Abstract
Eliminating disparities in health can benefit from the inclusion of diverse populations pursuing health disparity research careers. A goal of the Texas Center for Health Disparities (TCHD) is to provide opportunities for underrepresented minority faculty to become successful health disparity researchers. The TCHD created the Steps Toward Academic Research (STAR) fellowship program to provide faculty and community partners a yearlong face-to-face and online hybrid curriculum focused on acquiring fundamental concepts in biomedical and behavioral health disparity research, basics in grantsmanship as well as professional development skills. In total, this training approach is envisioned to provide mutually beneficial co-learning experiences that will increase the number of under-represented minorities (URMs) entering translational research focused on the elimination of health disparities.
Keywords: Minority, Faculty, Grant Writing, Professional Development, Health Disparities
Introduction
Advances to improve health outcomes through research and educating future researchers has reduced the burden of disease for many. Yet, inequity of these benefits continues to persist for racial/ethnic and the socio-economically deprived populations.1 Increasing the diversity of biomedical and behavioral scientists is believed to impact change, and improve health outcomes for all populations.2 In 2008, only 7.3% of all US medical school faculty represented racial/ethnic populations (eg, African Americans, Hispanic/Latino or Native American/Alaskan Native Islanders).3 Equally disparate is the number of underrepresented minority (URM) faculty conducting biomedical and behavioral science research.4 For example, recent statistics from the US Department of Education, National Center for Education Statistics reported that, in 2015, URM faculty represented only <10% of all faculty, 42% of faculty were White males and 35% were White females.5 Because faculty members are believed to be the cornerstone of the institution and serve as role models for their students, researchers argue that a lack of faculty from racially diverse backgrounds is one of several factors contributing to the disproportion of URM participation in the biomedical and behavioral fields.6
In addition to recruiting URM faculty into academic positions, diversity efforts also require an additional emphasis on supporting training opportunities and the provision of resources for those interested in conducting health research.7-10 Early stage faculty require the acquisition of numerous skill sets that are rarely taught (eg, laboratory management, establishing collaborations, maintaining research budgets, scholarly advancement). Instead, they often acquire such skills by one’s own experience, rather than by a systematic process. Research career progression should include opportunities for early-stage faculty to practice these skills with feedback. Senior faculty with complementary interests can be valuble mentors in modeling sucessful research careers but are rarely found in number at less research-intensive institutions. Other considerable barriers for URM faculty include: limited access to faculty training; poor resources to which faculty can connect; and the demands of teaching.11 These and other barriers are often exacerbated at minority-serving institutions (MSIs) that are historically under-resourced.12 If we do not address these barriers, a continued lack of parity will raise serious concerns due to the increase in URM within the United States and the dependency of URMs’ contributions to match the demand of the science, health and technology workforce.13,14
The University of North Texas Health Science Center (UNTHSC) established the Texas Center for Health Disparities (TCHD) with a vision to foster relationships to conduct research in areas of health disparity, promote education for academic constituencies and health care practitioners as well as educate policy makers on the existence of health disparities. To this end, the Research Training and Education Core became one of four major cores within the TCHD and created a successful training program, the Steps Toward Academic Research (STAR) fellowship in 2004. The objective of the STAR fellowship is to provide intensive training in grant writing and professional development activities to increase success among URM faculty pursuing health disparity research careers. To meet our objective, the STAR fellowship enlisted faculty interested in conducting health disparity research across the United States. In addition to academic faculty, individuals within the community (defined in methods) with interests in health disparity research were invited to participate in the STAR fellowship alongside faculty. Both academic fellows and community fellows participated in grant writing and professional development workshops with the expectation that community fellows would gain interest in forming partnerships with faculty to develop a health disparity research project, become knowledgeable of how to develop a grant proposal, and to a greater extent, enhance their professional careers as community stakeholders. To provide a bi-directional learning environment, academic fellows likewise would have the opportunity to learn from the experiences and skills of community fellows to help understand how to engage and conduct health disparity research relevant within respective communities. In this article, we report on the STAR fellowship design, curricula and outcomes in preparing URM faculty and community stakeholders for a successful career in health disparity research.
Methods
The STAR fellowship program includes an incoming class of 10 fellows per year. Information about the STAR fellowship program is disseminated by traditional strategies including: listserv announcements, website and recruitment by attending local, regional and national professional conferences. A valuable recruitment mechanism has also been the marketing of our program through long-standing relationships with academic and community partner institutions. Applicants of the STAR Fellowship were selected from a national pool of early-stage faculty (eg, assistant professors) and community stakeholders (eg, community directors, public health workers, governmental policy administrators, hospital managers and staffers at community centers) with an interest in pursuing health disparity research. Prospective STAR fellows applied through an online application requiring demographic information and a written essay about their knowledge of, and personal and career goals centered on pursuing the elimination of, health disparities. Applicants were also required to provide two letters of recommendation from their department academic chair and/or supervisor as affirmation of interest and time commitment to the one-year fellowship. In addition, applicants were surveyed on their specific needs including: access to computer technology; familiarity with concepts in health disparities; travel and individual support needs.
Fellows attended electronic meetings in July, September, November, January, and March, and on-campus meetings in August, October, December, February, and April. The intensive one-year curriculum was designed to incorporate major proficiency areas including; Principles in Research, Grant Writing and Professional Development, Principles of Health Disparities and Community-based Participatory Research (CBPR). Further detail of the STAR curriculum can be found at (https://www.unthsc.edu/research/texas-center-for-health-disparities/star-fellowship-program/).
UNTHSC has more than 60 faculty who collaborate with the Texas Center for Health Disparities and to a broader extent more than 300 biomedical research faculty who provide senior-level expertise in grant writing. The TCHD also takes advantage of its partnership with senior health disparity researchers across the United States. Mentors are selected from the UNTHSC faculty ranks, although faculty from other institutions of higher education across the United States can also serve as mentors. Identification and recruitment of mentors is based on their commitment to developing a health disparity research agenda at UNTHSC and other institutions and a personal commitment to increasing the number of health disparity researchers from URM and disadvantaged groups. The STAR fellows’ immersion into health disparities begins with an introduction by directors of the TCHD cores to its faculty, administrators and research projects. The STAR fellowship is led by a team of experienced research faculty who provide leadership in research, grant writing and research training expertise. During the initial three months, academic and community fellows attend interactive workshops on learning concepts, conducting research and grant development. Because the training plan and objective of this program are based on ensuring that fellows become productive health disparity researchers, the STAR Fellowship requires each fellow to develop an individual pilot research project. To facilitate the progress of his/her project, each fellow is assigned a faculty mentor, based on common interests, necessary skills and the mentor’s past or likely future successes in mentoring. Each fellow works closely with his/her mentor during campus visits and communicates frequently (about every two weeks) during the duration of the STAR Fellowship program. As fellows progress into the year, they receive training on the principles of health disparity research, including historical perspectives in health inequalities, defining and measuring health disparities and an introduction to CBPR. In addition, fellows participate in several networking sessions with former fellows by teleconferences. They also participate in TCHD activities that include attendance at monthly director’s meetings, Community Advisory Board (CAB) meetings and a community-based participatory field study. These activities are supplemented with topical guest lectures from UNTHSC faculty on the human subject review process, mechanisms of funding support and navigation of grant agency guidelines. Toward program end, fellows participate in a mock grant review in which they present their individual pilot project to the fellows and their mentors. In addition, all fellows are required to submit their pilot project, which is externally reviewed by TCHD faculty and community partners. Each year, one fellow is awarded up to $25,000 in pilot funding to facilitate their research studies. To complete their program, fellows attend the annual Texas Conference on Health Disparities and present their pilot project as part of the poster presentation session. Finally, the fellow pilot project awardee is recognized during the annual conference.
Although the TCHD has been in existence since 2004, data collected from the STAR fellowship program spanned nine cohorts consisting of 10 fellows each between 2008-2016. Applicant data of non-STAR Fellowship participants was not included as part of program evaluation because of limited access in tracking applicant information relevant to participant outcomes in this report. Each participant was followed for five years after completing the fellowship to track fellows’ success and career progression. Data were collected via online surveys at enrollment, at the completion of fellowship year, and each year after program completion for five years. Analysis of individual participant characteristics included race/ethnicity and sex. Information describing participants’ home academic institution, primary appointment, research discipline and/or employment was also collected from cohorts. An online survey was distributed to the STAR fellows; the survey assessed fellows’ self-reported feelings regarding the training they received and process of the STAR Fellowship. We also collected information about career outcomes including self-reported grants submitted and/or funded, publications authored by fellows prior to and up to five years beyond training. Data collected were also confirmed from online available curriculum vitae and PubMed (publications). All levels of authorship including first, middle and corresponding authorship were tabulated. Grant funding was collected by performing a search on NIH RePorter (grant awards). Grant funding was defined as those awarded as principal investigator including all NIH grant mechanisms (eg, R series, K series, Diversity Supplements, mentor-guided research awards). The primary indicators of STAR fellow’s success were number of publications, number of awards (reported in aggregate across two 5-year grant cycles), retention in academic institutions, promotion and tenure and scholarly achievements (eg, honors, awards, memberships). Additional indicators of success included feedback from fellows provided through correspondence. Appropriate statistical analysis was implemented for comparisons in determining outcome effects and denoted in figure legends.
Results
As of 2016, 71 fellows had completed the program and 10 fellows will complete their program in summer 2017. Most of our fellows have been African Americans (48%) with a greater proportion of females (49%). Asians (20%) are the next largest group followed by Hispanics (10%) and Whites (14%) (Table 1). Academic biomedical and behavioral scientists were the largest constituency (31%) of the fellowship followed by 16% public health, 13% community health and 11% nursing professionals, respectively (Table 2).
Table 1. Percentage of participants by sex and race/ethnicity.
| Male, n=29 (35%) | Female, n=53 (65%) | Total | |
| Race/Ethnicity | Male % | Female % | Total % |
| African American/Black | 44 | 49 | 48 |
| Asian | 24 | 28 | 20 |
| Hispanic | 8 | 11 | 10 |
| Native American | 2 | 0 | 1 |
| Pacific Islander | 0 | 1 | 2 |
| White | 16 | 14 | 14 |
| Undeclared | 6 | 0 | 5 |
Table 2. STAR Fellows’ academic or professional institution, type and rank.
| Institution Type | % |
| Minority-serving institution | 39 |
| Non-minority serving institution | 26 |
| Research medical health science center | 15 |
| Allied heath entity | 3 |
| Municipal or government agency | 13 |
| Private sector, charity, foundation | 3 |
| Academic Rank/Position Rank | |
| Assistant professor | 75 |
| Associate professor or higher | 7 |
| Community director | 3 |
| Staff employee | 7 |
| Other | 8 |
| Discipline/ Health Profession | |
| Biomedical /behavioral sciences | 31 |
| Medicine | 3 |
| Nursing | 11 |
| Public health | 16 |
| Community health | 13 |
| Psychology | 3 |
| Economics | 6 |
| Health policy | 8 |
| Immigrant health | 3 |
| Other | 2 |
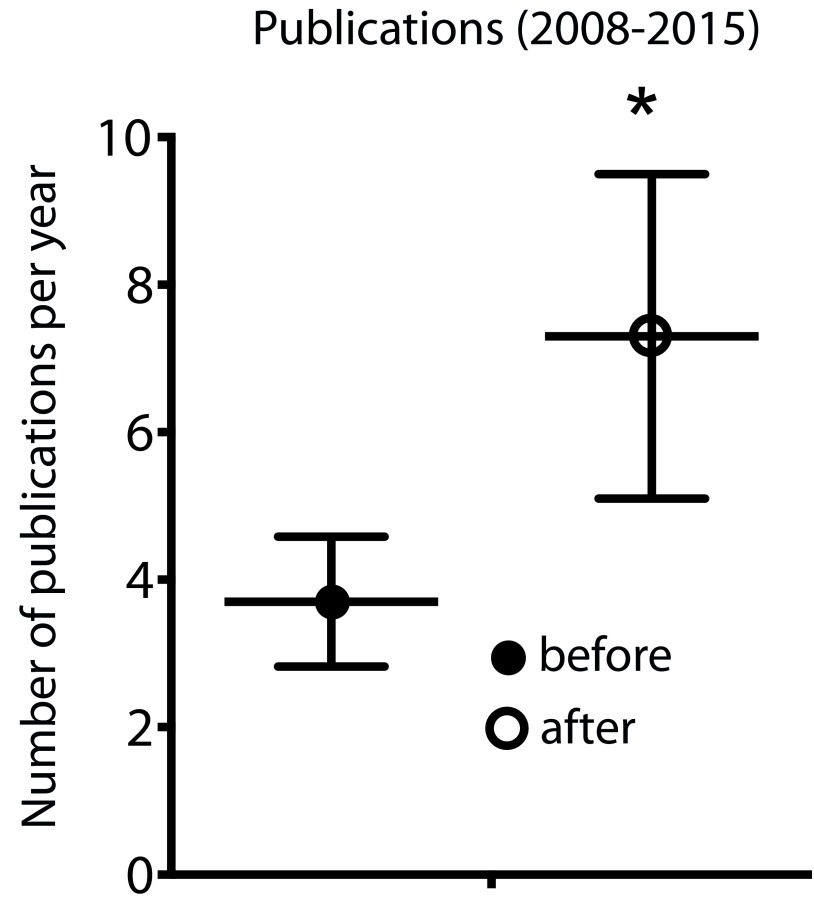
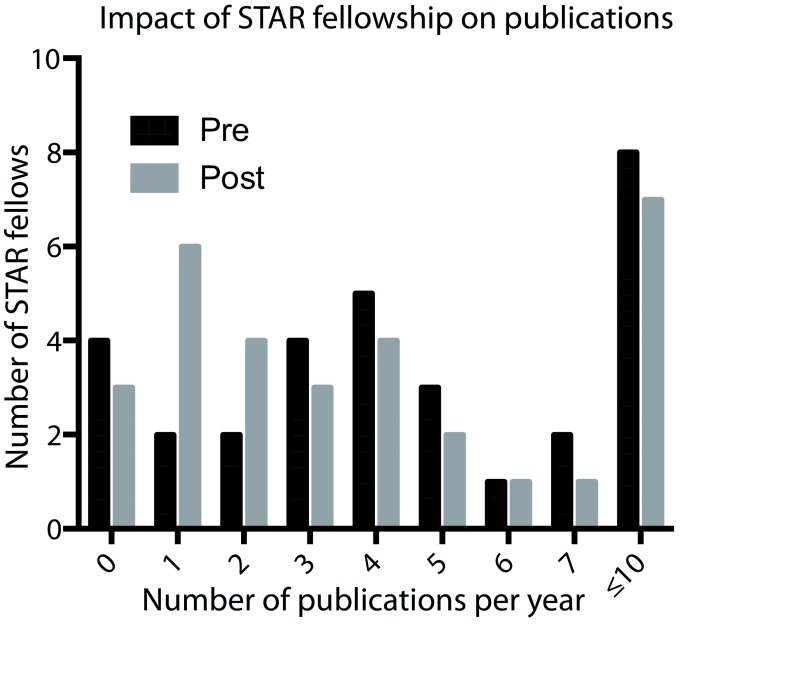
The number of publications by fellows was either self-reported or identified by performing a PubMed search (https://www.ncbi.nlm.nih.gov/pubmed/). We compared the number of publications by fellows prior to the start of their program with the number of publication two to five years beyond their training. Pre- and post-publications were collected from a total of 60 fellows. Publication data from 11 fellows were excluded because training was still in progress or the fellow had completed the program within the last year (Figure 1). STAR fellows entering the program with at least two publications per year demonstrated an increase in the number of publications beyond their training years. STAR Fellows having one publication prior to starting the fellowship had the greatest increase in the number of publications per year. In contrast, fellows entering the program with three or more publications per year maintained a similar publication rate or was slightly decreased (Figure 2).
Figure 1. Publication proficiency of STAR fellows.
Aggregate of mean number of fellows producing at least one or more publication(s) per year within two years after completing the STAR Fellowship program. Bars represents the mean (n=60) ± S.E (error bars). Asterisks (*) indicate significant (P<.05) difference as determined using students’ t test analysis.
Figure 2. Publication proficiency of STAR fellows: before and after.
Comparison of the number of publications per year by fellows prior to the start of their program to the number of publication two to five years beyond their training.
The ability to receive promotion and tenure among academic faculty is a critical measure of career success, particularly at research intensive institutions and increasingly among MSIs with graduate research training programs. Annual requests of grant support beyond one year after program completion was requested of STAR fellows. We also performed NIH RePorter (https://projectreporter.nih.gov/reporter.cfm) database searches when applicable. We report $6,811,559 (2008-2017) in extramural and intramural research awards to STAR Fellows. The average amount of grant funding per fellow was approximately $90,820. This includes funding reported by community fellows.
The STAR Fellowship has encouraged career advancement, as 27 out of 70 (39%) reported receiving promotion in academic rank. We report 25% of STAR fellows were promoted to associate professor and 12% promoted to professor, and of these, 13% promoted with tenure. Among the community fellows having completed one year of the program, 2 of 5 (20%) reported advancing to a directorship role or higher. STAR fellows engaged in meaningful professional development activities including scholarly pursuits, community outreach, invited lectures, grant reviewer and participation in additional progressional fellowships (Table 3).
Table 3. Aggregate scholarly achievements and professional development activities of STAR fellows.
| Achievements/Activities | Total | Average |
| Fellowships | 3 | .10 |
| Institutional/department service | 34 | 1.13 |
| Abstracts presented at professional/society meetings | 53 | 1.77 |
| Professional/society memberships joined | 24 | .80 |
| Invited lectures/presentations | 51 | 1.70 |
| Journal reviewer | 16 | .53 |
| Grant reviewer | 11 | .36 |
| Institutional recognition | 4 | .13 |
| Local/state/national community outreach | 18 | .60 |
Fellows are also asked to complete an online survey to evaluate the program operation and grant writing preparation workshops. On average, 57% and 36% scored the program as excellent to very good, respectively. Only 5.5% and 1.7% felt the program operations were fair or poor, respectively. Similarly, fellows were very positive about the quality of grant preparation and professional development workshops. Of the responding fellows, 32%-56% rated mentor alignment, mentor’s guidance, grant writing workshops and peer critique as very good to excellent. Less than 7% scored the grant writing preparation workshops as fair to poor.
Discussion
Increasing URMs’ entry into STEM academic programs alone is not enough to promote and sustain diversity efforts.1, 3,10 URM professionals in biomedical/behavioral science and health professions offer unique skills and motivation to serve underserved populations and to address health disparities.15-17 An important goal of the STAR fellowship program is to expand the research training abilities of URM faculty by building capacity to acquire grant writing and professional development skills, personal linkages and networks necessary for sustainable health disparity research careers.
The time and commitment required to establish a successful research career is particularly difficult for undergraduate faculty at less intensive research colleges and universities, particularly at MSIs where many faculty are faced with heavy teaching obligations. The lack of time is compounded by the necessity for summer release time, which may interfere with family responsibilities. The STAR fellowship’s approach of implementing a yearlong program takes advantage of online activities as well as having the assurance from the fellow’s dean, chair or supervisor. This timeframe is similarly optimal for fellows to acquire and enhance pre-requisite skills. Between 2008-2016, only two participants withdrew because of difficulty with scheduling.
The STAR Fellowship recognizes the value of tailoring proficiencies in grant writing depending on a fellow’s career stage and prior experiences critical to success in research and particularly for those with interest in health disparity research careers. In this regard, we intentionally designed a curriculum that would provide fellows the necessary framework focused on concepts related to health disparities and social determinants of health. Academic fellows were able to gain knowledge based on the understanding that conducting health disparity research requires skills to identify and implement the various domains of health disparity models (eg, individual, social behavioral, community, policy) into their community-based research programs. By integrating faculty and community stakeholders into the fellowship, we provide a co-learning experience so that faculty become exposed to CBPR. Likewise, community fellows appreciated learning form their faculty peers on how to conduct research. Importantly, these experiences are supported by grant writing activities, professional and career development workshops and mentored-guided grant development.
Beyond grant writing, the STAR fellowship program provides mentorship and professional development skills to promote a successful research career in health disparities for historically underrepresented populations. Overall, the objective of developing a strong, minority-based cadre of research faculty from URM partner institutions represents a worthy endeavor, despite its inherent challenges. To date, we have observed positive outcomes consistent with best practices validated by fellows’ success in publication proficiency, ability to compete for extramural research awards and career advancement. Community fellows have also benefitted from the STAR program in the form of collaborative research and professional advancement.
Individual factors have emerged from certain models including trainee characteristics defined by background and environment, social integration, cognitive factors and self identity as predictors of success.18-20 In addition, skill-building support, access to resource infrastucture and mentoring are also key institutional characteristics to a trainees’ success. In recent years, the STAR Fellowship program began assessing the “readiness” of fellows based on measures of self beliefs related to acquisition of grant writing skills, professional development and confidence factors related to career success. Although grant writing proficiency can not be captured through self-assessment, the strong sense of efficacy by STAR Fellows continues to emerge and positively correlates with successful outcomes including numbers of proposals submitted, reviewed, resubmitted, and funded. In addition, self-reported data from the fellows have provided valuable information of their grant writing proficiency, persistence and confidence in health disparity research.
Study Limitations
This descriptive study did not have a control group but, instead, was designed to gain a number of quantitative and qualitative outcomes assessed as outcomes of success. Although significant increases were observed in publications and acquisition of grant funding, we note that the exclusivity of data collection from PubMed, self survey and curriculum vitae in lieu of other search tools, may be a potential limitation. This may be the case particularly for those fellows whose research was in non-biomedical health fields of study. In addition, we recognize the inherent weakness in self-assessment evaluation in terms of predicting grant writing proficiency. Our ongoing analysis of cohorts still in process is considering these and other limitations.
Conclusion
The STAR Fellowship continues to learn from best practices and adds effective new practices to complement existing approaches in addressing the gap among URM and disadvantaged populations entering and pursuing health disparity careers. The STAR fellowship will continue to collect informative from past cohorts to report on self-belief factors that may be predictive of faculty success.
Acknowledgments
The authors would like to thank those individuals contributing to the generation of this work including: Bruce Dubin, DO, JD FCLM, FACOI, executive vice president for academic affairs, provost and dean of the College of Osteopathic Medicine, Kansas City University of Medicine and Bioscience, College of Osteopathic Medicine; Dr. Jose Pagan, director of the Center for Health Innovation at The New York Academy of Medicine; Andrea Gouldy, Terry Voss and Rajendra Sharma, PhD.
This research was funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Numbers P20MD001633 and P20MD006882 (JKV). Human subject data collection and the writing of the manuscript was supported by the grant P20MD006882 and U54MD006882 (JKV).
References
- 1. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186(1186):69-101. 10.1111/j.1749-6632.2009.05339.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gonzales R, Handley MA, Ackerman S, Oʼsullivan PS. A framework for training health professionals in implementation and dissemination science. Acad Med. 2012;87(3):271-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Page KR, Castillo-Page L, Wright SM. Faculty diversity programs in U.S. medical schools and characteristics associated with higher faculty diversity. Acad Med. 2011;86(10):1221-1228. 10.1097/ACM.0b013e31822c066d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gibbs KD Jr, McGready J, Bennett JC, Griffin K. Biomedical Science Ph.D. Career Interest Patterns by Race/Ethnicity and Gender. PLoS One. 2014;9(12):e114736. 10.1371/journal.pone.0114736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. U.S. Department of Education, National Center for Education Statistics Characteristics of Postsecondary Faculty. The Condition of Education 2017. (NCES 2017-144). Last accessed December 12, 2017 from https://nces.ed.gov/programs/coe/indicator_csc.asp
- 6. Finkelstein MJ, Conley VM, Schuster JH. The Faculty Factor Reassessing the American Academy in a Turbulent Era. Baltimore, Maryland: Johns Hopkins University Press; 2016. [Google Scholar]
- 7. Hitchcock P, Mathur A, Bennett J, et al. The future of graduate and postdoctoral training in the biosciences. Elife. 2017;6(6):e32715. 10.7554/eLife.32715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harawa NT, Manson SM, Mangione CM, et al. Strategies for enhancing research in aging health disparities by mentoring diverse investigators. J Clin Transl Sci. 2017;1(3):167-175. 10.1017/cts.2016.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Duncan GA, Lockett A, Villegas LR, et al. National Heart, Lung, and Blood Institute Workshop Summary: Enhancing Opportunities for Training and Retention of a Diverse Biomedical Workforce. Ann Am Thorac Soc. 2016;13(4):562-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jean-Louis G, Ayappa I, Rapoport D, et al. Mentoring junior URM scientists to engage in sleep health disparities research: experience of the NYU PRIDE Institute. Sleep Med. 2016;18:108-117. 10.1016/j.sleep.2015.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mahoney MR, Wilson E, Odom KL, Flowers L, Adler SR. Minority faculty voices on diversity in academic medicine: perspectives from one school. Acad Med. 2008;83(8):781-786. 10.1097/ACM.0b013e31817ec002 10.1097/ACM.0b013e31817ec002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rodriguez JE, Campbell KM, Fogarty JP, Williams RL. Underrepresented minority faculty in academic medicine: a systematic review of URM faculty development. Fam Med. 2014;46(2):100-104. [PubMed] [Google Scholar]
- 13. Rosenstock L, Silver GB, Helsing K, et al. Confronting the public health workforce crisis: ASPH statement on the public health workforce. Public Health Rep. 2008;123(3):395-398. 10.1177/003335490812300322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff (Millwood). 2002;21(5):90- 102. Millwood. https://doi.org/ 10.1377/hlthaff.21.5.90 PMID:12224912. 10.1377/hlthaff.21.5.90 [DOI] [PubMed]
- 15. Degazon CE, Mancha C. Changing the face of nursing: reducing ethnic and racial disparities in health. Fam Community Health. 2012;35(1):5-14. 10.1097/FCH.0b013e3182385cf6 10.1097/FCH.0b013e3182385cf6 [DOI] [PubMed] [Google Scholar]
- 16. Drolet BC, Lorenzi NM. Translational research: understanding the continuum from bench to bedside. Transl Res. 2011;157(1):1-5. 10.1016/j.trsl.2010.10.002 [DOI] [PubMed] [Google Scholar]
- 17. Fleming ES, Perkins J, Easa D, et al. The role of translational research in addressing health disparities: a conceptual framework. Ethn Dis. 2008;18(2)(suppl 2):S2-S155, 60. [PMC free article] [PubMed] [Google Scholar]
- 18. Villarejo M, Barlow AE, Kogan D, Veazey BD, Sweeney JK. Encouraging minority undergraduates to choose science careers: career paths survey results. CBE Life Sci Educ. 2008;7(4):394-409. 10.1187/cbe.08-04-0018 10.1187/cbe.08-04-0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Clark SL, Dyar C. Maung, N, London B. Psychosocial pathways to STEM engagement among graduate students in the life sciences. Life Sci Educ. 2016;15(3):1-36. 10.1187/cbe.16-01-0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Manson SM. Personal journeys, professional paths: persistence in navigating the crossroads of a research career. Am J Public Health. 2009;99(S1)(suppl 1):S20-S25. 10.2105/AJPH.2007.133603 [DOI] [PMC free article] [PubMed] [Google Scholar]