Abstract
Background
Although individuals classified as non-resident aliens, including undocumented immigrants, are entitled to receive emergency dialysis in the United States regardless of their ability to pay, most states do not provide them with subsidized care for maintenance dialysis or kidney transplantation. We explored whether non-resident aliens have similar outcomes to US citizens after receiving kidney transplants covered by Medicaid, a joint federal and state health insurance program.
Study Design
Retrospective observational cohort study.
Setting & Participants
All adult Medicaid patients in the US Renal Data System who received their first kidney transplant during 1990–2011.
Predictor
Citizenship status, categorized as US citizen, non-resident alien, or permanent resident.
Outcomes
All-cause graft loss.
Measurements
HRs and 95% CIs estimated by applying Cox proportional hazards frailty models with transplant center as a random effect.
Results
Of 10,495 patients, 8660 (82%) were US citizens, 1489 (14%) were permanent residents, and 346 (3%) were non-resident aliens, whom we assumed were undocumented immigrants. Non-resident aliens were younger, healthier, on dialysis longer, and more likely to have had a living donor. 71% had transplantation in California, and 61% had transplantation after 2005. Non-resident aliens had a lower unadjusted risk of graft loss compared to US citizens (HR, 0.48; 95% CI, 0.35–0.65). Results were attenuated but still significant when adjusted for demographics, comorbidities, dialysis, and transplant-related factors (HR, 0.67; 95% CI, 0.46–0.94).
Limitations
Citizenship status was self-reported, possible residual confounding.
Conclusions
Our study suggests that the select group of insured non-resident aliens who undergo transplantation with Medicaid do just as well as US citizens with Medicaid. Policymakers should consider expanding coverage for kidney transplantation in nonresident aliens, including undocumented immigrants, given the associated high quality outcomes in these patients.
Keywords: kidney transplantation, transplant outcomes, undocumented immigrants, non-resident aliens, citizenship, US health care policy, Medicaid, immigration, end-stage renal disease (ESRD)
Introduction
An estimated 6,000 undocumented immigrants in the United States have end-stage kidney disease (ESKD) based on 2014 data.1–3 Although the U.S. provides life-sustaining maintenance dialysis for virtually all of its citizens with ESKD, the care for undocumented immigrants is fragmented.1 While some states extend the benefit of scheduled, maintenance dialysis to undocumented immigrants, most states only dialyze them when their condition is acutely life-threatening, a situation under which federal funding may be used to cover costs.1
Access to kidney transplantation for this population is even more limited as there is no federal mandate to subsidize kidney transplantation for non-citizens.4 This is despite the fact that transplantation is a more cost-effective form of renal replacement therapy and provides better outcomes for patients with ESKD.5,6,7 Although some states provide funding for kidney transplantation for this population, most undocumented immigrants must rely on either charitable donations or private insurance to cover the costs of this procedure, making it unfeasible for the vast majority of these patients.8 Little is known about the outcomes of undocumented immigrant recipients of kidney transplants. Critics have voiced concerns that undocumented immigrants would not do well since they are subject to deportation, which could disrupt the social and financial stability necessary for proper post-transplantation healthcare.9
We hypothesized that undocumented immigrants would have similar outcomes to US citizens following kidney transplantation if they were equally insured. To test this, we analyzed a cohort of patients with Medicaid, a joint federal and state health insurance program for low-income patients, who received their first kidney transplant from 1990 through 2011. We compared the outcomes of presumed undocumented immigrants to those of US citizens.
Methods
Data Source and Study Population
From the US Renal Data System (USRDS), a national database of virtually all patients with ESKD, we identified all adult (18 years or older) patients with ESKD who received their first kidney transplant from January 1, 1990, through December 31, 2011 (Figure S1, available as online supplementary material). We excluded patients who underwent transplantation after 2011 because the categories for recording citizenship status were changed in 2012 to a combination of US citizen/non-US citizen and US resident/non-US resident, such that undocumented immigrants would be indistinguishable from permanent residents (since both would be listed as non-US citizen/US resident).10 By restricting the cohort to patients whose primary payer was Medicaid, we also minimized the inclusion of patients who traveled to the United States for the purpose of transplantation, as it would be unlikely that such “transplant tourists” would qualify for Medicaid.
Exposure and Outcomes
The primary exposure of interest was recipient citizenship status, which was self-reported on the Transplant Candidate Registration form (US citizen versus resident alien versus non-resident alien). The three-category exposure was used for all analyses. We considered resident aliens to be permanent residents, or individuals who are allowed to live and work in the United States indefinitely. We assumed non-resident aliens to be undocumented immigrants.
To assess the validity of the citizenship variable from the Transplant Candidate Registration form, we reviewed the medical records of all patients covered by Medicaid who had received a kidney transplant from 2009–2011 at a single center to find their UNOS registration number. For logistical reasons, we were unable to access records at other transplant centers. Whereas US citizens and permanent residents are registered in UNOS using their social security number, non-resident aliens are given UNOS registration numbers beginning with 9FN. We also reviewed the social work evaluations to determine whether patients had traveled to the United States for the purpose of receiving a transplant.
For the survival analyses, our primary outcome was all-cause graft failure. We analyzed non-fatal graft failure and all-cause mortality individually as secondary outcomes. We treated death as a competing event for non-fatal graft failure. All outcomes we ascertained from the USRDS transplant file.
Patient Characteristics
We obtained demographics, dialysis characteristics, comorbidities, transplant characteristics, and donor characteristics from the USRDS transplant files. These data are derived from the Organ Procurement and Transplantation Network (OPTN) candidates, recipients, donors, and histocompatibility files.
Statistical Analysis
We tabulated transplant recipient characteristics by citizenship status using frequencies and percentages and means ± standard deviations or medians (interquartile range) and compared the groups using ANOVA or the Kruskall-Wallis test for continuous variables, and Chi-square or Fisher’s exact test for categorical variables, as appropriate.
We used Cox proportional hazards frailty models with transplant center as a random effect to estimate the hazard ratio (HR) for all-cause graft failure and all-cause mortality in non-resident aliens versus US citizens. In the presence of the competing event of death, we used cause-specific hazards frailty models with transplant center as a random effect to estimate the cause-specific HRs for non-fatal graft failure by treating the competing event as censoring. We defined the index date as the date of transplantation. Patients were censored after 5 years of follow-up or on end of study (January 1, 2012), whichever was earlier. All HRs were accompanied by their corresponding 95% confidence interval (CI).
We created the following models: 1) unadjusted analysis (citizenship status only), 2) adjusted for demographics (age at transplantation, sex, and race/ethnicity), 3) model 2 plus dialysis factors (years on dialysis pre-transplantation and cause of kidney failure), 4) model 3 plus transplant factors (HLA 0-mismatch [versus any mismatch], living [versus deceased] donor, transplantation before year 2000 [versus year 2000 or after]), and 5) model 4 plus comorbidity count (number of comorbidities a patient has).
We assessed effect modification by living (versus deceased) donor, age (< or ≥ 50 years), and race/ethnicity separately by including an interaction term between the variable of interest and citizenship in the full model. Age was treated as a binary variable in the effect modification analyses to ease interpretation.
Sensitivity Analyses
We conducted two sensitivity analyses. In the first, given the potential for misclassification of non-resident aliens as permanent residents and vice versa, we conducted analyses combining these two groups and comparing them against US citizens. Since we cannot capture outcomes of non-resident aliens who leave the United States and do not return, this may bias the results towards a beneficial association with non-resident alien status. Thus, we conducted a second set of sensitivity analyses restricting the outcomes to 1- and 3- year survival, since the shorter the follow-up time, the less likely patients will have left the country.
All analyses were performed using R v. 3.3.0 (R Foundation for Statistical Computing; http://www.r-project.org). The Institutional Review Board of the Los Angeles Biomedical Institute at Harbor-UCLA Medical Center approved the study and waived the requirement for written consent owing to the de-identified nature of the data.
Results
Patient Characteristics
Out of the 278,779 adult patients who received their first kidney transplant from 1990 to 2011, Medicaid was the primary payer for 10,495 (Figure S1). Of these patients, 8,660 (82.4%) were US citizens, 1489 (14.2%) were permanent residents, and 346 (3.3%) were non-resident aliens (Table 1). Non-resident aliens were younger and more likely to be male and Hispanic than both US citizens and permanent residents. They generally had better functional status and were less likely to have comorbid conditions despite having spent more time on maintenance dialysis prior to transplantation. The panel reactive antibody (PRA) profiles of non-resident aliens did not differ significantly from those of US citizens, and they were more likely to have blood type O and to have received a 0-HLA-mismatched kidney. There was a longer duration of time for non-resident aliens to get waitlisted and undergo transplantation, with a higher proportion having transplantation in more recent years. Two hundred ten (61%) non-resident aliens underwent transplantation after 2005, while only 3704 (36%) of permanent resident and US citizen recipients had transplantation after 2005. Non-resident aliens were also more likely to have had living donors (40% vs. 32% of U.S. citizens and 27% of permanent residents). Like their recipients, donors of non-resident aliens tended to be younger, Hispanic, and to be permanent residents or non-resident aliens themselves. Non-resident aliens received transplants in 20 states, with 71% having transplantation in California, the state with the highest percentage of Medicaid-funded transplantations that went to nonresident aliens (Figure 1, Table S1).
Table 1.
Baseline characteristics of adult patients on Medicaid who received kidney transplants from 1990–2011.
| US citizens | Permanent residents | Nonresident aliens | P-value | ||
|---|---|---|---|---|---|
| (n=8660) | (n=1489) | (n=346) | |||
| Demographics | |||||
| Age, y | 42.0 [31.0–53.0] | 46.0 [34.0–57.0] | 34.5 [27.0–49.0] | <0.001 | |
| Male Sex | 4364 (50.4%) | 835 (56.1%) | 219 (63.3%) | <0.001 | |
| Race/Ethnicity | <0.001 | ||||
| Hispanic | 1766 (20.4%) | 890 (59.8%) | 265 (76.6%) | ||
| Non-Hispanic black | 2899 (33.5%) | 122 (8.2%) | 34 (9.8%) | ||
| Non-Hispanic white or other | 3995 (46.1%) | 477 (32.0%) | 47 (13.6%) | ||
| Dialysis Characteristics | |||||
| Dialysis Modalityb | <0.001 | ||||
| No dialysis | 1802 (20.8%) | 127 (8.5%) | –c | ||
| Hemodialysis | 5796 (66.9%) | 1195 (80.3%) | 289 (83.5%) | ||
| Peritoneal dialysis | 866 (10.0%) | 147 (9.9%) | 44 (12.7%) | ||
| Primary Cause of ESKD | <0.001 | ||||
| Other | 5107 (59.0%) | 904 (60.7%) | 214 (61.8%) | ||
| Diabetes | 2027 (23.4%) | 276 (18.5%) | 41 (11.8%) | ||
| Unknown | 1526 (17.6%) | 309 (20.8%) | 91 (26.3%) | ||
| Dialysis vintage of <1 Y before Transplantationd | 4842 (55.9%) | 568 (38.1%) | 120 (34.7%) | <0.001 | |
| Comorbidities | |||||
| Peripheral Vascular Diseasee | 277 (3.2%) | 47 (3.2%) | –c | >0.05f | |
| Cerebrovascular Diseaseg | 224 (2.6%) | 27 (1.8%) | –c | <0.05f | |
| Lung Disease (COPD)h | 98 (1.1%) | 11 (0.7%) | –c | <0.05f | |
| Canceri | 147 (1.7%) | 14 (0.9%) | –c | <0.05f | |
| Diabetesj | 3135 (36.5%) | 439 (29.5%) | 59 (17.1%) | <0.001 | |
| Functional Status | <0.001 | ||||
| NYHA I or II | 6812 (78.7%) | 1228 (82.5%) | 310 (89.6%) | ||
| NYHA III | 804 (9.3%) | 91 (6.1%) | 13 (3.8%) | ||
| NYHA IV | 191 (2.2%) | 68 (4.6%) | –c | ||
| Unknown | 853 (9.8%) | 102 (6.9%) | 18 (5.2%) | ||
| Comorbidity Count | 0.7 (0.5) | 0.8 (0.5) | 0.9 (0.4) | ||
| Transplant Characteristics | |||||
| <1 Y from Dialysis to Waitlistk | 4555 (52.6%) | 581 (39.0%) | 109 (31.5%) | <0.001 | |
| Transplant Date before 2000 | 2589 (29.9%) | 346 (23.2%) | 38 (11.0%) | <0.001 | |
| Deceased Donor | 5900 (68.1%) | 1094 (73.5%) | 206 (59.5%) | <0.001 | |
| >80% PRAl | 216 (2.5%) | 53 (3.6%) | –c | >0.05f | |
| 0-mismatch HLAm | 875 (10.1%) | 174 (11.7%) | 58 (16.8%) | <0.001 | |
| BMI, kg/m2n | 26.2 (5.2) | 25.1 (4.7) | 24.2 (4.4) | <0.001 | |
| Multiple Organ Recipient | 537 (6.2%) | 48 (3.2%) | –c | <0.001 | |
| ABO Blood Group | <0.001 | ||||
| A | 3119 (36.0%) | 486 (32.6%) | 98 (28.3%) | ||
| AB | 440 (5.1%) | 76 (5.1%) | 22 (6.4%) | ||
| B | 1206 (13.9%) | 212 (14.2%) | 34 (9.8%) | ||
| O | 3895 (45.0%) | 715 (48.0%) | 192 (55.5%) | ||
| Cold ischemia time of >14 ho | 3487 (40.3%) | 643 (43.2%) | 122 (35.3%) | 0.075 | |
| Donor Characteristics | |||||
| Donor Age, yp | 36.6 (15.4) | 37.0 (15.6) | 34.5 (15.7) | 0.02 | |
| Male Donorq | 4732 (54.6%) | 838 (56.3%) | 197 (56.9%) | 0.4 | |
| Donor Racer | <0.001 | ||||
| White | 6106 (70.5%) | 849 (57.0%) | 165 (47.7%) | ||
| Black | 1509 (17.4%) | 137 (9.2%) | 25 (7.2%) | ||
| Other | 1028 (11.9%) | 502 (33.7%) | 156 (45.1%) | ||
| Hispanic Donor | 1766 (20.4%) | 890 (59.8%) | 265 (76.6%) | <0.001 | |
| Donor Citizenship | <0.001 | ||||
| US citizen | 8181 (94.5%) | 1164 (78.2%) | 226 (65.3%) | ||
| Resident alien | 215 (2.5%) | 200 (13.4%) | 51 (14.7%) | ||
| Non-resident alien | 126 (1.5%) | 87 (5.8%) | 62 (17.9%) | ||
| Donor Serum Creatinine, mg/dLs | 1.1 (1.1) | 1.1 (1.0) | 1.0 (0.8) | 0.7 | |
Note: Values for categorical variables are given as number (percentage); values for continuous variables, as mean ± standard deviation or median [Q1–Q3].
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ESKD, end-stage kidney disease; NYHA, New York Health Association; PRA, panel reactive antibody
Missing for 196 US citizens, 20 permanent residents, and <10 non-resident aliens.
Per federal research regulations, any cell counts <10 must not be reported.
Missing for 426 US citizens, 69 permanent residents, and 11 non-resident aliens.
Missing for 1007 US citizens, 140 permanent residents, and 19 non-resident aliens.
We have masked the specific p-values to prevent the N<10 cells from being calculated.
Missing for 1218 US citizens, 175 permanent residents, and 36 non-resident aliens.
Missing for 897 US citizens, 125 permanent residents, and 17 non-resident aliens.
Missing for 956 US citizens, 126 permanent residents, and 16 non-resident aliens.
Missing for 641 US citizens, 100 permanent residents, and 13 non-resident aliens.
Missing for 1089 US citizens, 136 permanent residents, and 34 non-resident aliens.
Missing for 772 US citizens, 52 permanent residents, and 16 non-resident aliens.
Missing for 250 US citizens, 55 permanent residents, and 16 non-resident aliens.
Missing for 1629 US citizens, 247 permanent residents, and 53 non-resident aliens.
Missing for 1405 US citizens, 205 permanent residents, and 61 non-resident aliens.
Missing for 15 US citizens, 0 permanent residents, and 0 non-resident aliens.
Missing for 15 US citizens, 0 permanent residents, and 0 non-resident aliens.
Missing for 17 US citizens, <10 permanent residents, and 0 non-resident aliens.
Missing for 760 US citizens, 107 permanent residents, and 11 non-resident aliens.
Figure 1.
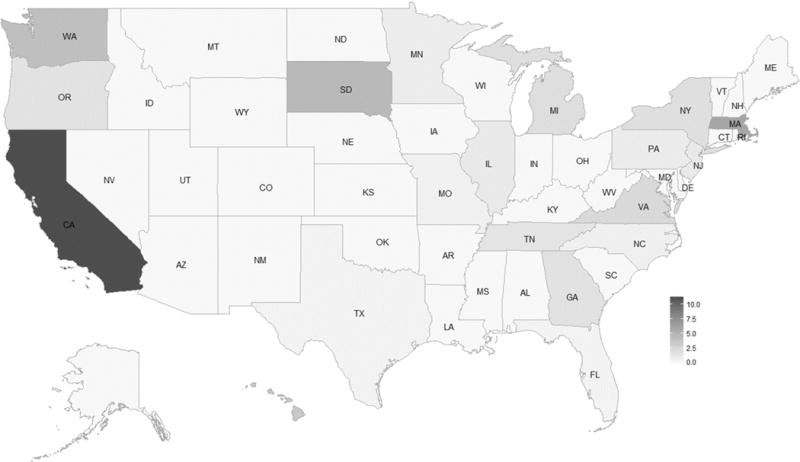
Percent of adult Medicaid patients who received kidney transplants from 1990–2011 who were non-resident aliens, by state. CA (244), MA (18), and NY (26) transplanted the most non-resident aliens with Medicaid. The following states transplanted between 1 and 9 undocumented patients with Medicaid: DC, FL, GA, HI, IL, MI, MN, MO, NC, NJ, OR, PA, SD, TN, TX, VA, WA. Per federal research regulations, any counts <10 must not be reported.
Association of Citizenship With Outcomes
We identified 2,741 graft losses over 37,000 person-years of follow-up, for a rate of 7.3 all-cause graft losses per 100 person-years (Table 2). Non-resident aliens had more than a 45% lower unadjusted risk of all-cause graft loss, death-censored graft loss, and death compared to US citizens (Table 3, Figure 2, Figures S2 and S3). Results were attenuated when further adjusted for demographics (model 2), dialysis factors (model 3), transplant factors (model 4), and comorbidity count (model 5), with no significant difference in mortality in model 4, nor in death-censored graft loss or death in the fully adjusted model 5. Type of donor (living versus deceased), age (<50 versus ≥ 50 years), and race/ethnicity did not modify any of the associations.
Table 2.
Number of events, follow-up time, and incidence and unadjusted survival rates for all study outcomes. Note that patients were only followed for up to 5 years.
| All Patients (N=10495) |
US Citizens (n=8660) | Permanent Residents (n=1489) | Non - resident aliens (n=346) |
|
|---|---|---|---|---|
| All - cause graft failure | ||||
| No. of events | 2741 | 2445 | 254 | 42 |
| Survival rate at 5 y | 70% | 68% | 79% | 84% |
| Follow-up time (years) | 3.56 ±1.78 | 3.57 ±1.78 | 3.54 ±1.75 | 3.31 ±1.80 |
| Total follow-up time, person-y | 37365 | 30936 | 5282 | 1147 |
| Incident rate (per 100 person-years) | 7.3 | 7.9 | 4.8 | 3.7 |
| Death-censored graft failure | ||||
| No. of events | 1824 | 1624 | 168 | 32 |
| Survival rate at 5 y | 80% | 79% | 86% | 88% |
| Follow-up time (years) | 3.95 ±1.58 | 4.00 ±1.57 | 3.79 ±1.63 | 3.52 ±1.73 |
| Total follow-up time, person-y | 41465 | 34602 | 5645 | 1218 |
| Incident rate (per 100 person-years) | 4.4 | 4.7 | 3.0 | 2.6 |
| Death from any cause | ||||
| No. of events | 1389 | 1243 | 128 | 18 |
| Survival rate at 5 y | 85% | 84% | 89% | 93% |
| Follow-up time (years) | 3.56 ±1.78 | 3.57 ±1.78 | 3.55 ±1.75 | 3.31 ±1.80 |
| Total follow-up time, person-y | 37365 | 30936 | 5282 | 1147 |
| Incident rate (per 100 person-years) | 3.7 | 4.0 | 2.4 | 1.7 |
Table 3.
Hazard ratios for adverse transplantation outcomes for non-resident aliens versus US citizens estimated from a frailty model clustered by transplant center.
| HR (95% CI)a | |||
|---|---|---|---|
| Model | All - cause graft loss | Death-censored graft lossb | Death |
| 1: unadjusted | 0.48 (0.35–0.65) | 0.55 (0.39–0.79) | 0.42 (0.26–0.67) |
| 2 : adjusted for demographicsc | 0.56 (0.41–0.76) | 0.59 (0.41–0.85) | 0.58 (0.36–0.93) |
| 3: model 2+ dialysis factorsd | 0.58 (0.42–0.78) | 0.60 (0.41–0.86) | 0.58 (0.36–0.93) |
| 4: model 3+ transplant factorse | 0.63 (0.45–0.85) | 0.65 (0.45–0.94) | 0.65 (0.40–1.06) |
| 5: model 4 + comorbidity countf | 0.67 (0.48–0.94) | 0.68 (0.46–1.01) | 0.68 (0.41–1.15) |
Note: Patients were followed up to 5 years.
CI, confidence interval; HR, hazard ratio
: Citizenship was a three-level variable. See Table d of Item S1 for HRs for permanent residents vs US citizens. Type II p-values of the Wald test (i.e. null hypothesis of no difference across all three groups) was <0.001 for all outcomes.
: HRs for death-censored graft loss are cause-specific.
: age, sex, race/ethnicity (Hispanic, non-Hispanic black, non-Hispanic white or other)
: time on dialysis (<1 or ≥1 year) cause of kidney failure (diabetes, other, or unknown)
: 0-HLA mismatch, living/deceased donor, transplant before 2000
: Count included peripheral vascular disease, cerebrovascular disease, lung disease, cancer, and diabetes
Figure 2.
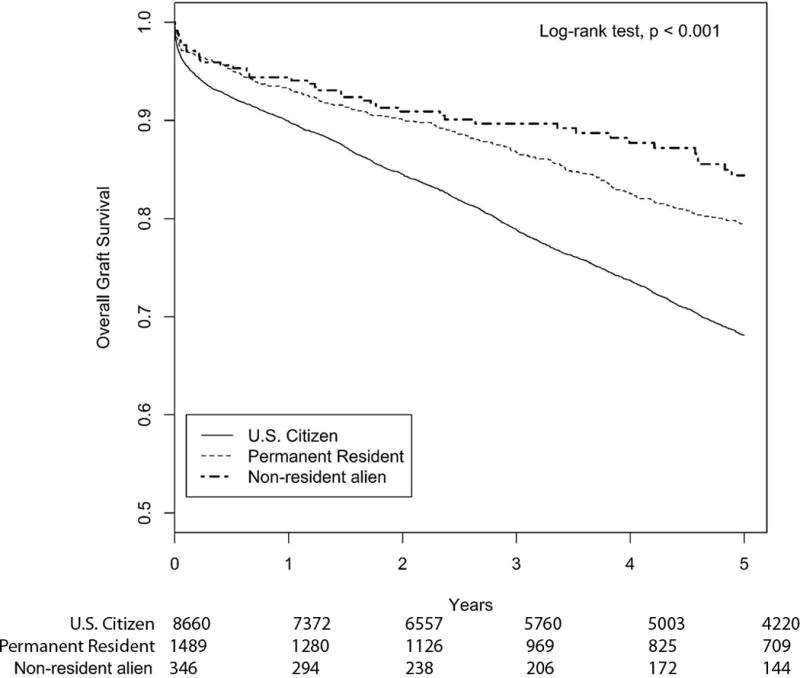
Kaplan-Meier Curve for unadjusted overall graft survival in adult Medicaid patients who received kidney transplants from 1990–2011, by citizenship.
We performed sensitivity analyses where we 1) addressed misclassification of immigrants by combining non-resident aliens and permanent residents into one group and compared them against US citizens and 2) restricted follow-up times to 1 and 3 years to minimize differential loss to follow-up between the groups. All results were materially unchanged from that of the primary analysis (tables a–c of Item S1). Citizenship was treated as a three-level variable in all analyses except for the first sensitivity analysis. Outcomes of permanent residents versus US citizens are reported in tables d–f of Item S1.
Validity of Exposure Variable
To assess the validity of the citizenship variable from the Transplant Candidate Registration form, we reviewed the medical records of all 29 patients covered by Medicaid who had received a kidney transplant from 2009–2011 at a single center. Of the 20 patients categorized as non-resident aliens on the form, 19 (95%) were confirmed to be non-resident aliens via chart review. Conversely, all 19 patients who were found to be non-resident aliens via chart review were correctly categorized as such on the form. The sensitivity of the non-resident alien variable was 95% and the specificity was 90%. None of the patients at this center had traveled to the United States for the purpose of receiving a transplant.
Discussion
Our study examined kidney transplantation outcomes in adult non-resident aliens in the United States and found that very few Medicaid patients who received their first kidney transplant between 1990 and 2011 were non-resident aliens. Our analyses suggest that they have comparable outcomes to US citizens when similarly insured. These results were robust in models that adjusted for various demographic, dialysis, and transplant-related factors, as well as sensitivity analyses that varied the length of follow-up and that combined permanent resident outcomes with those of non-resident aliens.
The non-resident aliens in this study likely represent a select subgroup of patients. We assumed they were undocumented immigrants, who have a high employment rate and tend to be younger and healthier than US citizens.1 Their younger age may explain the lower prevalence of diabetic nephropathy compared to US citizens. The predominantly Hispanic immigrants may also have a higher rate of Mesoamerican nephropathy that partly accounts for the high percentage of unknown etiology of ESKD in the group. Given the barriers to transplantation for non-citizens, these non-resident aliens that receive transplants are likely to be healthier, to have stronger family and financial support, and to be better able to navigate the healthcare system. Such selection bias could explain why the non-resident aliens had lower rates of all-cause graft loss than US citizens. While not all undocumented immigrants may be suitable transplant candidates, our study suggests that with proper screening, citizenship status itself is not predictive of poor outcomes.
Our findings that non-resident aliens have favorable transplant outcomes are in line with a recent single-center study of 289 pediatric kidney transplant recipients in California, 48 (17%) of whom were undocumented immigrants.11 In contrast to our study, citizenship status was ascertained by chart review. Patients were categorized as either undocumented immigrants or US citizens, with permanent residents considered as citizens. After adjustment for patient age, donor age, donor type, and HLA mismatch, the authors found that undocumented immigrant children had a lower risk of graft loss at 5 years as compared to permanent residents and US citizens (HR, 0.38; 95% CI, 0.15–0.96). Over 20% of the undocumented recipients who reached the age of 21 years or older subsequently lost their graft, primarily because they could not afford their immunosuppressive medications when they aged out of the state-funded program that cover these medications for pediatric patients. The insurance status of these patients was not reported, so it is not clear if these patients were covered by Medicaid or other insurance at the time of their transition out of the pediatric program.
Both our study and the pediatric study highlight the limited access non-resident aliens, including undocumented immigrants, have to kidney transplantation. Most adult US citizens have their dialysis and kidney transplantation costs covered by Medicare, a federal health insurance program.12 The Omnibus Reconciliation Act of 1986, on the other hand, restricts federal Medicaid funds from being spent on undocumented immigrants unless it is for a life-threatening or emergency situation.13 Thus, the estimated 6,000 undocumented immigrants in the United States with ESKD are entitled to emergency dialysis, regardless of their ability to pay, but maintenance dialysis is only available in certain areas depending on state and local legislation and policy interpretation.1, 3, 14 For instance, California, home to the most undocumented immigrants in the United States (2.35 million), uses state funds to provide maintenance dialysis for these patients.15 By contrast, Texas, which has the second largest number of undocumented immigrants (1.65 million), often only dialyzes these patients if they present with imminent, life-threatening symptoms, a practice that leads to increased costs, higher mortality rates, and a poor quality of life stemming from the physical and psychosocial distress of receiving emergent-only dialysis.15–20
Kidney transplantation is not considered an emergency treatment for ESKD. Thus, unlike dialysis, under no condition would it be federally subsidized for undocumented immigrants, even though it leads to lower morbidity and mortality rates and better quality of life for patients at a lower cost.5, 6 Transplant centers often deny uninsured patients kidney transplantation out of concern that they might not be able to pay for their graft-sustaining immunosuppressant medications.21,22,23 In the era of the Affordable Care Act, undocumented immigrants remain one of the few groups of patients ineligible for either Medicaid or insurance through the Health Insurance Marketplaces.24 Immigrants with valid visas are eligible to participate in the exchange. Undocumented immigrants can be insured through off-the-exchange commercial health insurance plans subsidized by charitable organizations, although it is unclear if this option is sustainable.25
As a result, many undocumented immigrants have turned to state programs for insurance coverage for transplantation. This is likely the reason that the vast majority of the undocumented immigrants in our study were transplanted in California. About 1,350 (2%) out of 61,000 patients on dialysis in that state are undocumented immigrants.26 Although emergency Medi-Cal (the California version of Medicaid) does not cover transplants, anecdotally, patients have been getting transplants by securing full-scope Medi-Cal as immigrants permanently residing in the United States under color of law (PRUCOL).27 PRUCOL patients are individuals living in the United States with the knowledge of the US Citizenship and Immigration Services (USCIS) but that the USCIS does not plan to deport. Undocumented immigrants not yet on dialysis do not qualify for the program. This is likely the reason none of the non-resident aliens in our study received pre-emptive transplants. Regarding pediatric patients, in 2016 California state law expanded Medi-Cal coverage to low-income children regardless of immigration status.28 In 2011 the state legislature also passed a bill mandating that Medi-Cal would continue to provide anti-rejection medications for up to two years post-transplantation if the patient has no other insurance coverage, even if patients later become ineligible for Medi-Cal (for example if they are no longer considered low-income).29 Many safety-net and county hospital programs will also provide these medications if patients cannot afford them, making long-term graft survival feasible even for low-income patients. These state-sponsored initiatives do not violate federal policies since they only use state and not federal funds. Notably, increasing access to kidney transplantation has not resulted in an influx of undocumented immigrants to California; in fact, after peaking in at 2.8 million in 2007, the number of undocumented immigrants has slowly fallen to 2.35 million.15
Illinois is another state that subsidizes transplantation for undocumented immigrants. In 2014, it passed Comprehensive Medicaid Legislation, which allows undocumented immigrants already enrolled in the state-funded dialysis program to receive state public aid funds to cover kidney transplantation.30 The financial savings were a driving factor in approving the bill. Even with the cost of surgery, transplantation is more cost effective than dialysis after less than two years. Based on an 8 year life expectancy, the projected savings would be $321,000 per patient.4 The savings would be even more dramatic in states that only provide emergent (rather than maintenance) dialysis, where costs are estimated to reach $285,000 a year per patient.18
In states without coverage for kidney transplantation, undocumented immigrants are often denied a better and more cost effective ESKD treatment option. Some have argued that such unequal access is inevitable given the relative scarcity of deceased donors in the United States. However, this argument fails to consider that undocumented immigrants disproportionately contribute to the pool of potential deceased donors for the United States.31 In the 22 years of our study, 990 deceased donors were non-resident aliens, more than 4 times the number of non-resident aliens on Medicaid who received a deceased donor transplant.32 Also, 40% of the non-resident aliens in our study had living donors and did not take away any organs from potential US citizen recipients. Similarly, a survey of undocumented immigrants on dialysis in New York found that 60% had potential living donors.4 Expanding coverage for kidney transplantation for these patients with living donors would improve their outcomes without negatively affecting the chances of US citizens undergoing transplantation. Even if half of the undocumented immigrants with ESKD in the UnitedStates were to be waitlisted for a deceased donor transplant, it would only increase the waitlist by 3%.
There would also be a societal benefit to having these patients receive transplants. They tend to be younger, healthier, and, thus, more likely to contribute to the US workforce if they undergo transplantation.4 As noted earlier, there would be healthcare savings associated with having non-resident alien patients receiving maintenance dialysis treatments undergo transplantation.
Our study has several limitations. The primary one is that citizenship status was self-reported as non-resident alien, resident alien, and U.S. citizen. Thus, it is difficult to discern whether non-resident aliens were undocumented immigrants, foreign nationals with a legal visa, or foreign nationals traveling to the United States for transplantation (though it is unlikely that the last group would have qualified for Medicaid). Similarly, undocumented immigrants may have been misclassified as resident aliens. Chart review from a single center found the citizenship variable to be highly sensitive and specific, but it is unclear how generalizable these measures are to other centers. Another limitation is that we cannot capture outcomes of non-resident aliens who leave the United States and do not return. This would bias the results towards a beneficial association with nonresident alien status. Given the low number of outcomes in the non-resident alien group, we also could not adjust for many potential confounders, including the specific cause of kidney failure, BMI, specific comorbidities (instead of a comorbidity count), and donor characteristics. We also could not adjust for unobserved confounders such as immunosuppressive regimen and employment status. Our results may not be generalizable to wealthier patients who do not qualify for Medicaid or to residents outside of California, the home state of >70% of the non-resident aliens. We were also unable to assess patient-reported outcomes such as quality of life. As with all observational studies, we cannot prove causation. However, the limitations must be balanced against the strengths of the study, which include a large, national cohort and results that were consistent across various sensitivity analyses.
In conclusion, we found that only a small percentage of patients with Medicaid who received transplants in the United States were non-resident aliens. The transplantations occurred mostly in California and have increased in recent years, and our study suggests that these nonresident aliens do no worse than US citizens after transplantation. Policymakers should consider expanding coverage for kidney transplantation in nonresident aliens, including undocumented immigrants, as it is associated with high quality outcomes.
Supplementary Material
Supplementary Material Descriptive Text for Online Delivery
Supplementary Figure S1 (PDF). Study population selection from USRDS.
Supplementary Figure S2 (PDF). Unadjusted death-censored graft survival in adult Medicaid patients who received kidney transplants from 1990–2011, by citizenship.
Supplementary Figure S3 (PDF). Kaplan-Meier curve for unadjusted patient survival in adult Medicaid patients who received kidney transplants from 1990–2011, by citizenship.
Supplementary Item S1 (PDF). HRs for adverse transplant outcomes estimated from a frailty model clustered by transplant center.
Supplementary Table S1 (PDF). Transplants of Medicaid recipient by state.
Acknowledgments
We thank Arleen Brown and Steven Wallace for critically reviewing earlier versions of the manuscript.
Support: Dr Shen is supported by grant K23DK103972 from the National Institutes of Health (NIH) and a generous gift honoring the life and work of nephrologist Henry Shavelle, MD. Dr Norris is supported by NIH grants UL1TR000124 and P30AG021684. The funders did not have any role in study design; collection, analysis, or interpretation of data; or initial drafting of the report; however, the manuscript was reviewed and approved for publication by an officer of the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors’ Contributions: Research idea and study design: JIS, LMB, UR, KCN; data acquisition: JIS; data analysis/interpretation: JIS, DH, LMB, HW, ELL, EH, LKS, SV, KCN, UR; statistical analysis: DH, HW, SV; supervision or mentorship: KCN. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Financial Disclosure: The authors declare that they have no other relevant financial interests.
Disclaimer: Data reported herein were supplied by the USRDS. Interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government.
Prior Presentation: Aspects of this study were presented in abstract form at the Society of General Internal Medicine Annual Meeting, April 19–22, 2017, Washington, DC.
Peer Review: Evaluated by three external peer reviewers, a Statistics/Methods Editor, an Associate Editor, and the Editor-in-Chief.
References
- 1.Rodriguez RA. Dialysis for undocumented immigrants in the United States. Advances in chronic kidney disease. 2015;22:60–65. doi: 10.1053/j.ackd.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Passel JCD. Numbers, Facts and Trends Shaping the World. Pew Research Center; 2016. Overall Number of U.S Unauthorized Immigrants Holds Steady Since 2009. [Google Scholar]
- 3.Campbell GA, Sanoff S, Rosner MH. Care of the undocumented immigrant in the United States with ESRD. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2010;55:181–191. doi: 10.1053/j.ajkd.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 4.Linden EA, Cano J, Coritsidis GN. Kidney transplantation in undocumented immigrants with ESRD: a policy whose time has come? American journal of kidney diseases : the official journal of the National Kidney Foundation. 2012;60:354–359. doi: 10.1053/j.ajkd.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 6.Schweitzer EJ, Wiland A, Evans D, et al. The shrinking renal replacement therapy “break-even” point. Transplantation. 1998;66:1702–1708. doi: 10.1097/00007890-199812270-00023. [DOI] [PubMed] [Google Scholar]
- 7.Purnell TS, Luo X, Kucirka LM, et al. Reduced Racial Disparity in Kidney Transplant Outcomes in the United States from 1990 to 2012. Journal of the American Society of Nephrology : JASN. 2016;27:2511–2518. doi: 10.1681/ASN.2015030293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grubbs V. Undocumented immigrants and kidney transplant: costs and controversy. Health affairs (Project Hope) 2014;33:332–335. doi: 10.1377/hlthaff.2013.0462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bramstedt KA. Supporting organ transplantation in non-resident aliens within limits. Ethics & medicine : a Christian perspective on issues in bioethics. 2006;22:75–81. [PubMed] [Google Scholar]
- 10.Glazier AK, Danovitch GM, Delmonico FL. Organ transplantation for nonresidents of the United States: a policy for transparency. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2014;14:1740–1743. doi: 10.1111/ajt.12770. [DOI] [PubMed] [Google Scholar]
- 11.McEnhill ME, Brennan JL, Winnicki E, et al. Effect of Immigration Status on Outcomes in Pediatric Kidney Transplant Recipients. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16:1827–1833. doi: 10.1111/ajt.13683. [DOI] [PubMed] [Google Scholar]
- 12.Rettig RA. Special treatment–the story of Medicare’s ESRD entitlement. N Engl J Med. 2011;364:596–598. doi: 10.1056/NEJMp1014193. [DOI] [PubMed] [Google Scholar]
- 13.Act PS-D. Omnibus Budget Reconciliation Act. Public law. 1990:4206. [Google Scholar]
- 14.Straube BM. Reform of the US healthcare system: care of undocumented individuals with ESRD. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2009;53:921–924. doi: 10.1053/j.ajkd.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 15.Hou NV,C, Raghavan R. Kidney Week. Chicago, IL: American Society of Nephrology; 2016. Undocumented with Stage End Renal Disease: Characteristics and Outcomes Associated with Delayed Initiation. [Google Scholar]
- 16.Raghavan R. When access to chronic dialysis is limited: one center’s approach to emergent hemodialysis. Seminars in dialysis. 2012;25:267–271. doi: 10.1111/j.1525-139X.2012.01066.x. [DOI] [PubMed] [Google Scholar]
- 17.Raghavan R, Nuila R. Survivors–dialysis, immigration, and U.S. law. N Engl J Med. 2011;364:2183–2185. doi: 10.1056/NEJMp1101195. [DOI] [PubMed] [Google Scholar]
- 18.Sheikh-Hamad D, Paiuk E, Wright AJ, Kleinmann C, Khosla U, Shandera WX. Care for immigrants with end-stage renal disease in Houston: a comparison of two practices. Texas medicine. 2007;103:54–58. 53. [PubMed] [Google Scholar]
- 19.Hogan AN, Fox WR, Roppolo LP, Suter RE. Emergent Dialysis and its Impact on Quality of Life in Undocumented Patients with End-Stage Renal Disease. Ethn Dis. 2017;27:39–44. doi: 10.18865/ed.27.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cervantes L, Fischer S, Berlinger N, et al. The Illness Experience of Undocumented Immigrants With End-stage Renal Disease. JAMA Intern Med. 2017 Apr 1;177(4):529–535. doi: 10.1001/jamainternmed.2016.8865. [DOI] [PubMed] [Google Scholar]
- 21.Herring AA, Woolhandler S, Himmelstein DU. Insurance status of U.S. organ donors and transplant recipients: the uninsured give, but rarely receive. International journal of health services : planning, administration, evaluation. 2008;38:641–652. doi: 10.2190/HS.38.4.d. [DOI] [PubMed] [Google Scholar]
- 22.Gill JS, Tonelli M. Penny wise, pound foolish? Coverage limits on immunosuppression after kidney transplantation. N Engl J Med. 2012;366:586–589. doi: 10.1056/NEJMp1114394. [DOI] [PubMed] [Google Scholar]
- 23.Evans RW, Applegate WH, Briscoe DM, et al. Cost-related immunosuppressive medication nonadherence among kidney transplant recipients. Clin J Am Soc Nephrol. 2010;5:2323–2328. doi: 10.2215/CJN.04220510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sommers BD. Stuck between health and immigration reform–care for undocumented immigrants. N Engl J Med. 2013;369:593–595. doi: 10.1056/NEJMp1306636. [DOI] [PubMed] [Google Scholar]
- 25.Raghavan R. New Opportunities for Funding Dialysis-Dependent Undocumented Individuals. Clin J Am Soc Nephrol. 2017 Feb 7;12(2):370–375. doi: 10.2215/CJN.03680316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurley L, Kempe A, Crane LA, et al. Care of undocumented individuals with ESRD: a national survey of US nephrologists. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2009;53:940–949. doi: 10.1053/j.ajkd.2008.12.029. [DOI] [PubMed] [Google Scholar]
- 27.Kuruvilla R, Raghavan R. Health care for undocumented immigrants in Texas: past, present, and future. Texas medicine. 2014;110:e1. [PubMed] [Google Scholar]
- 28.Fabi R, Saloner B. Covering Undocumented Immigrants — State Innovation in California. New England Journal of Medicine. 2016;375:1913–1915. doi: 10.1056/NEJMp1609468. [DOI] [PubMed] [Google Scholar]
- 29.Assembly Bill (AB) 2352, Perez. Chapter 676. Vol Statutes of 20102011:Welfare and Institutions Code.
- 30.Ansell D, Pallok K, Guzman MD, Flores M, Oberholzer J. Illinois law opens door to kidney transplants for undocumented immigrants. Health affairs (Project Hope) 2015;34:781–787. doi: 10.1377/hlthaff.2014.1192. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg AM, Simmerling M, Frader JE. Why nondocumented residents should have access to kidney transplantation: arguments for lifting the federal ban on reimbursement. Transplantation. 2007;83:17–20. doi: 10.1097/01.tp.0000247795.41898.55. [DOI] [PubMed] [Google Scholar]
- 32.United States Renal Data System. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material Descriptive Text for Online Delivery
Supplementary Figure S1 (PDF). Study population selection from USRDS.
Supplementary Figure S2 (PDF). Unadjusted death-censored graft survival in adult Medicaid patients who received kidney transplants from 1990–2011, by citizenship.
Supplementary Figure S3 (PDF). Kaplan-Meier curve for unadjusted patient survival in adult Medicaid patients who received kidney transplants from 1990–2011, by citizenship.
Supplementary Item S1 (PDF). HRs for adverse transplant outcomes estimated from a frailty model clustered by transplant center.
Supplementary Table S1 (PDF). Transplants of Medicaid recipient by state.


