Abstract
BACKGROUND
Identifying distinct trajectories of change in body weight during inpatient treatment for anorexia nervosa (AN) may provide knowledge about the process of weight restoration and may help detect optimal body weight response patterns among individuals who are at risk for not achieving weight restoration or leaving treatment prematurely.
OBJECTIVE
This study explored the extent to which distinct trajectories of change in body weight existed among individuals during inpatient treatment for AN.
DESIGN
Group-based trajectory modeling was used to identify distinct trajectories of change in body weight among 500 individuals receiving inpatient treatment for AN.
RESULTS
Four distinct trajectories were identified: weight gain (n = 197), treatment resistant (n = 177), weight plateau (n = 82), and weight fluctuate (n = 44).
CONCLUSION
Clinically, it is important to consider the heterogeneity of changes in body weight during inpatient treatment to help guide interventions and outcomes.
Keywords: anorexia nervosa, body weight, trajectories, inpatient treatment, weight restoration
Introduction
Weight restoration is an established integral component of inpatient treatment for anorexia nervosa (AN; American Psychiatric Association, 2006). Inpatient treatment for AN is often required to intervene with cognitive impairment and medical consequences resulting from severe deficiency in caloric energy intake and malnutrition (American Psychiatric Association, 2006). Research indicates that weight restoration during inpatient treatment may be the best predictor of outcome (Kaplan et al., 2009; Lund et al., 2009; Zipfel, Löwe, Reas, Deter, & Herzog, 2000). However, studies examining the efficacy of inpatient treatment suggest that up to 56% of patients choose to leave inpatient treatment prematurely (Fassino, Piero, Tomba, & Abbate-Daga, 2009; Huas et al., 2011; Sly & Bamford, 2011), an estimated 40% of weight-restored patients relapse within a year of discharge (Carter et al., 2012), and approximately 20% of patients remain chronically ill or die (Fichter, Quadflieg, & Hedlund, 2006; Steinhausen, 2002). These findings suggest that the majority of individuals do not achieve and/or maintain weight restoration with inpatient treatment.
Several studies have indicated that there is variation in weight restoration during an inpatient admission for AN (e.g., Davies & Jaffa, 2005; Garber, Michihata, Hetnal, Shafer, & Moscicki, 2012; Hart, Abraham, Franklin, & Russell, 2011; Hartmann, Wirth, & Zeeck, 2007; Lund et al., 2009; Mewes, Tagay, & Senf, 2008). For example, Hartmann et al. (2007) found that individuals who gained weight in Weeks 1 and 2 and then proceeded to have a significant weight gain during Weeks 3 and 4 without much fluctuation had a higher probability of at least moderate treatment success. In contrast, patients who lost weight in Weeks 1 and 2 and even more weight loss in Weeks 3 and 4 with fluctuation had a higher probability of treatment failure. Results also indicated that having a constant but slow weight gain during Weeks 1 and 2 does not indicate treatment failure. In another study, Hart and colleagues examined weekly and total weight gain in patients admitted to an inpatient eating disorders unit at a private psychiatric hospital (Hart et al., 2011). Findings suggest that a subset of individuals will initially lose weight secondary to fluid retention or have minimal weight gain during the first week of treatment, followed by significant weight gain and/or weight fluctuations for the remainder of their admission (Hart et al., 2011). Furthermore, Hart et al. (2011) reported that a smaller subset of patients will not gain but lose weight during their admission.
Over the past 20 years, research has begun to take into consideration the importance of capturing changes in body weight over a period of time by using statistical analyses that more appropriately fit the data. For example, Mewes et al. (2008) examined parameters of weight curves as predictors of dropout and completion of treatment. More specifically, the variables of interest relating to weight curves included the period of weight loss, the number of periods of weight loss, the average magnitude of weight loss, the average duration of weight loss, and the average weekly body mass index (BMI) gain. Findings suggest that three predictors of BMI gain up to discharge explained 69% of variance among treatment dropouts. A higher average weekly BMI gain, a lower average duration of weight loss, and a longer duration of the first half of treatment predicted higher BMI gain up to discharge. Among treatment completers, a lower BMI at admission and a higher average weekly BMI gain in the first half of treatment predicted a higher BMI gain up to discharge, and both predictors explained 51.8% of the variance.
Similarly, Lay, Jennen-Steinmetz, Reinhard, and Schmidt (2002) conducted a longitudinal study that investigated changes in body weight during and after inpatient treatment among female adolescents. In this study, the variables of interest relating to weight curves were average BMI, convexity of the weight curve, negative variation, total variation, and variability, and these parameters of weight curves were used to predict treatment outcomes. Results showed that the average overall weight increase was 9.4 kg, or 2.5 kg per month, but only 77% of participants (n = 31) achieved target weight and 22.5% (n = 9) maintained it for at least 10 days while in treatment (Lay et al., 2002). Additionally, about 72% of patients had substantial weight loss within 8 weeks of discharge, and 77.5% were readmitted within 12 months following discharge. Furthermore, patients with greater negative variation of weight curve and greater tempo of weight increase were more likely to lose weight after discharge compared to others.
Another study examined predictors of failure in the early course of first admission for inpatient treatment among 85 individuals using growth curve analysis and regression with methods of optimal scaling (Hartmann et al., 2007). The statistical analyses had three steps, including reduction of longitudinal weight gain data to three parameters of linear weight gain curves, nonlinear regression of outcome class with methods of optimal scaling using the three curve parameters, and receiver operating characteristic curve analyses. Results showed that BMI at admission was negatively correlated to outcome, with a higher mean BMI at admission for individuals who did not respond to treatment compared to those who did respond to treatment.
Although researchers have begun to take into consideration the nonlinearity and variability of weight changes during inpatient treatment for AN, the majority of existing studies are descriptive in nature or examined the relationship between weight change and treatment outcomes. The identification of distinct weight trajectories and potential differences in demographic and clinical characteristics among the identified trajectories will provide a better understanding of the process of weight restoration, including potential differences and similarities within this population. Such knowledge may also help identify optimal body weight response patterns among individuals who are at risk for not achieving weight restoration or leaving treatment prematurely. Thus, this study examined daily body weights to explore the extent to which distinct trajectories of change in body weight exist among individuals with AN during inpatient treatment.
Method
Participants
Participants were individuals diagnosed with AN (N = 500) admitted to the inpatient unit at an eating disorder treatment facility in the Northeast U.S. Inclusion criteria was a diagnosis of AN at admission based on both the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000) and DSM-5 (American Psychiatric Association, 2013). At time of admission, the mean BMI was 15.9 kg/m2 (SD = 1.5); 70.4% (n = 352) of the sample were restricting subtype of AN; the mean duration of illness was 8.8 years (SD = 11.1); and 46.6% of the sample (n = 234) had at least one prior inpatient treatment for AN. Diagnoses were determined by an unstructured clinical interview with a unit psychiatrist or advanced practice nurse practitioner. All participants met either DSM-IV-TR or DSM-5 criteria, which was dependent on the year of admission with the DSM-5 being used exclusively starting October 1, 2015. Exclusion criteria were (a) meets DSM-IV-TR or DSM-5 criteria for psychotic disorder at admission and (b) prior chart reviewed in the study (omitted repeat admissions).
Setting
The organization provides a full continuum of care to individuals suffering from eating and psychiatric disorders. In 2015, the eating disorders inpatient unit had a bed capacity of 23 with a readmission rate of 13.4% and an average length of stay of 13.8 days. The primary goals of the eating disorder inpatient program include weight restoration and monitoring, nutrition education, and milieu therapy to address abnormal eating attitudes and behaviors. On admission to the inpatient unit, medical, psychiatric, psychosocial, psychological, and nutritional evaluations were completed. The unit’s protocol recommends that individuals gain weight by ingesting liquids and/or solid foods during supervised meals, and individuals are expected to consume 100% the prescribed calories. If an individual is unable to or unwilling to consume the prescribed calories, then a liquid nutrition supplement or nasogastric feeding will be provided. Patients were weighed on the day of admission and then daily over the course of treatment. All weighins were supervised by nursing staff with the patient wearing underwear and/or hospital gown. Per protocol, patients were blindly weighed (i.e., not able to view weight). The anthropometric devices were inspected and calibrated per the treatment facility’s protocol. Detailed records of daily body weights were kept as part of the standard of care.
Procedures
This study was reviewed and approved by Boston College’s Institutional Review Board. Random sampling was used to ensure that each individual in the population has an equal probability of being selected (Creswell, 2014). Medical record numbers (MRNs) were randomly selected from the list of all admissions with a diagnosis of AN between January 1, 2012, and December 31, 2015, and stratified by quarters to account for seasonal and academic variability. The randomly selected admission was not necessarily the first admission for the patient. An MRN was included in the study up to one time, and subsequent selections of the number were discarded. This method allowed for 500 unique MRNs, which was the target sample size based on indications that the maximum likelihood estimates obtained in group-based trajectory modeling (GBTM) provide close estimate of the true population values and have normal distribution with a minimum of this sample size (Loughran & Nagin, 2006).
Analyses
Data were analyzed using GBTM with Stata software, Version 9.3 (StataCorp, 2015) and the PROC TRAJ macro (http://www.andrew.cmu.edu/user/bjones), a closed-source module developed specifically for use with Stata software. The purpose of GBTM is to group individuals who follow similar growth trends and identify differences of each trajectories, and it assumes that the population is composed of a mixture of distinct groups defined by trajectories (Nagin & Odgers, 2010). Unlike hierarchical and latent curve modeling (two main approaches for analyzing developmental trajectories), which provides modeling of a single average trajectory, GBTM identifies relatively homogenous clusters of trajectories (Loughran & Nagin, 2006).
Trajectories of change in body weight were based on the identification of relatively homogenous clusters of individuals who followed similar trends of change in body weight, and derived from daily body weights from admission to discharge. Bayesian information criterion (BIC) was used to identify the number of groups that best characterized the data with a stepwise approach to increase the number of groups in the model specification to the identified maximum solutions. A censored normal distribution was assumed, and shapes for the trajectories (e.g., cubic, linear) were compared for optimal mode fit. The BIC approach selects the number of groups that best represent the heterogeneity among the trajectories, and corrects for the complexity of the models (i.e., quadratic number of groups; Nagin & Odgers, 2010). Smaller BICs indicate a better fit, but theory and parsimony must also be considered in model selection (Nagin & Odgers, 2010).
Differences among the trajectories were examined using analysis of variance (ANOVA) with Tukey’s honestly significant difference post hoc tests (continuous variables) or chi-square (categorical variables). To protect against Type I error, α was set at .01. Statistically significant findings suggest that individuals were more likely to be in one trajectory compared to others, and did not assert that factors were predictors of trajectories. Clinical characteristics of interest were screened for skewness and kurtosis. Length of stay and duration of illness were positively skewed, and BMI at admission was negatively skewed. Transformations were made but did not significantly change the skewness of the data, and thus the original data were kept. To examine whether sub-samples of individuals clustered into any of the trajectories and to limit unneeded bias, analyses did not control for length of stay, an outcome variable.
Descriptive analyses compared the demographics of the sample to the target population, using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Approximately 96% (n = 482) of the data were completed cases, and 3.6% (n = 18) were missing data for level of education due to not being documented in the charts. Regarding daily weights, 2.6% (n = 13) of participants were missing data for up to four daily body weights, with 46.2% (n = 6) of those missing daily weight data for 1 day only. For all analyses, no changes or imputations were made (Nagin & Odgers, 2010). Statistical significance was set at p < .05, two-tailed.
Results
Demographic and Clinical Characteristics
Participants were predominantly Caucasian (91.4%) and female (90.4%), with a mean age of 26.8 years (SD = 13.9, range = 11–69). Details about demographic characteristics are provided in Table 1.
Table 1.
Demographic Characteristics of the Sample.
| Characteristic | N | % |
|---|---|---|
| Gender | ||
| Female | 452 | 90.4 |
| Male | 48 | 9.6 |
| Race/ethnicity | ||
| White | 458 | 91.6 |
| Black | 8 | 1.6 |
| Asian | 12 | 2.4 |
| Hispanic | 13 | 2.6 |
| Bi/multiracial | 6 | 1.2 |
| Other | 3 | 0.6 |
| Education (n = 482)a | ||
| ≤9th grade | 61 | 12.6 |
| >9th grade to ≤12th grade | 183 | 37.9 |
| >12th grade to ≤16 years of education | 201 | 41.7 |
| >16 years of education | 37 | 7.7 |
| Marital status | ||
| Never married | 401 | 80.2 |
| Married | 68 | 13.6 |
| Separated | 23 | 4.6 |
| Divorced | 8 | 1.6 |
| Living situation | ||
| Alone | 63 | 12.6 |
| With significant other | 38 | 7.6 |
| With roommate(s)/friend(s) | 36 | 7.2 |
| With family | 351 | 70.2 |
| Other (e.g., foster care) | 12 | 2.4 |
Sample sizes were smaller than N = 500 due to missing data.
Approximately 75% (n = 373) of individuals were diagnosed with at least one psychiatric comorbidity; 69.4% (n = 347) of individuals were prescribed at least one psychotropic medication at time of admission; and 28.2% (n = 141) were prescribed an atypical antipsychotic (e.g., olanzapine, quetiapine, risperidone). At time of admission, the mean body weight was 42.6 kg (SD = 6.2) and the average BMI was 15.9 kg/m2 (SD = 1.5). At time of discharge, the average change in body weight was 2.5 kg (SD = 2.3), and the mean change in BMI was 1.0 kg/m2 (SD = 0.9). The average length of stay was 16 days (SD = 12.6). Details about clinical characteristics are provided in Table 2.
Table 2.
Statistics for Clinical Characteristics of the Sample.
| Characteristic | M (SD) | Range |
|---|---|---|
| Length of stay (days) | 16.0 (12.6) | 2–106 |
| Duration of illness (years) | 8.8 (11.1) | 0–50 |
| Body weight (kg) at admission | 42.6 (6.3) | 24.3–63.3 |
| Body weight (kg) at discharge | 45.1 (6.3) | 25.3–70.2 |
| BMI (kg/m2) at admission | 15.9 (1.5) | 10.1–18.5 |
| BMI (kg/m2) at discharge | 16.9 (1.5) | 11.8–22.8 |
|
| ||
| N | % | |
|
| ||
| Subtype of AN | ||
| Binge/purge | 148 | 29.6 |
| Restricting | 352 | 70.4 |
| Discharge disposition | ||
| Residential | 135 | 27.0 |
| Partial hospitalization | 84 | 16.8 |
| Intensive outpatient | 34 | 6.8 |
| Lower level of care at different organization | 24 | 4.8 |
| Home to outpatient team | 93 | 18.6 |
| Home | 63 | 12.6 |
| Against medical advice | 37 | 7.4 |
| Transfer to medical facility | 18 | 3.6 |
| Other (e.g., state hospital) | 12 | 2.4 |
Note. AN = anorexia nervosa; BMI = body mass index.
Trajectories of Change in Body Weight
The maximum number of trajectories was five, and BIC was used with a stepwise approach to increase the number of groups in the model specification three-, four-, and five-group solutions. BIC values and predicted group proportions for solutions are shown in Table 3. The five-group solution was rejected because the predicted group proportions were less than the recommended minimum threshold of .70 for each group (Nagin & Odgers, 2010). Based on the BIC, fit statistics, and the size of each group, the four-group solution was selected as the best fitting model.
Table 3.
Fit Indices and Predicted Group Proportions for Group-Based Trajectory Models.
| No. of groups | BIC | AIC | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Group 6 |
|---|---|---|---|---|---|---|---|---|
| 3 | −22193.55 | −22161.94 | .21 | .50 | .29 | |||
| 4 | −20719.72 | −20677.57 | .16 | .39 | .36 | .09 | ||
| 5 | −19600.91 | −19566.76 | .10 | .27 | .34 | .24 | .05 |
Note. BIC = Bayesian information criterion; AIC = Akaike information criterion. Text in boldface denotes the best fitting model.
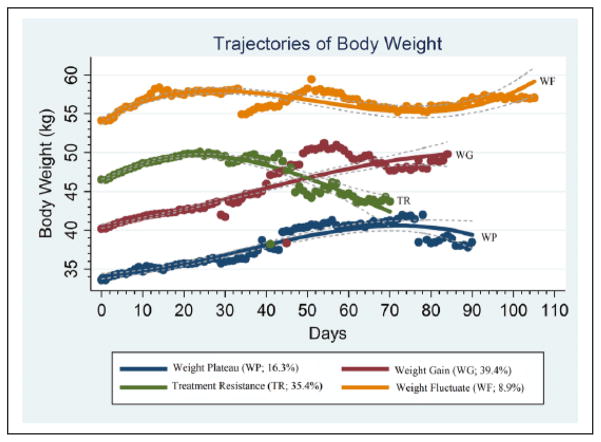
The final group-based trajectory model for body weight (kg) over time (days) was the four-group solution, and included weight gain (WG; n = 197; 39.4%), treatment resistant (TR; n = 177; 35.4%), weight plateau (WP; n = 82; 16.4%), and weight fluctuate (WF; n = 44; 8.8%) groups. Figure 1 provides the trajectories of the groups. The solid lines in Figure 1 are based on the parameter estimates of the model, and the dashed lines form the 95% confidence intervals on the estimated probabilities of group membership. The dots are calculated with the actual data in which individuals’ responses are weighted based on posterior probabilities of group membership. The confidence intervals on the graph have minimal overlap, indicating that the model captures distinctive features of the population distribution of trajectories.
Figure 1.
The four-group solution was the best-fitting model for trajectories of body weight (kg) over time (days).
Figure 1 indicates that body weight at admission influences trajectory group membership. Thus, a model for change in body weight over time (i.e., body weight at admission was subtracted from all weights) was considered. Additionally, a one-way ANOVA and Bonferroni post hoc test revealed that length of stay was significantly different based on discharge dispositions such that individuals who dropped out of treatment had a shorter length of stay (7.6 ± 6.5) compared to those discharged to residential treatment (16.9 ± 15.0, p < .005), partial hospitalization (17.8 ± 11.2, p < .001), lower level of care at different facility (18.4 ± 9.8 p < .05), home to outpatient team (16.7 ± 10.8, p < .01), and other disposition (27.2 ± 27.3, p < .001). Thus, a model that excluded individuals who were discharged within 7 days of admission was considered. Both alternative models were rejected because the original four-group model captured more distinctive features of the population distribution of trajectories.
Demographic and Clinical Characteristics by Trajectories
Table 4 provides a summary of the demographic and clinical characteristics by trajectory groups. There were significant group differences in demographic and clinical characteristics. Males were significantly more likely to be assigned to the WF group compared to other groups, χ2(3, n = 500) = 85.34, p < .001. Individuals assigned to the WF group were significantly less likely to have been readmitted to the unit compared to other groups, χ2(3, n = 500) = 7.87, p < .05.
Table 4.
Summary of Percentages, Means, and Standard Deviations for Demographic and Clinical Characteristics by Trajectory Groups.
| Characteristic | Weight gain (N = 197), n (%) | Treatment resistant (N = 177), n (%) | Weight plateau (N = 82), n (%) | Weight fluctuate (N = 44), n (%) | ||
|---|---|---|---|---|---|---|
| Female | 190 (96.4) | 160 (90.4) | 79 (96.3) | 21 (47.7) | ||
| Male | 7 (3.6)a | 17 (9.6)a | 3 (3.7)a | 23 (52.3)a | ||
| Binge eating/purging | 58 (29.4) | 58 (32.8) | 18 (22.0) | 14 (31.8) | ||
| Restricting | 139 (70.6) | 119 (67.2) | 64 (78.0) | 30 (68.2) | ||
|
| ||||||
| M (SD) | M (SD) | M (SD) | M (SD) | F | p | |
|
| ||||||
| History of prior inpatient treatment for AN | 98 (49.7) | 75 (42.4) | 44 (53.7) | 17 (38.6) | 1.60 | NS |
| Duration of illness (years) | 9.4 (11.2)a | 8.4 (11.2)b | 12.1 (12.6)c | 3.2 (3.5)a,b,c | 5.25 | .002 |
| Readmitted to unit | 73 (37.1)a | 56 (31.6)a | 30 (36.6)a | 7 (15.9)a | 2.64 | .05 |
| Age (in years) | 27.6 (14.2)a | 26.7 (14.0)b | 28.4 (14.8)c | 20.5 (7.8)a,b,c | 3.71 | .01 |
| Admission | ||||||
| Body weight (kg) | 40.2 (2.4)a,d,e | 46.5 (2.2)b,d,f | 33.6 (2.7)a,b,c | 54.2 (3.6)c,e,f | 883.98 | <.001 |
| BMI | 15.5 (1.2) | 16.9 (1.0) | 14.2 (1.1) | 17.4 (.8) | 159.44 | <.001 |
| % of IBW | 74.7 (6.3) | 81.4 (5.7) | 69.1 (6.8) | 83.7 (5.5) | 104.24 | <.001 |
| Discharge | ||||||
| Body weight (kg) | 42.8 (2.3)a,d,e | 48.9 (2.5)b,d,f | 36.4 (3.1)a,b,c | 56.8 (4.3)c,e,f | 707.67 | <.001 |
| BMI at discharge | 16.5 (1.2) | 17.8 (1.2) | 15.4 (1.4) | 18.2 (1.1) | 98.16 | <.001 |
| % of IBW | 79.5 (6.3) | 85.6 (6.6) | 74.8 (7.3) | 87.8 (6.5) | 67.43 | <.001 |
| Admission caloric intake (kcal) | 1,877 (373) | 1,976 (441)a | 1,791 (334)a,b | 2,032 (398)b | 5.98 | <.001 |
| Length of stay (days) | 16.3 (12.3) | 13.8 (9.7)a | 19.0 (14.6)a | 17.1 (18.3) | 3.47 | .02 |
Note. AN = anorexia nervosa; BMI = body mass index (kg/m2); IBW = ideal body weight; NS = not statistically significant. Different superscripts denote statistically significant group differences after post hoc comparisons.
As determined by one-way ANOVA, there were also significant group differences in age, gender, readmission to unit, duration of illness, admission caloric intake, body weight at admission and discharge, and length of stay. Group differences were tested using pairwise t tests adjusted for multiple comparisons with Tukey’s honest significant difference. These tests revealed that individuals assigned to the WF group were significantly younger compared to individuals assigned to the WG (−7.12 ± 2.30, p = .01), TR (−6.17 ± 2.32, p = .04), and WP (−7.97 ± 2.58, p = .01) groups. Furthermore, duration of AN was significantly less in the WF compared to other groups, in that individuals assigned to the WF group reported fewer years with AN compared to individuals assigned to the WG (−6.24 ± 1.98, p = .01), WP (−8.93 ± 2.31, p = .001), and TR (−5.22 ± 2 p = .05) groups. At admission, individuals assigned to the WP group were initiated on a significantly lower caloric intake than the TR (−184.71 ± 52.76, p = .003) and WF (−240.65 ± 73.81, p = .007) groups. The WP group also had significantly lower body weight at admission compared to the TR (−12.93 ± .33, p < .001), WF (−20.61 ± .46, p < .001), and WG (−6.62 ± .33, p < .001) groups. Moreover, the WG group had lower body weight at admission compared to the TR (−6.31 ± .26, p < .001) and WF (−13.98 ± .41, p < .001) groups, and the TR group had lower body weight compared to the WF group (−7.67 ± .42, p < .001). Group differences in body weight at discharge followed a comparable trend, in that body weight was significantly lower in the WP group compared to the TR (−12.46 ± .36, p < .001), WF (−20.42 ± .51, p < .001), and WG (−6.40 ± .36, p < .001) groups. Additionally, the WG group had significantly lower body weight at discharge compared to the TR (−6.06 ± .28, p < .001) and WF (−14.02 ± .45, p < .001) groups, and the TR group had lower body weight compared to the WF group (−7.96 ± .46, p < .001). Although there were significant group differences in body weight at time of admission and discharge, there were no group differences in overall change in body weight. Finally, individuals assigned to the TR group had a significantly shorter length of stay compared to the WP group (−5.15 ± 1.67, p = .01). Means, standard deviations, and percentages are presented in Table 4.
Discussion
This study examined trajectories of change in body weight during inpatient treatment for AN. The four-group solution was the final model; groups were identified as weight gain, treatment resistant, weight plateau, and weight fluctuate. These findings provide a better understanding of the process of weight restoration and potential mechanisms that may promote or inhibit weight restoration. This was one of the first studies to examine trajectories of change in body weight among a relatively large sample (N = 500) of unique individuals with AN who were admitted to inpatient treatment. Furthermore, all individuals of the randomized sample were included in the analyses regardless of length of stay or treatment failure.
Findings from this study are similar to other studies that have found variation in changes of weight during inpatient treatment (Garber et al., 2012; Hart et al., 2011). The WP group followed the most common weight curve for individuals during inpatient treatment for AN, in that individuals displayed a rapid weight gain at the beginning and then leveled off near the end of treatment (Davies & Jaffa, 2005; Lay et al., 2002; Vansteelandt, Pieters, Vanderlinden, & Probst, 2010). The WF group displayed fluctuations of body weight over the length of stay, had the highest body weights at admission, and longer lengths of stays compared to other groups. Individuals assigned to the WP group displayed a more constant increase in body weight and then plateaued followed by a slight decrease. This group had the lowest body weights and BMIs at admission, the lowest admission caloric intakes, and the greatest changes in body weight from admission to discharge.
Surprisingly, the TR group was the second largest subset of the sample, and individuals assigned to this group were more likely to have an initial increase in body weight, followed by a decrease with some body weights at discharge being lower than body weights at admission. According to Mehler, Winkelman, Andersen, and Gaudiani (2010), individuals with AN tend to have lower resting energy expenditure at time of admission compared to later in the admission. It is commonplace for individuals with AN to require high levels of caloric intake for abbreviated period of time to promote weight gain (Mehler et al., 2010). It is possible that individuals assigned to this trajectory did not have the necessary caloric requirements to maximize weight gain during inpatient treatment. Another explanation is that individuals who are assigned to the TR trajectory may experience more difficulties with inpatient treatment and choose to leave treatment prematurely.
Research suggests a balance between the physiological and psychological changes during inpatient treatment for AN (Hart et al., 2011; Herzog, Zeeck, Hartmann, & Nickel, 2004). However, since numerous stakeholders are involved in determining length of stay, decisions regarding length of stay are complex and may not be dependent on body weight alone. It is also possible that individuals assigned to different trajectories have different metabolic states throughout treatment, which may affect weight gain and loss as well as body weight at discharge. Results from this study suggest that there is a need for tailored assessments and interventions for individuals during inpatient treatment for AN.
There are several limitations to consider. First, as a retrospective chart review, the research design lacked a rigorously standardized prospective real-time approach, but it was representative of real-world treatment. Second, diagnoses of AN were based on unstructured interviews conducted by a number of different clinicians. It is possible that the current study does not have a representative sample of males because clinicians were more likely to diagnose males with unspecified eating disorders versus AN. Research suggests that eating disorders have a highly skewed sex distribution, with the proportion of unspecified eating disorder cases being significantly higher among males compared to females, and most likely a reflection of underdiagnosis and undertreatment in males (Raevuori, Keski-Rahkonen, & Hoek, 2014). Although the DSM-5 provides a more sex-neutral diagnostic criteria for AN, clinician bias may still have contributed to the underdiagnosis of AN in males (Merikangas et al., 2011). Third, the sample may not be fully representative of the target population. The setting was a proprietary health care company, and thus the treatment provided may not be representative of other treatment facilities with a different business or treatment model. Likewise, the homogeneity of the sample is a limitation. The majority of the participants were non-Hispanic White females. Although the current study was similar to studies that examined prevalence rates of eating disorders (Hudson, Hiripi, Pope, & Kessler, 2007; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011), the sample was not diverse with respect to race and sex. Research suggests that males are less likely to be diagnosed and seek treatment for an eating disorder, and mental health service utilization is significantly lower among ethnic and racial minority groups compared to Whites (Merikangas et al., 2011). Since the majority of studies recruit participants from treatment facilities, samples will inherently under-represent certain subpopulations. Finally, GBTM does not identify trajectories of actual groups of individuals; GBTM identifies relatively homogenous trajectories based on data and specifies the likelihood of individuals to be assigned to one of the trajectories (Loughran & Nagin, 2006; Nagin & Odgers, 2010). Despite these limitations, this is the largest data set to date to have looked at trajectories of change in body weight among individuals with AN during inpatient treatment.
Implications
This study highlighted the heterogeneous trajectories of changes in body weight among individuals with AN admitted to inpatient treatment. Replication of this study in different treatment settings and more diverse population is necessary to capture the similarities and differences in treatment across the continuum of care. Additionally, the examination of predictors of patterns of change in body weight is needed to help define and develop more effective clinical assessments and interventions that are more individualized and based on assessments at time of admission and throughout the length of the admission. Finally, intervention studies will provide knowledge to tailor interventions for optimizing weight restoration in the WG group and having crossover into the WG group. Hart et al. (2011) argue that best practice in the process of weight restoration involves the identification of patterns of change in body weight and is one of the most important aspect of inpatient treatment for AN. Further identification of differences between individuals during inpatient treatment will help develop assessments and interventions to alter trajectories toward the WG group and optimize weight restoration in the WG group. Such assessments and interventions would be tailored to the individual rather than the one-size-fits-all approach.
Acknowledgments
Funding
This paper was supported, in part, by the National Institute of Mental Health (T32MH082761), Jonas Nurse Leaders Scholar Program Scholarship, and Boston College Graduate Student Research Fellowship.
Footnotes
Author Roles
All authors contributed to proposal development, study procedures, writing and editing the article, and approving the final version to be published.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- American Psychiatric Association. Practice guideline for the treatment of patients with eating disorders. (3) 2006 Retrieved from http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/eatingdisorders.pdf.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Carter JC, Mercer-Lynn KB, Norwood SJ, Bewell-Weiss CV, Crosby RD, Woodside DB, Olmsted MP. A prospective study of predictors of relapse in anorexia nervosa: Implications for relapse prevention. Psychiatry Research. 2012;200:518–523. doi: 10.1016/j.psychres.2012.04.037. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. 4. Thousand Oaks, CA: Sage; 2014. [Google Scholar]
- Davies S, Jaffa T. Patterns of weekly weight gain during inpatient treatment for adolescents with anorexia nervosa. European Eating Disorders Review. 2005;13:273–277. [Google Scholar]
- Fassino S, Piero A, Tomba E, Abbate-Daga G. Factors associated with dropout from treatment for eating disorders: A comprehensive literature review. BMC Psychiatry. 2009;9:67. doi: 10.1186/1471-244X-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichter MM, Quadflieg N, Hedlund S. Twelve-year course and outcome predictors of anorexia nervosa. International Journal of Eating Disorders. 2006;39:87–100. doi: 10.1002/eat.20215. [DOI] [PubMed] [Google Scholar]
- Garber AK, Michihata N, Hetnal K, Shafer MA, Moscicki AB. A prospective examination of weight gain in hospitalized adolescents with anorexia nervosa on a recommended refeeding protocol. Journal of Adolescent Health. 2012;50:24–29. doi: 10.1016/j.jado-health.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart S, Abraham S, Franklin R, Russell J. Weight changes during inpatient refeeding of underweight eating disorder patients. European Eating Disorders Review. 2011;19:390–397. doi: 10.1002/erv.1052. [DOI] [PubMed] [Google Scholar]
- Hartmann A, Wirth C, Zeeck A. Prediction of failure of inpatient treatment of anorexia nervosa from early weight gain. Psychotherapy Research. 2007;17:218–229. doi: 10.1080/10503300600702315. [DOI] [Google Scholar]
- Herzog T, Zeeck A, Hartmann A, Nickel T. Lower targets for weekly weight gain lead to better results in inpatient treatmetn of anorexia nervosa: A pilot study. European Eating Disorders Review. 2004;12:164–168. [Google Scholar]
- Huas C, Godart N, Foulon C, Pham-Scottez A, Divac S, Fedorowicz V, … Rouillon F. Predictors of dropout from inpatient treatment for anorexia nervosa: Data from a large French sample. Psychiatry Research. 2011;185:421–426. doi: 10.1016/j.psychres.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan AS, Walsh BT, Olmsted M, Attia E, Carter JC, Devlin MJ, … Parides M. The slippery slope: Prediction of successful weight maintenance in anorexia nervosa. Psychological Medicine. 2009;39:1037–1045. doi: 10.1017/S003329170800442X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lay B, Jennen-Steinmetz C, Reinhard I, Schmidt MH. Characteristics of inpatient weight gain in adolescent anorexia nervosa: Relation to speed of relapse and readmission. European Eating Disorders Review. 2002;10:22–40. [Google Scholar]
- Loughran T, Nagin DS. Finite sample effects in group-based trajectory models. Sociological Methods & Research. 2006;35:250–278. [Google Scholar]
- Lund BC, Hernandez ER, Yates WR, Mitchell JR, McKee PA, Johnson CL. Rate of inpatient weight restoration predicts outcome in anorexia nervosa. International Journal of Eating Disorders. 2009;42:301–305. doi: 10.1002/eat.20634. [DOI] [PubMed] [Google Scholar]
- Mehler PS, Winkelman AB, Andersen DM, Gaudiani JL. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. Journal of Nutrition and Metabolism. 2010;2010 doi: 10.1155/2010/625782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, … Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mewes R, Tagay S, Senf W. Weight curves as predictors of short-term outcome in anorexia nervosa inpatients. European Eating Disorders Review. 2008;16:37–43. doi: 10.1002/erv.807. [DOI] [PubMed] [Google Scholar]
- Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Raevuori A, Keski-Rahkonen A, Hoek HW. A review of eating disorders in males. Current Opinion in Psychiatry. 2014;27:426–430. doi: 10.1097/YCO.0000000000000113. [DOI] [PubMed] [Google Scholar]
- Sly R, Bamford B. Why are we waiting? The relationship between low admission weight and end of treatment weight outcomes. European Eating Disorders Review. 2011;19:407–410. doi: 10.1002/erv.1061. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 14. College Station, TX: Author; 2015. [Google Scholar]
- Steinhausen H. The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry. 2002;159:1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vansteelandt K, Pieters G, Vanderlinden J, Probst M. Body dissatisfaction moderates weight curves in the inpatient treatment of anorexia nervosa. International Journal of Eating Disorders. 2010;43:694–700. doi: 10.1002/eat.20763. [DOI] [PubMed] [Google Scholar]
- Zipfel S, Löwe B, Reas DL, Deter HC, Herzog W. Long-term prognosis in anorexia nervosa: Lessons from a 21-year follow-up study. The Lancet. 2000;355:721–722. doi: 10.1016/s0140-6736(99)05363-5. [DOI] [PubMed] [Google Scholar]