogram showing successful coil embolization (circled).
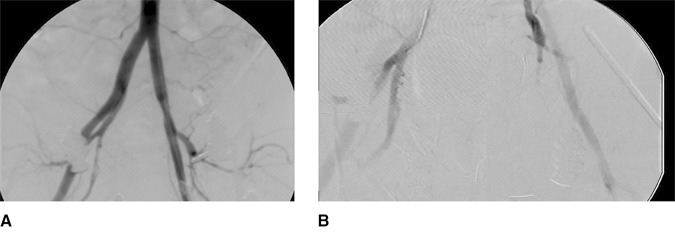
Figure 3.
A, Pelvic angiogram showing extravasation resulting from a Young and Burgess anterior-posterior compression type III pelvic injury in a 41-year-old man who was crushed by a forklift. B, The patient underwent laparotomy, external fixation with a femoral distractor, pelvic packing, and angiography with gel foam embolization of both internal iliac artery arteries.
Figure 4.
A and B, Angiograms showing extravasation (circled in panel A) from the anterior division of the internal iliac artery in a 41-year-old patient who sustained a Young and Burgess anterior-posterior compression type III pelvic injury as a result of a motor vehicle accident. The patient was treated initially with a binder. C, Angiogram showing successful embolization with a coil (circled).
Although their article did not specifically mention which vessels were embolized and thus is not included in Table 1, Matityahu et al24 reported that 79 of the 98 patients in their study required bilateral embolization. In that study, 53 embolizations were selective (ie, a specific branch was embolized), and 42 embolizations were nonselective (ie, a proximal branch was embolized; Figure 3). Velmahos et al22 reported that 32% of their patients required bilateral internal iliac artery embolization.
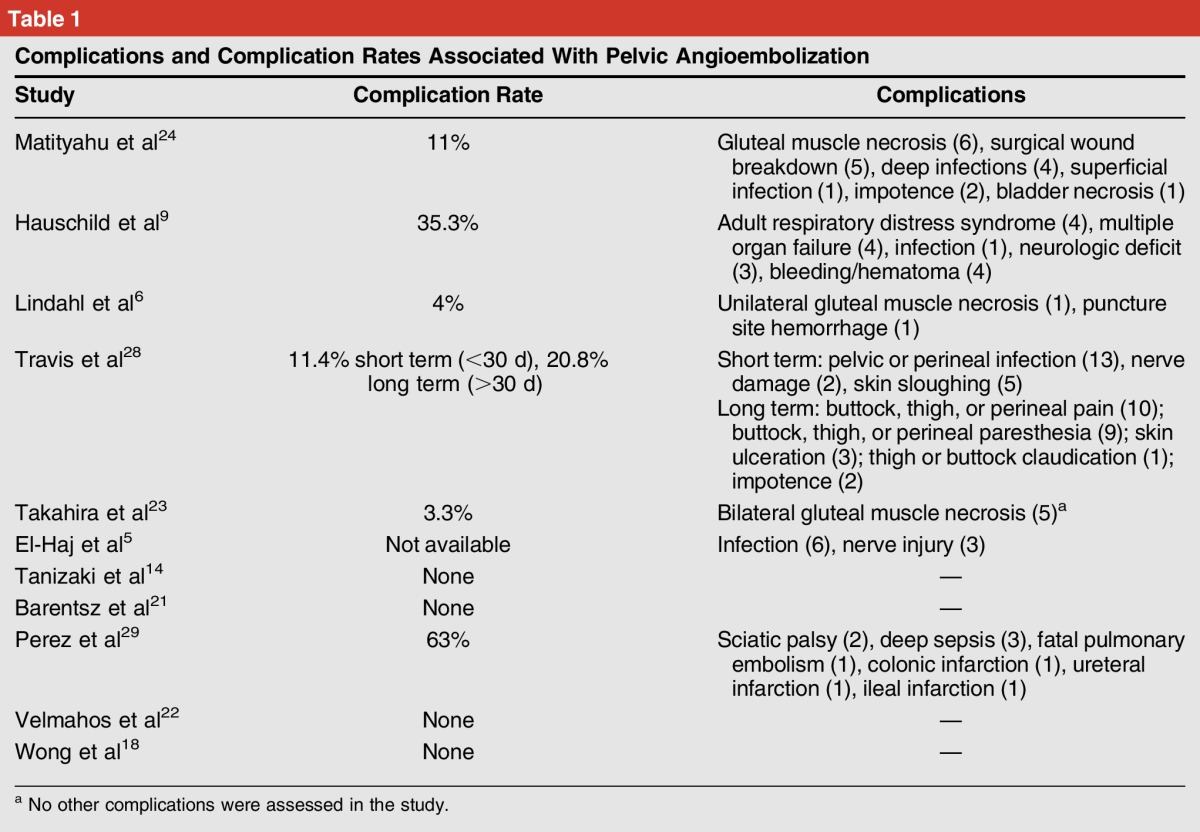
Table 1.
Complications and Complication Rates Associated With Pelvic Angioembolization
The indication for nonselective (proximal) embolization is usually an angiogram showing multiple bleeding arteries, or a high suspicion of multiple-vessel injury in a patient with substantial hemodynamic instability.1,22 Selective embolization is preferred because it can decrease the incidence of potential complications, such as gluteal muscle ischemia, especially if surgical intervention is planned.33
Time to Embolization
A consistent finding regarding angioembolization for the management of pelvic hemorrhage is the importance of the time to angiography and embolization. Early angiography with embolization, when needed, has been shown to improve patient outcomes. Agolini et al27 demonstrated that survival substantially improves when embolization is performed within 3 hours of arrival. In another study, mortality in embolized patients was 36.4% for those who arrived for angiography within 3 hours and 75% for patients arriving after 3 hours.27 Hak et al33 noted that angiography within 90 minutes of admission improved survival rates. Using even stricter time constraints, Tanizaki et al14 found that mortality in patients arriving for angiography within 60 minutes was 16%, with the rate increasing to 64% when angiography was delayed. In the study with the highest mortality rate after embolization (8 of 9 patients), Evers et al7 reported that the mean time from admission to angiography was >4 hours. Thus, time to angiography is an important factor to consider when treating a patient with suspected pelvic hemorrhage.2
Complications
Pelvic angioembolization has potential complications that are important to consider because they can affect the patient’s outcome. Complication rates were specifically stated in 11 articles that we reviewed; these rates ranged from zero to 63%5,6,9,14,18,21,22,23,24,28,29 (Table 1). The complications reported include surgical wound breakdown/deep infection (mentioned in five articles), gluteal muscle necrosis (four articles), nerve injury (four articles), bladder or ureteral infarction (two articles), bleeding or hemorrhage (two articles), bowel infarction (one article), thigh or buttock claudication (one article), and impotence (one article). This wide range of complications creates a confusing picture of what should be expected after the procedure.
Nonselective embolization of the internal iliac artery, especially bilateral embolization, has been suggested to have higher complication rates.5,14,22,24,28,29,32 Travis et al28 reported a statistically significant association between bilateral internal iliac artery embolization and buttock, thigh, or perineal paresthesia. However, they found no statistically significant associations with any other complications. In another study, every patient with a reported complication had undergone bilateral embolization.24 Several other studies reported no complications overall or no complications associated with bilateral nonselective embolization.14,21,22 Tanizaki et al14 attributed the absence of complications in their study to the use of a larger-than-average gelatin sponge for embolization, suggesting that smaller distal blood vessels should be left open to collateral blood flow to avoid substantial tissue ischemia. A similar theory was proposed but not proven by Takahira et al.23 They used steel coils and, in one patient, a large gelatin sponge to ensure proximal embolization in the vessel; however, five patients still experienced gluteal muscle necrosis. The authors theorized that this complication may have been the result of the initial trauma rather than a result of the embolization.
The etiology of complications after angioembolization is a mixed scenario involving the direct effects of embolization and the results of the often substantial initial trauma. Regardless of the cause, the physician must be vigilant in the detection of complications because they affect outcomes and can complicate surgical management. The high success rates and potentially lifesaving effect of emergent internal iliac artery embolization outweigh the marginal and uncertain risks of complications of the procedure.28
Summary
Pelvic angioembolization is an effective treatment for bleeding pelvic injuries. The importance of minimizing the time to embolization in patients with a true arterial hemorrhage cannot be overstated, and the patient must undergo angiography quickly when appropriate. The use of DPL, FAST examinations, and CT can help physicians locate the site of bleeding. Retroperitoneal pelvic packing with external fixation is used before angiography in many centers. This technique has shown promising results in terms of reducing mortality rates and the use of angiography. Although complications after retroperitoneal pelvic packing are difficult to predict, the clinician must be mindful of the potential complications that can affect patient morbidity and mortality and can further complicate treatment.
Footnotes
Dr. Vaidya or an immediate family member has received royalties from and is a member of a speakers’ bureau or has made paid presentations on behalf of DePuy Synthes and Smith & Nephew; serves as a paid consultant to Smith & Nephew; and has received research or institutional support from and nonincome support (such as equipment or services), commercially derived honoraria, or other non–research-related funding (such as paid travel) from DePuy Synthes. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Waldron, Dr. Scott, and Dr. Nasr.
References
References printed in bold type are those published within the past 5 years.
- 1.Durkin A, Sagi HC, Durham R, Flint L: Contemporary management of pelvic fractures. Am J Surg 2006;192(2):211-223. [DOI] [PubMed] [Google Scholar]
- 2.Costantini TW, Bosarge PL, Fortlage D, Bansal V, Coimbra R: Arterial embolization for pelvic fractures after blunt trauma: Are we all talk? Am J Surg 2010;200(6):752-758. [DOI] [PubMed] [Google Scholar]
- 3.Jeroukhimov I, Ashkenazi I, Kessel B, et al. : Selection of patients with severe pelvic fracture for early angiography remains controversial. Scand J Trauma Resusc Emerg Med 2009;17:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magnussen RA, Tressler MA, Obremskey WT, Kregor PJ: Predicting blood loss in isolated pelvic and acetabular high-energy trauma. J Orthop Trauma 2007;21(9):603-607. [DOI] [PubMed] [Google Scholar]
- 5.El-Haj M, Bloom A, Mosheiff R, Liebergall M, Weil YA: Outcome of angiographic embolisation for unstable pelvic ring injuries: Factors predicting success. Injury 2013;44(12):1750-1755. [DOI] [PubMed] [Google Scholar]
- 6.Lindahl J, Handolin L, Söderlund T, Porras M, Hirvensalo E: Angiographic embolization in the treatment of arterial pelvic hemorrhage: Evaluation of prognostic mortality-related factors. Eur J Trauma Emerg Surg 2013;39(1):57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evers BM, Cryer HM, Miller FB: Pelvic fracture hemorrhage: Priorities in management. Arch Surg 1989;124(4):422-424. [DOI] [PubMed] [Google Scholar]
- 8.Margolies MN, Ring EJ, Waltman AC, Kerr WS, Jr, Baum S: Arteriography in the management of hemorrhage from pelvic fractures. N Engl J Med 1972;287(7):317-321. [DOI] [PubMed] [Google Scholar]
- 9.Hauschild O, Aghayev E, von Heyden J, et al. : Angioembolization for pelvic hemorrhage control: Results from the German pelvic injury register. J Trauma Acute Care Surg 2012;73(3):679-684. [DOI] [PubMed] [Google Scholar]
- 10.Gourlay D, Hoffer E, Routt M, Bulger E: Pelvic angiography for recurrent traumatic pelvic arterial hemorrhage. J Trauma 2005;59(5):1168-1174. [DOI] [PubMed] [Google Scholar]
- 11.Gurevitz S, Bender B, Tytiun Y, Velkes S, Salai M, Stein M: The role of pelvic fractures in the course of treatment and outcome of trauma patients. Isr Med Assoc J 2005;7(10):623-626. [PubMed] [Google Scholar]
- 12.Flint L, Babikian G, Anders M, Rodriguez J, Steinberg S: Definitive control of mortality from severe pelvic fracture. Ann Surg 1990;211(6):703-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller PR, Moore PS, Mansell E, Meredith JW, Chang MC: External fixation or arteriogram in bleeding pelvic fracture: Initial therapy guided by markers of arterial hemorrhage. J Trauma 2003;54(3):437-443. [DOI] [PubMed] [Google Scholar]
- 14.Tanizaki S, Maeda S, Matano H, Sera M, Nagai H, Ishida H: Time to pelvic embolization for hemodynamically unstable pelvic fractures may affect the survival for delays up to 60 min. Injury 2014;45(4):738-741. [DOI] [PubMed] [Google Scholar]
- 15.Poole GV, Ward EF, Muakkassa FF, Hsu HS, Griswold JA, Rhodes RS: Pelvic fracture from major blunt trauma: Outcome is determined by associated injuries. Ann Surg 1991;213(6):532-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamill J, Holden A, Paice R, Civil I: Pelvic fracture pattern predicts pelvic arterial haemorrhage. Aust N Z J Surg 2000;70(5):338-343. [DOI] [PubMed] [Google Scholar]
- 17.Cook RE, Keating JF, Gillespie I: The role of angiography in the management of haemorrhage from major fractures of the pelvis. J Bone Joint Surg Br 2002;84(2):178-182. [DOI] [PubMed] [Google Scholar]
- 18.Wong YC, Wang LJ, Ng CJ, Tseng IC, See LC: Mortality after successful transcatheter arterial embolization in patients with unstable pelvic fractures: Rate of blood transfusion as a predictive factor. J Trauma 2000;49(1):71-75. [DOI] [PubMed] [Google Scholar]
- 19.Osborn PM, Smith WR, Moore EE, et al. : Direct retroperitoneal pelvic packing versus pelvic angiography: A comparison of two management protocols for haemodynamically unstable pelvic fractures. Injury 2009;40(1):54-60. [DOI] [PubMed] [Google Scholar]
- 20.Sarin EL, Moore JB, Moore EE, et al. : Pelvic fracture pattern does not always predict the need for urgent embolization. J Trauma 2005;58(5):973-977. [DOI] [PubMed] [Google Scholar]
- 21.Barentsz MW, Vonken EP, van Herwaarden JA, Leenen LP, Mali WP, van den Bosch MA: Clinical outcome of intra-arterial embolization for treatment of patients with pelvic trauma. Radiol Res Pract 2011;2011:935484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velmahos GC, Chahwan S, Falabella A, Hanks SE, Demetriades D: Angiographic embolization for intraperitoneal and retroperitoneal injuries. World J Surg 2000;24(5):539-545. [DOI] [PubMed] [Google Scholar]
- 23.Takahira N, Shindo M, Tanaka K, Nishimaki H, Ohwada T, Itoman M: Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury 2001;32(1):27-32. [DOI] [PubMed] [Google Scholar]
- 24.Matityahu A, Marmor M, Elson JK, et al. : Acute complications of patients with pelvic fractures after pelvic angiographic embolization. Clin Orthop Relat Res 2013;471(9):2906-2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stephen DJ, Kreder HJ, Day AC, et al. : Early detection of arterial bleeding in acute pelvic trauma. J Trauma 1999;47(4):638-642. [DOI] [PubMed] [Google Scholar]
- 26.Pereira SJ, O’Brien DP, Luchette FA, et al. : Dynamic helical computed tomography scan accurately detects hemorrhage in patients with pelvic fracture. Surgery 2000;128(4):678-685. [DOI] [PubMed] [Google Scholar]
- 27.Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, Reed JF, III: Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma 1997;43(3):395-399. [DOI] [PubMed] [Google Scholar]
- 28.Travis T, Monsky WL, London J, et al. : Evaluation of short-term and long-term complications after emergent internal iliac artery embolization in patients with pelvic trauma. J Vasc Interv Radiol 2008;19(6):840-847. [DOI] [PubMed] [Google Scholar]
- 29.Perez JV, Hughes TM, Bowers K: Angiographic embolisation in pelvic fracture. Injury 1998;29(3):187-191. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki T, Smith WR, Moore EE: Pelvic packing or angiography: Competitive or complementary? Injury 2009;40(4):343-353. [DOI] [PubMed] [Google Scholar]
- 31.Langford JR, Burgess AR, Liporace FA, Haidukewych GJ: Pelvic fractures: Part 1. Evaluation, classification, and resuscitation. J Am Acad Orthop Surg 2013;21(8):448-457. [DOI] [PubMed] [Google Scholar]
- 32.Dondelinger RF, Trotteur G, Ghaye B, Szapiro D: Traumatic injuries: Radiological hemostatic intervention at admission. Eur Radiol 2002;12(5):979-993. [DOI] [PubMed] [Google Scholar]
- 33.Hak DJ, Smith WR, Suzuki T: Management of hemorrhage in life-threatening pelvic fracture. J Am Acad Orthop Surg 2009;17(7):447-457. [DOI] [PubMed] [Google Scholar]
- 34.Dalal SA, Burgess AR, Siegel JH, et al. : Pelvic fracture in multiple trauma: Classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma 1989;29(7):981-1002. [PubMed] [Google Scholar]
- 35.Grimm MR, Vrahas MS, Thomas KA: Pressure-volume characteristics of the intact and disrupted pelvic retroperitoneum. J Trauma 1998;44(3):454-459. [DOI] [PubMed] [Google Scholar]
- 36.Ertel W, Eid K, Keel M, Trentz O: Therapeutical strategies and outcome of polytraumatized patients with pelvic injuries: A six-year experience. Eur J Trauma Emerg Surg 2000;26(6):278-286. [Google Scholar]
- 37.Pohlemann T, Bosch U, Gänsslen A, Tscherne H: The Hannover experience in management of pelvic fractures. Clin Orthop Relat Res 1994;305:69-80. [PubMed] [Google Scholar]
- 38.Smith WR, Moore EE, Osborn P, et al. : Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: Report of two representative cases and a description of technique. J Trauma 2005;59(6):1510-1514. [DOI] [PubMed] [Google Scholar]
- 39.Gilliland MG, Ward RE, Flynn TC, Miller PW, Ben-Menachem Y, Duke JH, Jr: Peritoneal lavage and angiography in the management of patients with pelvic fractures. Am J Surg 1982;144(6):744-747. [DOI] [PubMed] [Google Scholar]
- 40.Eastridge BJ, Starr A, Minei JP, O’Keefe GE, Scalea TM: The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. J Trauma 2002;53(3):446-451. [DOI] [PubMed] [Google Scholar]