Abstract
Rationale:
The fabella is a normal structure, but is occasionally reported to cause posterior knee pain. The aim of this study was to present fabella syndrome after high tibial osteotomy.
Patient concerns:
A 55-year-old female patient was admitted to the hospital due to about 1 year and 8 months of left knee pain. Sclerosis was observed in the anterior margin of the fabella in the preoperative magnetic resonance (MR) T2 image, and reactive bone marrow was found and was considered to be due to degeneration of the distal femur. Degenerative change (Kellgren and Lawrence—KL grade 2) of the left knee was observed, along with cartilage delamination corresponding to International Cartilage Repair Society (ICRS) grade 4 in the patellofemoral joint.
Diagnoses:
We present the first reported case of fabella syndrome in Korea, after high tibial osteotomy due to degenerative arthritis and varus deformity, rather than artificial joint surgery.
Interventions:
We excised the fabella from the patient's knee.
Outcomes:
There was no evidence of recurrence during 5 months of postoperative follow-up. Posterolateral Corner including the fabella might have sustained increased tensile force causing symptoms due to compression of the fabella by the posterior joint of the posterior femoral condyle.
Lessons:
We present the first reported case of fabella syndrome in Korea, after high tibial osteotomy due to degenerative arthritis and varus deformity, rather than artificial joint surgery. Collision syndrome caused by a fabella has previously been attributed to inconsistency of the joint surface due to excessive exercise and degenerative changes due to knee instability. We report this case since it appeared to involve collision syndrome due to mechanical change of an angular deformity.
Keywords: fabella, fabella syndrome, high tibial osteotomy
1. Introduction
The fabella is a sesamoid bone in the posterior aspect of the knee surrounded by the tendons of the external head of the gastrocnemius and can be identified as fibrocartilage or ossified sesamoid bone in simple radiographs or magnetic resonance (MR) imaging. The ratio varies depending on race and is particularly high in Asian populations. This sesamoid bone is a normal structure, but is occasionally reported to cause posterior knee pain. Collision syndrome, fracture, and paraplegia due to the fabella have been known to occur. Fabella syndrome is relatively rare both in Korea and abroad, although there have been cases of the syndrome due to collision of a posterolaterally located fabella after artificial arthroplasty.
We present the first reported case of fabella syndrome in Korea, after high tibial osteotomy due to degenerative arthritis and varus deformity, rather than artificial joint surgery.
2. Case report
A 55-year-old female patient was admitted to the hospital due to about 1 year and 8 months of left knee pain. One year six months earlier, arthroscopic partial meniscectomy of the medial meniscus and medial opening high tibial osteotomy had been performed on her left knee. Sclerosis was observed in the anterior margin of the fabella in the preoperative MR T2 image, and reactive bone marrow was found and was considered to be due to degeneration of the distal femur. Degenerative change (Kellgren and Lawrence—KL grade 2) of the left knee was observed, along with cartilage delamination corresponding to International Cartilage Repair Society (ICRS) grade 4 in the patellofemoral joint (Fig. 1).
Figure 1.
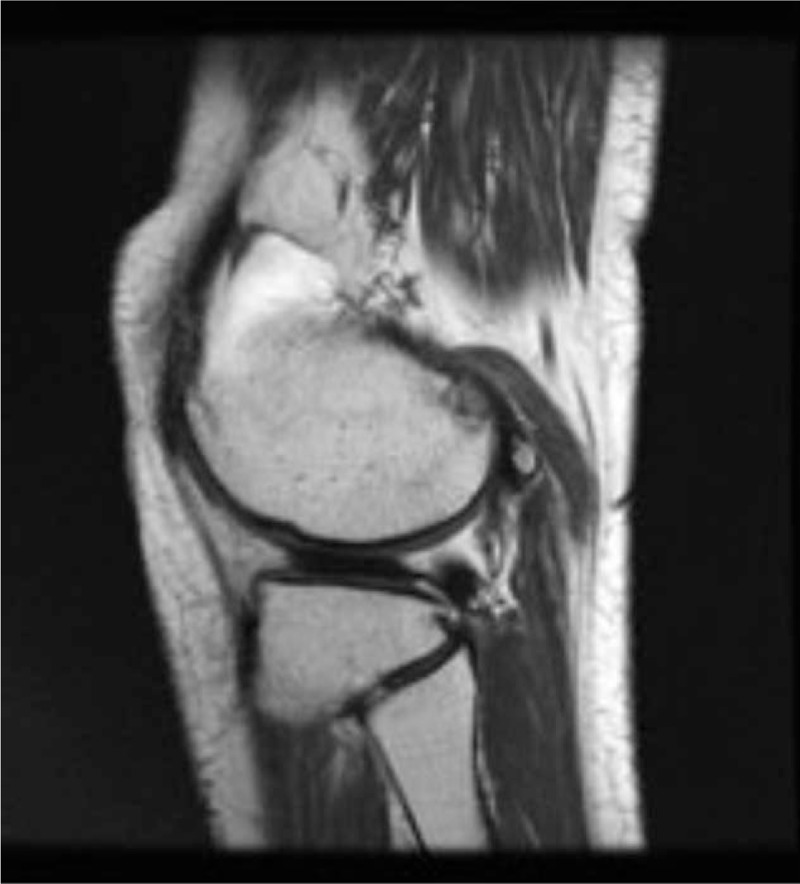
Preoperative MR T2 image.
The patient complained of postoperative pain and tenderness in the posterior aspect of the left knee. Physical examination revealed no signs of flexion contracture. However, there was a limitation of active flexion of 60° due to pain in the posterolateral aspect during flexion, and general tenderness of the posterior aspect was observed upon extension of the knee joint. Other physical examinations revealed no knee instability or other abnormal findings. Conservative treatment was performed with a topical steroid, lidocaine injections, and oral antiinflammatory medication for tenderness, but no improvement was observed.
Upon plain radiography, a 5-mm protrusion of the metal screw on the posterior aspect of the tibia was noted. The screw was removed, but there was no improvement postoperatively. Additional conservative treatment was performed, and a metal plate was surgically removed approximately 9 months after the operation, while another metal plate was removed after 1 year (Fig. 2). However, the patient continued to complain of tenderness of the posterolateral part of the knee and pain during joint movement. Subsequently, the patient reported local pain and tenderness on the lateral and posterior femur, and the tender point of the affected area could be palpated. Both preoperative and postoperative X-rays revealed a fabella on the posterior aspect of the femur, and no fracture was found. Ultrasonography confirmed that the fabella was located at the tender point (Fig. 3).
Figure 2.

Preoperative knee lateral X-ray.
Figure 3.
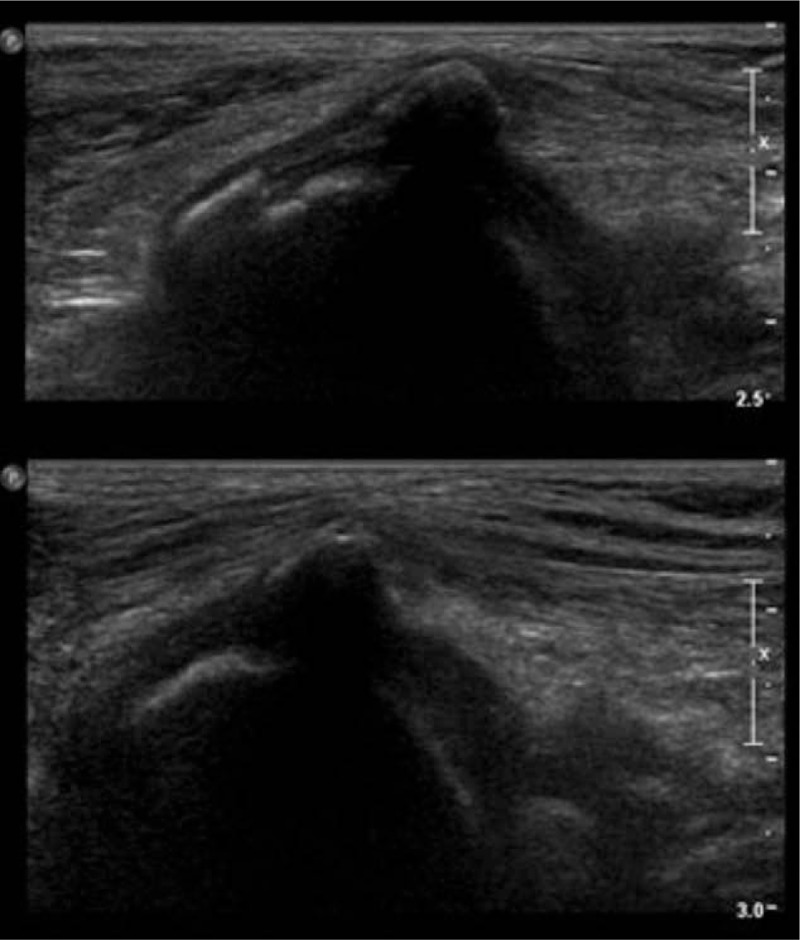
Preoperative ultrasonography.
The fabella in the lateral gastrocnemius was excised through a direct approach to the posterolateral aspect of the right knee while the patient was in the prone position (Fig. 4). After resection, the cartilage on the posterior side of femoral lateral condyle was examined, and superficial scratches or cartilage fissures were observed on the surface (Fig. 5).
Figure 4.
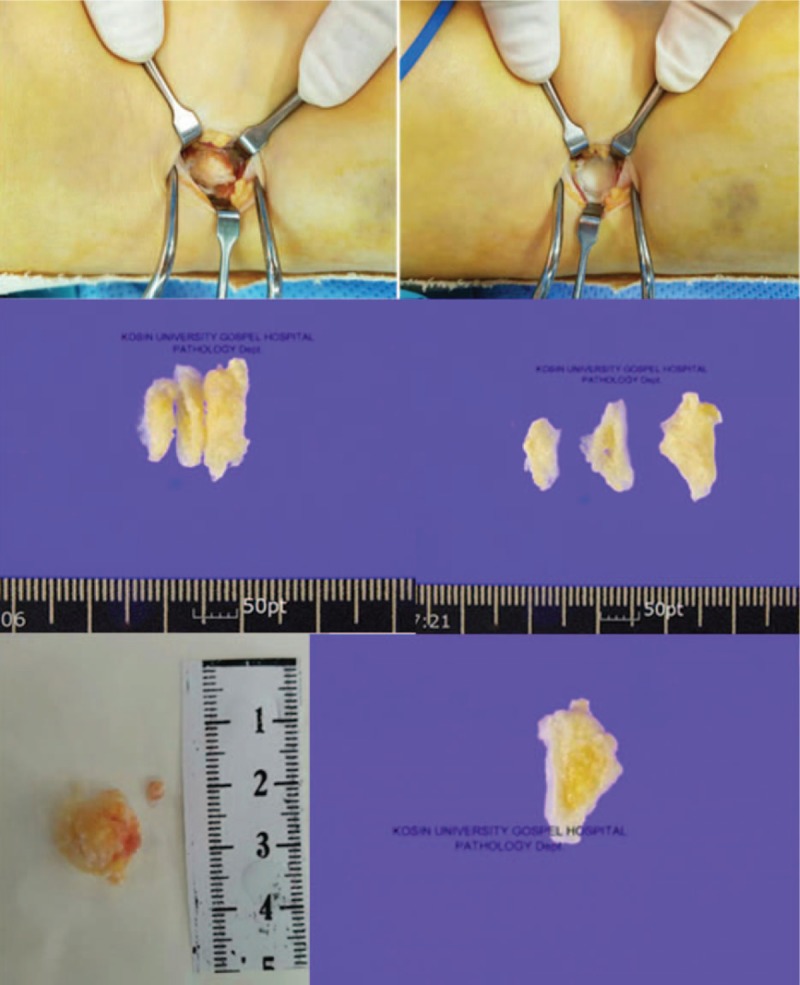
A direct approach to the posterolateral aspect of the right knee and resected tissue findings.
Figure 5.

Intraoperative clinical photo after resection.
After resection, active flexion of the knee was possible without pain in the posterolateral part of the knee, and active flexion, which was only about 60° preoperatively due to pain, was possible without any limitation up to 130°. There was no evidence of recurrence during 5 months of postoperative follow-up (Fig. 6).
Figure 6.

Preoperative and postoperative X-ray.
3. Discussion
In 10% to 30% of humans, a fabella is present in the posterolateral aspect of the knee, typically in the musculocutaneous junction of the lateral head of the gastrocnemius.[1] The fabella is adjacent to the posterior surface of the lateral femoral condyle and is either directly articulated or adjacent to the posterior aspect of the knee joint capsule. Anatomically, the fabella is embedded in the lateral head of the gastrocnemius and is the insertion site of the oblique popliteal ligament, connected to the fibular head via the fabellofibular ligament. It is also a common origin for the plantaris muscle and arcuate, forming a fabella complex on the posterolateral aspect of the knee.[2] In this anatomical position, the fabella exists at the intersection of tensile stress in the complex structure of the posterior lateral part of the knee and functions to reorient various forces as a static stabilizer (Fig. 7).
Figure 7.
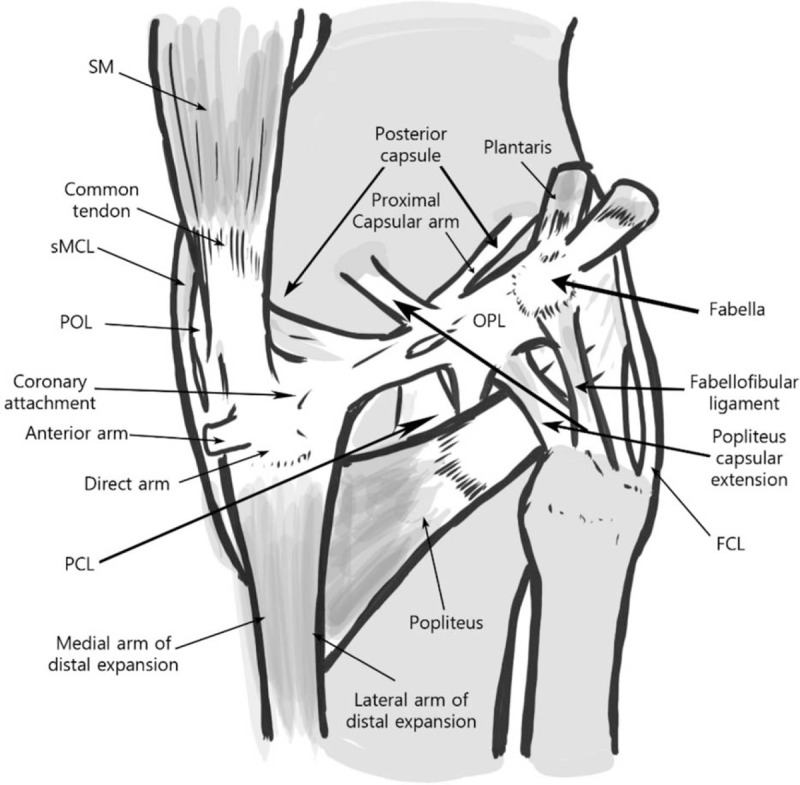
Anatomy of fabella.
It is supposed that there is a biomechanical contribution to the occurrence of the fabella. Mechanical stress and load applied to a specific posterolateral aspect of the knee joint might alter the biological developmental pathway leading to osteocartilaginous metaplasia and other genetic factors.[2]
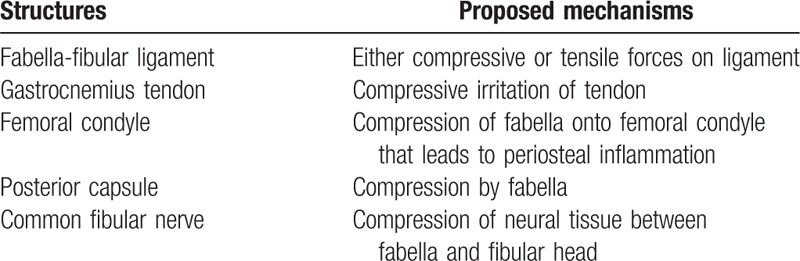
Although it is rare for the fabella to cause clinical symptoms, fabella syndrome has been reported in various clinical situations. In the presence of a fabella, knee flexion or extension can result in pain or tenderness of the posterolateral aspect, accompanied by catching, snapping, or swelling, mostly due to compression of the posterior aspect of the knee. In addition, paralysis of the total peroneal nerve due to compression between the fibular head and the fabella can occur (Table 1).
Table 1.
Structures associated with fabella.
In previously reported cases, athletes and highly active young people have experienced pain in the posterolateral aspect of the knee after intensive exercise,[3,4] and elderly patients with degenerative arthritis have experienced fabella syndrome after arthroplasty. The causes of fabella syndrome after arthroplasty include mechanical friction due to inappropriate size of the femoral component and friction between the tibial polyethylene insert and the posterior osteophyte, which was not completely removed, causing mechanical collision of the fabella.[4,5] This syndrome can be treated with arthroscopic resection, fabellectomy, or arthroscopic osteotomy.[4,6]
Theodorou et al[5] reported three cases of fabella stress fracture after total knee arthroplasty. Pain and swelling of the posterolateral aspect of the knee were noted, and the time of sesamoid bone fracture in each case varied from 4 months to 9 years after surgery. In these cases, the sustained unilateral varus deformity of the knee after surgery and unilateral varus malalignment of the insert caused a constant inward eccentric load to the knee joint, thus straining the posterolateral complex (PLC) and causing a stress fracture of the fabella via its collision with the femoral insert. In addition, Kwee et al[7] reported 2 cases of fabella fracture after total knee arthroplasty for the correction of degenerative arthritis with valgus deformity; 1 case was found immediately after surgery, and 1 case was found 45 days postoperatively. The authors posited that, when the anatomical alignment of the deformed knee was corrected, the increased tensile strength of the posterolateral structures fractured the fabella. Theoretically, as a valgus deformity is corrected relative to the anatomical axis, the tension in the fabella can increase during flexion and extension of the knee joint, and posterior articulation of the femoral lateral condyle can compress the fabella, causing symptoms of fabella syndrome.
In this reported case, we did not perform an artificial joint replacement surgery, but we performed an operation to correct a varus deformity of 8.3° to 7.5° of valgus (Fig. 8). Following a correction of about 15°, a PLC including the fabella might have sustained increased tensile force, as Kwee et al suggested, causing symptoms due to compression of the fabella by the posterior joint of the posterior femoral condyle.
Figure 8.
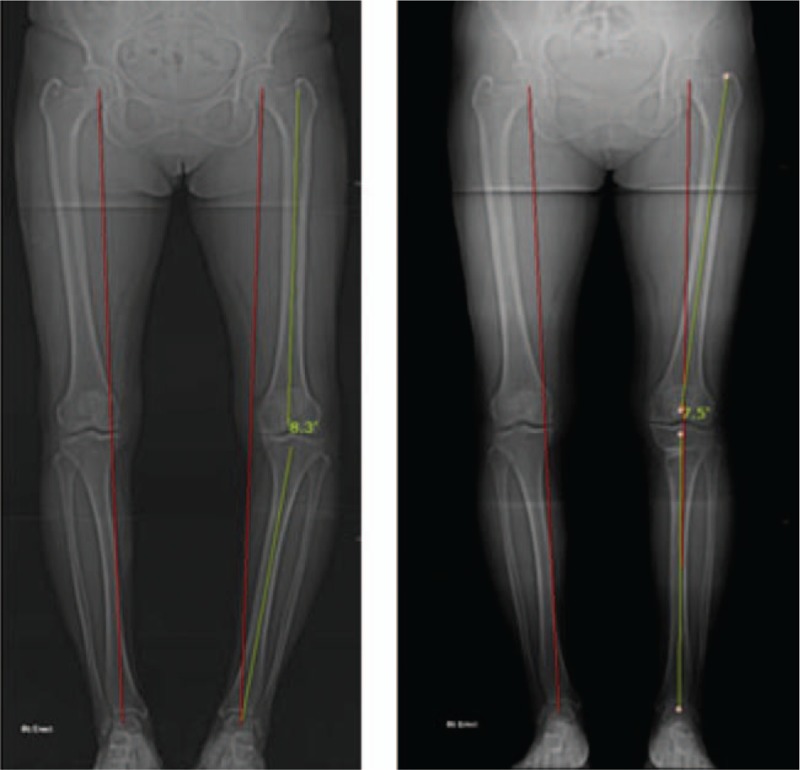
Preoperative and postoperative whole scanogram.
4. Conclusion
Collision syndrome caused by a fabella has previously been attributed to inconsistency of the joint surface due to excessive exercise and degenerative changes due to knee instability, causing knee pain.[5] There have been reports of knee pain due to artificial joint surgery, fabella syndrome, and its treatment via arthroscopic surgeries.[4,6] However, we reported this case since it appeared to involve collision syndrome due to mechanical change of an angular deformity. Excision of the fabella caused the subsidence of symptoms.
Footnotes
Abbreviations: ICRS = International Cartilage Repair Society, KL = Kellgren and Lawrence, MR = magnetic resonance.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent: For this type of study formal consent is not required.
The authors have no conflicts of interest to disclose.
References
- [1].Duncan W, Dahm DL. Clinical anatomy of the fabella. Clin Anat 2003;16:448–9. [DOI] [PubMed] [Google Scholar]
- [2].Kawashima T, Takeishi H, Yoshitomi S, et al. Anatomical study of the fabella, fabellar complex and its clinical implications. Surg Radiol Anat 2007;29:611–6. [DOI] [PubMed] [Google Scholar]
- [3].Zenteno Chávez B, Morales Chaparro IF, De La Torre IG. Fabella syndrome in a high performance runner. Case presentation and literature review. Acta Ortop Mex 2010;24:264–6. [PubMed] [Google Scholar]
- [4].Dannawi Z, Khanduja V, Vemulapalli KK, et al. Arthroscopic excision of the fabella. J Knee Surg 2007;20:299–301. [DOI] [PubMed] [Google Scholar]
- [5].Theodorou SJ, heodorou DJ, Resnick D. Painful stress fractures of the fabella in patients with total knee arthroplasty. AJR Am J Roentgenol 2005;185:1141–4. [DOI] [PubMed] [Google Scholar]
- [6].Jung UH, Chun CW, Park CS, et al. Arthroscopic treatment of fabella impingement syndrome after total knee arthroplasty—a case report. J Korean Orthop Assoc 2007;42:832–5. [Google Scholar]
- [7].Kwee TC, Heggelman B, Gaasbeek R, et al. Fabella fractures after total knee arthroplasty with correction of valgus malalignment. Case Rep Orthop 2016;2016:4749871. [DOI] [PMC free article] [PubMed] [Google Scholar]


