Abstract
Background:
It is a randomized study to compare cement penetration on x-rays after total knee arthroplasty (TKA) among 3 different ways to use tourniquets; application during the surgery, application only with implantation prosthesis and with no tourniquet use.
Methods:
A total 69 knees of 59 patients were included in the study in a quasirandom manner. Each patient had physical exams and standard radiographic evaluations at 6 weeks after the TKA procedure. Outcome evaluations included visual analog scale (VAS) scores, Knee Society Scores (KSS), blood transfusion, and drainage status after surgery for all groups. For radiographic review, the tibial plateau was divided into zones in the anterior–posterior and lateral views, according to the Knee Society Scoring System.
Results:
The average age of the patients who were eligible for the study was 65.05 (range 46–81) years. All 59 patients included in the study were female patients. Group 1 consisted of 24 patients who had TKA with use of a tourniquet during the entire operation. Group 2 consisted of 20 patients who had TKA with use of tourniquet only at the time of cementing and group 3 consisted of 25 patients with no use tourniquet. There is no significant difference in early cement penetration among the groups (group 1 2.50 mm, group 2 2.28 mm, group 3 2.27 mm; group 1 vs 2 P = .083, group 1 vs 3 P = .091, group 2 vs 3 P = .073). There is no significant difference for postoperative drainage among the 3 groups (group 1 245 mL, group 2 258.76 mL, group 3 175.88 mL; group 1 vs 2 P = .081, group 1 vs 3 P = .072, group 2 vs 3 P = .054). There was no need to transfuse more than 1 unit in any patient. The VAS score was significantly higher (group 1 3.58, group 2 1.55, group 3 1.52; group 1 vs 2 P = .022, group 1 vs 3 P = .018, group 2 vs 3 P = .062) and KSS was significantly lower in the tourniquet group (group 1 63, group 2 79, group 3 82; group 1 vs 2 P = .017, group 1 vs 3 P = .02, group 2 vs 3 P = .082).
Conclusion:
We do not suggest long-duration tourniquet use, which can lead higher pain scores and reduce functional recovery after total knee arthroplasty.
Keywords: arthroplasty, cement, knee, penetration, tourniquet
1. Introduction
Total knee arthroplasty (TKA) is the gold standard treatment in patients with primary knee osteoarthritis.[1–4] Cement penetration and the strength of the cement–bone interface in TKA is the one of most important factors in a long-term survey of implantation because the aseptic loosening is a major factor in the need for surgical revision.[5–7] Revision rates due to loosening are from 2% to 5% according to recent studies.[8]
There are many factors that affect the resistance against tensile and shear forces at the bone–implant interface.[9,10] The cement penetration depth determines the strength of the implant against shearing forces. Many studies have shown that a 4 mm penetration of the cement is required for adequate bone–cement interface resistance in TKAs.[7,11,12] Various techniques are employed by surgeons for cementation in knee arthroplasty. Also, studies are based on cementation techniques which determine the biomechanical strength of the bone–cement interface.[13–15] Furthermore, another important factor is to minimize contamination of the components by fat or blood and provide better penetration than application only to the bone surface.[16] Several studies have been conducted to determine the role of bleeding pressure on the cementing process.[17,18] Juliusson et al[19] obtained that circulating blood diminishes cement penetration into cancellous bone. Additional studies determined that blood contamination decreases viscosity of the cement, causing a reduction of penetration into the trabecular bone.[18,20] During the operation, use of a tourniquet is the most effective method for control of bleeding. Also, using a tourniquet ensures the surgeon does not need to employ bleeding control and has better visibility during the operation. However, a number of studies show that patients who have had tourniquets applied have lower functional scores due to quadriceps weakness after surgery as well as residual pain in the thigh[21–26] Huang et al[27] demonstrated that using tourniquet full time causes more excessive inflammation and muscle damage. Therefore, in recent years, orthopedic surgeons tend to perform operations without a tourniquet or only use one with a cement application.
We conducted a randomized study to compare cement penetration on x-rays after TKA among 3 different ways to use tourniquets; application during the surgery, application only with implantation prosthesis, and with no tourniquet use. We also compared additional factors such as drainage status after surgery, functional and pain scores and blood transfusion after operation which affect the knee function of patients. We wanted to investigate to see if there is a difference in cement penetration when no tourniquet is used during TKAs.
2. Material and methods
2.1. Patients
The local ethical board permission was obtained prior to the study and consent was also obtained from all patients preoperatively. Between 01/01/2015 and 01/03/2016, a total of 78 patients were diagnosed with gonarthrosis who were refractory to conservative treatment and identified as TKA candidates. Among these patients, 5 patients with secondary osteoarthritis, 3 with extreme deformity (foreseeable for extra thick bone resections or wedge usage during the surgery), and 5 patients with known cardiovascular disease were excluded from the study. From group 1 one patient and from group 2 five patients were removed from the study for being lost to follow-up at the 6th week. Remaining 69 knees of 59 patients were eligible for the study, thus they were enrolled in the study. Patients were separated to 3 groups according to the tourniquet usage. In group 1 tourniquet was used throughout the surgery, in group 2 tourniquet was used only during prosthesis implantation and in group 3 tourniquet was not used at all. Each eligible patient was assigned consecutively to one of the aforementioned 3 groups in a quasirandom manner before the surgery. Patients meeting the criteria were randomized according to the order of admission to the hospital. All surgeries were performed by the same senior surgeon using the surgical approach and prosthesis which is discussed further below.
2.2. Surgical procedure
Posterior cruciate retaining Genesis II (Smith & Nephew, Memphis, TN) cemented knee system and OrCem 3 low viscosity polymethylmetacrylate (PMMA) bone cement (European Medical Contract Manufacturing, Nijmegen, Netherlands) was used in all patients. All patients were operated under general anesthesia with propofol and desfluran. After standard mid-line skin incision and medial parapatellar approach, the distal femoral resection was in 6 of the valgus and the external rotation of the femoral cuts was determined with a plane parallel to the femoral posterior condyle by the measured resection technique. The position of the proximal tibial cut was determined using an intramedullary instrument with a 4 grade of posterior slope and 2 mm resection referenced off the medial tibial plateau, and cut surfaces were prepared with proper washing and drying. The cement was prepared in hand-mixing bowl and mixed for 1 minute. When the cement no longer adhered to the glove, we deemed it ready for use. The tibial and femoral components were precoated at the 2-minute interval with the cement, then the component was firmly impacted on the bony surface at the 5-minute interval at full knee extension and all excess cement was removed. No cement was applied directly to bony surfaces to provide standardization. After the placement of prosthesis, drain was placed at negative pressure and skin-subcutaneous closure was performed properly. In group 1, a tourniquet was used during the whole operation; in group 2 we used the tourniquet only at the time of cementing, which was applied 5 minutes before impacting the cemented component; and in group 3 no tourniquet was inflated during the surgery. The same cleaning procedure was administered in all patients. The operation room temperature and humidity were set points 20°C and 55%, respectively, for all procedures.
2.3. Outcome assessment
All patients were treated with intravenous cefazolin Na until drain is removed and applied 4000 IU low molecular weight heparin subcutaneously up to discharge. Outcome evaluations included VAS scores and KSS obtained before and at the 6th week of the surgery and cement penetration measurements obtained from the 6th week x-rays. In addition, we collected blood transfusion and drainage status after surgery (in first 24 hours) for all groups. For radiographic review, the tibial plateau was divided into zones in the anterior–posterior and lateral views, according to the Knee Society Scoring (KSS) System.[28] (Fig. 1A and B) The keel of the chosen prosthesis impaired assessment of the cement mantle penetration in some zones. Zones 1 and 4 were assessed in the anterior–posterior radiograph, and zones 1 and 2 were assessed in the lateral radiograph. Therefore, the cement mantle depth was measured in 4 zones of each tibial plateau. To prevent magnification error, the radiographic dimensions of the prosthesis were measured and compared with the real prosthesis dimensions. The radiographic findings were evaluated and independently measured by 1 orthopedic surgeon and checked by 2 other colleagues. The mean depth of cement penetration was calculated for each zone within groups 1, 2, and 3, giving 12 zones for assessment. A mean depth was also calculated for each of the 3 groups.
Figure 1.
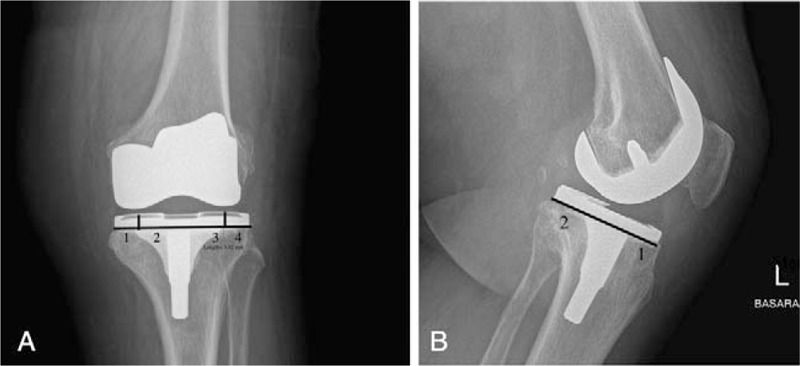
(A) Postoperative anterior–posterior views and zones, according to the Knee Society scoring system. Radiograph showing the measurement of the cement mantle thickness with the width measurement tool in the system (x-rays were scaled to 115% as standard). (B) Postoperative lateral views and zones, according to the Knee Society scoring system (x-rays were scaled to 115% as standard).
Statistical analysis was performed with SPSS software (ver. 13.0 SPSS Inc., Chicago, IL). Kolmogorov–Smirnov test was utilized to assess distribution of study parameters between groups which did not yield a normal distribution. Intergroup values comparison was done by Mann–Whitney U test. A significance value less than 0.05 was considered to be significant.
3. Results
After the removal of patients lost to follow up 69 knees of 59 patients were included in the study. The average age of patients reviewed was 65.05 (range 52–81) years. All of the cases were diagnosed as primary osteoarthritis. The effect of each tourniquet method is comparable when average cement penetration is calculated for each group.
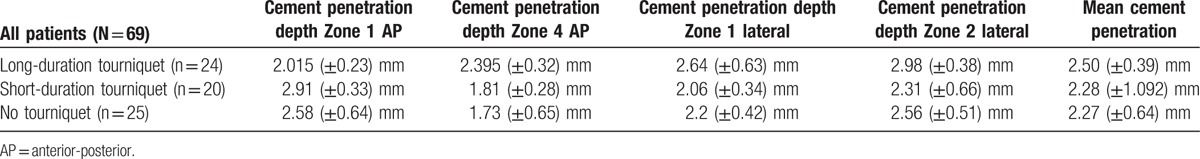
Group 1 consisted of 24 patients who had TKA with use of a tourniquet during the entire operation. Group 2 consisted of 20 patients who had TKA with use of tourniquet only at the time of cementing and group 3 consisted of 25 patients who had TKA with no use tourniquet. Four tibial zones on x-rays were assessed per patient. The mean cement penetration was 2.50 (±0.39) mm for group 1, 2.28 (± 1.09) mm for group 2 and 2.27 (±0.64) mm for group 3. There is no statistically significant difference in early cement penetration among the groups. (group 1 vs 2 P = .083, group 1 vs 3 P = .091, group 2 vs 3 P = .073). The values for each zone in all groups are shown in Table 1.
Table 1.
Values of cement penetration depth in all zones for each group.
Postoperative drainage and blood transfusion status were recorded for each group. The mean drainage was 245 (±24.6) mL in the tourniquet group, 258.76 (±32.4) mL in the no-tourniquet group and 175.88 (±40.3) mL in the tourniquet only during cementation group. There is no significant difference for postoperative drainage among the 3 groups (group 1 vs 2 P = .081, group 1 vs 3 P = .072, group 2 vs 3 P = .054). Blood transfusion was needed for only 5 patients in group 1, 4 patients in group 2 and 4 patients in group 3. There was no need to transfuse more than one unit in any patient.
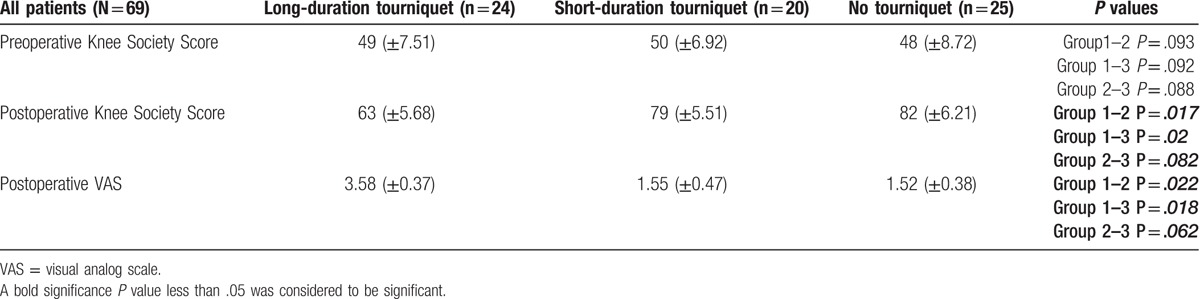
Outcome evaluation was measured by VAS score and KSS for all patients. In group 1, the mean VAS score was 3.58 (±0.37), 1.55 (±0.47) in group 2, and 1.52 (±0.38) in group 3, respectively. The VAS score was significantly higher (group 1 vs 2 P = .022, group 1 vs 3 P = .018, group 2 vs 3 P = .062) in the tourniquet group. We detected no statistically significant differences in preoperative KSS for all groups (group 1 vs 2 P = .093, group 1 vs 3 P = .092, group 2 vs 3 P = .088). But it was significantly worse in long duration tourniquet use group postoperatively (group 1 vs 2 P = .017, group 1 vs 3 P = .02, group 2 vs 3 P = .082) (Table 2). Any complication, for example implant failure, infection or vascular injury, was seen pre-and postoperatively for all patients.
Table 2.
Inpatient outcomes for all groups.
4. Discussion
Total knee arthroplasty is a successful operation for patients with end-stage arthritis in need of pain relief and improved function.[3,5] How long total knee arthroplasty lasts depends on many factors.[29] It is well known that increased initial fixation strength of the tibial component is an essential factor which influences the continued function of the implant. Therefore, cement penetration during the implantation process is of paramount importance in creating an ideal cement–bone bond and, thus, maximum fixation strength.[11,30,31] Fixation strength in cemented tibial components is reliant on a number of factors.[32] These include the depth of cement penetration and inherent bone strength. Lombardi et al[33] report that the revisions secondary to aseptic loosening are due to inadequate cement penetration. Prior studies investigated the adequate cement penetration depth, and the most well-known, Walker et al[11] suggests that the optimal depth of cement penetration is 3 to 4 mm for maximal cement–bone interface fixation. It is known that 2 to 3 mm of cement penetration is required to reach the first transverse trabeculae.[7,34] Hofmann et al[29] determined a 2.69 mm overall depth of penetration for all zones in 109 patients, and in a study by Schlegel et al[31] penetration depth ranged from 0.67 to 3.46 mm. In our study, the mean cement penetration depth was 2.35 mm, similar to other studies in the literature.
Many methods have been tested to improve cement penetration, as is seen in the literature.[35,36] Banwart et al[16] demonstrated that removing excess fluids and fat before cementing can enhance penetration. Tourniquet usage is another method which has been employed to preserve the cementation field where excessive bleeding can have an adverse effect on penetration.[37] Again, Juliusson et al[19] cemented femoral heads before and after osteotomy and found that the presence of blood circulation decreased the penetration of cement into the trabecular bone by approximately 50%. Breusch et al[20] found improved penetration into the trabecular bone when high-viscosity cement was used as compared with low viscosity cement. Miller et al[36] speculated that blood clots which interpose between the cement and bone might play a significant role in the loss of fixation and may contribute to the eventual clinical loosening of the cemented construct. In contrast, MacDonald et al[38] found greater cement penetration for standard viscosity cement when compared with high viscosity cement. Also, Miller et al[36] found similar penetration of cement into the trabecular bone when comparing standard viscosity cement with low viscosity cement. In light of all this information, it is possible that excessive bleeding, insufficient cementation time or poor pressurization can cause decreased cement penetration and strength depending on the density reduction of the cement. It was in response to these issues that we sought to determine the difference of cement penetration depth between long or short tourniquet usage times and non-usage of a tourniquet. In our study, we found no significant difference in penetration among the 3 groups in early postoperative control. Compared with the literature, there are studies showing that use of tourniquet improves cement penetration [18,25]as well as studies showing that use of tourniquet has no significant effect on cement penetration.[39,40]
This result was an important factor for us in deciding to use a tourniquet, because tourniquets are widely used during total knee arthroplasty to provide better visualization and to facilitate the cementing technique.[41,42] Moreover, tourniquet usage may reduce operating time, blood loss, and postoperative drainage, which may decrease the incidence of infection.[37,43] However, tourniquet usage may also carry certain disadvantages including thigh pain, limb swelling, nerve palsy, muscle injury, postoperative stiffness, and deep vein thrombosis.[41,43–47] Wang et al[47] determined that total blood loss was reduced with long duration tourniquet use, but short duration tourniquet use was associated with lower postoperative blood loss and would lead to faster recovery and less pain during the early rehabilitation after TKA. Also, Liu et al[41] found tourniquet use in TKA results in higher pain scores in the initial postoperative period and a reduction in quadriceps function for the first 6 months. Moreover, tourniquet usage had no effect on the prosthetic cement interface at 12 months postoperatively. Similar to these studies, in our study the VAS score was significantly higher and functional scores significantly worse in long duration tourniquet use when compared to the other groups. Additionally, there is no difference in postoperative drainage and blood transfusion requirements.
This study has limitations. Number of patients is low and the complication rates are not determined comparatively. Longer follow-up and additional functional tests are needed for better evaluation. Also it would be better to add blood loss for the patients during the surgery. We analysed only tibial component's cement mantle thickness. Additionally evaluation of femoral mantle thickness and using 3D CT scan may provide more accurate assessment. Finally, the fact that all patients are women can be a disadvantage in assessing outcomes. When researching the literature, there is a need for studies about cement penetration and strength due to tourniquet use with longer follow up so that more valuable data can be collective and assessed on this subject.
5. Conclusion
Total knee arthroplasty is a popular and useful treatment method for advanced osteoarthritis of the knee. It is necessary to avoid cementation failure that causes aseptic loosening in TKA. In the results of our study we determined no difference in cement penetration due to tourniquet use. Therefore, we do not suggest long-duration tourniquet use, which can lead higher pain scores and reduce functional recovery in the early postoperative period after total knee arthroplasty. Usually, our elective choice is cementation without tourniquet in our clinic.
6. Declaration
6.1. Ethics approval and consent to participate
Ethical board permission was given by Acibadem University (ATADEK2014-672). This study was approved by the authors’ institutional review board, and all patients gave informed consent to participate in this study. Detailed information regarding the surgical interventions was provided to all patients. All patients signed an informed consent form that thoroughly explained the operative technique and rehabilitation program that they would undergo.
Footnotes
Abbreviations: AP = anterior-posterior, CT = computerized tomography, KSS = Knee Society Score, TKA = total knee arthroplasty, VAS = visual analog scale, vs = versus.
The authors have no conflicts of interest to disclose.
References
- [1].Windsor RE, Scuderi GR, Moran MC, et al. Mechanisms of failure of the femoral and tibial components in total knee arthroplasty. Clin Orthop Relat Res 1989;248:15–9. [DOI] [PubMed] [Google Scholar]
- [2].Askew MJ, Steege JW, Lewis JL, et al. Effect of cement pressure and bone strength on polymethylmethacrylate fixation. J Orthop Res 1984;1:412–20. [DOI] [PubMed] [Google Scholar]
- [3].Parsch D, Kruger M, Moser MT, et al. Follow-up of 11-16 years after modular fixed-bearing TKA. Int Orthop 2009;33:431–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dixon MC, Brown RR, Parsch D, et al. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am 2005;87:598–603. [DOI] [PubMed] [Google Scholar]
- [5].Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am 1979;61:173–80. [PubMed] [Google Scholar]
- [6].Krause WR, Krug W, Miller J. Strength of the cement–bone interface. Clin Orthop Relat Res 1982;163:290–9. [PubMed] [Google Scholar]
- [7].Lutz MJ, Pincus PF, Whitehouse SL, et al. The effect of cement gun and cement syringe use on the tibial cement mantle in total knee arthroplasty. J Arthroplasty 2009;24:461–7. [DOI] [PubMed] [Google Scholar]
- [8].Arsoy D, Pagnano MW, Lewallen DG, et al. Aseptic tibial debonding as a cause of early failure in a modern total knee arthroplasty design. Clin Orthop Relat Res 2013;471:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bauze AJ, Costi JJ, Stavrou P, et al. Cement penetration and stiffness of the cement-bone composite in the proximal tibia in a porcine model. J Orthop Surg 2004;12:194–8. [DOI] [PubMed] [Google Scholar]
- [10].Bert JM, McShane M. Is it necessary to cement the tibial stem in cemented total knee arthroplasty? Clin Orthop Relat Res 1998;356:73–8. [DOI] [PubMed] [Google Scholar]
- [11].Walker PS, Soudry M, Ewald FC, et al. Control of cement penetration in total knee arthroplasty. Clin Orthop Relat Res 1984;185:155–64. [PubMed] [Google Scholar]
- [12].Dorr LD, Lindberg JP, Claude-Faugere M, et al. Factors influencing the intrusion of methylmethacrylate into human tibiae. Clin Orthop Relat Res 1984;183:147–52. [PubMed] [Google Scholar]
- [13].Lutz MJ, Halliday BR. Survey of current cementing techniques in total knee replacement. ANZ J Surg 2002;72:437–9. [DOI] [PubMed] [Google Scholar]
- [14].Norton MR, Eyres KS. Irrigation and suction technique to ensure reliable cement penetration for total knee arthroplasty. J Arthroplasty 2000;15:468–74. [DOI] [PubMed] [Google Scholar]
- [15].Ritter MA, Herbst SA, Keating EM, et al. Radiolucency at the bone–cement interface in total knee replacement. The effects of bone-surface preparation and cement technique. J Bone Joint Surg Am 1994;76:60–5. [DOI] [PubMed] [Google Scholar]
- [16].Banwart JC, McQueen DA, Friis EA, et al. Negative pressure intrusion cementing technique for total knee arthroplasty. J Arthroplasty 2000;15:360–7. [DOI] [PubMed] [Google Scholar]
- [17].Benjamin JB, Gie GA, Lee AJ, et al. Cementing technique and the effects of bleeding. J Bone Joint Surg Br 1987;69:620–4. [DOI] [PubMed] [Google Scholar]
- [18].Majkowski RS, Bannister GC, Miles AW. The effect of bleeding on the cement–bone interface. An experimental study. Clin Orthop Relat Res 1994;299:293–7. [PubMed] [Google Scholar]
- [19].Juliusson R, Flivik G, Nilsson J, et al. Circulating blood diminishes cement penetration into cancellous bone. In vivo studies of 21 arthrotic femoral heads. Acta Orthop Scand 1995;66:234–8. [DOI] [PubMed] [Google Scholar]
- [20].Breusch S, Heisel C, Muller J, et al. Influence of cement viscosity on cement interdigitation and venous fat content under in vivo conditions: a bilateral study of 13 sheep. Acta Orthop Scand 2002;73:409–15. [DOI] [PubMed] [Google Scholar]
- [21].Dennis DA, Kittelson AJ, Yang CC, et al. Does tourniquet use in TKA affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res 2016;474:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Huang HT, Su JY, Chang JK, et al. The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: report of a 2-year follow-up. J Arthroplasty 2007;22:1007–12. [DOI] [PubMed] [Google Scholar]
- [23].Wakai A, Winter DC, Street JT, et al. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg 2001;9:345–51. [DOI] [PubMed] [Google Scholar]
- [24].Clarke MT, Longstaff L, Edwards D, et al. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br 2001;83:40–4. [DOI] [PubMed] [Google Scholar]
- [25].Pfitzner T, von Roth P, Voerkelius N, et al. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2016;24:96–101. [DOI] [PubMed] [Google Scholar]
- [26].Rathod P, Deshmukh A, Robinson J, et al. Does tourniquet time in primary total knee arthroplasty influence clinical recovery? J Knee Surg 2015;28:335–42. [DOI] [PubMed] [Google Scholar]
- [27].Huang ZY, Pei FX, Ma J, et al. Comparison of three different tourniquet application strategies for minimally invasive total knee arthroplasty: a prospective non-randomized clinical trial. Arch Orthop Trauma Surg 2014;134:561–70. [DOI] [PubMed] [Google Scholar]
- [28].Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 1989;248:9–12. [PubMed] [Google Scholar]
- [29].Hofmann AA, Goldberg TD, Tanner AM, et al. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty 2006;21:353–7. [DOI] [PubMed] [Google Scholar]
- [30].Janssen D, Mann KA, Verdonschot N. Micro-mechanical modeling of the cement-bone interface: the effect of friction, morphology and material properties on the micromechanical response. J Biomech 2008;41:3158–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Schlegel UJ, Bishop NE, Puschel K, et al. Comparison of different cement application techniques for tibial component fixation in TKA. Int Orthop 2015;39:47–54. [DOI] [PubMed] [Google Scholar]
- [32].Peters CL, Craig MA, Mohr RA, et al. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res 2003;409:158–68. [DOI] [PubMed] [Google Scholar]
- [33].Lombardi AV, Jr, Mallory TH, Staab M, et al. Particulate debris presenting as radiographic dense masses following total knee arthroplasty. J Arthroplasty 1998;13:351–5. [DOI] [PubMed] [Google Scholar]
- [34].Walker PS, Greene D, Reilly D, et al. Fixation of tibial components of knee prostheses. J Bone Joint Surg Am 1981;63:258–67. [PubMed] [Google Scholar]
- [35].Bean DJ, Convery FR, Woo SL, et al. Regional variation in shear strength of the bone–polymethylmethacrylate interface. J Arthroplasty 1987;2:293–8. [DOI] [PubMed] [Google Scholar]
- [36].Miller MA, Race A, Gupta S, et al. The role of cement viscosity on cement-bone apposition and strength: an in vitro model with medullary bleeding. J Arthroplasty 2007;22:109–16. [DOI] [PubMed] [Google Scholar]
- [37].Tai TW, Lin CJ, Jou IM, et al. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2011;19:1121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].MacDonald W, Swarts E, Beaver R. Penetration and shear strength of cement-bone interfaces in vivo. Clin Orthop Relat Res 1993;286:283–8. [PubMed] [Google Scholar]
- [39].Molt M, Harsten A, Toksvig-Larsen S. The effect of tourniquet use on fixation quality in cemented total knee arthroplasty a prospective randomized clinical controlled RSA trial. Knee 2014;21:396–401. [DOI] [PubMed] [Google Scholar]
- [40].Vandenbussche E, Duranthon LD, Couturier M, et al. The effect of tourniquet use in total knee arthroplasty. Int Orthop 2002;26:306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Liu D, Graham D, Gillies K, et al. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Rel Res 2014;26:207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Zhang W, Liu A, Hu D, et al. Effects of the timing of tourniquet release in cemented total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res 2014;9:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hernandez AJ, Almeida AM, Favaro E, et al. The influence of tourniquet use and operative time on the incidence of deep vein thrombosis in total knee arthroplasty. Clinics 2012;67:1053–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Butt U, Ahmad R, Aspros D, et al. Factors affecting wound ooze in total knee replacement. Ann R Coll Surg Engl 2011;93:54–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Lohmann-Jensen R, Holsgaard-Larsen A, Emmeluth C, et al. The efficacy of tourniquet assisted total knee arthroplasty on patient-reported and performance-based physical function: a randomized controlled trial protocol. BMC Musculoskelet Disord 2014;15:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Tie K, Hu D, Qi Y, et al. Effects of tourniquet release on total knee arthroplasty. Orthopedics 2016;1–9. [DOI] [PubMed] [Google Scholar]
- [47].Wang K, Ni S, Li Z, et al. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc 2016;25:2849–57. [DOI] [PubMed] [Google Scholar]


