Abstract
Background & Aims
Recognition of rumination and supragastric belching is often delayed as symptoms may be mistakenly attributed to gastroesophageal reflux disease (GERD). However, distinct from GERD, rumination and supragastric belching are more responsive to behavioral interventions than to acid-suppressive and anti-reflux therapies. Postprandial high-resolution impedance manometry (PP-HRIM) is an efficient method to identify rumination and belches. We investigated the distribution of postprandial profiles determined by PP-HRIM, and identified patient features associated with postprandial profiles among patients with non-response to proton pump inhibitors (PPIs).
Methods
We performed a retrospective analysis of PP-HRIM studies performed on 94 adults (mean age, 50.6 yrs; 62% female) evaluated for PPI non-responsiveness at an esophageal referral center, from January 2010 through May 2016. Following a standard esophageal manometry protocol, patients ingested a solid refluxogenic test meal (identified by patients as one that induces symptoms) with postprandial monitoring up to 90 min (median 50 min). Patients were assigned to 1 of 4 postprandial profiles: normal; reflux only (>6 transient lower esophageal sphincter relaxations (TLESRs)/hour); supragastric belch (>2 supragastric belches/hour), with or without TLESR; or rumination (≥1 rumination episode/hour) with or without TLESR and supragastric belching. The primary outcome was postprandial profile.
Results
Of the study participants, 24% had a normal post-prandial profile, 14% had a reflux only profile, 42% had a supragastric belch profile, and 20% had a rumination profile. In multinomial regression analysis, the rumination group most frequently presented with regurgitation, the supragastric belch and rumination groups were younger in age, and the reflux-only group had a lower esophagogastric junction contractile integral. The number of weakly acidic reflux events measured by impedance-pH monitoring in patients receiving PPI therapy was significantly associated with frequency of rumination episodes and supragastric belches.
Conclusion
In a retrospective analysis of 94 non-responders to PPI therapy evaluated by PP-HRIM, we detected an abnormal post-prandial pattern in 76% of cases: 42% of these were characterized as supragastric belching, 20% as rumination, and 14% as reflux only. Age, esophagogastric junction contractility, impedance-pH profiles, and symptom presentation differed significantly among groups. PP-HRIM can be used in the clinic to evaluate mechanisms of PPI non-response.
Keywords: EGJ, belching, GERD, functional heartburn
INTRODUCTION
Up to 40% of patients with suspected gastroesophageal reflux disease (GERD) do not respond to proton pump inhibitor (PPI) therapy1. This population of PPI non-responders (PPINRs) represents a large health care burden, and strategies to effectively characterize and manage this heterogeneous group are critically needed. Prior studies report that approximately one-third of patients referred for PPI non-response suffer from functional gastroduodenal disorders, including rumination syndrome and belching disorders 2, 3. Since symptoms associated with rumination and supragastric belching overlap with GERD, diagnosis and appropriate treatment is often delayed4. Furthermore, rumination and supragastric belching are more responsive to behavioral interventions rather than acid-suppressive and anti-reflux strategies utilized for refractory GERD 2, 5, 6. Thus, timely detection and management of these behavioral conditions are essential.
High resolution impedance manometry (HRIM) concurrently assesses directionality of liquid and gas movement in the esophageal body and changes in cavity and sphincter pressures7. Additional postprandial HRIM (PP-HRIM) monitoring facilitates assessment of manometric responses to aversive digestive stimuli within a short time frame of less than 60 minutes. In recent years groups have defined objective HRIM criteria for transient lower esophageal sphincter relaxations (TLESRs), rumination syndrome, and supragastric belching7, 8. While research highlights PP-HRIM as an efficient and accurate diagnostic tool, the clinical applicability of PP-HRIM in identifying mechanisms of PPI non-response is unknown. Thus, the aims of this study were to investigate the distribution of postprandial profiles determined by PP-HRIM, and to identify patient features associated with postprandial profiles among a PPINR population.
Methods
Study Design & Subjects
This retrospective analysis examines all PP-HRIM studies performed on patients older than 18 years of age referred to a single tertiary care center for the evaluation of PPI non-response from January 2010 to May 2016. This protocol was approved by the Northwestern University Institutional Review Board.
Postprandial High-Resolution Impedance Manometry Protocol
Patients with persistent typical or atypical symptoms despite double dose PPI therapy who underwent a PP-HRIM study were included. All PP-HRIM studies were ordered by an esophagologist, predominantly for cases with a pre-test suspicion of a functional gastrointestinal disorder. All PP-HRIM studies followed a standardized HRIM protocol using a 36-channel solid-state catheter (Manoscan 360; Medtronic, Minneapolis, MN). First, patients were placed in the supine position and measurements were taken during a baseline phase followed by 10 swallows of 5-ml water. Next, patients were switched to a seated position, and measurements were taken during a baseline phase followed by 10 swallows of 5-ml water, and 200-ml water taken by rapid repeated swallows. Finally, patients ingested a solid refluxogenic test meal (the meal was self-identified by the patient as a meal that is typically symptom inducing) with postprandial monitoring up to 90 minutes. Studies were excluded if the manometry study did not include a minimum of seven technically adequate high quality wet swallows in the supine position or if the duration of postprandial monitoring was less than 20 minutes.
Each PP-HRIM study was independently reviewed by three members of the study team (RY, MT, JEP) using ManoView 3.0 to determine a motility diagnosis per Chicago Classification v3.09 and a postprandial diagnosis. Data from concurrent 24-hour pH-impedance monitoring performed on PPI therapy was collected when available.
Definitions & Groups
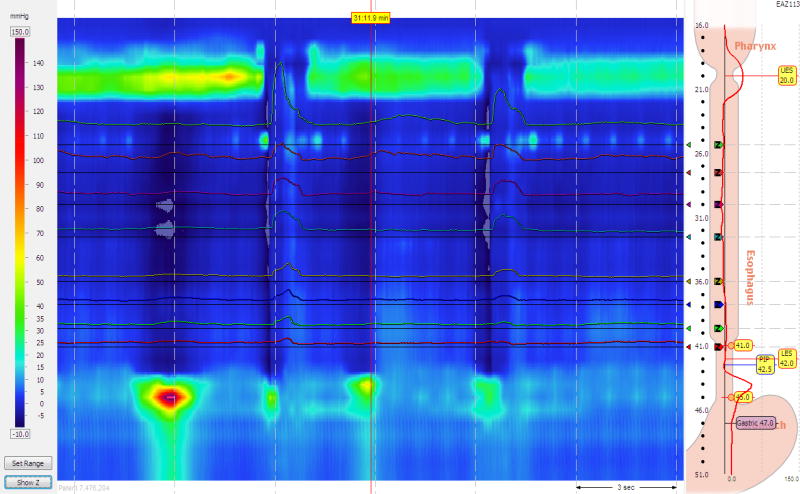
The following evidence based criteria was used to define manometric episodes: TLESR – lower esophageal sphincter (LES) relaxation in the absence of a swallow within 4s and 2s after the onset of LES relaxation associated with crural diaphragm inhibition and duration of LES relaxation lasting more than 10 seconds8; rumination – rise in intragastric pressure of at least 30 mmHg above baseline associated with a retrograde pressure gradient and return of gastric contents without retching proximal to the upper esophageal sphincter (UES) up to 10s after strain event7; supragastric belching –UES relaxation with aboral flow of air followed by rapid expulsion of air in the setting of either esophagogastric junction (EGJ) contraction and/or negative intra-thoracic pressure7 (Figure 1).
Figure 1.
Post-prandial events on high-resolution impedance manometry. A) Example of a transient lower esophageal sphincter with inhibition of the crural diaphragm and LES relaxation lasting for > 10 seconds, associated with a reflux episode (retrograde movement of gastric contents proximal to the LES). B) Example of a rumination episode with (1) rise in intragastric pressure > 30mmHg above baseline followed by (2) retrograde flow of gastric contents to the UES, with (3) increased esophageal pressure, and (4) UES relaxation. C) Example of a supragastric belch with (1) EGJ contraction, (2) negative intra-thoracic pressure, (3) UES relaxation, and (4) aboral flow of air as demonstrated by rise in impedance, and (5) retrograde movement and expulsion of air. Figure used with permission from the Esophageal Center at Northwestern’s Digestive Health Center.
Normative thresholds for the frequency of postprandial TLESR, rumination, and supragastric belches are not defined. Thus, in order to delineate thresholds for abnormal in this study, we examined data from a sub-group of our patients with no prior history of foregut surgery, no major esophageal motility disorder, an AET < 2.0% and less than 20 reflux events on impedance-pH testing, and no hiatal hernia as a representation of “normal” physiology and anatomy. We derived cut-offs from the 75th percentile data among this cohort to determine the abnormal frequency (number of episodes/hour) of TLESR, rumination episodes, and supragastric belches.
Outcomes
The primary outcome was postprandial diagnostic profile. PP-HRIM studies were a priori separated into four profiles: normal, reflux only, supragastric belch, or rumination. Normal group: normal frequency of TLESR episodes and an absence of abnormal rumination and/or supragastric belching. Reflux only: abnormal frequency of TLESR episodes in absence of abnormal rumination and/or supragastric belching. Supragastric belch: an abnormal frequency of supragastric belch episodes +/− abnormal frequency of TLESR episodes. Rumination: an abnormal frequency of rumination episodes +/− abnormal frequency of supragastric belch, +/− abnormal frequency of TLESR episodes.
Data Analysis
A complete case analysis was performed without a predetermined sample size; missing data was not imputed. The a priori goal for primary analysis was to identify independent predictors of postprandial diagnostic profile. As such, a univariate analysis examined differences in baseline clinical variables, physiologic data, and questionnaire scores between postprandial diagnostic profiles. One-way analysis of variance assessed variability among independent continuous variables and Chi Square examined differences in independent categorical variables. Covariates significant at P < 0.20 level were included in a multinomial logistic regression. P values < 0.05 in the regression model were considered statistically significant.
Since the postprandial diagnostic profiles were not based on standardized definitions or normative thresholds, we additionally examined the association between baseline variables and frequency of post-prandial events independent of classification by postprandial diagnostic profile. In this sensitivity analysis we performed multivariable linear regression modeling and included all variables (baseline clinical variables, physiologic data, and questionnaire scores) in the multivariable regression model. P values < 0.05 in the regression model were considered statistically significant.
Since patients that are status post foregut surgery or those with an EGJ outflow obstruction represent a unique mechanistic profile, we performed a post-hoc sub-analysis excluding this group of patients. One-way analysis of variance assessed variability among independent continuous variables and Chi Square examined differences in independent categorical variables.
All analyses were conducted using STATA 14.2 (StataCorp 2015, College Station, TX).
Results
Baseline Data
Overall, 99 PP-HRIM studies met protocol criteria. Among these, five studies uncovered a new diagnosis of achalasia and were excluded from the analysis. Of the 94 remaining studies, patients were a mean age of 45.5 ± 15.6 years and 58 (62%) were female. The most common indications for PP-HRIM included symptoms of regurgitation (54%), heartburn (26%), and dysphagia (25%). The majority of patients had normal esophageal motility (40%) or a minor motility disorder of ineffective esophageal motility or fragmented peristalsis (44%) (Table 1).
Table 1.
Baseline Clinical Data
| Baseline data | N=94 |
| Age (years) | 45.5 ± 15.6 |
| Female gender | 58 (62%) |
| Body mass index (kg/m2) (n=88) | 27.0 ± 7.5 |
| Prior foregut surgery | 13 (14%) |
| GerdQ Score (n=54) | 10 ± 2.8 |
| pH Impedance on PPI Data | |
| Subjects with a 24h pH-impedance study ON PPI available | 30 (32%) |
| Acid exposure on 24h pH-impedance ON PPI (n=30) | 5.7 ± 6.9 |
| Acidic reflux events | 6 (IQR 1–31) |
| Weakly acidic reflux events | 24 (IQR 9–38) |
| Study Indication | |
| Regurgitation | 50 (54%) |
| Heartburn | 24 (26%) |
| Dysphagia | 23 (25%) |
| Belching | 14 (15%) |
| Chest pain | 13 (14%) |
| Cough | 10 (11%) |
| Laryngeal symptoms | 10 (11%) |
| Manometric Findings | |
| Median IRP (mmHg) | 9.3 ± 6.9 |
| EGJ-CI (mmHg-s-cm) | 52.5 ± 32.9 |
| EGJ Morphology Type I | 70 (75%) |
| EGJ Morphology Type II | 20 (22%) |
| EGJ Morphology Type III | 3 (3%) |
| Normal Esophageal Motility | 37 (40%) |
| EGJ Outflow Obstruction | 12 (13%) |
| Absent Contractility | 2 (2%) |
| Hypercontractile Esophagus | 1 (1%) |
| Distal Esophageal Spasm | 1 (1%) |
| Minor Motility Disorder (Ineffective esophageal motility or fragmented peristalsis) | 41 (44%) |
| Post Prandial Testing | |
| TLESR episodes per 60 minutes | 4.7 (IQR 2.4–6.7) |
| Rumination episodes per 60 minutes | 0 (IQR 0-0) |
| Supragastric belch episodes per 60 minutes | 2.0 (IQR 0–7.6) |
| Post-prandial monitoring, minutes | 50 (32.5–60) |
Esophagogastric Junction (EGJ), Transient lower esophageal sphincter relaxation (TLESR); Proton pump inhibitor (PPI)
Postprandial Findings
The median duration of postprandial monitoring was 50 minutes (IQR 32.5–60 minutes). When averaged over 60 minutes of postprandial analysis there was a median of 4.7 (IQR 2.4–6.7) TLESR episodes, 0 (IQR 0-0) rumination episodes, and 2.0 (IQR 0.0–7.6) supragastric belches.
Derivation of Postprandial Thresholds and Profiles
Thirty-two patients had no prior history of foregut surgery, absence of a major esophageal motility disorder, an AET < 2.0%, less than 20 reflux events on impedance-pH monitoring, and did not have a hiatal hernia. Table 2 displays the frequencies of events for this ‘normal’ group. Based on this data we defined the threshold for abnormal frequencies (episodes/hour) as TLESR > 6, rumination > 0, and supragastric belch > 2. According to these thresholds, subjects were grouped as follows: 23 (24%) normal, 13 (14%) reflux only, 39 (42%) supragastric belch, and 19 (20%) rumination. Among the supragastric belch group 14 of 39 also had an abnormal frequency of TLESRs and among the rumination group, 2 of 19 had an abnormal frequency of TLESRs. In total, 42 (45%) had a functional disorder (supragastric belch and/or rumination) in absence of abnormal TLESR frequency.
Table 2.
Frequency of post-prandial episodes by percentile among 32 patients with impedance-pH monitoring with an acid exposure time <2.0 and less than 20 reflux events, and lack of hiatal hernia.
| Number of episodes/Hour |
Percentile | ||||
|---|---|---|---|---|---|
| 5th | 25th | 50th | 75th | 95th | |
| TLESR | 0 | 2.1 | 3.7 | 6.7 | 10.2 |
| Rumination | 0 | 0 | 0 | 0 | 8.6 |
| Supragastric belches | 0 | 0 | 0 | 3.5 | 38.3 |
Primary Analysis – Characteristics by Postprandial Profile
The primary unadjusted analysis is presented in Table 3. Variables significant at the p <0.20 level (age, EGJ-CI, regurgitation, dysphagia, chest pain, and belching) were included in a multinomial logistic regression. The normal group (54.7 ± 14.1 years) was significantly older in age compared to the supragastric belch (43.7 ± 13.8; OR 1.07 (95% CI 1.01 to 1.13), p=0.02) and rumination (36.6 ± 13.4; OR 1.08 (95% CI 1.02 to 1.14), p=0.01) groups. The reflux only group had a significantly lower EGJ contractile integral (31.0 ± 20.2 mmHg-cm) compared to the normal (59.6 ± 41.2 mmHg-cm; OR 0.96 (95% CI 0.92 to 1.00), p=0.02) and supragastric belch (60.7 ± 31.7 mmHg-cm; OR 0.96 (95% CI 0.92 to 1.00), p=0.01) groups. Patients with rumination were 19.7 times more likely to present with regurgitation compared to supragastric belchers (84% vs 45%, OR 19.7 (95% CI 17.4 to 22.0), p=0.01) and 11.6 times more likely to present with regurgitation compared to the reflux only group (84% vs 23%, OR 11.6 (95% CI 9.7 to 13.5), p=0.01). The normal group was 6.7 times more likely to present with dysphagia compared to the supragastric belchers (OR 6.7 (95% CI 5.0 to 8.4), p=0.03).
Table 3.
Predictors of Post-Prandial High Resolution Impedance Manometry Pattern
| Normal, (n=23) |
TLESR Only, (n=13) |
Supragastric Belch (± TLESR), (n=39) |
Rumination (± Supragastric belch; ±TLESR), (n=19) |
P-value | |
|---|---|---|---|---|---|
| Age (years) | 54.7 ± 14.1 | 46.9 ± 18.8 | 43.7 ± 13.8 | 36.6 ± 13.4 | <0.01 |
| Adjusted OR 1.07 (95% CI 1.01–1.13)‡ | Adjusted OR 1.08 (95% CI 1.02–1.14)‡ | ||||
| Female gender | 16 (70%) | 7 (54%) | 22 (56%) | 13 (68%) | 0.62 |
| Prior foregut surgery | 3 (13%) | 3 (23%) | 6 (15%) | 1 (5%) | 0.53 |
| Body mass index (kg/m2) | 28.9 ± 9.2 | 25.2 ± 5.5 | 26.7 ± 7.2 | 26.0 ± 6.5 | 0.47 |
| GerdQ Score | 9.3 ± 2.4 | 9.8 ± 2.4 | 10.2 ± 3.2 | 11.3 ± 1.7 | 0.61 |
| Hiatal hernia > 3cm | 7 (32%) | 2 (15%) | 8 (21%) | 6 (33%) | 0.52 |
| EGJ Contractile Integral (mmHg-cm) | 59.6 ± 41.2 | 31.0 ± 20.2 | 60.7 ± 31.7 | 45.7 ± 25.7 | 0.02 |
| Adjusted OR 0.96 (95% CI 0.92–1.00)‡$ | |||||
| EGJ Outflow Obstruction on Manometry | 5 (22%) | 2 (15%) | 4 (11%) | 1 (6%) | 0.40 |
| Symptoms | |||||
| Regurgitation | 14 (61%) | 3 (23%) | 17 (45%) | 16 (84%) | <0.01 |
| Adjusted OR 19.7 (95%CI 17.4 to 22.0)$; Adjusted OR 11.6 (95% CI 9.7 to 13.5)† | |||||
| Heartburn | 4 (17%) | 5 (38%) | 10 (26%) | 5 (26%) | 0.58 |
| Dysphagia | 10 (43%) | 3 (23%) | 7 (18%) | 3 (16%) | 0.10 |
| Adjusted OR 6.7 (95% CI 5.0 to 8.4)$ | |||||
| Chest pain | 3 (13%) | 5 (38%) | 5 (13%) | 0 (0%)¥ | 0.02 |
| Belching | 0 (0%) | 3 (23%) | 3 (8%) | 1 (5%) | 0.09 |
| Cough | 4 (17%) | 0 (0%) | 5 (13%) | 1 (5%) | 0.33 |
| Extraesophageal symptoms alone | 1 (4%) | 2 (15%) | 6 (15%) | 1 (5%) | 0.43 |
| Post-prandial findings | |||||
| Duration of post-prandial monitoring | 52.6 ± 18.8 | 52.4 ± 18.4 | 48.4 ± 19.0 | 36.3 ± 16.3‡ | 0.03 |
| Frequency of TLESR episodes per 60 minutes | 3.7 ± 1.9 | 8.9 ± 4.6 | 4.8 ± 3.1 | 3.0 ± 2.4 | <0.01 |
| Frequency of rumination episodes per 60 minutes | 0 ± 0 | 0.1 ± 0.2 | 0 ± 0 | 23.1 ± 26.3 | <0.01 |
| Frequency of supragastric belch episodes per 60 minutes | 0.3 ± 0.6 | 0.4 ± 0.5 | 19.6 ± 32.7 | 6.6 ± 12.2 | <0.01 |
| 24h pH impedance on PPI therapy | |||||
| Acid exposure time | 6.4 ± 6.6 | 4.3 ± 1.5 | 5.2 ± 7.7 | 8.1 ± 6.8 | 0.90 |
| Acidic reflux events | 11.1 ± 14.8 | 24.0 ± 26.9 | 14.8 ± 20.0 | 26.0 ± 23.9 | 0.64 |
| Weakly acidic reflux events | 28.9 ± 24.2 | 16.5 ± 16.3 | 32.3 ± 33.1 | 87.7 ± 125.9 | 0.24 |
p <0.05 compared to TLESR;
p <0.05 compared to normal;
p<0.05 compared to supragastric belch.
Esophagogastric Junction (EGJ), Transient lower esophageal sphincter relaxation (TLESR); Proton pump inhibitor (PPI)
Sensitivity Analysis – Factors Associated with Postprandial Episodes
Table 4 depicts the multivariable regression model including all covariates. Presence of regurgitation was associated with a mean difference of +7.26 rumination episodes/hour (β 7.26 (95% CI 1.32 to 13.20); p=0.02). In addition, each weakly acidic reflux event on pH-impedance monitoring performed on PPI was associated with +0.12 rumination episodes/hour (β 0.12 (95% CI 0.08 to 0.16); p<0.01) and +0.24 supragastric belches/hour (β 0.24 (95% CI 0.08 to 0.40);p<0.01).
Table 4.
Multivariable linear regression examining predictors of post-prandial episodes
| TLESR Episodes | Rumination Episodes |
Supragastric Belch Episodes |
||||
|---|---|---|---|---|---|---|
| β (95% CI) |
P- value |
β (95% CI) |
P- value |
β (95% CI) | P- value |
|
| Age | −0.01 (−0.05 to 0.03) | 0.53 | −0.19 (−0.39 to 0.01) | 0.07 | −0.29 (−0.60 to 0.02) | 0.07 |
| Female gender | 0.12 (−1.33 to 1.57) | 0.87 | −1.16 (−7.37 to 5.05) | 0.72 | −3.55 (−13.27 to 6.17) | 0.48 |
| Body mass index | −0.08 (−0.18 to 0.02) | 0.11 | −0.19 (−0.62 to 0.24) | 0.38 | −0.30 (−0.99 to 0.39) | 0.39 |
| Regurgitation | −0.67 (−2.06 to 0.72) | 0.35 | 7.26 (1.32 to 13.20) | 0.02 | 3.75 (−5.83 to 13.33) | 0.45 |
| Heartburn | 0.46 (−1.15 to 2.07) | 0.58 | 1.90 (−5.02 to 8.82) | 0.59 | 4.53 (−6.31 to 15.37) | 0.42 |
| Dysphagia | −0.47 (−2.10 to 1.16) | 0.57 | −3.98 (−11.0 to 3.0) | 0.27 | −4.51 (−15.51 to 6.49) | 0.42 |
| Chest pain | 1.37 (−0.65 to 3.39) | 0.18 | −5.43 (−14.11 to 3.25) | 0.22 | −7.80 (−21.44 to 5.84) | 0.27 |
| Belching | 1.73 (−0.92 to 4.38) | 0.20 | −4.61 (−16.08 to 6.86) | 0.43 | −6.04 (−24.05 to 11.97) | 0.51 |
| Cough | 0.82 (−1.43 to 3.07) | 0.48 | −5.18 (−14.96 to 4.60) | 0.30 | 7.78 (−7.61 to 23.17) | 0.32 |
| Extraesophageal symptoms | 0.49 (−1.78 to 2.76) | 0.67 | −4.71 (−14.45 to 5.03) | 0.35 | −2.45 (−17.82 to 12.92) | 0.76 |
| GerdQ Score | −0.15 (−0.42 to 0.12) | 0.27 | 0.04 (−0.06 to 0.14) | 0.40 | 3.62 (1.23 to 6.01) | <0.01 |
| Baseline EGJ Pressure | −0.01 (−0.07 to 0.05) | 0.70 | −0.04 (−0.31 to 0.23) | 0.77 | −0.34 (−0.75 to 0.07) | 0.11 |
| EGJ Contractile Integral | 0.00 (−0.02 to 0.02) | 0.70 | −0.02 (−0.12 to 0.08) | 0.78 | −0.02 (−0.12 to 0.08) | 0.76 |
| Median Integrated Relaxation Pressure | −0.10 (−0.20 to −0.00) | 0.06 | −0.24 (−0.67 to 0.19) | 0.28 | −0.49 (−1.18 to 0.20) | 0.17 |
| Acid exposure time* | 0.05 (−0.17 to 0.27) | 0.68 | 0.16 (−0.21 to 0.53) | 0.41 | −0.49 (−1.73 to 0.74) | 0.44 |
| Number of acidic reflux events* | 0.04 (−0.04 to 0.12) | 0.39 | 0.11 (−0.03 to 0.25) | 0.11 | 0.11 (−0.34 to 0.56) | 0.63 |
| Number of weakly acidic reflux events* | −0.02 (−0.06 to 0.02) | 0.26 | 0.12 (0.08 to 0.16) | <0.01 | 0.24 (0.08 to 0.40) | <0.01 |
Results from impedance-pH monitoring performed on PPI therapy.
Esophagogastric Junction (EGJ).
Sub-analysis Excluding Patients with a History of Foregut Surgery of Outflow Obstruction
Twenty-two of 94 patients had an EGJ outflow obstruction on manometry and/or a history of prior foregut surgery, and were excluded from the sub-analysis. Of the remaining 72, the postprandial profiles were: 15 (21%) Normal, 9 (13%) reflux only, 31 (43%) supragastric belch, and 17 (24%) rumination. The results are displayed in supplemental Table 1. Briefly, compared to the other groups, the normal group was older in age and supragastric belchers had the highest EGJ contractile integral. The rumination group was more likely to present with regurgitation compared to the other groups. In addition, chest pain was less frequently seen among supragastric belchers and ruminators compared to the refluxers.
Discussion
The management of PPI non-responders is a major health care challenge. After failing PPI optimization, patients often undergo various paths including diagnostic testing with endoscopy and reflux testing, referral to tertiary care centers, consideration for anti-reflux interventions, and/or indefinite PPI therapy1, 10. In many cases, these strategies fail to clarify the underlying mechanism of PPI non-response or improve outcomes. This study assessed 94 PP-HRIM studies performed at a tertiary care esophageal referral center in patients referred for PPI non-response in order to examine the diagnostic utility of PP-HRIM. PP-HRIM detected an abnormal postprandial pattern in 76% of patients, with 62% of cases exhibiting a behavioral pattern – 42% with supragastric belching and 20% with rumination. Patients demonstrating behavioral patterns were younger, and those with rumination presented more commonly with regurgitation.
Understanding mechanisms of reflux symptoms is essential, as treatment strategies differ accordingly. For instance, among the 14% of the cohort with reflux only, management options include TLESR inhibition and potentially anti-reflux interventions10. On the other hand, for the 45% (n=42) with an abnormal frequency of rumination and/or supragastric belching in the absence of increased TLESR episodes, management should focus on behavioral treatment strategies such as diaphragmatic breathing, speech therapy and hypnosis. Importantly, this is a group that may not require long-term PPI therapy or anti-reflux interventions4. For the 17% of subjects with reflux and behavioral overlap it would be reasonable to consider a combined approach of TLESR inhibition, optimization of acid-suppression, and behavioral therapy, reserving invasive interventions as a second-line option. Elucidating post-prandial profiles may also have investigative value. For instance, despite optimism for lesogaberan as an effective TLESR inhibitor for PPI non-response, a clinical trial in 2010 examining lesogaberan reported considerable variability in the number of TLESRs among subjects and a small (8%) therapeutic gain. It is possible that patients with functional heartburn, rumination and/or supragastric belching diluted the study group 11, 12. Future studies could benefit from using PP-HRIM to select representative patient populations.
In this study, we performed a primary analysis as well as sensitivity and sub-analyses in attempt to identify predictors of postprandial patterns. Overall, EGJ contractility as measured by the EGJ-CI was lowest among refluxers, with the mean EGJ-CI falling below published normative values of 39 mmHg-cm13. These results are consistent with prior literature demonstrating lower EGJ-CI among GERD patients13, 14. In contrast, the EGJ-CI was high among supragastric belchers and the normal group, suggesting that dysfunction of the anti-reflux barrier is not a driver of supragastric belching. In addition, the rumination group demonstrated a borderline mean EGJ-CI of 46 mmHg-cm. While EGJ-CI values in rumination have not been previously reported, prior studies do report lower resting EGJ pressures among patients with rumination6, 15. Our data further corroborates the idea that patients with rumination do not have an intact anti-reflux barrier or reflex arc.
The study results also support pre-existing notions regarding the relationship between symptoms and underlying mechanism. For instance, patients with rumination were more likely to present with regurgitation compared to the other groups whereas patients with rumination never presented with chest pain. Although not statistically significant, a greater portion of normal patients presented with dysphagia and also were found to have EGJ outflow obstruction on manometry. TLESR is the primary mechanism of gastric belching, and in this study belching was most commonly encountered among refluxers.
In addition, both rumination episodes and supragastric belches were associated with an elevated number of weakly acidic reflux events. Belches are identifiable on a careful evaluation of combined impedance-pH monitoring as impedance detects direction of flow and discerns liquid from gas 5. However, impedance-pH monitoring is limited by an inability to measure pressure and gradient alterations in the esophageal body. As such, rumination episodes may be misinterpreted as reflux events and/or elevated acid exposure on pH-impedance leading to a misdiagnosis of GERD or esophageal hypersensitivity.
These study findings suggest that PP-HRIM should be included in the armamentarium of diagnostic tools to evaluate PPI non-response, particularly when a primary behavioral or overlap profile is suspected. In order for PP-HRIM to be easily adopted and used in the clinical setting, future work is needed to identify the optimal clinical postprandial protocol such as meal type, monitoring period, and role of provocation, the normative thresholds for frequency of events, and the inter-rater diagnostic reliability. In our study, most postprandial profiles were apparent within 20 minutes of monitoring, and the duration of postprandial monitoring was shorter among rumination and supragastric belches supporting the idea that early pattern detection resulted in early study termination. Similar to reflux monitoring, it would be interesting to measure symptom association with postprandial evetns to understand which episodes carry clinical significance. While appropriate diagnosis is paramount, it is even more important that we develop pragmatic strategies to effectively treat these patients. Future studies should examine treatment impacts on patient outcomes, health care utilization and costs.
This study has important strengths and limitations. Generalizability of this study is limited due to referral and selection biases. The data likely overestimates the prevalence of rumination and/or belching disorders in the general gastroenterology setting as the study was performed at a single urban academic esophageal referral center and PP-HRIM studies were performed for a pre-test suspicion of a behavioral disorder. However, the patient mix is diverse and adequately representative of referrals to tertiary care centers for evaluation of ongoing PPI non-response. Since thresholds for postprandial diagnoses are not available, we defined postprandial groups based on our ‘normative’ cohort. In an attempt to address this limitation, we performed a sensitivity analysis examining the number of postprandial episodes linearly. In addition, the postprandial meal content and duration were not standardized. However, patients were given options of refluxogenic meals and we excluded studies with less than 20 minutes of monitoring. Given the retrospective nature of the study, we do not have complete reflux testing data prior to PP-HRIM testing for all patients which limits our ability to discern the presence of underlying GERD based on pH-metry, however, we do include data for the subset of patients for whom we performed pH-MII.
In conclusion, a significant portion of patients with PPI non-response may suffer from rumination or belching disorders and PP-HRIM offers an efficient and sophisticated method to evaluate underlying mechanisms of PPI non-response. Clinicians should consider performing or referring for PP-HRIM studies in PPINRs, particularly when the etiology of non-response is not forthcoming, in the setting of a history or suspicion of behavioral disorders, in younger patients presenting with regurgitation and in patients with elevated weakly acidic reflux events on pH-impedance monitoring.
Supplementary Material
Acknowledgments
Funding: RY & JEP supported by NIH R01DK092217-04A1 (JEP)
Abbreviations
- EGJ
Esophagogastric junction
- GERD
Gastroesophageal reflux disease
- HRIM
High resolution impedance manometry
- LES
Lower esophageal sphincter
- PPI
Proton pump inhibitor
- PPINRs
PPI non-responders
- PP-HRIM
Postprandial high-resolution impedance manometry
- TLESRs
Transient lower esophageal sphincter relaxations
- UES
Upper esophageal sphincter
Footnotes
Potential Conflict of Interest (Financial, Professional or Personal): None
Writing Assistance: None
Specific Author Contributions
RY: Study oversight; study concept and design; acquisition of data; analysis and interpretation of data; drafting of manuscript; critical revision of the manuscript for important intellectual content; finalization of manuscript.
MT: Study concept and design; acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; finalization of manuscript.
SR: Study concept and design; interpretation of data; critical revision of the manuscript for important intellectual content; finalization of manuscript.
KR: Acquisition of data; critical revision of the manuscript for important intellectual content; finalization of manuscript.
PJK: Interpretation of data; critical revision of the manuscript for important intellectual content; finalization of manuscript.
JEP: Study concept and design; analysis and interpretation of data; drafting of manuscript; critical revision of the manuscript for important intellectual content; finalization of manuscript.
References
- 1.Cicala M, Emerenziani S, Guarino MP, et al. Proton pump inhibitor resistance, the real challenge in gastro-esophageal reflux disease. World J Gastroenterol. 2013;19:6529–35. doi: 10.3748/wjg.v19.i39.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bravi I, Woodland P, Gill RS, et al. Increased prandial air swallowing and postprandial gas-liquid reflux among patients refractory to proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2013;11:784–9. doi: 10.1016/j.cgh.2012.12.041. [DOI] [PubMed] [Google Scholar]
- 3.Herregods TV, Troelstra M, Weijenborg PW, et al. Patients with refractory reflux symptoms often do not have GERD. Neurogastroenterol Motil. 2015;27:1267–73. doi: 10.1111/nmo.12620. [DOI] [PubMed] [Google Scholar]
- 4.Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal Disorders. Gastroenterology. 2016;150:1380–92. doi: 10.1053/j.gastro.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Kessing BF, Bredenoord AJ, Smout AJ. The pathophysiology, diagnosis and treatment of excessive belching symptoms. Am J Gastroenterol. 2014;109:1196–203. doi: 10.1038/ajg.2014.165. (Quiz) 1204. [DOI] [PubMed] [Google Scholar]
- 6.Halland M, Parthasarathy G, Bharucha AE, et al. Diaphragmatic breathing for rumination syndrome: efficacy and mechanisms of action. Neurogastroenterol Motil. 2016;28:384–91. doi: 10.1111/nmo.12737. [DOI] [PubMed] [Google Scholar]
- 7.Kessing BF, Bredenoord AJ, Smout AJ. Objective manometric criteria for the rumination syndrome. Am J Gastroenterol. 2014;109:52–9. doi: 10.1038/ajg.2013.428. [DOI] [PubMed] [Google Scholar]
- 8.Roman S, Holloway R, Keller J, et al. Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry. Neurogastroenterol Motil. 2016 doi: 10.1111/nmo.12920. [DOI] [PubMed] [Google Scholar]
- 9.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. doi: 10.1111/nmo.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scarpellini E, Ang D, Pauwels A, et al. Management of refractory typical GERD symptoms. Nat Rev Gastroenterol Hepatol. 2016;13:281–94. doi: 10.1038/nrgastro.2016.50. [DOI] [PubMed] [Google Scholar]
- 11.Boeckxstaens GE, Beaumont H, Mertens V, et al. Effects of lesogaberan on reflux and lower esophageal sphincter function in patients with gastroesophageal reflux disease. Gastroenterology. 2010;139:409–17. doi: 10.1053/j.gastro.2010.04.051. [DOI] [PubMed] [Google Scholar]
- 12.Boeckxstaens GE, Denison H, Jensen JM, et al. Translational gastrointestinal pharmacology in the 21st century: 'the lesogaberan story'. Curr Opin Pharmacol. 2011;11:630–3. doi: 10.1016/j.coph.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Nicodeme F, Pipa-Muniz M, Khanna K, et al. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353–60. doi: 10.1111/nmo.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil. 2015;27:1423–31. doi: 10.1111/nmo.12638. [DOI] [PubMed] [Google Scholar]
- 15.Soykan I, Chen J, Kendall BJ, et al. The rumination syndrome: clinical and manometric profile, therapy, and long-term outcome. Dig Dis Sci. 1997;42:1866–72. doi: 10.1023/a:1018854925196. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.