Abstract
Objective
Community Partners in Care (CPIC) was a group-randomized study of 2 approaches to implementing expanded collaborative depression care: Community Engagement and Planning (CEP), a coalition approach, and Resources for Services (RS), a technical assistance approach. Collaborative care networks in both arms involved healthcare and non-healthcare agencies in 5 service sectors. This study examined 6- and 12-month outcomes for CPIC participants with serious mental illness.
Methods
This study conducts secondary analysis of CPIC data. The study focused on low-income, racial/ethnic minority participants in under-resourced Los Angeles communities with serious mental illness (n=504). Serious mental illness was defined by self-reported severe depression (PHQ-8≥20) at baseline or lifetime history of bipolar disorder or psychosis. Analyses used logistic and Poisson regression with multiple imputation and response weights, controlling for covariates, to model intervention effects on outcomes.
Results
Among CPIC participants, 50% had serious mental illness. Among those with serious mental illness, CEP relative to RS reduced poor mental health-related quality of life (OR=.62, CI=.41–.95) but not depression (primary outcomes); increased mental wellness; reduced homelessness risk factors and behavioral health hospitalizations; reduced specialty mental health medication/counseling visits; and increased faith-based depression visits (each p<.05) at 6 months. There were no statistically significant 12-month effects.
Conclusions
Findings suggest a coalition approach to implementing expanded collaborative depression care, compared to technical assistance to individual programs, may reduce short-term behavioral health hospitalizations and improve mental health quality of life and some social outcomes for adults with serious mental illness, without evidence for long-term effects within this sub-sample.
INTRODUCTION
Depression was recently identified as the leading cause of adult disability worldwide(1). In the US, disparities in access to, quality of, and outcomes for depression care exist by race, ethnicity, and socioeconomic status(2). People with serious mental illnesses have an estimated lifetime prevalence of comorbid depression of up to 50%(3–5). Recent policy changes such as the Helping Families in Mental Health Crisis Act and states’ adoption of Home and Community-based Service incentivize increased healthcare and community-based services collaboration for people with serious mental illnesses(6–8). Collaborations among healthcare, social services, and community-based services are effective at addressing mental health and social needs of those with serious mental illness(9–13), but a 2015 Cochrane review reported finding only one “high-quality” study on the specific issue of the added value of coalition versus non-coalition-based interventions to improve the health of minority communities, Community Partners in Care (CPIC)(14,15). This study presents a sub-analysis focusing on CPIC participants with serious mental illness to inform future research.
Community Partners in Care
CPIC was a group-level randomized comparative effectiveness trial that compared 2 approaches to implement an expanded model of collaborative depression care(15,16). CPIC was conducted within 95 programs in 5 sectors: outpatient primary care, outpatient mental health, substance use treatment (residential and outpatient), homeless services, and other community-based services (e.g., faith-based programs, parks-and-recreation senior/community centers, exercise clubs, hair salons) in 2 under-resourced Los Angeles communities.
The study compared Resources for Services (RS) versus Community Engagement and Planning (CEP), implemented at the program-level in all 5 sectors above using an evidence-based toolkit for collaborative depression care. RS used expert technical assistance for providers, administrators, and other staff, while CEP used a coalition approach to plan, co-lead, and monitor training and implementation. At 6-month follow-up, compared to RS, those in CEP experienced greater improvements in mental health-related quality of life (MHRQL) and mental wellness, increased physical activity, reduced risk factors for homelessness, and fewer behavioral health hospitalizations(15). At 12-month follow-up, primary analyses suggested statistically significant, modest improvements in MHRQL and fewer hospitalizations in the CEP versus RS; these findings remained in the same direction but were statistically significant in some but not all sensitivity analyses (e.g., longitudinal analyses without response weights)(16).
CPIC differs from most collaborative depression care studies by including healthcare and non-healthcare agencies as sites for recruitment and intervention; by focusing on safety-net programs in diverse, urban, under-resourced communities (87% identified as Latino and/or African American and nearly three-quarters lived below federal poverty level(15); and few exclusion were applied, including allowing for comorbid disorders.
CPIC and Serious Mental Illness
This secondary analysis focused on CPIC participants, all of whom had probable depression defined by Patient Health Questionnaire (PHQ)-8≥10, who also met study criteria for serious mental illness, a pre-specified sub-group analysis documented in study protocols(17). Serious mental illness has been variously defined in the literature by specific diagnoses—psychotic illnesses, bipolar disorder, and sometimes including major depressive disorder—and in epidemiologic and policy contexts by functional limitations in one or more life activities(18,19). Among CPIC participants, we defined serious mental illness as severe symptoms of depression or lifetime histories of bipolar disorder or psychosis and explored the sensitivity of intervention effects to different definitions.
The first study aim was to describe the prevalence of serious mental illness among CPIC participants, by the sector in which they were initially screened, which is important given few studies have participants identified from the breadth of service sectors in CPIC. The second aim was to explore whether some of the benefits seen in the parent study for CEP versus RS participants were also observed among participants with serious mental illness, particularly important as many collaborative depression care studies exclude people with histories of bipolar disorder or psychosis. We hypothesized that CPIC’s CEP approach to depression quality improvement (QI) would lead to significantly improved mental health and social outcomes for those with serious mental illness compared to RS, particularly within the first 6-months of follow-up where intervention effects were strongest in the parent study. Alternatively given limited tailoring of trainings and services for those with serious mental illness, there may have been few differences in outcomes in CEP versus RS participants. We also explored whether outcomes differed for CPIC participants with and without serious mental illness, hypothesizing no significant intervention-by-serious-mental-illness interactions as further potential support for consistency of intervention effects between this sub-sample and the parent study.
METHODS
Study Design and Population
A secondary analysis on 6- and 12-month outcomes of CPIC participants with serious mental illness(15,16) was conducted. CPIC was a community-partnered participatory study emphasizing equal partnership among community and academic partners, facilitated by a partnered oversight council. CPIC was conducted in 2 communities in LA: Hollywood-Metro and South LA. Partners nominated 4 vulnerable populations for intentional sampling by inclusion of programs serving these groups: substance use treatment clients, African Americans, individuals who were homeless, and seniors.
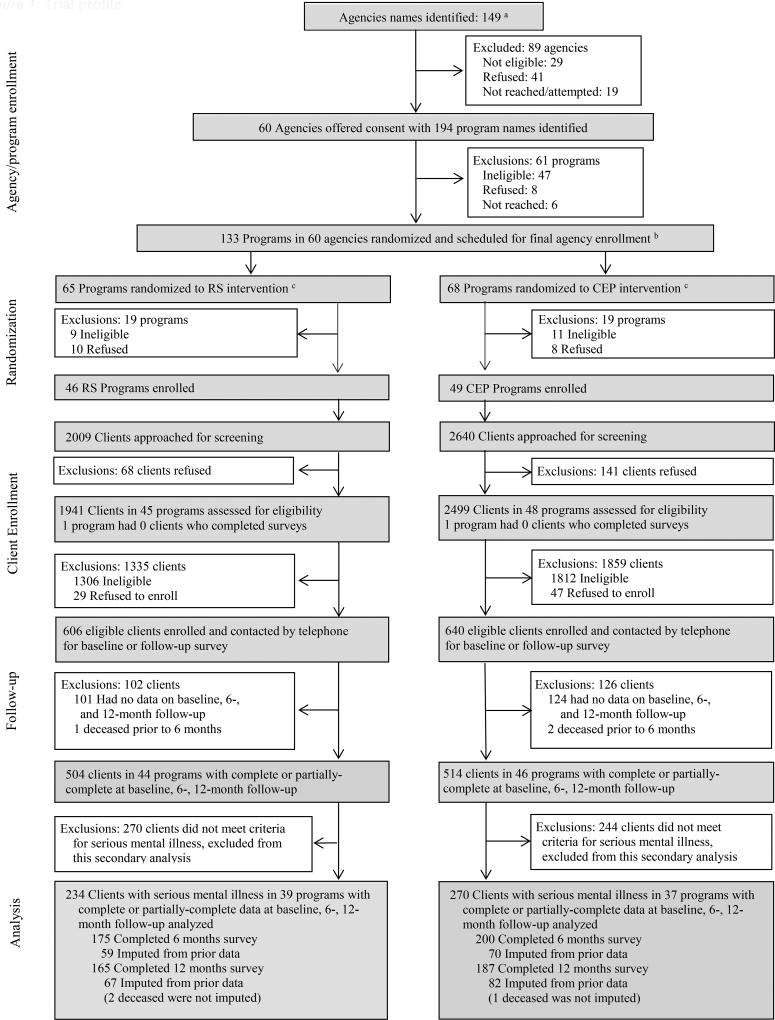
Agencies and programs within the 5 sectors described above were enrolled between November 2008 through August 2010. Within each community, using a multi-stage process involving county lists and partner nominations, potentially eligible agencies were identified and contacted (Figure 1)(15). These programs were randomized to RS or CEP. To reduce intervention cross-over, programs with strong pre-existing referral relationships were grouped for randomization to CEP or RS. Post-randomization, program eligibility and enrollment was finalized at site visits (see footnote, Figure 1).
Figure 1. Trial profile.
Footnotes:
aAgency eligibility criteria: agencies had to provide services for adults or parents of child clients and be financially stable, i.e., not expecting to close during the study time period. Agencies were entities with administrative responsibilities
bProgram eligibility criteria: programs had to serve at least 15 clients per week, have one or more staff, not focused on psychotic disorders or home services, and be willing to identify a staff liaison
cWithin sectors, programs were matched on client size and smaller programs (faith-based, hair salons) were joined based on established relationships. Programs/clusters were randomized within communities, but a few unique programs were randomized across communities. We used a random number generator and CPIC Council members who provided seed numbers to initiate randomization. Randomization was overseen by a statistician not involved in recruitment.
Client enrollment occurred March to November 2010. A sampling strategy was developed for different types of locations (e.g., groups, waiting rooms). All English- and Spanish-speaking adults (≥ 18 years) receiving services (or parents of children receiving services) at participating programs were identified during a screening/enrollment time period and then approached for screening for study eligibility. All who were present were approached simultaneously (e.g., in the case of small groups) or were approached using random number tables. RAND staff blinded to intervention status approached 4645 people for screening and 4440 (95.6%) agreed. Inclusion criteria were adults providing contact information with moderate depressive symptoms by PHQ-8≥10(15,20,21). RAND staff excluded individuals unable to answer screening items due to gross cognitive impairment. Of those screened, eligible, and enrolled, 1018 completed baseline or 6- or 12-month follow-up surveys (Figure 1, Appendix Table S1). Of these, 504 met criteria for serious mental illness (see Baseline Measures below) and comprise the analytic subsample (Figure 1). This study and all procedures were approved by the Institutional Review Board at RAND and at participating agencies that required separate review.
Interventions
RS and CEP, both active interventions, were implemented using an expanded collaborative depression care toolkits from Partners in Care, WeCare, IMPACT, and Mental Health Infrastructure and Training(22). The toolkit (available in hardcopy, online, USB drives) included resources on clinical assessment, psychotropic medication management, psychotherapy, skill building for case managers and community health workers, and patient education. The toolkit included trainings on assessment and management for those with histories of bipolar or psychotic disorders (treatment engagement, referral to specialty mental health services).
In RS, using a train-the-trainer approach, an expert study team (psychiatrist, psychologist, care manager, collaborative depression care leader, community outreach expert, and staff) offered 12 webinars via phone or online to all RS programs plus one site visit for each primary care program in each community. There was no intentional promotion of agency collaboration.
CEP programs provided one or more liaisons for biweekly coalition planning meetings for 4 months to adapt toolkits and write a training and implementation plan incorporating community preferences and strengths, supported by $15K/coalition. CEP explicitly promoted networking among programs to encourage referrals and sharing of collaborative care tasks to increase capacity. CEP coalitions adapted toolkits by incorporating alternative therapies into medication management, trainings on provider self-care and listening skills, and piloting innovative case management and psychoeducation strategies(23). CEP relative to RS was associated with increased program and provider participation in trainings and case managers’ use of psychotherapeutic skills and time spent providing community services(23–25).
Following an encouragement design, programs were encouraged but not required to use toolkit resources, and individual participants were free to seek services as they wished(26). CEP, but not RS, program administrators were provided lists of their program’s participants for safekeeping in a secure file, except for one agency with a shared waiting room for CEP and RS programs where both were given lists.
Baseline Measures
Baseline measures (screener and telephone) included demographics (age, sex), having ≥3 of 18 chronic health conditions (e.g., diabetes, cancer, heart disease), education level and race/ethnicity; physical and mental health composite scores from the 12-item Short Form health survey (SF-12)(15,27). The Mini-International Neuropsychiatric Interview-6 (MINI) was included to assess Diagnostic & Statistical Manual of Mental Disorders, fourth edition criteria for: probable 12-month diagnoses for major depressive or dysthymic disorder, hypomania/mania, recent anxiety (one-month panic or post-traumatic stress or 6-month generalized anxiety disorder), and alcohol abuse or use of illicit drugs. Psychosis history was assessed at baseline using a 4-item screener of ever receiving a diagnosis by a physician of schizophrenia or schizoaffective disorder or hospitalized for experiences such as: hearing voices others could not hear, believing that people were trying to hurt him/her, feeling that he/she could hear another person's thoughts, or feeling someone was putting thoughts in or taking thoughts out of his/her mind(28). Depression was assessed using the PHQ-8 at baseline and PHQ-9 at 6- and 12-month follow-up(20,21).
CPIC participants were defined for this study as having serious mental illness if they met criteria for severe depression at baseline (PHQ-8≥20), lifetime history of hypomania/mania consistent with bipolar disorder (MINI), or lifetime history of psychosis (4-item screener). Sensitivity analyses were conducted for 2 sub-groups: those also reporting poor MHRQL at baseline, defined as SF-12 mental component summary (MCS-12) score ≤40, one standard deviation below the population mean; and lifetime history of bipolar disorder or psychosis.
Outcome Measures
The 2 primary outcomes were poor MHRQL (MCS-12≤40) and probable depression (PHQ-9≥10) at 6- and 12-month follow-up. Secondary outcomes prioritized by community partners through a pre-specified participatory process included mental wellness (a response of at least “sometimes in the prior 4 weeks” to feeling calm or peaceful, having energy, or being happy); homelessness risk, defined as current homelessness or living in a shelter or having ≥2 risk factors (e.g., no place to stay for ≥2 nights or eviction from a primary residence, financial crisis, or food insecurity in the past 6 months); and self-reported behavioral health hospitalizations(15,16). This study did not include measures of psychosis symptom severity.
Secondary self-reported outpatient and community-sector service use outcomes were examined at 6- and 12-months. Self-report data were collected for total visits, visits with depression-related services (see footnote, Table 4), and names and locations for up to 4 providers for visits with depression-related services for each of 7 service categories (mental health specialty, primary care, substance use, social services, faith-based, parks-and-recreation, and other community programs) for 6-months prior to baseline, 6-, and 12-month follow-up. Self-report data on program locations for depression-related services were used to describe service use from programs in assigned and opposite intervention arms.
TABLE 4.
Intervention effects on service utilization at 6 months among participants with serious mental illnessa
| Unadjusted Estimatesb | Adjusted Analysisc | |||||||
|---|---|---|---|---|---|---|---|---|
| RS | CEP | CEP vs RS | ||||||
| Total N | M | SD | Total N | M | SD | IRR | 95% CI | |
| Among those with serious mental illness | ||||||||
| Healthcare sector visits for depressiond e | 170 | 19.9 | 38.5 | 186 | 18.7 | 35.2 | .87 | .57–1.33 |
| Outpatient primary care services for depression | 170 | 1.3 | 3.4 | 188 | 1.5 | 2.9 | 1.12 | .74–1.68 |
| Mental health outpatient visits | 171 | 15.2 | 33 | 189 | 10.6 | 2.9 | .69 | .43–1.11 |
| Mental health outpatient visits received advice for medication | 171 | 9.1 | 28.6 | 189 | 4.3 | 7.7 | .44 | .29–.67 |
| Mental health outpatient visits received counseling | 171 | 12.7 | 31.5 | 189 | 7.0 | 13.2 | .55 | .35–.86 |
| Community sector visits for depressionf | 171 | 4.9 | 21.3 | 190 | 6.0 | 22.3 | 1.36 | .66–2.78 |
| Religious services for depression | 171 | .6 | 2.2 | 190 | 1.4 | 6.1 | 2.94 | 1.19–7.25 |
| Among those with serious mental illness with poor mental health-related quality of lifeg | ||||||||
| Healthcare sector visits for depression | 106 | 21.8 | 41.2 | 108 | 17.6 | 34.1 | .88 | .53–1.47 |
| Outpatient primary care services for depression | 106 | 1.8 | 4.1 | 108 | 2.0 | 3.3 | 1.07 | .66–1.72 |
| Mental health outpatient visits | 106 | 16.0 | 34.6 | 110 | 9.2 | 15.7 | .66 | .39–1.12 |
| Mental health outpatient visits received advice for medication | 106 | 9.9 | 3.7 | 110 | 4.0 | 5.0 | .45 | .26–.79 |
| Mental health outpatient visits received counseling | 106 | 14.3 | 33.7 | 110 | 7.0 | 11.3 | .53 | .31–.90 |
| Community sector visits for depression | 106 | 6.1 | 25.1 | 110 | 4.0 | 12.2 | .87 | .27–2.79 |
| Religious services for depression | 106 | .7 | 2.5 | 110 | 1.0 | 4.3 | 2.08 | .66–6.56 |
| Among bipolar disorder or psychosis, lifetime history | ||||||||
| Healthcare sector visits for depression | 133 | 22.0 | 42.5 | 154 | 19.6 | 37.9 | .86 | .54–1.36 |
| Outpatient primary care services for depression | 133 | 1.2 | 2.9 | 156 | 1.4 | 2.9 | 1.28 | .80–2.05 |
| Mental health outpatient visits | 134 | 17.1 | 36.5 | 157 | 1.4 | 21.7 | .65 | .38–1.11 |
| Mental health outpatient visits received advice for medication | 134 | 1.3 | 31.8 | 157 | 4.5 | 8.2 | .40 | .26–.63 |
| Mental health outpatient visits received counseling | 134 | 14.1 | 34.9 | 157 | 6.8 | 13.7 | .50 | .30–.83 |
| Community sector visits for depression | 134 | 5.5 | 23.8 | 158 | 6.4 | 23.8 | 1.31 | .59–2.92 |
| Religious services for depression | 134 | .7 | 2.5 | 158 | 1.6 | 6.7 | 2.89 | 1.20–6.99 |
Serious mental illness, defined as the presence of 1 or more of the following: severe major depressive disorder (PHQ-8 score ≥ 20), lifetime history of bipolar disorder or psychosis
Raw data without weighting or imputation
Adjusted analyses used multiply imputed data, weighted for eligible sample for enrollment; Poisson regression models (presented as incidence rate ratios, IRR), adjusted for baseline status of the dependent variable, age, race/ethnicity, education, 12-month depressive disorder, and community and accounted for the design effect of the cluster randomization
Total healthcare sector visits for depression defined as outpatient primary care services for depression; emergency or urgent care visits for alcohol, drug, and mental health problems; mental health specialty outpatient visits; outpatient substance abuse services for depression
For all service settings, depression-related visits were defined as services for which clients reported talking about depression or medications for depression; counseling for depression, stress, or emotional problems; or being referred to specialty mental health services
Community sector visits for depression defined as homeless and social/community sector services for depression
Poor mental health-related quality of life, defined as MCS-12 ≤ 40; one standard deviation below population mean
Statistical Analysis
We conducted univariate analyses to describe the sample and bivariate analyses to compare screening locations (primary care, mental health, substance abuse, homeless, social/community) by participants’ serious mental illness-status. We examined intervention effects among those with serious mental illness to determine whether CEP was more effective than RS in improving mental health and service utilization. We described baseline differences between CEP and RS using bivariate analyses. We conducted intention-to-treat analysis using regression analyses: logistic regression for dichotomous outcomes and Poisson regression for counts. The independent variable was intervention status (CEP, RS). Covariates for the models were the baseline status of the dependent variable, age, race/ethnicity, 12-month depressive disorder, and community.
CPIC used non-response weighting to address missing data for non-enrollment among eligible clients and for attrition(29,30). We used a hot-deck multiple imputation technique for item nonresponse and an approximate Bayesian bootstrap for unit nonresponse among the analytic sample(31). For these sub-analyses, we used Taylor series linearization with a “subpopn” statement in SUDAAN version 11.1 (RTI International, Research Triangle, NC), accounting for clustering (clients within programs), weighting, and multiple imputations(32,33). Significance of intervention effects was assessed using contrasts among regression coefficients. Results from logistic regression models are presented as odds ratios (OR) and Poisson regression models are presented as incidence rate ratios (IRR) with 95% confidence intervals. We supplement adjusted models with unadjusted raw data to assess robustness.
For sensitivity analyses, we examined variations in intervention effects at 6-months by 3 definitions of serious mental illness, described above. We fit models using the full parent study sample including indicators of intervention status, serious mental illness, and their interaction. We conducted longitudinal analyses, as described in a supplementary appendix.
RESULTS
Baseline Distribution of Serious Mental Illness by Sector
At baseline, half of the parent study sample met criteria for serious mental illness, with prevalence of 41% in primary care programs. There were significant differences (p<.05) in prevalence of serious mental illness across 5 sectors, with the highest proportions in substance use treatment (64%) and homeless settings (56%) (Table 1).
TABLE 1.
Illness characteristics of CPIC participants by screening locationa
| Illness Category | Overall (N=1018) |
Primary care (N=290) |
Mental health (N=195) |
Substance abuse (N=230) |
Homeless (N=162) |
Social community (N=141) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Serious mental illness | 504 | 50 | 117 | 41 | 107 | 55 | 144 | 64 | 92 | 56 | 45 | 32 |
| Severe major depressive disorder | 171 | 17 | 38 | 14 | 43 | 22 | 41 | 18 | 30 | 19 | 19 | 13 |
| Serious mental illness with poor mental health quality of life | 308 | 30 | 75 | 26 | 70 | 37 | 87 | 38 | 52 | 32 | 23 | 17 |
| Bipolar disorder or psychosis, lifetime history | 419 | 41 | 97 | 33 | 90 | 47 | 123 | 54 | 77 | 47 | 32 | 23 |
Data were multiply imputed and weighted for eligible sample for enrollment; n (unweighted), % (weighted). Chi-square test was used for a comparison of differences across five service settings. Serious mental illness, defined as the presence of 1 or more of the following: severe major depressive disorder (PHQ-8 score ≥ 20), lifetime history of bipolar disorder or psychosis. Poor mental health quality of life at baseline, defined as MCS-12 ≤ 40; one standard deviation below population mean.
Study Participants
Screening, recruitment, and survey completion data by service sector are summarized in Appendix Table S1. All baseline characteristics of participants with serious mental illness were similar between CEP and RS arms (Table 2). Thirty-two percent of the sample identified as Latino and 53% as African American. Forty-three percent had less than a high school education, 76% had a family income below federal poverty level, and 57% were uninsured.
TABLE 2.
Characteristics at baseline of clients with serious mental illness (N=504) by intervention group statusa
| Characteristic | Overall (N=504) |
RS (N=234) |
CEP (N=270) |
|||
|---|---|---|---|---|---|---|
|
| ||||||
| N | % | N | % | N | % | |
| Female | 264 | 51 | 113 | 46 | 151 | 55 |
| Ethnicity | ||||||
| Latino | 156 | 32 | 74 | 32 | 82 | 32 |
| African American | 280 | 53 | 123 | 52 | 157 | 54 |
| Non-Hispanic White | 48 | 10 | 22 | 10 | 26 | 11 |
| Other | 20 | 5 | 15 | 6 | 6 | 4 |
| Married or living with partner | 95 | 19 | 47 | 20 | 48 | 18 |
| Less than high school education | 220 | 43 | 102 | 44 | 117 | 43 |
| ≥3 chronic medical conditions | 306 | 61 | 149 | 64 | 157 | 59 |
| Family income under federal poverty level | 382 | 76 | 182 | 78 | 200 | 74 |
| No health insurance | 285 | 57 | 139 | 60 | 146 | 55 |
| 12-month depressive disorder | 383 | 76 | 180 | 77 | 203 | 75 |
| Alcohol abuse or use of illicit drugs, past 12 months | 241 | 48 | 99 | 44 | 141 | 53 |
| Mental wellnessb | 152 | 30 | 70 | 30 | 82 | 30 |
| Homelessness or ≥2 risk factors for homelessnessc | 303 | 62 | 155 | 68 | 148 | 56 |
| Working for pay | 62 | 12 | 35 | 14 | 28 | 11 |
| Illness sub-groups | ||||||
| Serious mental illness with poor mental health quality of life | 308 | 61 | 145 | 62 | 163 | 60 |
| Bipolar disorder or psychosis, lifetime history | 419 | 83 | 189 | 81 | 230 | 85 |
|
| ||||||
| Mean ± SD | Mean ± SD | Mean ± SD | ||||
|
| ||||||
| Age, y | 45.8 ± 12.0 | 45.2 ± 11.3 | 46.2 ± 12.6 | |||
| PHQ-8d | 16.7 ± 4.5 | 17.0 ± 4.5 | 16.5 ± 4.4 | |||
| MCS-12e | 37.8 ± 7.1 | 37.6 ± 7.1 | 38.0 ± 7.0 | |||
Data were multiply imputed and weighted for eligible sample for enrollment. Chi-square test was used for a comparison of differences across five service settings. Serious mental illness, defined as the presence of 1 or more of the following: severe major depressive disorder (PHQ-8 score ≥ 20), lifetime history of bipolar disorder or psychosis. Poor mental health quality of life is defined as SF-12 MCS score ≤ 40 at baseline.
At least good bit of time on any of three items: feeling peaceful or calm, being a happy person, having energy
Homeless or living in a shelter, or at least two risk factors of four (at least two nights homeless, food insecurity, eviction, financial crisis)
MCS-12 = mental component summary score of the Short Form-12. Possible scores range from 0 to 100, with higher scores representing better mental health-related quality of life.
PHQ-8 = 8-item Patient Health Questionnaire. Possible scores range from 0 to 24, with higher scores representing greater depression severity.
Intervention Effects
At 6-month follow-up, a significantly lower percentage of participants with serious mental illness in CEP versus RS had poor MHRQL (OR=.62, CI=.41–.95) and a significantly higher percentage reported mental wellness (OR=1.98, CI=1.11–3.55) (Table 3). CEP participants relative to RS were significantly less likely to have 2 or more risk factors for homelessness at follow-up (OR=.48, CI=.29–.80) and behavioral health hospitalizations (OR=.45, CI=.22–.88). There was no significant difference between the 2 arms in percentages of participants having at least moderate depression at 6-months. Participants in CEP reported significantly fewer specialty mental health medication management visits (IRR=.44, CI=.29–.67) and mental health counseling visits (IRR=.55, CI=.35–.86); but greater mean visits to faith-based programs for depression services (IRR=2.94, CI=1.19–7.25) at 6-months (Table 4). There were no significant outcome differences between CEP and RS at 12-month follow-up (Appendix Tables S2–S3).
TABLE 3.
Intervention effects on primary and community-prioritized outcomes at 6 months among participants with serious mental illnessa
| Unadjusted Estimatesb | Adjusted Analysisc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RS | CEP | CEP vs. RS | ||||||||
| Clients N |
Total N |
N | % | Total N |
N | % | N | OR | 95% CI | |
| Among those with serious mental illness | ||||||||||
| Primary outcomes | ||||||||||
| Poor mental health quality of life (MCS-12 ≤ 40)d | 359 | 171 | 104 | 61 | 188 | 94 | 50 | 504 | .62 | .41–.95 |
| At least mild depression (PHQ-9 ≥ 10)e | 358 | 171 | 142 | 83 | 187 | 133 | 71 | 504 | .59 | .29–1.18 |
| Community-prioritized (secondary) outcomes | ||||||||||
| Mental wellnessf | 360 | 170 | 39 | 23 | 190 | 70 | 37 | 504 | 1.98 | 1.11–3.55 |
| Homelessness or ≥ 2 risk factors for homelessnessg | 360 | 171 | 87 | 51 | 189 | 54 | 29 | 504 | .48 | .29–.80 |
| Any behavioral health hospitalizations, past 6 mo. | 361 | 171 | 27 | 16 | 190 | 17 | 9 | 504 | .45 | .22–.88 |
| Among those with serious mental illness with poor mental health-related quality of life | ||||||||||
| Primary outcomes | ||||||||||
| Poor mental health quality of life (MCS-12 ≤ 40) | 215 | 106 | 71 | 67 | 109 | 59 | 54 | 308 | .61 | .35–1.04 |
| At least mild depression (PHQ-9 ≥ 10) | 215 | 106 | 92 | 87 | 109 | 85 | 78 | 308 | .61 | .21–1.75 |
| Community-prioritized (secondary) outcomes | ||||||||||
| Mental wellness | 215 | 105 | 20 | 19 | 110 | 35 | 32 | 308 | 1.84 | .92–3.70 |
| Homelessness or ≥ 2 risk factors for homelessness | 216 | 106 | 59 | 56 | 110 | 32 | 29 | 308 | .45 | .26–.78 |
| Any behavioral health hospitalizations, past 6 mo. | 216 | 106 | 16 | 15 | 110 | 8 | 7 | 308 | .43 | .14–1.29 |
| Among bipolar disorder or psychosis, lifetime history | ||||||||||
| Primary outcomes | ||||||||||
| Poor mental health quality of life (MCS-12 ≤ 40) | 290 | 134 | 84 | 63 | 156 | 73 | 47 | 419 | .54 | .33–.90 |
| At least mild depression (PHQ-9 ≥ 10) | 289 | 134 | 113 | 84 | 155 | 110 | 71 | 419 | .58 | .29–1.15 |
| Community-prioritized (secondary) outcomes | ||||||||||
| Mental wellness | 291 | 133 | 33 | 25 | 158 | 58 | 37 | 419 | 1.85 | 1.00–3.44 |
| Homelessness or ≥ 2 risk factors for homelessness | 291 | 134 | 69 | 52 | 157 | 45 | 29 | 419 | .51 | .30–.88 |
| Any behavioral health hospitalizations, past 6 mo. | 292 | 134 | 24 | 18 | 158 | 14 | 9 | 419 | .42 | .22–.81 |
Serious mental illness, defined as the presence of 1 or more of the following: severe major depressive disorder (PHQ-8 score ≥ 20), lifetime history of bipolar disorder or psychosis
Raw data without weighting or imputation
Adjusted analyses used multiply imputed data, weighted for eligible sample for enrollment; logistic regression models adjusted for baseline status of the dependent variable, age, race/ethnicity, education, 12-month depressive disorder, and community and accounted for the design effect of the cluster randomization
MCS-12 = mental component summary score of the Short Form-12. MCS-12 ≤ 40 = one standard deviation below the population mean
PHQ-9 = 9-item Patient Health Questionnaire. PHQ-9 score ≥ 10 corresponds to at least mild depression severity.
At least good bit of time on any of three items: feeling peaceful or calm, being a happy person, having energy
Homeless or living in a shelter, or at least two risk factors of four (at least two nights homeless, food insecurity, eviction, financial crisis)
Sensitivity analyses using more restrictive clinical and policy definitions of serious mental illness revealed similar patterns of intervention effects on primary, community-prioritized, and service use outcomes (Tables 3, 4). Sensitivity analyses with longitudinal modeling among participants with serious mental illness also showed similar patterns of outcomes at 6-months as reported above, except for behavioral health hospitalizations (in one of two models) and visits to faith-based programs for depression which were not statistically different between CEP and RS (Tables S4–6). The above results at 6 months were also confirmed in change from baseline analyses for mental wellness, behavioral health hospitalization, specialty mental health medication and counseling visits (Appendix Table S4–S6). There were no significant intervention-by-serious mental illness-status interaction effects (Tables S7, S8).
Service Use in Assigned and Opposite Treatment Arm
Self-reported raw data revealed 64% (RS) and 61% (CEP) used depression services in programs in their assigned treatment arms in the 6-months prior to baseline, 56% and 45% at 6-month follow-up, and 33% and 40% at 12-months. Self-reported data revealed rates of intervention cross-over: 16% (RS) and 23% (CEP) in the 6-months prior to baseline, declining to 13% and 14% at 6-months and 11% and 13% respectively at 12-months, similar to rates for the overall study sample(34).
DISCUSSION
CPIC was conducted in under-resourced communities with a predominantly racial/ethnic minority sample served by safety-net programs. Given the absence of clinical exclusion criteria, we found a high prevalence of serious mental illness across sectors, illustrated by 41% in primary care, similar to other safety-net studies(35,36). We also found a high prevalence of socioeconomic risk factors, such as unemployment and low income. We examined the added value of a multi-sector coalition approach above technical assistance to implement expanded collaborative depression care for CPIC participants meeting study criteria for serious mental illness.
Findings from this pre-specified sub-group analysis were consistent with the parent study’s outcomes at 6-months, despite a smaller sample size (50% of the parent study sample), including statistically significant improvement for CEP versus RS groups on 1 of 2 primary outcomes and for 3 community-prioritized outcomes at 6 months. Further, we found these comparisons remained significant or borderline significant in longitudinal models (except for behavioral health hospitalizations, significant in 1 of 2 longitudinal models). Thus, all significant comparisons (4 of 5 outcomes) were in the hypothesized direction favoring CEP.
We found no main intervention effects on outcomes at 12-month follow-up, which could be due to a lack of significant long-term intervention differences in this sub-sample or due to limited power (due to smaller sample size) for detecting the smaller intervention effects at 12 months in the parent study. We also found some reduction in CEP versus RS in specialty mental health medication and counseling visits, which also could have contributed to the lack of significant 12-month findings, particularly as people with serious mental illness may require more specialty services. Nevertheless, both the general pattern of similarity to the overall sample at 6 months and the lack of significant intervention-by-“serious mental illness” interaction effects may suggest the parent study’s findings at 6- and 12-months generally apply to this sub-sample. We also found that the overall pattern of outcomes favoring CEP at 6-months was consistent in sub-groups defined by more restrictive definitions of serious mental illness: those with serious mental illness and poor MHRQL at baseline and people with histories of bipolar or psychotic illnesses.
Aspects of the CEP intervention that were similar to evidence-based interventions for those with serious mental illness may have contributed to the positive 6-month outcomes in this sub-sample and overall: multi-sector collaboration, task sharing, relationship building across sectors, and building staff knowledge and capacity to work with those with mental illness(9–11,13,37). CEP promoted sharing of screening and engagement activities with non-healthcare sectors (e.g., social services, recreation centers, faith-based organizations) and non-licensed providers and enabled largely minority participants to receive supports within familiar, trusted locations.
Community partnerships and multi-sector care are emerging approaches to the growing realization that unmet social needs exacerbate health disparities for at-risk groups, including those with serious mental illness and racial/ethnic minority populations(38). Many collaborative care studies exclude those with serious mental illness. These findings, while exploratory to inform future research, suggest that those with serious mental illness may have also benefited from a coalition model similarly to the parent sample, for short-term outcomes. This may support inclusion of people with co-morbid psychiatric diagnoses in collaborative depression care research and services, an issue for future research. This may also involve further tailoring of interventions to the needs of those with serious mental illness, such as a greater focus on specialty consultation. Our study in this respect may add to the existing literature suggesting that multi-sector collaboration, including community-wide models of collaborative depression care, may improve some outcomes for those with serious mental illness(38–41). Future research may also focus on how to strengthen and extend outcome improvements.
This study has important limitations. Randomization occurred within communities, with potential for intervention cross-over. Self-reported cross-over rates were non-trivial during the active intervention (but highest in the 6-months preceding baseline), comparable to the overall study. This cross-over would lead to under-estimation of CEP effects. Missing data due to participant dropout was handled using weighting and item- and wave-level imputation in intention-to-treat analyses. CEP programs were given lists of clients who were enrolled from their site whereas RS programs were not. These lists could have contributed in part to the positive effects seen in the CEP arm, but were kept in a secure files and were not a registry. Prior studies, further, indicate that the provision of lists to providers about the depression status of patients are generally not effective alone in improving the detection of depression, rates of intervention, or outcomes(42,43). Implementation was tracked using service utilization measures, rather than programs’ use of toolkit manuals and forms. The study was limited to 2 urban settings and use of client self-report. Psychosis history was defined by self-report. This sub-sample may have been too small to detect modest outcome differences between CEP and RS (e.g., outcomes at 12-months).
CONCLUSIONS
CPIC was conducted in full partnership with community stakeholders and the findings apply to a highly racially/ethnically diverse and socially at-risk sample subject to disparities. This secondary analysis suggested that intervention effects of CEP versus RS for participants with serious mental illness were largely consistent, at least at 6-months, with the overall study findings, including improvement in one primary outcome (MHRQL) and all community-prioritized outcomes (improved mental wellness and reduced behavioral health hospitalizations and homelessness risk). Future research should use more standard diagnostic and outcome measures for serious mental illness, tailor interventions to this population, and address continuity and sustainment of services through innovations in case management and technology. This study may serve as an important step toward developing and evaluating community-wide coalition approaches to reduce mental health disparities that may include people with serious mental illness.
Supplementary Material
Abbreviations
- CEP
Community Engagement and Planning
- CPIC
Community Partners in Care
- MCS
mental component summary
- MHRQL
mental health-related quality of life
- MINI
Mini-International Neuropsychiatric Interview-6
- PHQ
Patient Health Questionnaire
- QI
quality improvement
- RS
Resources for Services
- SF-12
12-item Short Form Health Survey
Contributor Information
Enrico Guanzon Castillo, University of California Los Angeles - Psychiatry, Los Angeles, California, egcastillo@gmail.com; Los Angeles County Department of Mental Health, Los Angeles, California.
Roderick Shaner, Los Angeles County Department of Mental Health, Los Angeles, California.
Lingqi Tang, UCLA - Psychiatry, Los Angeles, California.
Bowen Chung, UCLA Robert Wood Johnson Clinical Scholars Program, David Geffen School of Medicine, Department of Psychiatry.
Felica Jones, Health African American Families II (HAAF), Los Angeles, California.
Yolanda Whittington, LA County Department of Mental Health, Los Angeles, California.
Jeanne Miranda, University of California, Los Angeles - Psychiatry, Center for Health Services and Society, Los Angeles, California.
Kenneth Wells, UCLA - Psychiatry and Behavioral Sciences.
References
- 1.Friedrich MJ. Depression Is the Leading Cause of Disability Around the World. JAMA. 2017;317:1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- 2.Cook BL, McGuire T, Miranda J. Measuring Trends in Mental Health Care Disparities, 2000 2004. Psychiatric Services. 2007;58:1533–1540. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- 3.Parks J, Svedson D, Singer P, et al. 13th technical report. Alexandria, VA: National Association of State Mental Health Program Directors, Medical Directors Council; 2006. Morbidity and mortality in people with serious mental iIllness. [Google Scholar]
- 4.Hjorth jC, St rup AE, McGrath J, et al. SA57. Life Expectancy and Years of Potential Life Lost in Schizophrenia: A?Systematic Review and Meta-Analysis. Schizophrenia Bulletin. 2017;43:S133–S134. [Google Scholar]
- 5.Buckley PF, Miller BJ, Lehrer DS, et al. Psychiatric comorbidities and schizophrenia. Schizophrenia Bulletin. 2008;35:383–402. doi: 10.1093/schbul/sbn135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.New York State Office of Mental Health. New York State: Health and Recovery Plan (HARP) Adult Behavioral Health Home and Community Based Services (BH HCBS) Provider Manual [Internet] 2016 Available from: https://www.omh.ny.gov/omhweb/bho/docs/hcbs-manual.pdf.
- 7.Mechanic D. Seizing opportunities under the Affordable Care Act for transforming the mental and behavioral health system. Health Aff (Millwood) 2012;31:376–382. doi: 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- 8.Murphy T. H.R.2646 - Helping Families in Mental Health Crisis Act of 2016. 114th Congress. 2016 https://www.congress.gov/bill/114th-congress/house-bill/2646.
- 9.Rickards LD, McGraw SA, Araki L, et al. Collaborative initiative to help end chronic homelessness: Introduction. The journal of behavioral health services & research. 2010;37:149–166. doi: 10.1007/s11414-009-9175-1. [DOI] [PubMed] [Google Scholar]
- 10.Randolph F, Blasinsky M, Morrissey JP, et al. Overview of the ACCESS program. Psychiatric Services. 2002 doi: 10.1176/appi.ps.53.8.945. [DOI] [PubMed] [Google Scholar]
- 11.Tsai J, Middleton M, Retkin R, et al. Partnerships Between Health Care and Legal Providers in the Veterans Health Administration. Psychiatric Services appi.ps.201600486. 2016 doi: 10.1176/appi.ps.201600486. [DOI] [PubMed] [Google Scholar]
- 12.Goldman HH, Morrissey JP, Ridgely MS. Evaluating the Robert Wood Johnson Foundation program on chronic mental illness. Milbank Q. 1994:37–47. [PubMed] [Google Scholar]
- 13.Druss BG, Esenwein von SA, Glick GE, et al. Randomized Trial of an Integrated Behavioral Health Home: The Health Outcomes Management and Evaluation (HOME) Study. American Journal of Psychiatry. 2017;174:246–255. doi: 10.1176/appi.ajp.2016.16050507. [DOI] [PubMed] [Google Scholar]
- 14.Anderson LM, Adeney KL, Shinn C, et al. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;6:CD009905. doi: 10.1002/14651858.CD009905.pub2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26075988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells KB, Jones L, Chung B, et al. Community-Partnered Cluster-Randomized Comparative Effectiveness Trial of Community Engagement and Planning or Resources for Services to Address Depression Disparities. Journal of General Internal Medicine. 2013;28:1268–1278. doi: 10.1007/s11606-013-2484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung B, Ong M, Ettner SL, et al. 12-Month outcomes of community engagement versus technical assistance to implement depression collaborative care: a partnered, cluster, randomized, comparative effectiveness trial. Ann Intern Med. 2014;161:S23–S34. doi: 10.7326/M13-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang R, Lagakos SW, Ware JH, et al. Statistics in medicine—reporting of subgroup analyses in clinical trials. New England Journal of Medicine. 2007;357:2189–2194. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 18.United States Social Security Administration. Disability Evaluation Under Social Security [Internet] 2016 httpswww.ssa.govdisabilityprofessionalsbluebook.-MentalDisorders-Adult.htm Available from: https://www.ssa.gov/disability/professionals/bluebook/12.00-MentalDisorders-Adult.htm.
- 19.Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-, HHS Publication No. SMA -, 2014. Available from: http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf.
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11556941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. Journal of affective disorders. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 22.Community Partners in Care: Depression Toolkit Resources. 2016 httpwww.communitypartnersincare.orgdepression-toolkit-resources.
- 23.Khodyakov D, Sharif MZ, Dixon EL, et al. An implementation evaluation of the community engagement and planning intervention in the CPIC depression care improvement trial. Community Mental Health Journal. 2014;50:312–324. doi: 10.1007/s10597-012-9586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung B, Ngo VK, Ong MK, et al. Participation in Training for Depression Care Quality Improvement: A Randomized Trial of Community Engagement or Technical Support. Psychiatr Serv. 2015;66:831–839. doi: 10.1176/appi.ps.201400099. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25930037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landry CM, Jackson AP, Tang L, et al. The Effects of Collaborative Care Training on Case Managers’ Perceived Depression-Related Services Delivery. Psychiatric Services appi.ps.201500550. 2016 doi: 10.1176/appi.ps.201500550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West SG, Duan N, Pequegnat W, et al. Alternatives to the randomized controlled trial. American Journal of Public Health. 2008;98:1359–1366. doi: 10.2105/AJPH.2007.124446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.John E Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8628042. [DOI] [PubMed] [Google Scholar]
- 28.Wells KB, Sturm R, Burnam A. National Survey of Alcohol, Drug, and Mental Health Problems (Healthcare for Communities), 1997–1998 (2nd ICPSR Version) Los Angeles, CA: 2003. [Google Scholar]
- 29.Groves RM, Dillman DA, Eltinge JL, et al. Survey nonresponse. New York, NY: Wiley-Interscience; 2002. [Google Scholar]
- 30.Korn EL, Graubard BI. Analysis of health surveys. In: Groves RM, Kalton G, Schwarz N, et al., editors. Probability and Statistics Survey Methodology Section. New York, NY: 1999. [Google Scholar]
- 31.Lavori PW, Dawson R, Shera D. A multiple imputation strategy for clinical trials with truncation of patient data. Statistics in Medicine. 1995;14:1913–1925. doi: 10.1002/sim.4780141707. [DOI] [PubMed] [Google Scholar]
- 32.Binder DA. On the variances of asymptotically normal estimators from complex surveys. International Statistical Review/Revue Internationale de Statistique. 1983:279–292. [Google Scholar]
- 33.Rubin DB. Multiple imputation for nonresponse in surveys. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- 34.Ong MK, Jones L, Aoki W, et al. A community-partnered, participatory, cluster-randomized study of depression care quality improvement: Three-year outcomes. Psychiatric Services. doi: 10.1176/appi.ps.201600488. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murali V, Oyebode F. Poverty, social inequality and mental health. Advances in psychiatric treatment. 2004;10:216–224. [Google Scholar]
- 36.Jenkins R, Bhugra D, Bebbington P, et al. Debt, income and mental disorder in the general population. Psychological Medicine. 2008;38:1485–1493. doi: 10.1017/S0033291707002516. [DOI] [PubMed] [Google Scholar]
- 37.Bond GR, Drake RE, Mueser KT, et al. Assertive community treatment for people with severe mental illness. Disease Management and Health Outcomes. 2001;9:141–159. [Google Scholar]
- 38.Alley DE, Asomugha CN, Conway PH, et al. Accountable Health Communities--Addressing Social Needs through Medicare and Medicaid. N Engl J Med. 2016;374:8–11. doi: 10.1056/NEJMp1512532. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26731305. [DOI] [PubMed] [Google Scholar]
- 39.California Department of Health Care Services. Whole Person Care Pilots [Internet] 2016 Available from: http://www.dhcs.ca.gov/services/Pages/WholePersonCarePilots.aspx.
- 40.Los Angeles County Department of Mental Health. MHSA Innovation 2 Project – Health Neighborhoods. 2015 [Google Scholar]
- 41.New York State Department of Health: Frequently Asked Questions (FAQs) New York’s MRT Waiver Amendment Delivery System Reform Incentive Payment (DSRIP) Plan [Internet] 2016 Available from: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/dsrip_faq/docs/2016-07_dsrip_faq.pdf.
- 42.Gilbody SM, House AO, Sheldon TA. Routinely administered questionnaires for depression and anxiety: systematic review. BMJ. 2001;322:406–409. doi: 10.1136/bmj.322.7283.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Connor EA, Whitlock EP, Beil TL, et al. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151:793–803. doi: 10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.