Abstract
Objectives:
The aim of this systematic review was to evaluate the cost-effectiveness of occupational safety and health interventions from the employer perspective.
Methods:
A comprehensive literature search (2005 to 2016) in five electronic databases was conducted. Pre-2005 studies were identified from the reference lists of previous studies and systematic reviews, which have similar objective to those of this search.
Results:
A total of 19 randomized controlled trials and quasi-experimental studies were included, targeting diverse health problems in a number of settings. Few studies included organizational-level interventions. When viewed in relation to the methodological quality and the sufficiency of economic evidence, five of 11 cost-effective occupational safety and health (OSH) interventions appear to be promising.
Conclusion:
The present systematic review highlights the need for high-quality economic evidence to evaluate the cost-effectiveness of OSH interventions, especially at organizational-level, in all areas of worker health.
Learning Objectives
Discuss the need for research on the cost-effectiveness and cost benefits of occupational safety and health (OSH) interventions, along with the limitations of previous studies.
Summarize the findings of the present review of economic evaluations of OSH interventions from the employer's perspective, including the characteristics of the cost-effective interventions identified.
Discuss the implications for future efforts to analyze the financial benefits of OSH interventions.
There is a growing interest in the economic value of occupational safety and health interventions mainly because of the limited resources allocated for occupational safety and health (OSH) interventions and the knowledge that proven economic gains are attractive to employers. Recent survey data from 500 organizations found that 73% of employers believe health and safety requirements benefit their business as a whole, while 64% reported they save money in the long term. As safety initiatives may be efficient but may not always bring a financial return to an organization, information about the economics of OSH interventions is important and an invaluable input for decision making.1–3 Health economic evaluation seeks to explicitly identify, measure, and value all relevant cost and benefit parameters and aims to inform all decision-makers of the circumstances where indirect costs exceed direct costs and the relative costs and benefits (cost-effectiveness) of the different intervention options available.4
The costs of occupational injuries and illnesses together with the demonstrated cost-effectiveness of OSH interventions constitute an important incentive for employers to adopt these interventions.5 They are especially interested in whether investment in a program is cost-effective (the effects give good value for the money invested) or cost beneficial (the financial benefits are favorable).6 A previously published systematic review evaluating the economics of OSH concluded that most published intervention studies so far focused on interventions’ effectiveness rather than on their cost-effectiveness. It also concluded that further high-quality studies conducting full economic evaluations are needed in order to be able to draw further conclusions about the cost-effectiveness of OSH interventions from an employer's perspective.7
Because of the above-mentioned problems, our knowledge on the cost-effectiveness of OSH interventions remains unsatisfactory. In order to fill the gaps and shortcomings previously identified in the literature, the aim of the present review was to evaluate the cost-effectiveness of primary and secondary OSH interventions from the perspective of the employer. Primary preventive interventions are proactive and aim to prevent the occurrence of illness among healthy individuals, while secondary interventions are ameliorative and aim to reduce prevalence by early detection. Thus, both primary and secondary OSH interventions can contribute to overall disability prevention or control before the disability becomes chronic or severe. Tertiary preventive interventions, as reactive strategies, were not part of our aim.8–10 Furthermore, this review only looked at interventions that attempted to reduce exposure to deleterious aspects of the workplace.11 According to Alli,12OSH is generally defined as the science of the anticipation, evaluation, recognition and control of hazards arising in or from the workplace, achieving a strong preventive safety culture (pp. vii). Worksite Health Promotion interventions that attempted to change the individual behavior related to health problems that did not arise in or from the workplace, promoting healthy behaviors such as weight control, healthy nutrition, smoking cessation, influenza vaccination, were excluded.6,11,13
The systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement14,15 and the Assessment of Multiple Systematic Reviews (AMSTAR) guidelines.16 The protocol was registered with PROSPERO (registration no: CRD42016046897).
METHODS
Inclusion Criteria and Search Strategy
A systematic review of economic evaluations of OSH interventions from the employer perspective was conducted. A search strategy following PICOS was developed. The PICOS process is a method for putting together a search strategy that facilitates a more evidence-based approach to literature searching. PICOS is an acronym that stands for population, intervention, comparison, outcome, and study design. It orients the construction of the literature search and helps to rapidly and accurately locate the best available scientific information and avoid unnecessary searching.17
Two experienced search specialists from the university library developed the search strategy (see Table C) based on PICOS and some relevant published papers known to the project group. The search strategy included working population, primary and secondary OSH interventions, all types of control groups, economic consequences and health outcomes, randomized controlled trials (RCTs), and quasi-experimental study designs. Schelvis, et al18 highly recommend researchers conducting systematic reviews to broaden their inclusion criteria and not neglect evidence from studies which apply alternative research designs, thereby improving the quality of reporting non-RCTs. We therefore decided to include all study designs with a predefined control group.
The search was conducted in five electronic databases: Medline (OVID), EMBASE.com, Web of Science Core Collection, Cochrane Library (Wiley), and PubMed (not Medline) and covered the period 2005 to April 2016. The studies conducted before 2005 have been included in previous studies and systematic reviews with similar aims as the present search with regard to the economic evaluation of workplace interventions (see for instance).2,6–8,19–21 These studies were thus identified from the reference lists and included if they fulfilled our inclusion criteria. Additional databases were also searched. Supplemental searches were conducted in the National Institute for Occupational Safety and Health database (NIOSH), the NHS Economic Evaluation database (NHS EED), and in the Google scholar search engine, using the same search words as in the other databases. The search was carried out in accordance with the process recommended by the Cochrane Collaboration.22
Selection Strategy
The screening of abstracts and titles was conducted by four reviewers (EC, CS, MLK, AG). The abstracts were included if at least one of the following criteria was met: the title/abstract implied or referred to a workplace setting; the title/abstract referred to an OSH intervention study; the title/ abstract referred to a full economic evaluation study. Two reviewers (AG, MRC) then independently determined the eligibility of studies on the basis of a review of the full texts, using a predesigned criteria form (see Table A; Supplementary Material file). Differences between them were resolved through a consensus procedure or, if the disagreements persisted, a third reviewer was consulted (MLK). Studies were selected on the basis of the following criteria: 1) the study was a primary or a secondary OSH intervention; 2) the study included a full economic evaluation; and 3) the economic analysis of the intervention was conducted from an employer/company perspective. Only studies written in English were included. In addition, only studies where the described intervention was undertaken in a Western developed country were included---based on the assumption that the OSH context varies between developed and developing countries.7 Studies that constitute “grey literature,” editorials, letters, reviews, and articles describing either a partial economic evaluation or the design of an economic evaluation or an economic evaluation tool without any reported results were excluded.
Data Extraction and Evidence Synthesis
To guide the data extraction procedure, the key elements of existing guidelines and relevant systematic reviews as well as texts about economic evaluation were identified (see for instance).2,7,19,20,22 A data extraction form was developed, reviewed, and refined by the researchers to better capture the key factors that were essential for evaluation, synthesis, and presentation, thus ensuring the adequacy of the tool. The data extraction form included location, occupation/the industrial sector of the target population, number of participants, company size and type, health category and target problem, type of study design, total study duration, type and description of the intervention, type of economic evaluation and description of economic analysis, main economic evaluation results, costs, economic consequences, other outcomes, and a description of these. One reviewer extracted the data (AG), while a second reviewer (MLK) checked all the extracted data. Any discrepancies were resolved through a consensus procedure. It was not possible to conduct a meta-analysis due to the heterogeneity of study designs, populations, interventions, and outcomes. Because of the diversity of the studies’ components, we chose to stratify them according to health problems.
Quality Assessment
In order to evaluate the methodological quality of the studies included in the review, two quality assessment tools were used. After a thorough search, the Cochrane Collaboration Risk of Bias (CCRBT)22,23 and the Consensus on Health Economic Criteria (CHEC-list)24 were chosen. The Cochrane Collaboration strongly encourages all reviewers to use the CCRBT to establish consistency and avoid discrepancies in the assessment of methodological quality among all review groups. It also encourages reviewers to use the CHEC-list for critical appraisal of the methodological quality of health economic evaluation studies.25
CCRBT is a two-part tool, addressing seven evidence-based domains, namely random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other sources of bias (other bias). The first part of the tool gives sufficiently detailed support for judging the risk of bias, ensuring its transparency. The second part assigns a judgment relating to the risk of bias for each domain. This is achieved by assigning a judgment of “Low risk” of bias (+), “High risk” of bias (-), or “Unclear risk” of bias (?). In line with the Cochrane Collaboration's recommendations, those studies in which all the domains were rated positively were judged as having a low risk of bias, while the studies with one or more unclear domains were judged as having an unclear risk of bias. Furthermore, studies with one or more negatively rated domains were judged as having a high risk of bias.22,25 In our review, the first two domains (random sequence generation and allocation concealment) were marked as not applicable for the quasi-experimental study designs. Although the tool was not developed with nonrandomized studies in mind, the general structure of the tool and the assessments seems useful to follow when creating risk of bias assessments for quasi-experimental studies.22
The CHEC-list consists of 19 yes (1) or no (0) questions, which address internal and external validity aspects of economic evaluation studies (19, or 100%, was the highest score). In accordance with the summary assessment of Uegaki et al,20 the studies that met less than 50% of criteria were seen as having low methodological quality of undertaking and reporting economic evaluations, while the studies that met more than 75% of criteria were seen as having a high methodological quality of undertaking and reporting economic evaluations. The studies that met between 50% and 75% of criteria were considered to have a moderate methodological quality of undertaking and reporting economic evaluations. Five of the internal quality criteria relate to study design; 11 internal criteria relate to the conduct of the economic evaluation, while the last two internal criteria address the issue of incremental analysis of costs and outcomes and sensitivity analysis. Finally, one external criterion relates to the discussion of the generalizability of the obtained results.20,24
Two review authors (AG, EA) independently evaluated the methodological quality of each study using both assessment tools. Discrepancies were resolved by means of a consensus procedure. If the disagreements persisted, the reviewers consulted a third reviewer (MLK). A senior expert (GB) contributed to the assessment procedure whenever it was deemed to be necessary.
RESULTS
Literature Searches
Our primary search in the predefined databases resulted in 4096 hits. A further 899 hits were found in other sources, giving a total of 4995 citations (see Fig. 1). The latter included references from relevant studies and systematic reviews, publications from the NIOSH, the NHS EED, and Google scholar. After duplicates were removed (n = 1415), a total of 3580 citations were screened. Of these, 3342 citations were excluded on the basis of title, keywords, and abstract. The full text of the remaining articles (n = 238) was then assessed, resulting in 19 articles being retained. The reasons for exclusion are presented in Fig. 1.
FIGURE 1.
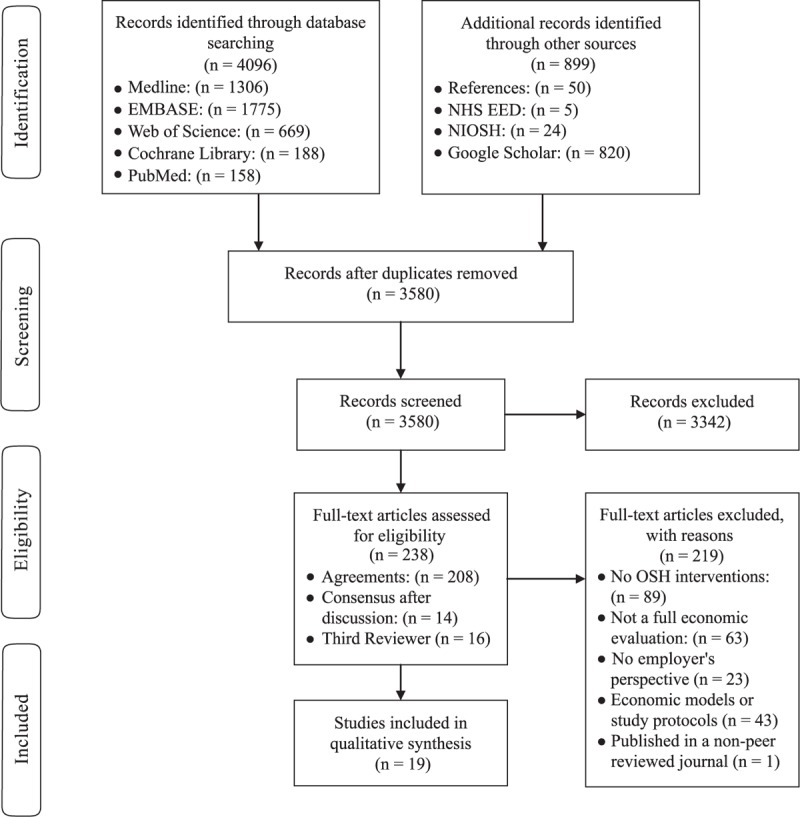
Flow chart.
Description and Characteristics of Included studies
Working populations from the following sectors were represented: health care, retail and trade, construction, manufacturing and warehousing, transportation, communication, business, and professional services. Half of the studies (10 of 19) were undertaken in Europe. Six studies were carried out in the United States and one each in Canada, North America, and Australia. Sample sizes ranged from 50 to 3047 employees (10,026 in total; mean sample size: 528; median sample size: 262). The studies reported on a range of intervention types, such as training, education, naturopathic care, visits to practitioners and therapists, as well as safety equipment (for instance back belts, safety cutters, ceiling lifts, protective devices). The studies addressed either individual-level (n = 14) or organizational-level interventions (n = 4), or both (n = 1). The follow-up period ranged from 6 months to 6 years, with 12 months as the most common duration for most studies (n = 12). In 15 studies, the design was a RCT. Three studies had a controlled before-after design, while one used a case–control design. Eight studies were conducted in the 1990s, while only two studies were conducted during the following decade. The remaining half of the included studies were published between 2010 and the beginning of 2016. The intervention studies included in the review covered a broad range of interventions targeting different types of health outcomes. Some interventions focused on primary prevention, others on secondary prevention, and some on both. The studies were stratified according to the targeted health problems. Three categories were compiled: musculoskeletal disorders (MSDs) (n = 10), mental health (n = 3), and other preventive interventions (n = 6).
Table 1 includes an overall description of the interventions and details of the study designs. The largest group of economic evaluations of OSH interventions was conducted on MSDs, such as low back pain (n = 5), back injuries (n = 3), and neck and upper limb symptoms (n = 2).26–35 The participants were workers with a high prevalence of MSDs from large, diverse industries, such as bus drivers, county government workers, postal workers, computer workers, warehouse workers, and coal miners. Half of the studies were conducted in the 1990s. Eight were individual-level RCT interventions and one was a multilevel intervention.28 Only one study was an organizational-level case–control study intervention.31
TABLE 1.
Data Extraction Presented for Targeted Health Problems: Study Design Characteristics and Intervention Description
| Country; Industrial Sector; Company size | Number of Participants; Target Problem | Type of Study Design; Measurement Time Period | Type and Description of the Intervention | ||
| Musculoskeletal disorders | Aboagye et al26 | Stockholm, Sweden | 159 workers; low back pain | RCT; 12 months | Individual (training therapies and advice); Group A: medical yoga (n = 52), Group B: exercise therapy (n = 52), Group C: self-care advice group (n = 55). |
| Bernaards et al27 * | Netherlands; 6 companies | 466 computer workers; neck and upper limb symptoms | RCT; 12 months | Individual (work style and physical activity); Group A (WS): work style intervention (n = 152; 60 min/meeting), Group B (WSPA): work style and physical activity intervention (n = 156; 90 min/ meeting), Group C: usual care (n = 158; receive breaks and exercise reminder software like the other groups). | |
| Driessen et al28 | Netherlands; 4 large companies (railway transportation company, airline company, university, medical hospital, steel company). | 3,047 workers; low back pain | RCT; 12 months | Individual and Organizational (Stay@Work participatory ergonomics program); Both groups watched 3 short (45 s) educative movies about LBP and NP prevention. Group A: interventional group (brainstormed about, evaluated and prioritized 3 top risk factors for LBP & NP and 3 top ergonomic measures, writing down in an implementation plan), Group B: control group. | |
| Greenwood et al29 | West Virginia, US; Large Underground coal mining | 278 workers; low back disability | RCT; 9 months | Individual (recovery management after health and psychological evaluation); Very early intervention with 2 groups. Group A: Experimental group [n = 117; recovery management after health and psychological evaluation using a risk for extended disability predictive factor scale (at least 8 days after injury)], Group B: Control group (n = 161). | |
| Herman et al30 * | North America; Large warehouse company | 70 workers; low back pain | RCT; 6 months | Individual (naturopathic care); Group A: intervention group (n = 39; naturopathic care visits: acupuncture, exercise and dietary advice, relaxation training, back care educational booklet), Group B: control group (n = 31; standardized physiotherapy advice, back care educational booklet). | |
| Mitchell et al31 | Oklahoma, US; Defense (Air force Base) | 1,316 warehouse workers; back injuries | Case--control; 6 years | Ergonomic intervention with training; Back belt use, back injury prevention training for all new hires, annual instruction period for proper lifting techniques. Group A: workers using a back belt; Group B: control group (workers who chose not to wear belts). | |
| Shi32 * | California, US; 6 Government divisions | 205 workers; back injuries | RCT; 12 months | Individual with ergonomic improvements; Group A: control group (n = 4,398 country employees), Group B: intervention group (n = 205; health risk assessment before and after the injury prevention program that included education, training, physical fitness activities, and ergonomic improvement). | |
| Speklé et al33 | Netherlands; 7 companies | 638 computer workers; neck and upper limb symptoms | RCT; 12 months | Individual (RSI QuickScan intervention); Group A: intervention group (n = 320; a set of 16 individual and group-level interventions, ie, individual workstation check, eyesight check, education program on the prevention of arm, shoulder, and neck symptoms, training on handling stress), Group B: usual care group (n = 318). | |
| Tuchin34 * | Sydney, Australia; Large Postal service | 121 workers; back injuries | RCT; 6 months | Individual (education program); Group A: control group (n = 27; no education, instructed to perform a series of daily exercises), Group B: intervention group (n = 34; spinal care lecture ≈ 120 min included an educational part of spinal anatomy, causes of back pain and injuries, as well as preventive and treatment activities), Group C: nonintervention group (n = 60). | |
| Versloot et al35 * | Netherlands; Transportation (bus company) | 500 workers; low back pain | RCT; 48 months | Individual (back school health education program); Group A: experimental group (n = 200; back school program consisted of 3 training sessions: first session included education and practice related to physical health; second and third sessions included workers’ experiences of the last 6 months, summary of the first session), Group B: control group (n = 300). | |
| Mental health | Geraedts et al36 | Netherlands; 6 large companies (2 banking companies, 2 research institutes, 1 security company, 1 university) | 231 workers; depressive symptoms | RCT; 12 months | Individual (brief Web-based intervention); Group A: intervention group (n = 116; Happy@Work intervention including problem solving treatment cognitive therapy and a guideline to prevent work-related stress; 6 weekly lessons (information about the theme, examples, assignments); participants start with a new lesson after feedback reception on their assignment from a coach), Group B: usual care (n = 115). |
| Noben et al37 * | Netherlands; Health care; Large | 413 workers; mental health complaints | RCT; 6 months | Individual (occupational physician program; Group A: intervention group (n = 207; personalized feedback, referral to the occupational physician [3-hour training following a 7-step protocol)], Group B: control group (n = 206; screening without feedback, unrestricted access to usual care). | |
| Smoot and Gonzales38 * | Atlanta, US; Health care; Large | 72 workers; work-related stress | Controlled before and after; 12 months | Individual (communication skills training); Group A: control group (n = 37), Group B: intervention group (n = 35; a 32-hour interpersonal communications program, based on the Carkhuff model, in sequential 8-hour sessions held once a week for 4 weeks; Included didactic experiential component, cognitive component & accurate empathy). | |
| Other health problems | Banco et al39 * | Connecticut, US; Retail and trade (supermarket employees); Large company | 199 workers; cutting injuries | RCT; 12 months | Organizational (Ergonomic intervention with education); 3 groups of similar stores. Group A stores: new safety cutters with training, Group B stores: old cutters with training, Group C stores: control group (old cutters without training). |
| Engst et al40 * | Canada; Health care | 50 workers; risk injuries | Controlled before and after; 48 months | Organizational (ceiling lift program); Group A: intervention group (75-bed extended care unit with ceiling lifts, tracking directly into all of the washrooms, 1-hour session (education and training) by occupational therapist), Group B: control group (75-bed extended care unit without ceiling lifts). | |
| Orenstein et al41 | Virginia; US; Health care | 262 workers; Needlestick injuries | Controlled before and after; 12 months | Organizational (protective devices); Group A: control group, Group B: intervention group (6 months without the use of protective devices, 6 months extensive educational program to introduce protective devices). | |
| Hengel et al42 * | Netherlands; Construction; | 293 workers; health and work ability | RCT; 12 months | Individual; Group A: intervention group (two 30-min training sessions with a physical therapist, Rest-Break tool, two empowerment training sessions), Group B: control group (usual practice). | |
| van der Meer et al43 | Netherlands; Health care | 1,649 workers; hand eczema | RCT; 12 months | Individual (multifaceted implementation strategy); Group A: intervention group (n = 876; education on HE, participatory working groups, role models, reminders, leaflet), Group B: control group (n = 773; leaflet). | |
| Watson et al44 * | UK; Local Authority Council | 57 workers; substance abuse (alcohol) | RCT; 12 months | Individual (brief intervention one-to-one consultation by a registered nurse); Group A: intervention group (n = 28; incorporates Feedback, Responsibility, Advice, Menu of options, Empathy, Self-efficacy model), Group B: control group (n = 29). |
*Cost-effective studies.
Three studies evaluated the cost-effectiveness of interventions targeting mental health problems such as depressive symptoms, mental health complaints, and work-related stress.36–38 Two of the studies were carried out in 2015 and were RCTs, while the older study was a controlled before-and-after design. All studies were individual-level interventions. The participants were from banking companies, research institutes, security companies and universities, or were health care workers.
In the group of other preventive interventions, the studies focused on other health categories, particularly injuries,39–41 health and work ability,42 hand eczema,43 and substance abuse.44 Four such studies were conducted over the last 15 years. Four of these were RCTs, while the remaining two studies were controlled before-and-after design. Most of the studies (n = 3) dealt with organizational-level interventions. The participants were from large diverse industries, such as the healthcare, construction, local authority council, retail, and trade.
The main characteristics of the economic evaluations carried out in each of the studies are presented in Table 2.
TABLE 2.
Data Extraction by Targeted Health Problems: Economic Evaluation Characteristics of Included Studies
| Type and Description of Economic Analysis | Economic Evaluation Results | Cost Description | Economic Consequences; Description of Economic Consequences | Other Outcomes and Results; Outcomes and Results Description | ||
| Musculoskeletal disorders | Aboagye et al26 | CUA (with Sensitivity Analysis); The Incremental cost-effectiveness ratio was estimated using mean incremental cost and the adjusted mean incremental QALY. | Medical yoga costs 206€ less than exercise therapy and 150€ more than self-care advice. The improvement in HRQL appeared to be better with medical yoga than with self-care advice (ICER: 4,984€/ QUALY) and equal for medical yoga and exercise therapy. Medical yoga can be cost-effective if an employer considers that the improvement in employee's HRQL can translate into productivity benefits. | Direct costs: physician assessment (medical yoga: 3,588€, exercise: 3,588€, advice: 3,795€), physician advice (1898€), yoga trainer (9568€), physiotherapists (19,061€), equipment (medical yoga: 120€, exercise: 1,316€, advice: 127€). Total direct costs: medical yoga (1,3276€), exercise (23,965€), advice (5,819€). Mean direct cost: medical yoga (255€), exercise (461€), advice (106€). | . | HRQL (improved significantly by medical yoga compared with self-care advice, but not more than by exercise therapy). |
| Bernaards et al27 * | CEA (with Sensitivity Analysis); Total costs were compared to the effects on recovery & pain intensity. | The total costs for WS were 451€ less than for the usual care, while for WSPA were 230€ more than usual care and 694€ more than WS. Neither intervention was cost-effective in improving overall recovery compared with usual care. WS intervention was cost-effective in reducing average pain compared with usual care (statistically significant results but has weak clinical effect and cannot, therefore be recommended).Company's willingness to pay: 900€/1-point reduction in average pain. | Direct and indirect costs; Intervention costs: counselors (12.5€/worker), time spent on group meetings (WS: 79.5€/ worker, WSPA: 109.5€/ worker), costs of elastic bands for WSPA group (3.2€/ worker), breaks and exercise reminder software (4.5€/ worker or 25€/ worker), Total intervention costs: WS (108€), WSPA (141€), usual care (16€), Costs of productivity loss: WS (1,799€), WSPA (2,670€), usual care (2,294€), Total costs: WS (1907€), WSPA (2,811€), usual care (2,310€). | The costs of productivity loss for WS were 543€ less than for usual care, while for WSPA were 104€ more than usual care and 661€ more than WP. The costs for sickness absence for WS were 583€ less than for usual care, while for WSPA were 51€ more than usual care and 648€ more than WP. | Neck/shoulder average pain reduction | |
| Driessen et al28 | CEA and CBA (without Sensitivity Analysis); ICER was conducted using the four health outcomes. | Monetary loss of 78€/worker. The PE intervention program was neither cost-effective nor cost-beneficial. | Direct and indirect costs; Health care costs: visits to health care providers, diagnostic examinations, medication. PE intervention costs: 29€/worker (study protocol development, ergonomists’ training costs, ergonomists’ costs for guiding the working groups, costs of the total work time, costs of the 4-hour implementation training, costs for room rental, refreshments and training materials). | Mean total costs (health care costs, costs of productivity losses) in the intervention group were 127€ higher than those in the control group. | Low back pain, neck pain, work performance, sick leave (no statistically significant differences between groups). | |
| Greenwood et al29 | CBA (without Sensitivity Analysis) | The overall costs of the intervention were $49,505. The very early intervention was as costly as the standard care and was not more effective. | Direct and indirect costs; Initial evaluation costs/ case including travel: $110. Mean cost for the recovery management services/ case: $651.38; Medical costs: $3,365 (intervention) and $2,965 (control); Disability costs: $5,568 (intervention) and $4,967 (control). | Medical costs increased with the management intervention, while disability costs were not reduced. | Predictive factors of disability and medical benefits; locus of control, alcohol abuse & poor or unsafe environmental surroundings (statistically significant). | |
| Herman et al30 * | CEA (with Sensitivity Analysis); CEA was calculated in terms of cost/day of absenteeism reduced and ROI. | Naturopathic care is a cost-effective alternative to standardized physiotherapy education. ICER: $154/absentee day avoided. ROI: 7.9%. | Direct and indirect costs; Study treatment costs: naturopathic care ($1,469), control ($337). Total adjunctive care costs (chiropractic visit costs, massage visit costs, physiotherapist visit costs, pain medication costs): naturopathic care (-$840), control ($363). Estimated productivity loss: naturopathic care (-$817), control ($324). Adjunctive costs paid by employer: naturopathic care ($17), control ($124). | Total adjunctive care savings: $1,203. Productivity loss savings: $1,141. Adjunctive costs paid by the employer (savings): $107 | Absenteeism (reduction); treatment of chronic low back pain. | |
| Mitchell et al31 | CEA (without Sensitivity Analysis); CEA was performed on costs applicable to providing the belts, treatment of injury and lost or limited duty work days. | Back belts appear to be minimally effective in preventing injury, however they are not cost-effective. Costs of injury wearing a belt are substantially higher than if injured otherwise. | Direct and indirect costs; Costs of belts: $60,000 (intervention); Costs of treatment (medication, back belt, back school, roentgenograms, physical therapy, specialist referral): $18,910 (intervention) and $10,971 (control); Costs of lost days: $101,010 (intervention) and 138,320 (control); Costs of limited days: $215,880 (intervention) and $ 91,030 (control). Total costs: $395,800 (intervention) and $240,321 (control). | Total costs/injured worker (evaluation, treatment and referral uniformly): in the intervention group were $15,5479 higher than those in the control group; lost work days savings ($37,310); costs of limited days (-$124,850). | Rate of limited working days (increase), rate of lost time injury (decrease), rate of back injuries/1,000 workers (increase). | |
| Shi32 * | CBA (without Sensitivity Analysis) | The net benefit of back injury prevention program was $161,108; the return on investment (ROI) was 179%. The intervention was beneficial. | Direct costs: Payments to outside consultants and providers: $60,000, Materials for the program: $ 10,000, Wages: $20,000. | Medical claims savings: $113,348; sick day savings: $137,760; Total costs reduced: $251,108. | Back pain prevalence (modest decline), satisfaction (improved), risk reduction (improved). | |
| Speklé et al33 | CEA and CBA (with Sensitivity Analysis); CEA used the total costs for the outcome's risk factors and prevalence. | The difference in total direct costs between the two groups: 30.73€. Monetary investments: 58.97€/ worker (intervention) & 28.24€/ worker (usual care). ICER/ point change in cost of sick leave: 0.39€. The intervention was not cost-effective compared to usual care. | Direct and indirect costs; Health care costs: general practitioner (21.03€/ visit), medical specialist (102.01€/ visit), physiotherapist and alternative therapist (23.68€/ visit), occupational physiotherapist (121.50€/hour), occupational psychologist (126.50€/ hour), occupational physician (70.00€/ 20 min). Purchased products for symptom reduction: 0--50€ range costs. Intervention costs: RSI Quick-Scan questionnaire (15.00€), information session (30.00€), training RSI & Stress (90.00€), consult occupational physician (70.00€/ 20 min), eyesight test (20.00€), individual workplace assessment (330.00€), task analyses (60.00€). Sick leave: 20.89€-49.78€ range costs/ hour. | Indirect costs due to sick leave (80.20€ higher in the intervention group). | Exposure to risk factors, the prevalence of arm, shoulder & neck symptoms, the number of days of sick leaves (increase). | |
| Tuchin34 * | CBA (without Sensitivity Analysis) | The implied net present value was $52,080. The saving could be in excess of $50,000 for a 3- month period (authors’ comment). A short-term reduction of back injuries was reported. The intervention was cost-effective in reducing working days lost due to back pain or injury. | Direct & indirect costs; Total costs (training costs ($35/ worker) and worker time costs for training ($36/ worker)): $19,880; $71/worker. | Total absenteeism savings: $71,960; $257/worker due to absence expenses reduction. | Days lost from work & number of spinal injuries (reduced) | |
| Versloot et al35 * | CEA (without Sensitivity Analysis); The costs of the back school program were compared with the savings of the reduction in absenteeism. | The net present value was $103,400 (change in absenteeism was assessed in relation to the change in the control group). The net present value was $70,200 (change in absenteeism was assessed only within the intervention group). The back school program was cost-effective in relation to the reduction of costs of absenteeism. | Direct and indirect costs; Total costs of the intervention (costs of the total training program and wages due to lost working hours): $46,000; $230/ worker | Total absenteeism savings (based on changes between the intervention and control group): $149,400; $900/ worker. Total absenteeism savings (based on changes within the intervention group): $116,200; $700/ worker. | Sick leave, quality, and perceived effect of program; A reduction in mean length of absenteeism/worker: 6.5 days/ year (based on changes between the intervention and control group) and 5 days/year (based on changes within the intervention group). | |
| Mental health | Geraedts et al36 | CEA and CUA (with Sensitivity Analysis); ICER was calculated for the depressive symptoms. CEACs: the probability of the intervention being cost-effective in comparison with usual care for a range of ceiling ratios. ROI. | ICER for depressive symptoms: 224, Probability gradually increases with increasing values of willingness to pay to a maximum of 0.95 at a ceiling ratio of 3,500€, ICER for clinically significant change: -4664, Probability gradually increases with increasing values of willingness to pay to a maximum of 0.95 at a ceiling ratio of 115,000€. Cost-savings: 382,354€/every QALY lost. Total benefits (occupational health, absenteeism, presenteeism costs): 793€ (average), Net benefit: 508€ (average), BCR: 2.8, ROI: 178%. The intervention's probability of financial return: 0.63. Significant intervention effect on depressive symptoms. The intervention is not cost-saving to the employer. | Direct and indirect costs; Intervention costs (web site hosting, maintenance costs, labor costs of the coaches): 285€; Occupational health costs: 41€ (for intervention group) and 48€ (for control group); Absenteeism costs: 8,668€ (for interventional group) and 8,175€ (for control group); Presenteeism costs: 13,980€ (for intervention group) and 1,5259€ (for control group); Total: 22,974€ (for interventional group) and 2,3482€ (for control group). | Costs of Productivity losses: Absenteeism costs (mean cost difference between the two groups): 492€; Presenteeism costs (mean cost difference between the two groups): -1278. | Depressive symptoms (improved) |
| Noben et al37 * | CBA (with Sensitivity Analysis); ROI. | Net benefits: 651€/ worker. ROI: 11€/ 1€ investment. Beneficial intervention (limited time horizon). | Direct and indirect costs; Intervention costs (web-based screening and feedback module, periodically upgrading the module, hosting on a server: 4€/ worker; occupational physician consulting: 73€/ worker; occupational physician assistant: 3€/ worker; occupational physician training in using the protocol: 50€/ visit): 130€/ worker. Costs of productivity losses. Mean/ worker intervention costs: 89€ (intervention group) and 25€ (control group). | Cost difference between the two groups: 64€ (statistically significant). Cost reductions resulting from greater productivity: 715€ (statistically significant) | Mental health complaints (anxiety, distress, work-related fatigue, risky drinking, depression, & post-traumatic stress disorder), productivity (improved) | |
| Smoot and Gonzales38 * | CBA (without Sensitivity Analysis) | Substantial savings for the intervention group and increased expenditures for the control group. The training focusing on improving empathic communication skills is promising as a proactive, cost-effective approach to reducing staff turnover ($21,606) and improving both staff and patient outcomes. | Direct and indirect costs; Total cost for training staff: $13,145. For intervention group: Staff resignations and transfers: $35,358 (1990), $13,752 (1991); Sick leave: $26,490 (1990), $19,032 (1991); Annual leave: $35,142 (1990), $9,408 (1991); Patients’ rights complaints: $3,690 (1990), $1,110 (1991); Incidents of restraint and seclusion: $17,280 (1990), $12,096 (1991); Assaults on staff: $276 (1990), $246 (1991); Total: $118,236 (1990), $55,644 (1991).For control group: Staff resignations and transfers: $25,536 (1990) and $29,466 (1991); Sick leave: $21,948 (1990) and $20,544 (1991); Annual leave: $25302 (1990) and $27,246 (1991); Patients’ rights complaints: $738 (1990) & $2592 (1991); Incidents of restraint and seclusion: $16,416 (1990) & $32,832 (1991); Assaults on staff: $768 (1990) and $276 (1991); Total: $90,708 (1990) and $112,956 (1991). | Expenditures for intervention group were reduced by ≈$62,592. Expenditures for control group increased by $22,248. | Lower staff turnover (-61.1%), less sick (-28.2%) & annual leave (-73.2%), staff satisfaction (increased), fewer patients’ rights complaints (-69.9%), fewer assaults on staff (-10.9%), less incidents of restraint & seclusion (-30% | |
| Other health problems | Banco et al39 * | CBA (without Sensitivity Analysis) | Total net savings for the Group A stores (new cutter and education) were $245 per 100,000 man hours/store and a total net savings of $29,413/ year for the chain. Benefits for the Group B stores (education) were: $106 per 100,000 man-hours/ store and for the chain was $12.773. Intervention A was more cost-effective. | Direct and indirect costs; Supply costs (case cutters): $0.17/ cutter for old cutters vs $2.35/cutter for new safety cutters, $362 (group A), $269 (group B), and $403 (group C); Education costs: $20/ =hour health educators, $333 (group A) and $362 (group B); Compensation savings (medical care and workers’ compensation): $317 (group A) and $188 (group B); Time lost savings: $107 (group A) and $98 (group B). | Wage value of time loss from work due to injury, employees’ compensation expenses (medical care and indemnity). | Injury rates/100,000 man hours; reduction of cutting injuries, reduction of other types of injuries. |
| Engst et al40 * | CBA (without Sensitivity Analysis) | Payback period for the intervention: 9.6 years (including all resident handling claims) and 6.5 years (including only lifting and transferring claims). Ceiling lifts were effective method only for lifting and transferring residents. | Direct and indirect costs; Total intervention costs: $284,297. Medical costs, lost work time costs, purchasing and installing the intervention, hiring a program coordinator, staff replacement costs for education, and training. | Adjusted direct savings: $9,835 (all resident handling) and $14,493 (lifting and transferring tasks). Compensation Claims for the intervention group: 22.7% decrease (resident handling), 68.3% decrease (lifting and transferring), and 52.5% increase (repositioning). Compensation Claims for the control group: 12.2% decrease (resident handling), 68.3% increase (lifting & transferring) and 33.9% decrease (repositioning). | Risk for musculoskeletal injuries (decrease), job satisfaction (increase for both groups), physical discomfort, staff perceptions, and preferences. | |
| Orenstein, et al.,41 (1995) | CEA (with Sensitivity Analysis) | The average evaluation cost/ NSI: $260. Total NSI evaluation cost: $8,580 (before intervention) and $3,649 (after intervention). Cost per NSI prevented: $789. The use of protective devices was not beneficial. | Direct costs of NSI: cost of employee time, laboratory technician time, testing fees. Total device costs: $2,444 [before intervention (needles, heparin locks, 3 ml syringes)] and $22,558 [after intervention (protective devices, needles, syringes)]. Total costs: $11,024 (before intervention) and $ 26,198 (after intervention). | Total NSI cost savings: $4,940. Excess cost: $15,178. | Number of needle-stick injuries decreased (not statistically significant). | |
| Hengel et al42 * | CEA and CBA (with Sensitivity Analysis); CEA was calculated for the three health outcomes; Benefit cost ratio: by dividing the benefits by the costs. ROI. | ICER for work ability: 5,243€, ICERs for physical health: 798, ICERs for mental health: -642, ICERs for upper extremities: 12,133, ICERs for lower extremities: 59,716. Net benefit: 641€. Benefit cost ratio: 6.4 (for each 1€ invested, 6.4€/ worker was gained). ROI: 544%. The intervention was cost-effective only for absenteeism reduction (and cannot therefore be recommended). | Direct and indirect costs; Mean intervention costs (physician therapist, empowerment trainer, material costs): 118€/ worker. Costs of productivity losses. | Costs of productivity losses from absenteeism and presenteeism; Savings in sickness absenteeism costs: 760€/ worker. | ||
| van der Meer et al43 | CEA (with Sensitivity Analysis); CEACs: the probability of the intervention being cost-effective in comparison with usual care for a range of ceiling ratios. ROI. | ICER for HE: -57,299, CEAC: 0.09, Probability gradually increases with increasing values of willingness to pay to a maximum of 0.84 at a ceiling ratio of 580,000€, ICER for compliance measure: 15,559, CEAC: 0.09, Probability gradually increases with increasing values of willingness to pay to a maximum of 0.82 at a ceiling ratio of 480,000€. ROI was negative during the following up. The intervention's probability of financial return is: 0.12. The intervention was neither cost-effective nor cost-beneficial to the employer. | Direct & indirect costs; Intervention costs: 114€/ worker. Primary and secondary health care services costs, costs of absenteeism, costs of presenteeism. Total savings: 3,318€. | Costs of productivity losses due to HE. Presenteeism costs (the difference between the two groups): 2,764€. | Prevalence of hand eczema. | |
| Watson et al44 * | CUA (without Sensitivity Analysis) | The difference between two groups: -0.002 - (-0.010). Net advantage of the intervention: 0.008 QALYs. Net saving (the difference in service costs between two groups): £344.5/person. The alcohol brief intervention appears to be cost-effective. | Direct costs; Costs of the intervention: £12.48/26 min or £0.48/min. No analytical costs were presented. | . | Maximum number of units in 1 day, number of drinking days/week, total weekly consumption, AUDIT scores, general health. |
*Cost-effective studies.
Quality Assessment
The overview of risk of bias assessment is summarized in Table 3. Overall, the intervention studies were judged as having an unclear risk of bias, as the majority of them were rated as having either low or unclear risk of bias (see Cochrane Collaboration's recommendations).22 Older studies (before 2005) had at least one domain judged as having unclear or high risk of bias, while more recent studies were rated as having either low or unclear risk of bias.
TABLE 3.
Risk of Bias in Included Studies: Low Risk (+); Unclear Risk (?); High Risk (-); Not Applicable N/A
| Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias | Summary Assessments | ||
| Musculoskeletal disorders | Aboagye et al26 | (+) | (?) | (?) | (+) | (?) | (+) | (?) | Unclear risk of bias |
| Bernaards et al27 * | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias | |
| Driessen et al28 | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias | |
| Greenwood et al29 | (+) | (+) | (?) | (?) | (?) | (+) | (?) | Unclear risk of bias | |
| Herman et al30 * | (+) | (?) | (+) | (+) | (+) | (+) | (+) | Unclear risk of bias | |
| Mitchell et al31 | N/A | N/A | N/A | (?) | (?) | (+) | (?) | Unclear risk of bias | |
| Shi32 * | (?) | (?) | (+) | (+) | (?) | (?) | (?) | Unclear risk of bias | |
| Speklé et al33 | (+) | (+) | (+) | (+) | (?) | (+) | (+) | Unclear risk of bias | |
| Tuchin34 * | (?) | (-) | (?) | (+) | (?) | (+) | (?) | High risk of bias | |
| Versloot et al35 * | (?) | (?) | (+) | (+) | (?) | (+) | (-) | High risk of bias | |
| Mental health | Geraedts et al36 | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias |
| Noben et al37 * | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias | |
| Smoot and Gonzales38 * | N/A | N/A | (-) | (+) | (?) | (?) | (?) | High risk of bias | |
| Other health problems | Banco et al39 * | (?) | (?) | (+) | (+) | (?) | (+) | (?) | Unclear risk of bias |
| Engst et al40 * | N/A | N/A | (+) | (+) | (?) | (+) | (+) | Unclear risk of bias | |
| Orenstein, et al41 | N/A | N/A | (+) | (+) | (?) | (+) | (+) | Unclear risk of bias | |
| Hengel et al42 * | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias | |
| van der Meer et al43 | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias | |
| Watson et al44 * | (+) | (+) | (+) | (+) | (+) | (+) | (+) | Low risk of bias |
*Cost-effective studies.
The overview of the CHEC-list and the percentage achieved by the studies are presented in Table 4. Older studies generally scored poorly (between 42% and 74%) on the aspects of the assessment due to the insufficient information, while more recent studies achieved better methodological quality scores (between 58% and 95%) related to undertaking and reporting economic evaluations. The most prevalent methodological shortcomings for more than half of the studies were no sensitivity analysis and no discussion of the generalizability of findings. None of the studies discussed ethical issues or elaborated on the characteristics of the intervention population, which indicates possible distributional implications. All studies except two29,38 conducted an incremental analysis.
TABLE 4.
Internal and External Validity of Included Studies; The Consensus Health Economic Criteria List: Yes = 1; No = 0
| Musculoskeletal Disorders | Mental Health | Other Health Problems | |||||||||||||||||
| Aboagye et al26 | Bernaards et al27 * | Driessen et al28 | Greenwood et al29 | Herman et al30 * | Mitchell et al31 | Shi32 * | Speklé et al33 | Tuchin34 * | Versloot et al35 * | Geraedts et al36 | Noben et al37 * | Smoot and Gonzales38 * | Banco et al39 * | Engst et al40 * | Orenstein, et al41 | Hengel, et al42 * | van der Meer et al,43 | Watson, et al44 * | |
| Is the study population clearly described? | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 |
| Are competing alternatives clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is a well-defined research question posed in answerable form? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the economic study design appropriate to the stated objective? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the chosen time horizon appropriate in order to include relevant costs and consequences? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Is the actual perspective chosen appropriate? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Are all important and relevant costs for each alternative identified? | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 |
| Are all costs measured appropriately in physical units? | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 |
| Are costs valued appropriately? | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| Are all important and relevant outcomes for each alternative identified? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Are all outcomes measured appropriately? | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Are outcomes valued appropriately? | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Is an incremental analysis of costs and outcomes of alternatives performed? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| Are all future costs and outcomes discounted appropriately? | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| Are all important variables, whose values are uncertain, appropriately subjected to sensitivity analysis? | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 |
| Do the conclusions follow from the data reported? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Does the study discuss the generalizability of the results to other settings and patient/client groups? | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Does the article indicate that there is no potential conflict of interest of study researcher(s) and funder(s)? | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 |
| Are ethical and distributional issues discussed appropriately? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total score (%) | 17 (89) | 18 (95) | 17 (89) | 9 (47) | 17 (89) | 9 (47) | 11 (58) | 17 (89) | 11 (58) | 8 (42) | 18 (95) | 18 (95) | 12 (63) | 11 (58) | 11 (58) | 14 (74) | 18 (95) | 17 (89) | 13 (68) |
*Cost-effective studies.
Cost-effective Interventions
The review has identified 11 cost-effective OSH interventions based on statistically significant results. Of the MSD interventions, five studies27,30,32,34,35 reported cost savings or monetary benefits in favor of the following interventions: work style, naturopathic care, back injury prevention program, spinal care lecture, back school program. The cost-effective study with the work style intervention achieved a high score on CHEC-list and had a low risk of bias.27 The other four cost-effective studies in the group30,32,34,35 achieved high, moderate, or low scores on the CHEC-list and had either unclear or a high risk of bias (see Table 5). Three of the cost-effective studies conducted a cost-effectiveness analysis (CEA),27,30,35 while two conducted a cost–benefit analysis (CBA).32,34 The cost-effective studies reported the difference between monetary benefits and program costs as net savings or benefits, or as the return on investment (ROI). They also identified the direct as well as the indirect costs of the interventions. The main economic consequence was savings due to absenteeism or productivity loss. Other outcomes dealt with the reduction of neck/shoulder pain, (low) back pain, and back injuries.
TABLE 5.
A Summary of the Methodological Quality of Cost-Effective Interventions
| High Score on the CHEC-List With Low Risk of Bias | High Score on the CHEC-List With Unclear Risk of Bias | Moderate Score on the CHEC-List With Low Risk of Bias | Moderate Score on the CHEC-List With Unclear Risk of Bias | Moderate Score on the CHEC-List With High Risk of Bias | Low Score on the CHEC-List With High Risk of Bias | |
| Musculoskeletal disorders | Bernaards et al27Intervention: work styleOutcomes: neck/shoulder pain reduction (significant but small effect) | Herman et al30Intervention: naturopathic careOutcomes: absenteeism reduction; treatment of chronic low back pain | . | Shi32Intervention: back injury programOutcomes: back pain prevalence; back injury risk reduction | Tuchin34Intervention: spinal care lectureOutcomes: reduction of spinal injuries and back pain | Versloot et al35Intervention: back school programOutcomes: mean length of absenteeism |
| Mental health | Noben et al37Intervention: occupational physician consultationOutcomes: reduction of mental health complaints; production improvement | . | . | . | Smoot and Gonzales38Intervention: communication skills training programOutcomes: reduction of staff stress and turnover | . |
| Other health problems | Hengel et al42Intervention: physical therapist training sessionOutcomes: reduction in days of sick leave | . | Watson et al44Intervention: alcohol brief interventionOutcomes: reduction of alcohol-related harm | Banco et al39Intervention: new safety cuttersOutcomes: reduction of cutting injuries | . | . |
| . | . | . | Engst et al40Intervention: ceiling liftsOutcomes: reduction of risk of injuries and physical discomfort | . | . |
In the group of mental health interventions, the occupational physician consultation program37 and the communication skills training program38 were cost beneficial. The intervention study with the occupational physician consultation program achieved a high score on the CHEC-list and had a low risk of bias,37 while the other study achieved a moderate score on the CHEC-list and had a high risk of bias38 (see Table 5). Both studies conducted a CBA and reported the difference between monetary benefits and program costs as net savings or benefits, or ROI. The studies included both direct and indirect costs. The economic consequence of the interventions of both studies was the savings due to absenteeism or productivity loss. A range of outcomes were evaluated, such as mental health complaints, staff turnover, and work-related stress.
In the group of other preventive interventions, two organizational-level interventions (new safety cutters with education39 and ceiling lifts),40 which conducted a CBA, one individual-level intervention (physical therapist training session),42 which conducted both a CEA and a CBA, and one individual-level intervention (alcohol brief consultation),44 which conducted a CUA, reported cost savings or monetary benefits. The individual-level intervention study of Hengel et al42 achieved a high score on the CHEC-list and had a low risk of bias, while the other individual-level intervention study achieved a moderate score on the CHEC-list and had a low risk of bias.44 The two organizational-level intervention studies had moderate scores on CHEC-list and unclear risk of bias39,40 (see Table 5). The studies reported the difference between monetary benefits and program costs as net savings or benefits. Most of the studies took both the direct and the indirect costs of the interventions into account. The predominant economic consequences were productivity losses, the wage value of working time loss due to injury, and workers’ compensation expenses.
Interventions not Shown to be Cost-effective
Eight OSH interventions not shown to be cost-effective were identified. In the group of MSD interventions, five studies26,28,29,31,33 were not shown to be cost-effective. Driessen et al28 achieved a high score on the CHEC-list and had a low risk of bias. The other four studies in the group achieved either high26,33 or low29,31 scores on the CHEC-list and had an unclear risk of bias. Two studies conducted both CEA and CBA,28,33 while three conducted a CEA,31 a CBA,29 or a CUA.26 The studies identified both the direct and the indirect costs of the interventions, except for Aboagye et al26 who did not include indirect costs.
In the group of mental health interventions, the intervention of the study carried out by Geraedts et al36 was not cost beneficial. The intervention study achieved a high score on the CHEC-list and had a low risk of bias. The study conducted both CEA and CUA and included both direct and indirect costs.
In the group of other preventive interventions, two studies,41,43 which conducted a CEA, were not shown to be cost-effective. van der Meer et al43 achieved a high score on the CHEC-list and had low risk of bias, while Orenstein et al41 achieved a moderate score on the CHEC-list and had unclear risk of bias. Orenstein et al41 did not include indirect costs, which is essential information in order to be able to draw unambiguous conclusions about the cost-effectiveness of an intervention.
DISCUSSION
Main Findings
The main aim of this systematic review was to evaluate the cost-effectiveness of OSH interventions from the employer perspective. The small number of published studies, the variety of OSH-interventions, the targeted health problems, and outcomes in combination with shifting quality make it difficult to draw conclusions about the cost-effectiveness of specific OSH-interventions. This heterogeneity was also the reason why we did not apply meta-analytical approach to the data. Nevertheless, the single studies do give some interesting results.
Nineteen individual-level and organizational-level intervention studies, divided into three groups (MSD, mental health, and other preventive interventions), fulfilled the inclusion criteria and were included in the study. MSD and mental health disorders are the two most common causes of sickness absence and high costs for employers.45,46 Both these conditions have previously been shown to be related to the work environment.46–48 Only one of the MSD studies looked at an organizational-level intervention, while another looked at both organizational and individual levels. None of these interventions were shown to be cost-effective. Of the mental health intervention studies, none included organizational-level changes, which indicates inadequate interest in interventions at this level. As mental health problems can arise as a result of work environment problems, there is a need of OSH interventions targeting the organizational level to prevent these problems. According to several studies, organizational-level changes to improve psychosocial working conditions can have important and beneficial effects on health.49,50 However, difficulties in evaluating the effectiveness of such interventions can affect employers in their decision to conduct them.51 As economic incentives are important for several employers in order to motivate them to engage in OSH interventions, studies evaluating cost-effectiveness of organizational-level interventions are needed. In the group of “other preventive interventions,” two cost-effective organizational-level interventions39,40 and one which was not shown to be cost-effective41 were related to injuries (cutting injuries, MSD injuries, needle-stick injuries). Although the workplace is a setting venue that provides access to employees with work-related health problems, companies do not appear to take advantage of this for their benefit by implementing organizational-level interventions. They tend rather to focus on interventions at individual-level. It is unclear whether this is due to company preference or because researchers tend to conduct mostly individual-level interventions.
The main type of economic analysis of the interventions was the CBA, which is highly appropriate for OSH studies. However, CEA and CUA are also useful in OSH if the outcome of interest can be measured in natural units.52 Several studies were excluded from the review during the eligibility process because they lacked a control group. The control group is an essential element of a full economic evaluation; lack of control group blurs the distinction between the effects of an intervention and autonomous change over time. Conducting a full economic evaluation, which is the only type of economic analysis that provides valid information about efficiency,20,25 requires the identification, measurement, and valuation of costs and consequences because it compares the effectiveness and the benefits of two or more interventions. If one wants to be able to draw conclusions about the cost-effectiveness of OSH, only the results of full economic evaluations (such as benefit–cost ratio, net benefits or savings, incremental cost-effectiveness ratio, cost per quality-adjusted life-year) should be used. Some economic studies that claim to be full economic evaluations may in fact only be partial evaluations.53 For instance, an intervention can appear to be cost-effective but when compared with a control group it proves not to be.18 This is a problem when evaluating the cost-effectiveness of OSH interventions. Moreover, small-medium enterprises (SMEs) are a neglected sector in OSH research and practice and there is a lack of economic evaluations of OSH interventions in this type of company, despite the fact that they dominate in most economies. SMEs need special attention because their knowledge of and financial resources for conducting interventions are limited. It is also difficult for SMEs to implement and adopt the strategies employed by larger organizations.3,54,55
Eight of the studies included in this review were published during the 1990s, most of them related to MSDs. Only two studies were published during the next decade, while there was a substantial increase in relevant published studies from 2010 onwards. Our findings indicate that older studies (pre-2005) scored poorly on the aspects of the assessment due to the insufficient information, while newer studies were rated as having high-quality evidence. However, further improvements in line with the CHEC-list are still needed, for example, the sensitivity analysis, the discussion of the generalizability of the results, and that of ethical and distributional issues.24,52 In common with previous systematic reviews2,6–8,19,20,56 that evaluated the cost-effectiveness of workplace interventions, the present review concludes that there is a need for further research and methodological quality improvements because of insufficient and poor results. High-quality evidence is also related to indirect costs, such as productivity losses, being sufficiently reported. Some economic evaluations, for example, may not present incremental cost-effectiveness and/or resource use (such as intervention staff hours, materials used, depreciation, overhead activities, traveling), or they may not include a full identification of all important and relevant costs (for instance indirect costs such as productivity loss, absenteeism, presenteeism). The costs may not have been measured appropriately, using a valid instrument, or they may not include any type of sensitivity analysis to assess the robustness of results.2,19,20 The lack of this economic information makes it difficult to draw robust conclusions. In particular, the interventions of Aboagye et al26 and Orenstein et al41 might have been identified as noncost-effective due to the lack of productivity losses costs.
In all, 11 interventions were evaluated as being cost-effective. Only three of them, one from each group, were rated as having high methodological quality with regard to undertaking and reporting economic evaluations and a low risk of bias. These were the following: MSD: work style27; mental health: occupational physician consultation37; other preventive interventions: physical therapist training session.42 None of them, however, is recommended without reservation in its current form. According to Bernaards et al,27 the observed pain reductions in the work style intervention group compared with usual care were significant but less than 30% and therefore not clinically relevant. Noben et al37 recommended a wider implementation of the intervention because the period was too short to be able to judge whether the effects will be maintained over time. According to Hengel et al,42 the intervention was cost-saving in terms of reduced sickness absenteeism costs, but not in terms of primary and secondary health outcomes. The generalizability and comparability of the studies of cost-effectiveness are debatable because of methodological differences and heterogeneous characteristics and effect measures, which make the evidence ambiguous. Even in the MSD group, where the health outcomes were similar (back pain and back injuries), the studies used a variety of interventions, with education as the only common factor. In addition, uncertainty surrounding unit cost estimates does not appear to have been considered within the analyses. As a result, the amount of economic evidence was very limited. The results should therefore be viewed with caution and regarded as preliminary. Nevertheless, the studies of Herman et al30 and Watson et al44 appear promising, given their methodological quality and sufficient degree of economic evidence. They also include features that encourage further research.
Strengths and Limitations
One of the strengths of this systematic review is the comprehensive search strategy used, which facilitated a more evidence-based approach to literature searching. Another important strength is the use of two methodological quality assessment tools, both recommended by Cochrane Collaboration, to assess simultaneously the risk of bias and the economic quality of the included studies. In the present systematic review, we did not include “grey” literature, which may have excluded some studies from the review. In addition, due to the heterogeneity of study designs, populations, interventions, and outcomes, we were unable to conduct a meta-analysis.
Conclusion and Implications for Future Research
Information about the financial benefits of OSH interventions is important for employers. The results of the present systematic review do not enable us to draw conclusions about specific interventions due to the limited number of economic evaluations, the diverse nature of the interventions, the number of targeted health problems and health outcomes, and the insufficient reporting of economic quality and risk of bias. Thus, our review highlights the need for more well-designed studies that address the economic merits of OSH interventions from the employer perspective and target diverse health problems, such as mental health, cardiovascular diseases, respiratory diseases, substance abuse, dangerous substances, and outcomes. Nevertheless, five of the cost-effective intervention studies can be considered promising, under certain conditions and modifications.27,30,37,42,44
An economic evaluation should serve to measure productivity, health, and safety, motivating the firms’ principles to improve each of these methods of measurement, rather than just presenting a cost–benefit analysis of an intervention.3 Although economic evaluation studies have been improved over the years, there is still room for further improvements. Although CBA is highly appropriate for OSH studies, CEA and CUA are also useful in OSH if the outcome of interest can be measured in natural units. We would also encourage the authors of economic evaluations to adopt more ambitious analytical strategies with more advanced regression techniques (see for instance the net benefit regression framework, recommended by Hoch and Dewa).57 A full identification of all important and relevant costs should be given in relation to the perspective and the research question. The costs should be measured appropriately in physical units, using valid instruments. The sources of valuation should be clearly stated, the main cost should not be calculated using tariffs, and the discounting should be done appropriately. The outcomes should also be measured appropriately, using valid instruments, while the valuation method should be clearly stated. In addition, all important variables should be subjected to an appropriate sensitivity analysis.1,5,24,58 Finally, further much-needed improvements are the inclusion of control groups and the development of intervention studies at organizational level.
The above findings are of value to employers, OSH practitioners, and policymakers who are interested in knowing what interventions are worth undertaking from a financial point of view.2,7 Economic evaluations provide a unique opportunity to estimate the resource implications of OSH interventions at low incremental cost. However, when interpreting economic evaluations of OSH interventions, it is important to consider that their results may not be directly applicable to other countries due to differences in health care and social security systems or other relevant factors. Nonetheless, economic evaluation results can be generalized from one country to another, after necessary calculations. Employers and stakeholders can exploit the extensive description of the interventions, the detailed list of resource use as well as information of the health care system and the allocation of costs.5
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the assistance of AFA Insurance for funding the study. The authors extend their gratitude to the Karolinska Institutet University Library staff, Carl Gornitzki and Susanne Gustafsson, for their time and expertise in developing and running the search strategy. The authors also thank Emma Cedstrand and Carl Strömberg for their assistance with the screening process.
Footnotes
AG (Aikaterini Grimani) was the leader author and contributed to the study design, screening process (as a reviewer), eligibility process (as a reviewer), data extraction, methodological quality evaluation. GB (Gunnar Bergström) contributed, as a senior expert, to the study design, methodological quality assessment procedure, revised the paper critically, and contributed to it intellectually. MRC (Martha Isabel Riaño Casallas) contributed to the study design, eligibility process (as a reviewer), data extraction, and was involved in the writing process. EA (Emmanuel Aboagye) contributed to the study design and methodological quality evaluation. IJ (Irene Jensen) contributed, as a senior expert, to the study design, revised the paper critically, and contributed to it intellectually. MLK (Malin Lohela Karlsson) was the study supervisor and contributed to the screening process (as a reviewer), the eligibility process, data extraction, methodological quality evaluation (as a consultant reviewer), revised the paper critically, and contributed to it intellectually. All the authors have read and approved the final version of the manuscript.
The funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Authors Grimani, Bergström, Casallas, Aboagye, Jensen, and Lohela-Karlsson have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
REFERENCES
- 1.Tompa E, Dolinschi R, de Oliveira C. Practice and potential of economic evaluation of workplace-based interventions for occupational health and safety. J Occup Rehab 2006; 16:375–400. [DOI] [PubMed] [Google Scholar]
- 2.Tompa E, Dolinschi R, de Oliveira C, Irvin E. A systematic review of occupational health and safety interventions with economic analyses. J Occup Environ Med 2009; 51:1004–1023. [DOI] [PubMed] [Google Scholar]
- 3.Biddle E, Ray T, Owusu-Edusei K, Camm T. Synthesis and recommendations of the economic evaluation of OHS interventions at the company level conference. J Safety Res 2005; 36:261–267. [DOI] [PubMed] [Google Scholar]
- 4.Miller P, Haslam C. Why employers spend money on employee health: interviews with occupational health and safety professionals from British Industry. Safety Sci 2009; 47:163–169. [Google Scholar]
- 5.van Dongen JM, van Wier MF, Tompa E, et al. Trial-based economic evaluations in occupational health: principles, methods, and recommendations. J Occup Environ Med 2014; 56:563–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamberg-van Reenen HH, Proper KI, van den Berg M. Worksite mental health interventions: a systematic review of economic evaluations. Occup Environ Med 2012; 69:837–845. [DOI] [PubMed] [Google Scholar]
- 7.Tompa E, Dolinschi R, de Oliveira C, Amick BC, 3rd, Irvin E. A systematic review of workplace ergonomic interventions with economic analyses. J Occup Rehab 2010; 20:220–234. [DOI] [PubMed] [Google Scholar]
- 8.Verbeek J, Pulliainen M, Kankaanpaa E. A systematic review of occupational safety and health business cases. Scand J Work Environ Health 2009; 35:403–412. [DOI] [PubMed] [Google Scholar]
- 9.Last J. A Dictionary of Epidemiology. Toronto: Oxford University Press; 1988. [Google Scholar]
- 10.Frank J, Cullen K, Gr IWHAHW. Preventing injury, illness and disability at work. Scand J Work Environ Health 2006; 32:160–167. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson C. Fundamentals of Health at Work: The Social Dimensions. New York: Taylor and Francis; 2003. [Google Scholar]
- 12.Alli B. Fundamental Principles of Occupational Health and Safety. 2 ed.Geneva: International Labor Office; 2008. [Google Scholar]
- 13.O’ Donnell M. Health Promotion in the Workplace. Toronto: American Journal of Health Promotion Inc; 2014. [Google Scholar]
- 14.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 349:g7647. [DOI] [PubMed] [Google Scholar]
- 16.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007; 7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014; 14:579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schelvis RMC, Hengel KMO, Burdorf A, Blatter BM, Stnjk JE, van der Beek AJ. Evaluation of occupational health interventions using a randomized controlled trial: challenges and alternative research designs. Scand J Work Environ Health 2015; 41:491–503. [DOI] [PubMed] [Google Scholar]
- 19.Tompa E, de Oliveira C, Dolinschi R, Irvin E. A systematic review of disability management interventions with economic evaluations. J Occup Rehab 2008; 18:16–26. [DOI] [PubMed] [Google Scholar]
- 20.Uegaki K, de Bruijne MC, Lambeek L, et al. Economic evaluations of occupational health interventions from a corporate perspective: a systematic review of methodological quality. Scand J Work Environ Health 2010; 36:273–288. [DOI] [PubMed] [Google Scholar]
- 21.Tompa E, Dolinschi R, Laing A. An economic evaluation of a participatory ergonomics process in an auto parts manufacturer. J Safety Res 2009; 40:41–47. [DOI] [PubMed] [Google Scholar]
- 22.Higgins J, Green S. The Cochrane Collaboration, Cochrane Handbook for Systematic Reviews of Interventions. London, UK: 2011. [Google Scholar]
- 23.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2012; 18:12–18. [DOI] [PubMed] [Google Scholar]
- 24.Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on Health Economic Criteria. Int J Technol Assess Health Care 2005; 21:240–245. [PubMed] [Google Scholar]
- 25.Deeks J, Higgins JPT, Altman DG. Higgins J, Green S. Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions. London, UK: The Cochrane Collaboration; 2011. 243–296. [Google Scholar]
- 26.Aboagye E, Karlsson ML, Hagberg J, Jensen I. Cost-effectiveness of early interventions for non-specific low back pain: a randomized controlled study investigating medical yoga, exercise therapy and self-care advice. J Rehab Med 2015; 47:167–173. [DOI] [PubMed] [Google Scholar]
- 27.Bernaards CM, Bosmans JE, Hildebrandt VH, Tulder MW, Heymans MW. The cost-effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on recovery from neck and upper limb symptoms and pain reduction in computer workers. Occup Environ Med 2011; 68:265–272. [DOI] [PubMed] [Google Scholar]
- 28.Driessen M, Bosmans J, Proper K, Anema J, Bongers P, Beek A. The economic evaluation of a participatory ergonomics programme to prevent low back and neck pain. Work (Reading, Mass) 2012; 41 Suppl 1:2315–2320. [DOI] [PubMed] [Google Scholar]
- 29.Greenwood JG, Wolf HJ, Pearson JC, Woon CL, Posey P, Main CF. Early intervention in low-back disability among coal-miners in West-Virginia: negative findings. J Occup Med 1990; 32:1047–1052. [PubMed] [Google Scholar]
- 30.Herman PM, Szczurko O, Cooley K, Mills EJ. Cost-effectiveness of naturopathic care for chronic low back pain. Altern Ther Health Med 2008; 14:32–39. [PubMed] [Google Scholar]
- 31.Mitchell LV, Lawler FH, Bowen D, Mote W, Asundi P, Purswell J. Effectiveness and cost-effectiveness of employer-issued back belts in areas of high risk for back injury. J Occup Med 1994; 36:90–94. [PubMed] [Google Scholar]
- 32.Shi L. A cost-benefit analysis of a California county's back injury prevention program. Public Health Rep 1993; 108:204–211. [PMC free article] [PubMed] [Google Scholar]
- 33.Speklé EM, Heinrich J, Hoozemans MJ, et al. The cost-effectiveness of the RSI QuickScan intervention programme for computer workers: results of an economic evaluation alongside a randomised controlled trial. BMC Musculoskelet Disord 2010; 11:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tuchin P, Pollard H. The cost-effectiveness of spinal care education as a preventive strategy for spinal injury. J Occup Health Saf 1998; 14:43–51. [Google Scholar]
- 35.Versloot JM, Rozeman A, Vanson AM, Vanakkerveeken PF. The cost-effectiveness of a back school program in industry: a longitudinal controlled field-study. Spine (Phila Pa 1976) 1992; 17:22–27. [DOI] [PubMed] [Google Scholar]
- 36.Geraedts AS, van Dongen JM, Kleiboer AM, et al. Economic evaluation of a web-based guided self-help intervention for employees with depressive symptoms results of a randomized controlled trial. J Occup Environ Med 2015; 57:666–675. [DOI] [PubMed] [Google Scholar]
- 37.Noben C, Evers S, Nieuwenhuijsen K, et al. Protecting and promoting mental health of nurses in the hospital setting: is it cost-effective from an employer's perspective? Int J Occup Med Environ Health 2015; 28:891–900. [DOI] [PubMed] [Google Scholar]
- 38.Smoot SL, Gonzales JL. Cost-effective communication-skills training for state-hospital employees. Psychiatr Serv 1995; 46:819–822. [DOI] [PubMed] [Google Scholar]
- 39.Banco L, Lapidus G, Monopoli J, Zavoski R. The safe teen work project: a study to reduce cutting injuries among young and inexperienced workers. Am J Ind Med 1997; 31:619–622. [DOI] [PubMed] [Google Scholar]
- 40.Engst C, Chhokar R, Miller A, Tate RB, Yassi A. Effectiveness of overhead lifting devices in reducing the risk of injury to care staff in extended care facilities. Ergonomics 2005; 48:187–199. [DOI] [PubMed] [Google Scholar]
- 41.Orenstein R, Reynolds L, Karabaic M, Lamb A, Markowitz SM, Wong ES. Do protective devices prevent needlestick injuries among health care workers? Am J Infect Control 1995; 23:344–351. [DOI] [PubMed] [Google Scholar]
- 42.Hengel KMO, Bosmans JE, Van Dongen JM, Bongers PM, Van der Beek AJ, Blatter BM. Prevention program at construction worksites aimed at improving health and work ability is cost-saving to the employer: results from an RCT. Am J Ind Med 2014; 57:56–68. [DOI] [PubMed] [Google Scholar]
- 43.van der Meer EW, van Dongen JM, Boot CR, van der Gulden JW, Bosmans JE, Anema JR. Economic evaluation of a multifaceted implementation strategy for the prevention of hand eczema among healthcare workers in comparison with a control group: the Hands4U study. Acta Derm Venereol 2016; 96:499–504. [DOI] [PubMed] [Google Scholar]
- 44.Watson H, Godfrey C, McFadyen A, McArthur K, Stevenson M, Holloway A. Screening and brief intervention delivery in the workplace to reduce alcohol-related harm: a pilot randomized controlled trial. Int J Nurs Stud 2015; 52:39–48. [DOI] [PubMed] [Google Scholar]
- 45.Evans-Lacko S, Koeser L, Knapp M, Longhitano C, Zohar J, Kuhn K. Evaluating the economic impact of screening and treatment for depression in the workplace. Eur Neuropsychopharmacol 2016; 26:1004–1013. [DOI] [PubMed] [Google Scholar]
- 46.Odeen M, Magnussen LH, Maeland S, Larun L, Eriksen HR, Tveito TH. Systematic review of active workplace interventions to reduce sickness absence. Occup Med (Lond) 2013; 63:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pohling R, Buruck G, Jungbauer KL, Leiter MP. Work-related factors of presenteeism: the mediating role of mental and physical health. J Occup Health Psychol 2016; 21:220–234. [DOI] [PubMed] [Google Scholar]
- 48.Stansfeld S, Candy B. Psychosocial work environment and mental health: a meta-analytic review. Scand J Work Environ Health 2006; 32:443–462. [DOI] [PubMed] [Google Scholar]
- 49.Montano D, Hoven H, Siegrist J. Effects of organisational-level interventions at work on employees’ health: a systematic review. BMC Public Health 2014; 14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Biron C, Karanika-Murray M, Coope C. Improving Organizational Interventions for Stress and Well-being: Addressing Process and Context. London: Routledge; 2012. [Google Scholar]
- 51.Martinsson C, L-KM, Kwak L, Bergström G, Hellman T. What incentives influence employers to engage in workplace health interventions? BMC Public Health 2016; 16:854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rivero-Arias O, Jowett S, de Weerd M. Rivero-Arias O. Basic principles of economic evaluation of occupational health and safety interventions. Current Topics in Occupational Epidemiology. Oxford: Oxford University Press; 2013. 237–251. [Google Scholar]
- 53.Drummond N, Sculpher MJ, Claxton K, Stoddark GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. 4 ed.Oxford, UK: Oxford University Press; 2015. [Google Scholar]
- 54.Hasle P, Limborg HJ. A review of the literature on preventive occupational health and safety activities in small enterprises. Ind Health 2006; 44:6–12. [DOI] [PubMed] [Google Scholar]
- 55.Martin A, Sanderson K, Scott J, Brough P. Promoting mental health in small-medium enterprises: an evaluation of the “Business in Mind” program. BMC Public Health 2009; 9:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Niven KJ. A review of the application of health economics to health and safety in healthcare. Health Policy 2002; 61:291–304. [DOI] [PubMed] [Google Scholar]
- 57.Hoch JS, Dewa CS. Advantages of the net benefit regression framework for economic evaluations of interventions in the workplace: a case study of the cost-effectiveness of a collaborative mental health care program for people receiving short-term disability benefits for psychiatric disorders. J Occup Environ Med 2014; 56:441–445. [DOI] [PubMed] [Google Scholar]
- 58.Tompa E, Verbeek J, van Tulder M, de Boer A. Developing guidelines for good practice in the economic evaluation of occupational safety and health interventions. Scand J Work Environ Health 2010; 36:313–318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


