Abstract
Background and Objectives
Management of postoperative pain after laparoscopic segmental colonic resections remains controversial. We compared 2 methods of analgesia within an Enhanced Recovery After Surgery (ERAS) program. The goal of the study was to investigate whether administration of intrathecal bupivacaine/morphine would lead to an enhanced recovery.
Methods
A single-center, randomized, double-blind controlled trial was performed (NL43488.101.13). Patients scheduled for laparoscopic segmental intestinal resections were considered. Exclusion criteria were patients in whom contraindications to spinal anesthesia were present, conversion to open surgery, and gastric and rectal surgery. The intervention group received single-shot intrathecal bupivacaine/morphine (12.5 mg/300 μg), with an altered dose for older patients. The control group received a sham procedure and a bolus of piritramide (0.1 mg/kg). Both groups received standardized general anesthesia and a patient-controlled intravenous analgesia pump as postoperative analgesia. All patients were treated according to an ERAS protocol. A decrease in days to “fit for discharge” was the primary outcome.
Results
Fifty-six patients were enrolled. Intervention group patients were fit for discharge earlier (median of 3 vs 4 days, P = 0.044). Furthermore, there was a significant decrease in opioid use and lower pain scores on the first postoperative day in the intervention group. There were no differences in adverse events (except for more pruritus), time to mobilization, fluid administration, or patient satisfaction.
Conclusions
This randomized controlled trial shows that intrathecal morphine is a more effective method of postoperative analgesia in laparoscopic surgery than intravenous opioids within an ERAS program. Recovery is faster and less painful with intrathecal morphine. Other studies have confirmed these results, although data on faster recovery are new and require confirmation in future trials.
Clinical Trial Registration
This study was registered at ClinicalTrials.gov, identifier NCT02284282.
Enhanced Recovery After Surgery (ERAS) programs have changed postoperative management for abdominal surgery in the past decade. One of the recommendations in an ERAS protocol for colorectal surgery is to limit opioid use via administration of multimodal analgesics, including regional anesthesia techniques.1 Thoracic epidural analgesia is recommended for open surgery; however, its use in laparoscopic surgery is associated with a prolonged length of hospital stay due to delayed mobilization.2,3
Pain after laparoscopic surgery is intense, but relatively short-lived when compared with open surgery, and the analgesia should be tailored accordingly.4 Two common methods for postoperative analgesia in laparoscopic surgery are systemic opioids per requisite (eg, patient-controlled intravenous analgesia [PCIA]) or intrathecal morphine.2,5,6 The benefit of intrathecal morphine is limited systemic uptake due to its hydrophilic properties and thus a minor effect on bowel motility. Proclaimed disadvantages include the risk of an intrathecal injection, pruritus, and delayed respiratory depression.7,8 However, when a low dose of morphine is used, there seems to be no more respiratory depression than with systemic opioids.7 Patient-controlled intravenous analgesia has the benefit that the dose of opioids is matched to the patient's need, although its analgesic effect is limited by the patient's understanding and the adverse effects of the opioid.9,10
Previous studies on laparoscopic colonic resections have shown a decrease in systemic opioid use with an increase of quality of analgesia for intrathecal morphine when compared with PCIA.2,5,6 However, recovery was measured only as length of hospital stay, and recovery protocols were not standardized. We therefore designed a confirmation trial with a few methodological adaptations in an existing ERAS program to investigate whether intrathecal bupivacaine and morphine can increase the speed of recovery after laparoscopic colonic resections. These adaptations include higher intrathecal morphine dose, similar postoperative analgesia, fluid-restrictive management rather than goal-directed fluid management, predefined “fit for discharge” (FFD) criteria, and a longer follow-up period. We hypothesized that intrathecal bupivacaine and morphine would enhance the speed of recovery by decreasing systemic opioid utilization and concomitant systemic adverse effects.
METHODS
Study Design
The SALMON study (SpinAL MOrphiNe) was an investigator-initiated, single-center, randomized trial performed in a large teaching hospital. The study was approved by the ethics committee of Maasstad Hospital (Toetsingscommissie Wetenschappelijk Onderzoek Rotterdam, the Netherlands, NL43488.101.13) and CCMO (Dutch abbreviation for Central Committee on Research Involving Human Subjects). Patients provided written informed consent before enrollment. The study was registered as NCT02284282 at ClinicalTrials.gov on November 6, 2014, and as NTR4870 at trialregister.nl on October 29, 2014. This article adheres to the applicable EQUATOR guidelines.
Participants
All patients who were scheduled for laparoscopic gastrointestinal surgery between October 2014 and October 2016 were asked to participate. Exclusion criteria were as follows:
rectal and bariatric surgery;
contraindications to spinal anesthesia (eg, severe aortic stenosis, increased intracranial pressure, coagulation disorders);
contraindications to study medication (allergy for morphine, local anesthetics [amides], nonsteroidal anti-inflammatory drugs, paracetamol, or glomerular filtration rate <30 mL/min);
conversion to an open procedure; and
scheduled postoperative intensive care unit admission.
Patients who were considered eligible for the study were informed on the preoperative screening unit with written and oral information. Within a week, the patients were called for further explanation and definitive inclusion. After inclusion of 2 patients for gastric resection, we concluded that this type of surgery has a different recovery profile than segmental colonic resections, and we eliminated them from analysis.
Randomization, Allocation, and Blinding
Randomization was conducted by using sealed, opaque envelopes. An independent colleague randomized these envelopes in blocks of 6 with a ratio of 1:1. These envelopes were stacked and stored. The upper envelope was taken by the attending anesthesiologist when an included patient arrived on the preparation ward. The patient, the surgical team, the nurses on the ward, and the researchers were all blinded. Only the attending anesthesiology team and the nurse on the recovery ward were aware of the randomization, in case there was an emergency. They were instructed not to tell the patient in which group he/she was allocated.
Study Protocol
All patients were prepared according to the ERAS protocol, consisting of a carbohydrate drink the night before surgery and no bowel preparation; 1000 mg intravenous (IV) cefazolin was administered 30 minutes before surgery. No sedative premedication was given.
In the operation theater, the patients received standard monitoring (pulse oximetry, 3-lead electrocardiogram, automatic noninvasive blood pressure measurements every 3 minutes). After the time-out procedure, the surgical team left the theater for blinding.
According to the envelope, the patient received either an intrathecal injection of bupivacaine/morphine or a sham procedure. In both cases, the patient was placed in an upright sitting position, and the skin over the lumbar region of the back was cleaned with chlorhexidine, and sterile drapes were placed.
For the intrathecal injection, the skin was infiltrated with 3 mL of lidocaine 1%. A sterile 27-gauge pencil-point needle (Pencan; Braun Melsungen AG, Melsungen, Germany) was used to enter the intrathecal space at the L2–3 or L3–4 interspace. After obtaining cerebrospinal fluid, medication was administered through a single injection; 12.5 mg isobaric bupivacaine and 300 μg morphine in 5 mL were administered when the age of the patient was younger than 76 years, and 10 mg isobaric bupivacaine and 240 μg morphine in 4 mL were given when the age was older than 75 years.
For the sham procedure, the skin was infiltrated with 3 mL of lidocaine 1%. After this, the anesthesiologist pressed on the skin with a finger and talked as if he/she gave an intrathecal injection. The patients who were randomized to the control group received 0.1 mg/kg piritramide intravenously during surgery, which was common practice in our hospital.
Standardized general anesthesia was administered immediately after the puncture. After preoxygenation, 0.4 μg/kg sufentanil, 2 mg/kg propofol, and 0.6 mg/kg of rocuronium were administered, and the trachea was intubated. Sterile drapes were placed after positioning of the patient, and the surgery was started as soon as possible. Pneumoperitoneum was installed by needle insufflation through a small periumbilical incision with an insufflation pressure of 14 mm Hg and changed at the discretion of the surgeon.
Standard IV medication of 1000 mg paracetamol, 1000 mg metamizol, 0.625 mg droperidol, and 4 mg ondansetron were given before the end of surgery. Ten micrograms of IV sufentanil was administered when an increase in heart rate or blood pressure of greater than 10% occurred compared with a stable phase during surgery. Ten milligrams of IV rocuronium was administered when ventilator dyssynchronization or abdominal wall contraction occurred that remained after 10 μg IV sufentanil. Vasoactive medication was given at the discretion of the executive anesthesiologist (ie, phenylephrine, ephedrine, and norepinephrine). Every patient received an IV drip with 500 mL lactated Ringer's solution to keep an open IV line, and the targeted fluid balance was less than +750 mL. Blood loss was compensated with a blood transfusion according to the Dutch national guidelines, maintaining the hemoglobin level between 6.4 and 9.4 g/dL or Voluven (HES 130/0.4 [6%]; Fresenius Kabi, Bad Homburg, Germany) in a 1:1 manner, at the discretion of the anesthesiologist.
After completion of surgery, patients were allowed to wake up and were extubated in the operation theater. Nasogastric tubes were removed. A train-of-4 measurement was done in order to exclude residual relaxation. If necessary, rocuronium was antagonized with atropine/neostigmine or sugammadex at the discretion of the anesthesiologist.
Standard monitoring continued in the recovery ward. Pain scores (on a numerical rating scale [NRS]) were noted at admission to and discharge from the recovery ward and regularly at a 10-minute interval by the recovery nurse; 2.5 mg piritramide IV was administered when the patient reported an NRS of greater than 4 and repeated every 10 minutes if necessary. Nausea was treated with a repeated dose of 0.625 mg IV droperidol Intravenous propofol 30 mg was available for complaints of pruritus. Discharge from the recovery unit to the ward was allowed when the patient was hemodynamically and respiratory stable, reported an NRS of less than 4, and had a Glasgow Coma Scale score of greater than 14. All patients received 2 L of oxygen per minute by nasal cannula. Paracetamol 1000 mg 4 times a day, metamizol 1000 mg 4 times a day, and piritramide by PCIA system were prescribed as postoperative analgesic management. The PCIA was set up to give 1 mg of piritramide per bolus with a lockout time of 6 minutes. The PCIA system was stopped on the second postoperative day. Four milligrams of ondansetron per requisite was available for nausea, and 1 mg clemastine per requisite was available for pruritus. All patients received daily macrogol 13.7 g as a laxative.
An ERAS protocol has been fully functional for multiple years on the ward. It consisted of early enteral feeding (eg, drinks immediately on arrival on the ward, a small meal on the night of surgery), early mobilization, and removal of the urinary catheter the day after surgery.
Data Collection
Baseline characteristics and laboratory results were noted from the patient data file. The anesthesia team was asked to fill in a case record form during the surgery and the recovery phase. The patients were asked to fill in a questionnaire 3 times a day regarding pain scores (NRS 0–10), nausea (yes/no), pruritus (yes/no), drowsiness (yes/no), and satisfaction regarding pain management (0–3, where 0 is “very unsatisfied,” and 3 is “very satisfied”). They were also asked to note the time for first drinks, first food, first full meal, first mobilization, first flatus, and first bowel movement. This was then converted to hours after discharge from the recovery room, which was T = 0. An anesthetic nurse visited the patient daily for a reminder of the questionnaire and for checking and explaining the pain medication. The PCIA system was electronically checked for demands and delivered boluses.
Outcomes
Primary outcome was the number of days until FFD since the day of the surgery (which is day 0). Fit for discharge was defined as a patient who
was taking only oral pain medication,
was able to walk around in the room independently,
was tolerating a full oral diet and had bowel movements,
was hemodynamic and respiratory stable, and
had no drains or urinary catheters in situ.
Patients were checked for the criteria once a day during morning rounds. This assessment continued during the admission, even if the patient was FFD earlier.
Secondary outcomes included use of piritramide per PCIA in milligrams, patient satisfaction, pain scores and occurrence of adverse effects, difficulty of surgery, laboratory results, and adverse events.
Definitions
Time of surgery was defined as the time between start of pneumoperitoneum and the start of emergence of anesthesia. The time on the recovery ward was defined as the time between arrival and the call to the ward for picking up the patient. A conversion of surgical approach was defined as an unforeseen change in incision. An ileus was defined as an insertion of a draining nasogastric tube and nothing by mouth lasting more than 24 hours. An anastomotic leakage was defined as an intra-abdominal infection that required surgery or percutaneous drainage.
Statistical Analysis
A power analysis showed that we needed 46 subjects in order to detect a difference in FFD from 5 ± 1 day to 4 ± 1 day with a 2-sided power of 90% and P = 0.05. We suspected a 20% loss to follow-up, for which we added 10 patients. Therefore, we needed a minimum of 56 patients, which we set to n = 60. The values we used were in accordance with previous studies.11,12
We performed a per-protocol analysis. Data are described in median (interquartile range) (range). Comparisons for non–normally distributed outcomes were made by a Mann-Whitney U test. For ordinal data, a Fisher exact test was used. P = 0.05 was considered statistically significant. Values were calculated with SPSS version 21.0 (IBM, Armonk, New York), and graphics were made by GraphPad Prism version 7.1 (GraphPad Software, San Diego, California).
RESULTS
Sixty patients were randomized. Two patients who were randomized into the intervention group were treated as a control because in 1 patient the study medication was unavailable and a misconception occurred in the other patient. Because we performed a per-protocol analysis, these patients were analyzed as a control group. Two other patients in the control group were converted to an open procedure because of adhesions and were excluded from analysis. Patients with gastric resections (n = 2) were excluded from analysis (see Methods). A flowchart is presented in Figure 1.
FIGURE 1.
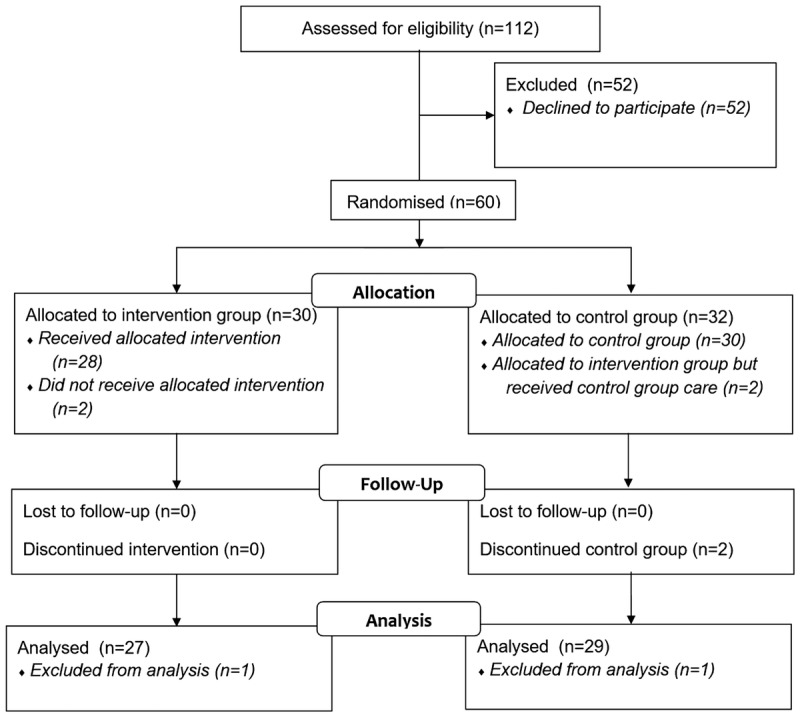
Flowchart of inclusion. See text for specifications.
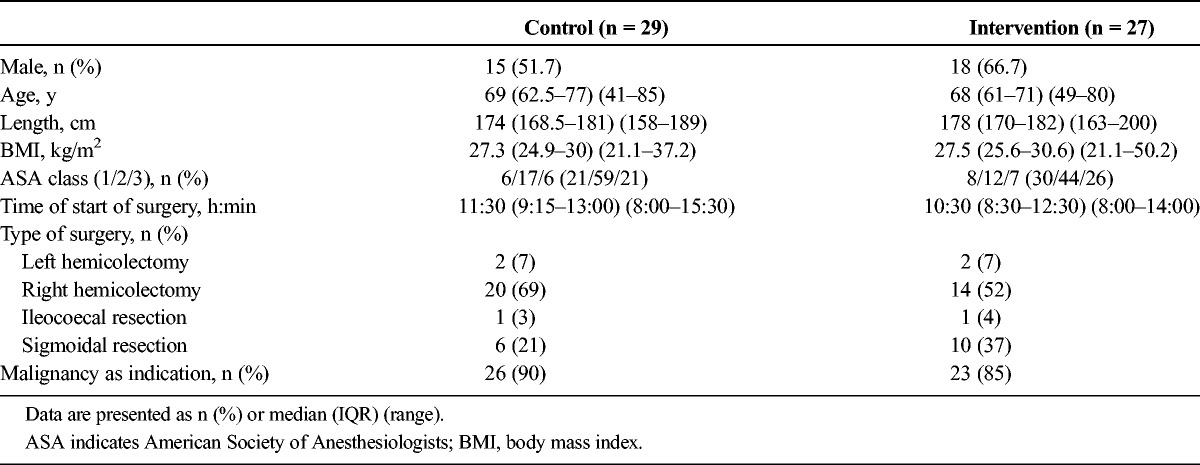
Baseline characteristics are presented in Table 1. There were more sigmoidal resections in the intervention group, whereas there were more right-sided hemicolectomies in the control group. Age and comorbidities were nonsignificantly different. For the intervention group, all attempts for intrathecal injection succeeded, because cerebrospinal fluid was obtained in all patients.
TABLE 1.
Baseline Characteristics
Primary Outcome Parameters
Patients in the intervention group were FFD earlier than patients in the control group (median, 3 [3–4] [1–28] vs 4 [3–5] [2–25] days; P = 0.044). After 3 days, 16 patients (59%) in the intervention group versus 10 patients (34%) were FFD (Fig. 2), P = 0.056. No difference was detected for actual length of stay (median, 4 [4–6] [1–33] vs 5 [4–7] [2–26] days; P = 0.270). No regression to “not FFD” occurred in any patient when scored as being FFD. Also, no readmissions occurred within 30 days after discharge.
FIGURE 2.
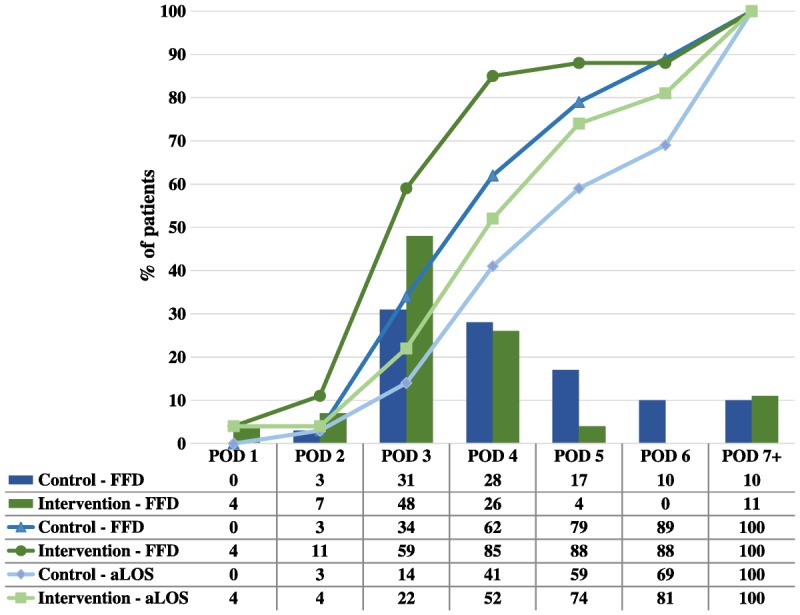
Patients in the intervention group were earlier FFD (4 [3–5] [2–25] vs 3 [3–4] [1–28] days; P = 0.044). The bars in the chart correspond to the upper 2 rows in the table and represent the percentage of patients who met the FFD criteria per day. The dark lines represent the cumulative percentage of patients who met the FFD criteria, and the light lines represent the cumulative percentage of the aLOS. These lines correspond to the middle 2 and the lower 2 rows in the table, respectively. The table displays the percentages in a numeric fashion. aLOS indicates actual length of stay; POD, postoperative day.
Secondary Outcome Parameters
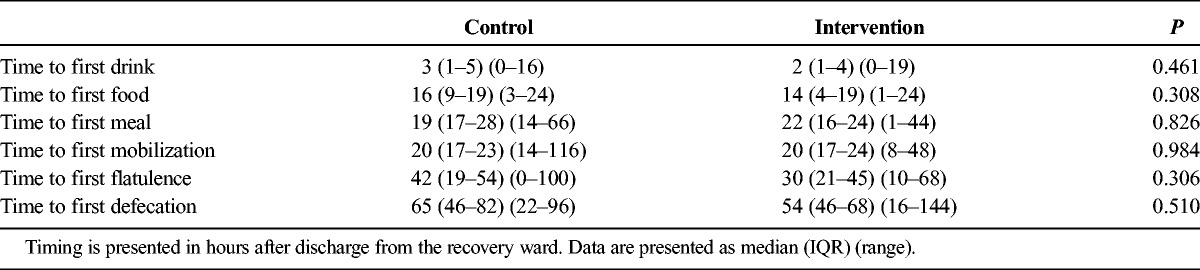
All patients were treated according to an ERAS protocol. No difference was detected in time to first drinks, foods, meals, mobilization, flatus, or defecation (Table 2).
TABLE 2.
Indicators of ERAS Adherence
Pain scores were lower in the intervention group on the first postoperative day, as indicated by lower NRS scores (Table 3). This effect was despite a lower opioid use per PCIA in the intervention group. The difference in use of PCIA lasted for the first 20 hours after surgery (Fig. 3). The difference in opioid use occurred in the first 20 hours, which led to a difference in piritramide dose of 9 mg (3–17 mg) (0–36 mg) versus 33 mg (26–61 mg) (13–112 mg), P < 0.001. The difference was 15 mg (4–25 mg) (0–60 mg) versus 44 mg (33–77 mg) (14–127 mg), P < 0.001, after 48 hours. Only 5 patients used additional opioids (10 mg long-acting oxycodone by mouth) when the PCIA pump was removed: 1 patient (4%) in the intervention group compared with 4 (14%, no difference, P = 0.353) in the control group.
TABLE 3.
Patients' Self-reported Scores
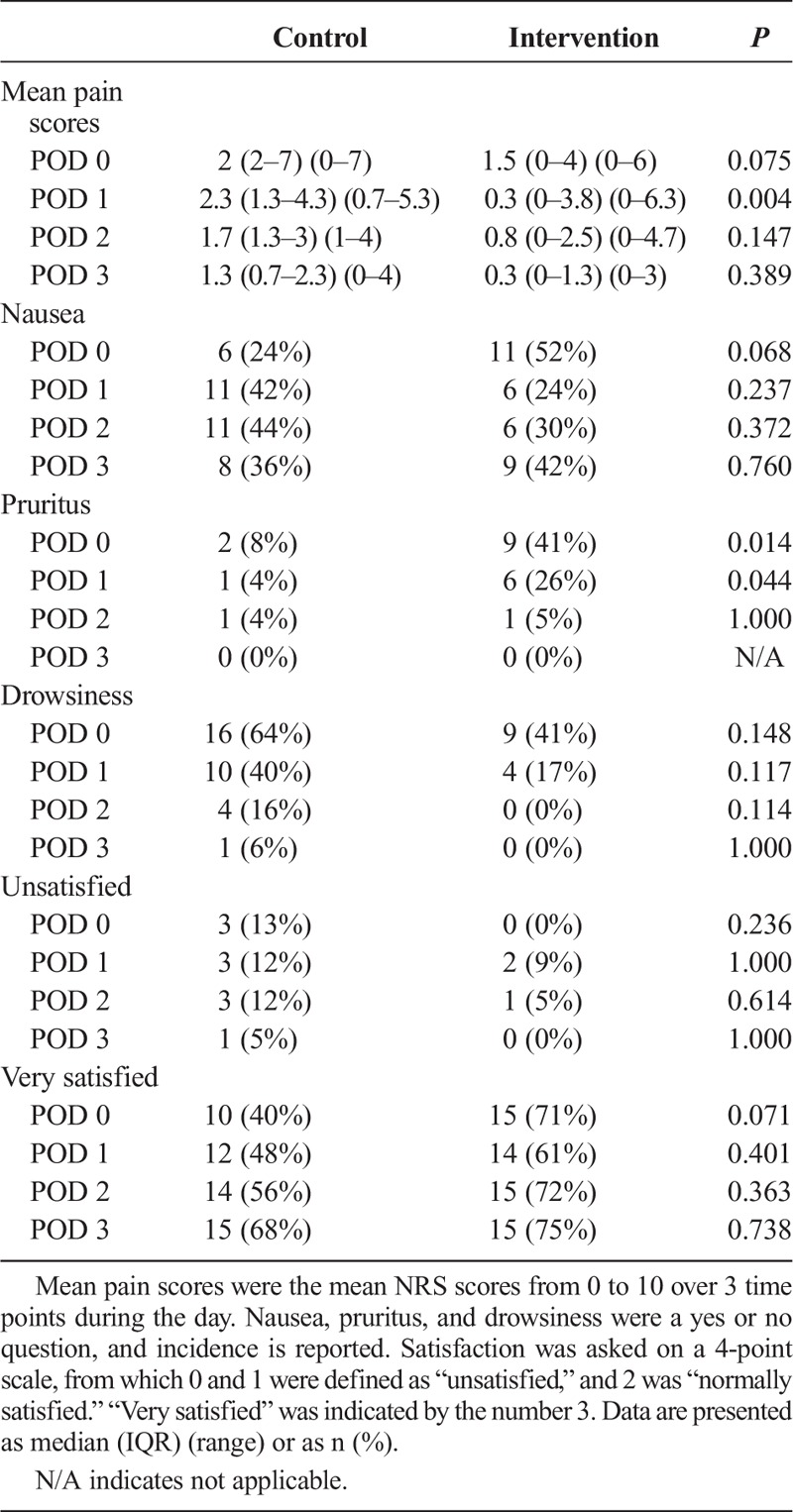
FIGURE 3.
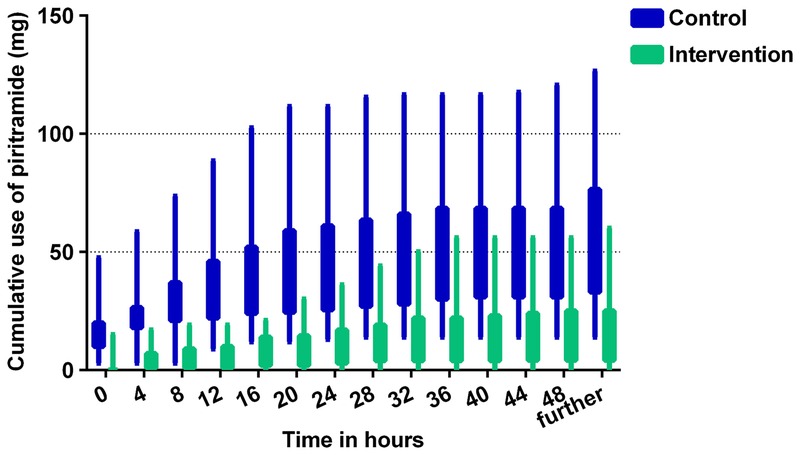
Cumulative use of piritramide per PCIA.
Patients in the intervention group received less intraoperative sufentanil (30 [25–35] [15–50] vs 45 [35–50] [20–75] μg, P < 0.001), had lower pain scores upon arrival on the recovery (0 [0–3] [0–6] vs 4 [1–6] [0–9], P = 0.001), and had less pain by discharge to the ward (0 [0–2] [0–3] vs 3 [2–4] [0–4], P < 0.001). No difference was detected in difficulty for the surgeon, duration of surgery, duration on the recovery ward, blood loss, or fluid administration.
Residual sensory block was tested in all intervention patients and was detected below a median of Th10 (Th7–Th12) (none–L2). No motoric blockade could be detected in any intervention patient.
More patients with intrathecal morphine had pruritus than the control group (41% vs 8%, P = 0.001), although solely on the first day (Table 3). Interestingly, none of the patients asked for treatment of the pruritus. There was no difference detected in nausea, drowsiness, or adverse events.
One patient in the control group died on the eighth postoperative day because of septic shock. The focus for shock was most likely to be an abdominal focus, although an autopsy was not performed. Two patients in the control group were converted to an open procedure. An ileus occurred in 3 patients (11%) in the intervention group versus 5 patients (17%) in the control group (nonsignificant), and in both groups, there was 1 patient with anastomotic leakage. Other nonanastomotic leakage infections occurred in 3 patients (10%) in the control group versus 2 patients (7%) of the intervention group (nonsignificant). There were 3 other minor complications in the control group (severe pain requiring rescue medication [n = 1], exacerbation chronic obstructive pulmonary disease [n = 1], and severe hypokalemia [n = 1]), whereas no other complications were noted in the intervention group.
No statistically significant differences were found between groups regarding patient satisfaction, even though a trend was observed on the day of surgery (40% vs 71% were very satisfied with the analgesia, P = 0.071, and 13% vs 0% were unsatisfied regarding pain control, P = 0.236) (Table 3).
DISCUSSION
This study shows that a single intrathecal injection of bupivacaine/morphine when compared with patients on systemic opioids leads to a faster recovery in a laparoscopic surgery enhanced recovery protocol. Less PCIA opioids were used in the first 20 hours after laparoscopic surgery, and patients reported lower pain scores with intrathecal morphine. There was a higher incidence of pruritus. Our study was unable to detect a difference in patient satisfaction.
The faster recovery is displayed in the fact that patients were FFD earlier. We believe that meeting the FFD criteria reflects recovery better than the length of stay, because the latter is also influenced by social or nonmedical decisions (eg, no place available in the nursing home, discharge preferred during workdays). Our FFD criteria were in accordance with international consensus.13
The reason for the faster recovery is unclear, because both groups had similar adherence to the ERAS protocol. The difference in faster recovery could be explained by the preoperative fitness, although there are no signs that differences in preoperative fitness played a role, because the groups were well randomized in other aspects. However, the use of systemic opioids and the pain scores were lower in the intervention group, which could lead to a difference in the extent of mobilization or enteral feeding. For example, first mobilization could have been 5 steps in the room or a walk to the coffee machine in the hall. Unfortunately, this was not measured.
Our results differ from the study of Wongyingsinn et al,6 which did not find a faster recovery. That study measured the actual length of hospital stay instead of FFD criteria, with the aforementioned limitations. Furthermore, different postoperative regimens for analgesia were used (PCIA vs oral oxycodone), and a different dose of intrathecal morphine was used. Still, the recovery profile was deemed very comparable in regard to pain scores, opioid use, and duration of intense pain.
A large variance in PCIA use was observed in the control group, whereas in the intervention group the variance was less. Still a substantial amount of systemic piritramide was saved in the intervention group during the first 20 hours, which indicates the effect of a single shot of intrathecal morphine. Moreover, pain scores were lower in the intervention group, despite the same availability of PCIA piritramide. This indicates that even though PCIA is used, patients still have room left for lowering the pain scores. Explanations for this observation are either the patient does not need a lower pain score or the PCIA is unable to achieve lower pain scores because of patient knowledge gaps, inadequate medication or settings of the PCIA, or occurrence of adverse effects. Unfortunately, this study was not set up to investigate this.
Pain scores and PCIA piritramide use were similar after the first day, indicating that either the effect of intrathecal morphine or the pain of laparoscopic surgery has worn off.14,15 In both groups, only small amounts of opioids were used after the first day, and no rebound pain was observed during the follow-up period. These facts suggest that the duration of analgesia of intrathecal morphine is appropriate to cover the pain for this type of surgery.
Appropriate analgesia without serious adverse effects and delaying recovery is the primary goal of analgesia in the ERAS program.1 In this study, this dose proved to provide appropriate analgesia during the first 24 hours. Furthermore, apart from pruritus, neither significant adverse effects nor any adverse events were observed, although the number of patients may be too low for detection. The dose of 300 μg of morphine was chosen based on a meta-analysis and a review.7,16 To our knowledge, a dose-finding study of intrathecal morphine for laparoscopic surgery has not been published.
Ten to 12.5 mg of bupivacaine was added to enhance intraoperative analgesia, and its effect is displayed in the lower intraoperative sufentanil use. It could also have contributed to the lower pain scores on the recovery ward. A preemptive analgesic effect might be involved as well, although there are no data available to support this claim. However, because we observed no adverse events related to bupivacaine (eg, prolonged motor blockade or sympatholysis), we would recommend adding bupivacaine to the intrathecal mixture.17 Common doses of vasopressors were used in this study, and a fluid-restrictive management was still achieved in both groups, without a significant difference between groups.
The intervention group suffered from a higher incidence of pruritus, despite the use of prophylactic measures.7,18–20 Interestingly, patients did not ask for medication to treat the pruritus, even though it was available and prescribed on demand for them. A trend toward more nausea on the first day for the intervention group was observed, but this was reversed on the second postoperative day. Perhaps administration of dexamethasone at induction of anesthesia and/or prescribing 5-HT3 antagonists at standardized times rather than per requisite would alter the nausea.
A well-known adverse effect of intrathecal morphine is delayed respiratory depression.21,22 In this study, all patients received supplemental oxygen by nasal cannula, and sedatives were prohibited during the first night. None of the patients' vital signs were monitored after discharge from the recovery ward. We did not study respiratory frequency or oxygen saturation during the first night, so we cannot comment on the occurrence of a delayed respiratory depression; however, no clinically relevant consequences were observed. This observation is in line with the meta-analysis of Gehling and Tryba,7 which concluded that at less than 500 μg intrathecal morphine does not cause serious respiratory adverse events. Another meta-analysis does warn for respiratory depression, but it did not investigate whether there was a dose dependency.8 A few case reports suggest respiratory depression after intrathecal morphine with a dose lower than 500 μg, but it is not clearly related to morphine as multiple sedatives were used as well.23,24 Therefore, we prohibited sedative medication to prevent an interaction with the intrathecal morphine.
We found no difference in patient satisfaction, which indicates that both groups perceived pain levels to their expectations. Although a trend was observed, it did not reach statistical significance. We measured satisfaction on a nonvalidated 4-point scale, which could be too insensitive to measure any effect. However, in our opinion, a smaller effect is hardly clinically relevant.
This study has several strengths, which contribute to the search for a fitting method of analgesia for laparoscopic colonic resections.2,5,6,12 Its follow-up lasts for the total time of admission, the departments were used to an ERAS program, the 2 study arms received similar postoperative care, and it was a double-blind study. Unlike Levy et al,2 we did not use goal-directed fluid management, but rather we used a fluid-restricted management and early oral hydration. This was more in line with contemporary guidelines for fluid management in patients without severe cardiovascular comorbidity.25
This study has several limitations. First, we excluded the converted surgeries, so we cannot comment on the effect of intrathecal morphine on laparotomy surgery. However, it seems reasonable to assume that intrathecal morphine still has an analgesic effect after open surgery during the first day and still exerts an advantage in this setting. Second, we did not measure the magnitude of mobilization, which could be the underlying explanation for the faster recovery in the intervention group. Third, the measurement of patient satisfaction may be too insensitive, as mentioned previously. Unfortunately, we did not use a quality-of-recovery questionnaire, which is recommended by the European Society of Anaesthesiology for measuring quality of recovery. Fourth, allocation went wrong in 2 patients. Because it was a per-protocol analysis, we analyzed these patients in the control group. This mistake was due to implementation of the study in the daily work and unrelated to the patient. Furthermore, the sample size is relatively low, so a confirmatory trial is necessary, especially for the faster recovery.
In addition, we did not measure the cost-effectiveness of the intervention. The intervention will probably become cost-effective when the actual length of stay is reduced, because the costs of an admission day are higher than the intervention. Thus, additional efforts are needed to reduce the actual length of stay in order to reduce the costs.
Further research should focus on a confirmatory trial using fitness for discharge as the primary outcome, evaluating extent of mobilization as an explanation for how intrathecal morphine enhances recovery and to also clarify how the time between FFD and actual discharge can be minimized. Also, given the large variance of postoperative opioid use, investigations for which patients benefit most from this intervention should be initiated.
In conclusion, this randomized controlled trial shows that intrathecal bupivacaine/morphine provides a short-lasting analgesic effect during the first postoperative day after laparoscopic surgery. Most important, this method of analgesia leads to faster recovery, lower pain scores, and less opioid use after laparoscopic gastrointestinal surgery when compared with patients on systemic opioids. There is more pruritus in the intervention group, but no patient required treatment for this adverse effect. We recommend further research regarding intrathecal bupivacaine/morphine within an ERAS program, because recovery could be further enhanced with this method of analgesia.
ACKNOWLEDGMENTS
The authors thank the nurses and doctors of the surgery, anesthesiology, and pharmacy departments of Maasstad Hospital, Rotterdam, especially Bart de Bruijn, Alwin Nieto, Janneke Klip, Trudy Rapmund, and Cora den Ouden, who helped in the execution of the study.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37:259–284. [DOI] [PubMed] [Google Scholar]
- 2.Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg. 2011;98:1068–1078. [DOI] [PubMed] [Google Scholar]
- 3.Hubner M, Blanc C, Roulin D, Winiker M, Gander S, Demartines N. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg. 2015;261:648–653. [DOI] [PubMed] [Google Scholar]
- 4.Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118:934–944. [DOI] [PubMed] [Google Scholar]
- 5.Kong SK, Onsiong SM, Chiu WK, Li MK. Use of intrathecal morphine for postoperative pain relief after elective laparoscopic colorectal surgery. Anaesthesia. 2002;57:1168–1173. [DOI] [PubMed] [Google Scholar]
- 6.Wongyingsinn M, Baldini G, Stein B, Charlebois P, Liberman S, Carli F. Spinal analgesia for laparoscopic colonic resection using an Enhanced Recovery After Surgery programme: better analgesia, but no benefits on postoperative recovery: a randomized controlled trial. Br J Anaesth. 2012;108:850–856. [DOI] [PubMed] [Google Scholar]
- 7.Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia. 2009;64:643–651. [DOI] [PubMed] [Google Scholar]
- 8.Meylan N, Elia N, Lysakowski C, Tramer MR. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth. 2009;102:156–167. [DOI] [PubMed] [Google Scholar]
- 9.Momeni M, Crucitti M, de Kock M. Patient-controlled analgesia in the management of postoperative pain. Drugs. 2006;66:2321–2337. [DOI] [PubMed] [Google Scholar]
- 10.McNicol ED, Ferguson MC, Hudcova J. Patient controlled opioid analgesia versus non-patient controlled opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2015:CD003348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cakir H, van Stijn MF, Lopes Cardozo AM, et al. Adherence to Enhanced Recovery After Surgery and length of stay after colonic resection. Colorectal Dis. 2013;15:1019–1025. [DOI] [PubMed] [Google Scholar]
- 12.Virlos I, Clements D, Beynon J, Ratnalikar V, Khot U. Short-term outcomes with intrathecal versus epidural analgesia in laparoscopic colorectal surgery. Br J Surg. 2010;97:1401–1406. [DOI] [PubMed] [Google Scholar]
- 13.Fiore JF, Jr, Bialocerkowski A, Browning L, Faragher IG, Denehy L. Criteria to determine readiness for hospital discharge following colorectal surgery: an international consensus using the Delphi technique. Dis Colon Rectum. 2012;55:416–423. [DOI] [PubMed] [Google Scholar]
- 14.Rathmell JP, Lair TR, Nauman B. The role of intrathecal drugs in the treatment of acute pain. Anesth Analg. 2005;101:S30–S43. [DOI] [PubMed] [Google Scholar]
- 15.Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997;79:369–378. [DOI] [PubMed] [Google Scholar]
- 16.Mugabure Bujedo B. A clinical approach to neuraxial morphine for the treatment of postoperative pain. Pain Res Treat. 2012;2012:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koning MV, Teunissen AJW, van der Harst E, Stolker RJ. Combined spinal/general anaesthesia for laparoscopic colonic surgery. Anaesthesia Correspondence. Available at: http://www.respond2articles.com/ANA/forums/thread/1995.aspx. Accessed November 11, 2017.
- 18.Koju RB, Gurung BS, Dongol Y. Prophylactic administration of ondansetron in prevention of intrathecal morphine-induced pruritus and post-operative nausea and vomiting in patients undergoing caesarean section. BMC Anesthesiol. 2015;15:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen TK, Jones CA, Habib AS. Dexamethasone for the prophylaxis of postoperative nausea and vomiting associated with neuraxial morphine administration: a systematic review and meta-analysis. Anesth Analg. 2012;114:813–822. [DOI] [PubMed] [Google Scholar]
- 20.Horta ML, Morejon LC, da Cruz AW, et al. Study of the prophylactic effect of droperidol, alizapride, propofol and promethazine on spinal morphine-induced pruritus. Br J Anaesth. 2006;96:796–800. [DOI] [PubMed] [Google Scholar]
- 21.Houwelingen EV, Koning MV, Teunissen AJW, Stolker RJ. Ambiguous policies in anaesthetic pain management in laparoscopic colonic surgery: a national survey. Nederlands Tijdschr Anesthesiol. 2016;27:124–128. [Google Scholar]
- 22.Joshi GP, Bonnet F, Kehlet H. PROSPECT collaboration. Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis. 2013;15:146–155. [DOI] [PubMed] [Google Scholar]
- 23.Dworzak H, Fuss F, Buttner T. Persisting respiratory depression following intrathecal administration of morphine and simultaneous sedation with midazolam [in German]. Anaesthesist. 1999;48:639–641. [DOI] [PubMed] [Google Scholar]
- 24.Krenn H, Jellinek H, Haumer H, Oczenski W, Fitzgerald R. Naloxone-resistant respiratory depression and neurological eye symptoms after intrathecal morphine. Anesth Analg. 2000;91:432–433. [DOI] [PubMed] [Google Scholar]
- 25.Phan TD, D'Souza B, Rattray MJ, Johnston MJ, Cowie BS. A randomised controlled trial of fluid restriction compared to oesophageal Doppler-guided goal-directed fluid therapy in elective major colorectal surgery within an Enhanced Recovery After Surgery program. Anaesth Intensive Care. 2014;42:752–760. [DOI] [PubMed] [Google Scholar]


