Abstract
Objective
We set out to determine if a primarily Internet-delivered behavioral weight loss intervention produced differential weight loss in African American and non-Hispanic White women, and to identify possible mediators.
Design
Data for this analysis were from a randomized controlled trial, collected at baseline and 4-months.
Setting
The intervention included monthly face-to-face group sessions and an Internet component that participants were recommended to use at least once weekly.
Participants
We included overweight or obese African American and non-Hispanic White women (n=170), with at least weekly Internet access, who were able to attend group sessions.
Intervention
Monthly face-to-face group sessions were delivered in large or small groups. The Internet component included automated tailored feedback, self-monitoring tools, written lessons, video resources, problem solving, exercise action planning tools, and social support through message boards.
Main Outcome Measure
Multiple linear regression was used to evaluate race group differences in weight change.
Results
Non-Hispanic White women lost more weight than African American women (-5.03% vs.-2.39%, P=.0002). Greater website log-ins and higher change in Eating Behavior Inventory score in non-Hispanic White women partially mediated the race-weight loss relationship.
Conclusions
The weight loss disparity may be addressed through improved website engagement and adoption of weight control behaviors.
Keywords: Obesity, Weight Loss, African American, Intervention, Randomized Controlled Trial
Introduction
Around two-thirds of adults in the United States are overweight or obese (68.8%).1 Among racial/ethnic subgroups, African American (AA) women are the most affected by overweight/obesity (82.1%).1 This disparity indicates a need for solutions, as unhealthy weight increases the risk of developing type 2 diabetes, cardiovascular disease, and some cancers.2 Behavioral weight loss interventions (BWI) are an effective solution that include diet, physical activity (PA), and behavior modification to produce clinically significant weight reduction (5%-10% of baseline weight).3–5
African American, compared with non-Hispanic White (NHW), women consistently lose 2-3 kg less weight in BWI,6,7 which can reduce the potential to maximize health benefits. Reasons for the weight loss disparity are not well understood. Mixed findings on racial differences in dietary and PA changes during BWI,8,9 difficulty recruiting and retaining minorities, and a lack of conducting or reporting such analyses contribute to the knowledge gap.7,10 More evidence is needed to understand and reduce the racial weight loss disparity.
We conducted a secondary data analysis of a randomized controlled trial using BWI to examine the impact of race on women’s weight loss and weight-related behaviors. We hypothesized that: 1) NHW women would achieve greater weight loss than AA women; 2) diet, PA, and study engagement would differ by race such that NHW women would have more favorable changes compared with AA women at 4 months post-baseline. We further hypothesized that these changes would mediate the relationship between race and weight loss.
Methods
Data Source and Study Design
A 4-month randomized controlled trial (N=195), fully described elsewhere and based on the Diabetes Prevention Program, provided data for this analysis.9 Briefly, eligible participants were overweight or obese (body mass index ≥ 25 kg/m2), had Internet access at least once weekly, and were able to attend the 4 monthly sessions. Participants were randomized to receive monthly face-to-face sessions in a large or small group (approximately 100 vs 20 individuals). The primarily Internet-delivered intervention promoted adoption of a reduced-calorie dietary pattern (1200-1500 calories/day) and increased moderate-intensity PA. Both groups received the same Internet components: weekly automated tailored feedback, self-monitoring tools (online or paper calorie tracking diary), tailored lessons and tools for problem-solving dietary and PA barriers, video resources, exercise planning tools (online scheduler and progression plan), and a message board for social support. Participants provided informed consent online. Measurements were collected at baseline and 4 months. Our study’s sample (n=170) included only NHW and AA women. The Institutional Review Board of the University of North Carolina at Chapel Hill approved the study.
Measures
All measures, except demographic and study engagement variables, were assessed at baseline and 4-months. Age, marital status, and annual household income were assessed at baseline. Weight was assessed with a digital scale. The Automated Self-Administered 24 Dietary Assessment Tool evaluated calorie intake.11 Self-reported PA (calories/week) was measured using the 7-item Paffenbarger Physical Activity Questionnaire.12 The 26-item Eating Behavior Inventory (EBI) assessed weight control self-monitoring and dietary management behaviors.13 Process variables included total website log-ins and session attendance.
Statistical Analysis
All analyses were conducted using SAS version 9.3 (Cary, NC).14 A P of <.05 was considered statistically significant. Racial differences in demographic variables were evaluated with chi-square and t-tests for categorical and continuous variables, respectively. Demographic variables that differed significantly by race did not significantly impact regression parameter estimates in our analyses, and thus were not included as covariates. We conducted complete case analyses of AA and NHW women (n=170), and controlled for group assignment.9 Data were assumed missing at random due to the lack of association between demographic and outcome variables.
Multiple linear regression was used to examine group differences in 4-month change in weight, PA, calorie intake, and EBI score. Regression assumptions held for all variables. Variables that differed by group at 4-months were explored as potential mediators with the PROCESS macro in a multiple mediation model that controlled for group randomization.15 Bootstrapping (5,000 sampling distributions) was applied to determine the significance of the mediated effect.
Results
Baseline Characteristics
Participants (n=170) included 55.3% AA and 44.7% NHW women who were aged 46.10±10.8 years (Table 1). Baseline weight (P=.002) and BMI were higher for AA women (39.57±8.0) compared with NHW women (35.82±7.3; P=.002). Non-Hispanic White women had a higher annual household income (P<.0001), and more were married or living as married (P=.0002) compared with AA women. Baseline age, dietary intake, PA, total EBI score, and use of EBI-measured weight control strategies were not different between groups.
Table 1. Baseline demographic and behavioral characteristics by race/ethnicity of participants.
| Variable | AA, n=94 | NHW, n=76 | P |
| Age, years | 44.73 (10.13) | 47.79 (11.48) | .07 |
| Annual household income, n (%) | |||
| < $50,000/year | 53 (63.86) | 21 (29.58) | <.0001 |
| ≥ $50,000/year | 30 (36.14) | 50 (70.42) | |
| Marital status, n (%) | |||
| Married or living as married | 47 (50.00) | 59 (77.63) | .0002 |
| Single, divorced, separated | 47 (50.00) | 17 (22.37) | |
| Weight, kg | 106.60 (23.52) | 95.50 (20.68) | .002 |
| BMI, kg/m2 | 39.57 (7.99) | 35.82 (7.34) | .002 |
| Physical activity, kcal/day | 841.9 (953.90) | 708.30 (910.00) | .36 |
| Daily intake, kcal/day | 1906.30 (614.9) | 1893.80 (534.00) | .90 |
| Eating Behavior Inventory score, total | 64.13 (7.89) | 60.38 (9.24) | .13 |
| Eating Behavior Inventory score, dichotomous | .68 (.11) | .68 (.12) | .86 |
All values reported as mean and standard deviation, unless otherwise indicated.
Weight, Physical Activity, and Calorie Intake
Non-Hispanic White, compared with AA, women lost significantly more weight (mean (SD): -5.03% (4.54) vs -2.39% (3.82), P=.0002; Table 2). No differences in PA or calorie intake change were observed between race groups over 4-months.
Table 2. Four-month outcome change and regression values.
| Mean (SD) | Regression Results | ||||
| Outcome | N | AA | NHW | Parameter Estimate (SE) | P |
| Change in weight, % | 124 | -2.39 (3.82) | -5.03 (4.54) | -2.85 (0.74) | .0002 |
| Change in physical activity, calories | 123 | 158.86 (1092.71) | 291.47(867.07) | 151.66 (183.34) | .41 |
| Change in dietary intake, calories | 102 | -406.84 (631.62) | -257.59 (786.84) | 144.71 (142.76) | .31 |
| Change in EBI score | 125 | 5.94 (9.13) | 9.55 (10.03) | 3.95 (1.73) | .02 |
| Session attendance | 170 | 2.54 (1.40) | 2.93 (1.28) | .26 (.20) | .20 |
| Total website log-ins | 170 | 31.0(55.7) | 51.8(68.2) | .67 (.26) | .01 |
Study Engagement
Non-Hispanic White, compared with AA, women had a significantly higher change in EBI score (P=.02) and website log-ins (P=.01; Table 2). When viewed dichotomously (never/rarely used vs some of the time), the EBI score difference may be attributed to either more consistent or greater adoption of total EBI strategies among NHW (20.11) vs AA (19.33) women (P=.09). No race differences were observed in session attendance.
Multiple Mediation
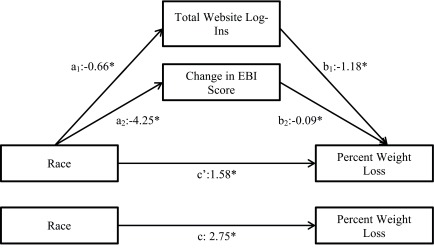
Behavioral and study engagement variables were assessed to determine if they mediated the race-weight loss relationship. Race was associated with fewer website log-ins (log-transformed) in AA women (path a1; β(SE)=-.66(.25), P=.01). Website log-ins were associated with greater weight loss (path a2: β(SE)=-1.18(.25), P<.01) (Figure 1). Race was associated with lower change in EBI score among AA women (path b1: β(SE)=-4.25(1.63), P<.01). Change in EBI was associated with better weight loss (path b2: β(SE)=-.09(.04), P=.01). The total (path c: β(SE)=2.75(.74), P<.01) and direct effect (path c’: β(SE)=1.58(.72), P<.05) of race on weight loss were significant, such that AA women had a lower weight change than NHW women. The effect of race on weight loss was attenuated by the number of log-ins and change in EBI score in the model (path c’), indicating partial mediation. Table 3 shows the significant total indirect effects when controlling for group assignment and baseline EBI score.
Figure 1. Multiple Mediation Model.
Table 3. Multiple mediation indirect effects.
| Coefficient (SE) | 95% CI | |
| Total indirect effects | 1.17 (.42) | .43, 2.10 |
| Total website log-ins | .78 (.32) | .23, 1.50 |
| Change in EBI score | .38 (.23) | .05, 1.02 |
Discussion
Our study examined the impact of race on weight loss among women in a primarily Internet-delivered BWI. We observed significantly greater weight loss in NHW women compared with AA women at 4 months post-baseline. Better study engagement, demonstrated by more website log-ins, and greater adoption of weight control behaviors were also observed in NHW vs AA women. Website log-ins and change in EBI score partially mediated the racial difference in weight loss. Session attendance, change in PA and dietary calorie intake did not differ by race group.
We observed approximately 3% greater weight loss in NHW vs AA women, a magnitude of weight loss difference previously observed.16 Importantly, minorities consistently lose low-to-modest amounts of weight in BWI.17–19 In our study, NHW women achieved modest weight loss (-5.03%), while AA women (-2.39%) did not, which confirms previous findings in the literature.7,16,19
Weight loss differences may reflect varying change in calorie intake, but our results indicated no race group difference. A previous face-to-face intervention also had similar calorie intake findings,18 but racial differences in diet adherence were observed in an ancillary Dietary Approaches to Stop Hypertension study. Dietary underreporting, seen in AA women, and predicted by increasing BMI,20–22 lower income and higher social desirability bias,22 regardless of the assessment method23 may influence results. The higher weight and lower income status of AA women in our study may contribute to underreporting and explain the weight loss differences. The lack of baseline and 4-month differences may signal the persistence of dietary underreporting throughout the study.
Change in self-reported PA did not differ by group in our study. Previous findings are mixed, reporting no19 or greater self-reported PA in NHW compared with AA.4,18 Importantly, NHW, compared with AA, women have engaged in less objectively measured PA.18 Sustained overestimation of self-reported PA before and after weight loss treatment has been observed in AA women, while NHW women reduced overestimation.24 Perhaps our PA findings reflect AA women’s overestimation, or racial differences in the conceptualization of PA. Different from NHW, AA may perceive PA to include domains of daily work and activities,25 while our study goal was increased leisure-time PA. Social desirability bias may also inflate self-reported PA. Objective PA measurement is recommended to better evaluate PA change within BWI. Strategies to define and increase PA to recommended amounts (250-300 minutes/week)26 among AA women in BWI may be key for weight loss.
Our weight loss results were informed by women’s intervention engagement through attendance, website log-ins, and adoption of EBI-measured weight control behaviors. While we found no difference in session attendance, which has been associated with greater weight loss,4,27 differences may have emerged if more face-to-face sessions were offered. Log-ins and engagement with website self-monitoring features have been associated with better weight loss.28,29 In our study, website log-ins mediated the race-weight loss relationship, which partially explains the racial weight loss differences. More log-ins among NHW vs AA women is not a unique finding, as it was seen before in the Weight Loss Maintenance trial, where AAs were more likely to be minimal vs consistent users of the Internet component.30 Our study required participants to have reliable Internet access. However, the observed fewer log-ins in AA women may reflect national data, where AAs and lower income individuals have less home-based Internet access.31 African American women also had lower income than NHW women in this study, but we were unable to assess changes in Internet access. Fewer log-ins may also reflect lower motivation, interest in weight loss, or use of an Internet program. Our results align with previous evidence, which highlights the role of website engagement on weight outcomes. Future studies may wish to assess additional variables to better elucidate reasons for engagement.
Consistently, increased EBI score is associated with weight loss.13,32 We found that change in total EBI-measured behaviors mediated the race-weight loss relationship. Higher change in total EBI score in NHW women, considered alongside our dichotomous EBI analysis that showed one less strategy was adopted by AA women, suggests that AA women used strategies less consistently. Qualitative methods may be useful to determine how well supports are used and what supports may be needed for AA women to adopt weight control behaviors.
Strengths and Limitations
While this primarily Internet-based intervention complements the mostly face-to-face intervention evidence, limitations exist. Self-reported measures of adherence, dietary intake and PA are limitations of this study. By nature, self-reported data may be inaccurate. An important finding of this study was the racial differences in website engagement during the BWI. However, the lack of post-intervention detail regarding Internet access may have limited our understanding of website engagement throughout the study.
Research Directions
There are many directions investigators could follow to address the weight loss disparity. Researchers may choose to develop research questions with a primary goal to study the weight loss disparity between AA and NHW women to uncover differences in behavior change and treatment. Recruitment and retention of large samples of racial/ethnic minorities will enable subgroup analysis, and are required to understand the outcome disparity. Additionally, objective measurement of behaviors and study engagement may lead to more definitive conclusions. While modest weight loss (5%-10% reduction of baseline weight) is the standard goal, it largely remains an elusive outcome for AA women. Solutions to maximize their outcomes remains important.
While quantitative investigation is valuable, qualitative methods can complement findings, providing a deeper understanding of processes that impact weight loss.10 A mixed methods approach may inform which behaviors and how EBI-measured weight control behaviors are differentially adopted by AA and NHW women in a BWI. Understanding the influence of culture through qualitative methods may improve the effectiveness of BWI approaches in AA women. Considering EBI items like “my emotions cause me to eat,” culturally sensitive BWI approaches may address race-gender-based stress. The persistence of this outcome disparity signals that more research is needed to understand the contexts and mechanisms behind weight loss in AA women.
Conclusions
Results from this study suggest that a predominantly Internet-delivered behavioral weight loss intervention was less effective for AA compared with NHW women. We observed similar self-reported dietary and PA adherence and session attendance, but differing website and weight control behavior adoption that partially explained the race-weight loss relationship. The current study aligns with earlier evidence7,16,19 indicating lower weight loss, behavior change and study engagement in AA compared with NHW women. Greater understanding of study engagement and weight control behaviors in AA enrolled in behavioral weight loss interventions is needed to reduce the racial disparity in women’s weight loss.
Acknowledgments
Funding for this study was provided by the University Cancer Research Fund at the University of North Carolina at Chapel Hill. Informed consent was obtained from all participants.
References
- 1. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491-497. 10.1001/jama.2012.39 [DOI] [PubMed] [Google Scholar]
- 2. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625-1638. 10.1056/NEJMoa021423 [DOI] [PubMed] [Google Scholar]
- 3. Diabetes Prevention Program (DPP) Research Group The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165-2171. 10.2337/diacare.25.12.2165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wadden TA, West DS, Neiberg RH, et al. ; Look AHEAD Research Group . One-year weight losses in the Look AHEAD study: factors associated with success. Obesity (Silver Spring). 2009;17(4):713-722. 10.1038/oby.2008.637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wing RR; Look AHEAD Research Group . Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566-1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev. 2012;13(3):193-213. 10.1111/j.1467-789X.2011.00945.x 10.1111/j.1467-789X.2011.00945.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goode RW, Styn MA, Mendez DD, Gary-Webb TL. African Americans in standard behavioral treatment for obesity, 2001-2015: what have we learned? West J Nurs Res. 2017;39(8):1045-1069. 10.1177/0193945917692115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wing RR, Tate D, Espeland M, et al. Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13(1):300. 10.1186/1471-2458-13-300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tate DF, Valle CG, Crane MM, et al. Randomized trial comparing group size of periodic in-person sessions in a remotely delivered weight loss intervention. Int J Behav Nutr Phys Act. 2017;14(1):144. 10.1186/s12966-017-0599-3 10.1186/s12966-017-0599-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kumanyika SK, Whitt-Glover MC, Haire-Joshu D. What works for obesity prevention and treatment in black Americans? Research directions. Obes Rev. 2014;15(October)(suppl 4):204-212. 10.1111/obr.12213 10.1111/obr.12213 [DOI] [PubMed] [Google Scholar]
- 11.Automated Self-Administered 24-Hour (ASA24®) Dietary Assessment Tool. Last accessed October 18, 2017 from https://epi.grants.cancer.gov/asa24/.
- 12. Paffenbarger RS Jr, Wing ALHR, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108(3):161-175. 10.1093/oxfordjournals.aje.a112608 10.1093/oxfordjournals.aje.a112608 [DOI] [PubMed] [Google Scholar]
- 13. O’Neil PM, Rieder S. Utility and validity of the eating behavior inventory in clinical obesity research: a review of the literature. Obes Rev. 2005;6(3):209-216. 10.1111/j.1467-789X.2005.00192.x 10.1111/j.1467-789X.2005.00192.x [DOI] [PubMed] [Google Scholar]
- 14. SAS® 9.3. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 15. Hayes A. Introduction to Mediation, Moderation, and Conditional Process Analysis : A Regression- Based Approach. New York: The Guilford Press; 2013. [Google Scholar]
- 16. West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity (Silver Spring). 2008;16(6):1413-1420. 10.1038/oby.2008.224 [DOI] [PubMed] [Google Scholar]
- 17. Samuel-Hodge CD, Johnson CM, Braxton DF, Lackey M. Effectiveness of Diabetes Prevention Program translations among African Americans. Obes Rev. 2014;15(October)(suppl 4):107-124. 10.1111/obr.12211 [DOI] [PubMed] [Google Scholar]
- 18. Davis KK, Tate DF, Lang W, et al. Racial differences in weight loss among adults in a behavioral weight loss intervention: role of diet and physical activity. J Phys Act Health. 2015;12(12):1558-1566. 10.1123/jpah.2014-0243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wingo BC, Carson TL, Ard J. Differences in weight loss and health outcomes among African Americans and whites in multicentre trials. Obes Rev. 2014;15(October)(suppl 4):46-61. 10.1111/obr.12212 [DOI] [PubMed] [Google Scholar]
- 20. Amend A, Melkus GD, Chyun DA, Galasso P, Wylie-Rosett J. Validation of dietary intake data in black women with type 2 diabetes. J Am Diet Assoc. 2007;107(1):112-117. 10.1016/j.jada.2006.10.004 [DOI] [PubMed] [Google Scholar]
- 21. Samuel-Hodge CD, Fernandez LM, Henríquez-Roldán CF, Johnston LF, Keyserling TC. A comparison of self-reported energy intake with total energy expenditure estimated by accelerometer and basal metabolic rate in African-American women with type 2 diabetes. Diabetes Care. 2004;27(3):663-669. 10.2337/diacare.27.3.663 [DOI] [PubMed] [Google Scholar]
- 22. Scagliusi FB, Ferriolli E, Pfrimer K, et al. Characteristics of women who frequently under report their energy intake: a doubly labelled water study. Eur J Clin Nutr. 2009;63(10):1192-1199. 10.1038/ejcn.2009.54 [DOI] [PubMed] [Google Scholar]
- 23. Black AE, Cole TJ. Biased over- or under-reporting is characteristic of individuals whether over time or by different assessment methods. J Am Diet Assoc. 2001;101(1):70-80. 10.1016/S0002-8223(01)00018-9 [DOI] [PubMed] [Google Scholar]
- 24. Walsh MC, Hunter GR, Sirikul B, Gower BA. Comparison of self-reported with objectively assessed energy expenditure in black and white women before and after weight loss. Am J Clin Nutr. 2004;79(6):1013-1019. [DOI] [PubMed] [Google Scholar]
- 25. Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe A. Perceptions and beliefs about exercise, rest, and health among African-Americans. Am J Health Promot. 1995;9(6):426-429. 10.4278/0890-1171-9.6.426 [DOI] [PubMed] [Google Scholar]
- 26. Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78(4):684-689. [DOI] [PubMed] [Google Scholar]
- 27. Walcott-McQuigg JA, Chen SP, Davis K, Stevenson E, Choi A, Wangsrikhun S. Weight loss and weight loss maintenance in African-American women. J Natl Med Assoc. 2002;94(8):686-694. [PMC free article] [PubMed] [Google Scholar]
- 28. Krukowski RA, Harvey-Berino J, Bursac Z, Ashikaga T, West DS. Patterns of success: online self-monitoring in a web-based behavioral weight control program. Health Psychol. 2013;32(2):164-170. 10.1037/a0028135 10.1037/a0028135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Neve M, Morgan PJ, Jones PR, Collins CE Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev. 2010;11(4):306-321. htps://doi.org/ 10.1111/j.1467-789X.2009.00646.x. PMID:19754633. [DOI] [PubMed]
- 30. Funk KL, Stevens VJ, Appel LJ, et al. Associations of internet website use with weight change in a long-term weight loss maintenance program. J Med Internet Res. 2010;12(3):e29. 10.2196/jmir.1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Demographics of Internet and Home Broadband Usage in the United States. Pew Research Center. Last accessed October 1, 2017 from: http://www.pewinternet.org/fact-sheet/internet-broadband/.
- 32. Jakicic JM, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002;34(10):1653-1659. 10.1097/00005768-200210000-00018 [DOI] [PubMed] [Google Scholar]