Abstract
Major depressive disorder (MDD) in young people is a leading cause of disability but most depressed youth are not treated, emphasizing the need for effective prevention. Our goal is to synthesize MDD onset prevention effects for the Blues Program, a brief cognitive-behavioral (CB) indicated prevention group, by merging data from four trials (three of which included CB bibliotherapy) and conducting an individual patient data (IPD) meta-analysis. Data were available from 766 high school/college students (M age = 16.4, SD = 2.3; 60% female, 64% White). CB group resulted in significantly lower MDD incidence rates relative to brochure control that persisted to 6-month follow-up; CB group also was associated with a lower 2-year MDD incidence rate relative to bibliotherapy but heterogeneity across trials was detected. Contrasts between bibliotherapy and brochure control were nonsignificant. For significant contrasts, the number needed to treat (NNT) by CB group to prevent one MDD onset relative to brochure or bibliotherapy ranged from 10 to 21. A brief CB group depression prevention intervention for at-risk adolescent is achieving meaningful effects compared to both active and minimal controls but outcomes need to be improved, perhaps by better screening or augmentations to produce more persistent intervention effects.
Keywords: major depression, prevention, adolescents, cognitive-behavioral, group intervention, bibliotherapy
Major depressive disorder (MDD) in young people is common and highly impairing (e.g., Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015). However, 60-80% of depressed young people do not receive treatment (Cummings & Druss, 2011) and many do not fully benefit from extant treatments (Cuijpers et al., 2014), underscoring the need for effective depression prevention programs. Several depression prevention programs for young people, predominantly focused on high school samples, have been developed, with selective and indicated, but not universal, cognitive-behavioral (CB) prevention programs having the strongest evidence base (e.g., Hetrick, Cox, Witt, Bir, & Merry, 2016; Horowitz & Garber, 2006).
The goal of this report is to synthesize MDD onset prevention effects for the briefest evidence-based group-based CB indicated depression prevention intervention, the Blues Program (Stice, Burton, Bearman, & Rohde, 2007) by merging data from the four available randomized controlled trials (RCTs) that collected diagnostic data and conducting an individual patient data (IPD) meta-analysis. IPD meta-analysis is a specific type of review that differs from standard meta-analysis. In standard meta-analysis, summary scores on a topic are extracted from each study; conversely, in IPD meta-analysis the original data for that topic from participants in each of the various studies are obtained, combined, and re-analyzed. By increasing statistical power, IPD meta-analyses should improve the reliability of results regarding both intervention effects and allow for testing the role of participant-level covariates on effects (Thomas, Radji, & Benedetti, 2014). The first study, which was an efficacy trial conducted with 341 high school students with elevated depressive symptoms, found that participants randomized to CB group or CB bibliotherapy showed lower depressive disorder (MDD or minor depression) onset relative to educational brochure controls over 2-year follow-up (Stice, Rohde, Gau, & Wade, 2010). Based on promising results, the second study, which was an effectiveness trial conducted with 378 high school students with elevated depressive symptoms, found that participants randomized to CB group showed lower MDD onset relative to CB bibliotherapy participants over 2-year follow-up, but neither group differed from educational brochure controls (Rohde, Stice, Shaw, & Gau, 2015). Because youth attending college show high rates of MDD, both due to first incidence and recurrence (e.g., Rohde, Lewinsohn, Klein, Seeley, & Gau, 2013), the next two studies examined this population. The third study, an effectiveness trial conducted with 79 college students with elevated depressive symptoms, found no differences in MDD onset between CB group, CB Bibliotherapy, or educational brochure controls by 1-year follow-up (Rohde, Stice, Shaw, & Gau, 2014). In the fourth trial, we added dissonance-induction elements and participant-driven cognitive and behavioral change plans to improve the depression prevention effects among college students, based on successful outcomes achieved in eating disorder prevention for interventions using cognitive dissonance and participant-driven change principles (Stice, Rohde, Shaw, & Gau, in press); this efficacy pilot with 58 college students with elevated depressive symptoms found no significant differences in MDD onset between CB group and educational brochure controls by 3-month follow-up (Rohde, Stice, Shaw, & Gau, 2016). Thus, the trials differed across sample age, recruitment procedures, exact intervention content, and duration of follow-up, but all examined a 6-session CB group-based prevention program designed to prevent MDD onset versus a brochure control condition. Further, three trials included CB-based bibliotherapy as a second active intervention condition, providing the evaluation of a low-cost intervention previously shown to effectively treat and prevent depression (Gregory, Schwer-Canning, Lee, & Wise, 2004).
The present report sought to document the magnitude and timing of MDD prevention effects up to 2-years post-intervention for the group-based and bibliotherapy-based CB indicated depression prevention interventions relative to both brochure control and each other, in a one-stage IPD meta-analysis with a binary outcome (Thomas et al., 2014). Given the relatively small number of participants who develop MDD in a single RCT, statistical analyses are often underpowered to detect meaningful differences. Synthesizing data from multiple trials using IPD meta-analysis provides a more sensitive method of examining effects. The greater statistical power provided by IPD meta-analysis also increased our ability to examine whether sex and age moderates MDD onset outcomes, as prior standard meta-analyses have found larger symptom reductions for female and older adolescents receiving depression prevention interventions (Horowitz & Garber, 2006).
Method Participants and Procedures
The current study assembled data from 4 RCTs, resulting in 269 adolescents who received the CB group invention, 229 who received CB bibliotherapy, and 268 who served as brochure controls. An adaptation of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Puig-Antich & Chambers, 1983) was used to diagnose DSM-IV MDD in all trials; inter-rater agreement for MDD diagnostic is good (κ = .73 – 1.00; Stice et al., 2010). Additional details regarding each trial are provided in the outcome reports.
Trial 1: High School Efficacy Trial
Between 2004 and 2007, 341 high school students were recruited on the basis of elevated scores (> 20) on the Center for Epidemiologic Studies-Depression scale (CES-D; Radloff, 1977). Participants had a baseline mean age of 15.6 years (SD = 1.2) at pretest, were 56% female and 46% European-American. Eligible participants were randomized to 4 conditions: (1) CB group (n = 88), (2) Supportive-expressive group (n = 88), (3) CB bibliotherapy (n = 80), or (4) Brochure control (n = 83). Groups were facilitated by a clinical psychology graduate student with an undergraduate student co-facilitator. Participants were assessed at pretest, posttest, 6-, 12-, and 24-month post-intervention follow-ups. As this was the only study to employ the supportive-expressive group condition, those participants were not included in the present analyses.
Trial 2: High School Effectiveness Trial
Between 2009 and 2011, 378 high school students were recruited based on a streamlined process in which students self-selected on the basis of a modified CES-D. Participants had a baseline mean age of 15.5 years (SD = 1.2), were 68% female and 72% European-American. Eligible participants were randomized to 3 conditions: (1) CB group (n = 126), (2) CB bibliotherapy (n = 128), or (3) Brochure control (n = 124). Groups were facilitated by pairs of trained personnel at each high school. Participants were assessed at pretest, posttest, 6-, 12-, 18-, and 24-month post-intervention follow-ups.
Trial 3: College Effectiveness Pilot
Between 2010 and 2011, 79 first and second-year college students were recruited based on the same streamlined process as in Trial 2. Participants had a baseline age of 19.0 years (SD = 0.9), were 69% female and 81% European-American. Eligible participants were randomized to 3 conditions: (1) CB group (n = 27), (2) CB bibliotherapy (n = 21), or (3) Brochure control (n = 31). Groups were facilitated by pairs of masters-level graduate students in clinical psychology. Participants were assessed at pretest, posttest, 6- and 12-month follow-ups.
Trial 4: College Pilot with Enhanced CB Intervention
Between 2013 and 2014, 58 college students were recruited using the same screening procedure as Trial 1. Participants had a baseline age of 21.8 years (SD = 2.3), were 68% female and 70% European-American. Eligible participants were randomized to 2 conditions: (1) the enhanced CB group (n = 28) or (2) Brochure control (n = 30). Participants were assessed at pretest, posttest, and 3-month follow-up.
Interventions
CB Group
In all 4 trials, the CB group consisted of 6 weekly 1-hour sessions with approximately 5-8 participants focused on building rapport, increasing pleasant activities, cognitive restructuring, and developing response plans for future life stressors. In Trial 4, we added verbal and written dissonance-induction exercises to enhance motivation and participant-driven cognitive and behavioral change plans to enhance efficacy.
CB Bibliotherapy
Bibliotherapy participants were given a copy of Feeling Good (Burns, 1980), which provides CB techniques for preventing and reducing negative moods written at a high-school reading level. Research or school staff were encouraged to make two reminder calls encouraging participants to use the book.
Educational Brochure control
Participants were given an NIMH educational brochure describing MDD symptoms and treatment (“Let's Talk About Depression” NIH Pub. 01-4162), as well as referral information, which was provided to participants in all conditions.
Statistical Analysis
We used logistic regressions to compare cumulative MDD incidence (onset) between conditions at posttest and 3-, 6-, 12-, and 24-month follow-up. Datasets were merged and analyzed together, controlling for trial. Mplus 7.1 was used to fit separate logistic regressions at each follow-up. Models were run with permutations in dummy-coded conditions to test all pairwise comparisons between conditions, controlling for trial. Our intention was to model the onset of MDD, which was considered a yes-or-no event. Thus, MDD incidence at one time-point was considered incidence at all subsequent time-points but that does not assume the disorder continued (we did not model the duration of MDD episodes primarily because the follow-up period was too short in 2 of the 4 trials). Each pairwise comparison included all trials with available information. Missing data were taken into account using maximum likelihood estimation (FIML). We tested moderation by sex and age by adding Condition X Sex/Age interaction terms in models. To examine heterogeneity across studies, we examined interactions between intervention effects and trial in fixed effects models (Thomas et al., 2014), which is the most feasible and informative option given the small number of trials.
In merging the data sets, we discovered that six participants had been enrolled who inadvertently met criteria for a current diagnosis of MDD (n = 5) or had incomplete diagnostic information (n = 1) at baseline; these participants were removed from the sample. Table 1 includes descriptive information on individual and combined samples. The pairwise comparison, analyses were balanced in terms of sex, race, parent education.
Table 1. Characteristics of the original trials and current sample.
| Variable | Brochure Control | CB Bibliotherapy | CB Group | Total Sample |
|---|---|---|---|---|
| Original RCT samples | ||||
| Trial 1: High School Efficacy | 83 | 80 | 88 | 251 |
| Trial 2: High School Effectiveness | 124 | 128 | 126 | 378 |
| Trial 3: College Effectiveness Pilot | 31 | 21 | 27 | 79 |
| Trial 4: College Pilot with Enhanced CB | 30 | 0 | 28 | 58 |
| Current Sample (Combined) | ||||
| N | 268 | 229 | 269 | 766 |
| % Females | 60 | 59 | 60 | 60 |
| Age, in years (M, SD) | 16.6 (2.6) | 15.8 (1.5) | 16.6 (2.4) | 16.4 (2.3) |
| % White | 64 | 70 | 60 | 64 |
To supplement our primary analyses examining cumulative MDD onset, we compared the interventions on time to MDD onset using survival analysis. We used right censoring when participants had not developed MDD by the end of their respective trial (i.e., 2-years in Trials 1 and 2, 12 months in Trial 3, 3 months in Trial 4) or when participants missed their first follow-up assessment, as survival models were developed to handle right-censored data. We used Cox regression to obtain a statistical comparison of time to MDD onset in conditions. We tested a basic proportional hazards model, as well as non-proportional hazards models in which the effect of CB group prevention interacted with time (linear, quadratic, cubic or log-linear patterns).
Rates of missing data were 5% at posttest (all trials), 12% at 3-month follow-up (all trials), 13% at 6-month follow-up (all trials except Trial 4), 18% at 12-month follow-up (all trials except Trial 4), and 25% at 24-month follow-up (Trials 1 and 2 only). Analyses showed no difference in attrition between conditions. Regarding receipt of the Blues Program intervention, average session attendance across the 4 trials was M = 4.5 (SD = 1.5) of 6 sessions.
Results
Table 2 presents the cumulative MDD incidence rates for the three intervention conditions and the odds of MDD incidence for each pairwise contrast at each of the available follow-ups, adjusted for trial. The table also shows the number needed to treat (NNT) for each comparison. NNT reflects the average number of adolescents who would need to receive an intervention to prevent one MDD incidence compared to the respective control group.
Table 2. Cumulative MDD incidence rates for conditions and the odds of MDD incidence for pairwise contrasts at assessed follow-up points.
| Cumulative MDD incidence (%) | Odds of MDD Incidence; OR (95% CI); NNT | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| CB group | Bibliotherapy | Control | Control vs. CB group | Control vs. Bibliotherapy | Bibliotherapy vs. CB group | |
|
|
||||||
| Post | 0.8 | 2.8 | 5.5 | 7.3 (1.7-32.3), p=.009, NNT=21 | 1.9 (0.7-5.0), p=.23, NNT=48 | 3.2 (0.7-15.4) p=.14, NNT=53 |
| 3 mo | 1.7 | 4.0 | 8.5 | 5.4 (1.8 - 15.9), p=.002, NNT=15 | 2.0 (0.9-4.9), p=.11, NNT=26 | 2.2 (0.7-7.4), p=.20, NNT=48 |
| 6 mo | 3.3 | 5.5 | 9.8 | 3.2 (1.3-7.7), p=.01, NNT=19 | 1.9 (0.9-4.0), p=.11, NNT=23 | 1.7 (0.7-4.5), p=.27, NNT=46 |
| 12 mo | 8.9 | 13.2 | 14.3 | 1.7 (0.9-3.3), p=.12, NNT=19 | 1.1 (0.6-2.0), p=.75, NNT=90 | 1.5 (0.8 - 3.0), p=.22, NNT=23 |
| 24 mo | 14.3 | 24.0 | 21.7 | 1.7 (0.9-3.0), p=.09, NNT=14 | 0.9 (0.6-1.6), p=.82, NNT=43 | 1.8 (1.02-3.3), p=.04, NNT=10 |
Notes: mo = months. The rates (%) presented for the CB group and the Control condition in the table includes all available trials. For comparisons involving Bibliotherapy, rates differ slightly at posttest and 3-month follow-up because Trial 4. Estimates for CB group include all trials at post and 3 months, all trials except Trial 4 at 6 months, and only Trials 1 and 2 at 12 and 24 months. Estimates for bibliotherapy include all trials except Trial 4 at post, 3 months, 6 months, and only Trials 1 and 2 at 12 and 24 months. Results are adjusted for trial.
The effects of CB group relative to Brochure control were strongest at posttest, with odds of MDD incidence more than seven times greater in Brochure controls than CB group participants (Table 2). This corresponds to an NNT = 21, suggesting that one MDD episode is prevented for every 21 adolescents who receive the CB group immediately after the program versus receiving an educational brochure. This effect remained significant at 3- and 6-month follow-up, with a three times greater odds of MDD incidence of Brochure controls compared to CB group participants. Differences at 12- and 24-months were not significant but were in the hypothesized direction. To investigate heterogeneity, we examined interactions between condition by trial in fixed effects models wherever possible (if no episodes of MDD occurred in one or more of the examined conditions by a certain time-point, the interaction could not be computed). None of the interactions between trial and the contrast of CB group relative to Brochure control were significant.
We also explored whether sex and age moderated effects by adding Condition X Moderator interaction terms into the models. These analyses were exploratory due to the low rates of MDD incidence early in follow-up. The interaction with sex at posttest could not be computed because there was no MDD incidence among male participants in the CB group condition (versus 4.0% for Brochure controls; comparable rates of MDD incidence for female participants were 1.3% vs. 6.4%, respectively). Interactions by sex at later time-points were nonsignificant. The interaction with age was significant at posttest (p = .038), with greater effects for CB group relative to Brochure control in adolescents 15 years of age or older (0.5% vs. 5.6%) but no difference in adolescents younger than 15 (2.0% vs. 5.3%). There were no significant interactions by age at later time-points.
In the contrasts comparing main effects for CB bibliotherapy to Brochure control, rates of MDD incidence at all time-points did not significantly differ. Additionally, interactions by sex and by age for the comparison of CB Bibliotherapy versus Brochure control at all time-points were nonsignificant. Regarding heterogeneity, interactions between trial and the contrast of CB Bibliotherapy and Brochure control were significant between Trials 1 and 2 at 12-month (p = .009; OR = 0.2, p < .05 vs. OR = 1.7, ns) and 24-month follow-up (p = .02; OR = 0.3, p < .05 vs. OR = 1.6, ns). Thus, there was no evidence of heterogeneity prior to 1-year but variance across trials for longer-term effects.
In the contrasts comparing main effects for the two active CB interventions, cumulative MDD incidence effects of CB group relative to CB Bibliotherapy were not significant except at the final follow-up, where the odds of MDD among CB Bibliotherapy participants were almost twice that of CB group participants, with an NNT of 10. Regarding sex and age moderation effects, the interaction by sex at posttest could not be computed given no MDD incidence in males (as in the comparison between CB group and Brochure control). Sex did not moderate effects at each of the subsequent assessments. As in the heterogeneity analyses for bibliotherapy versus control, no significant interactions between trial and the contrast of CB group and CB bibliotherapy were found at post, 3-month, and 6-months but significant differences between Trials 1 and 2 were present at 12-month (p = .03; OR = 0.3, p < .05 vs. OR = 2.3, ns) and 24-month (p = .007; OR = 0.3, p < .05 vs. OR = 2.7, ns) follow-ups.
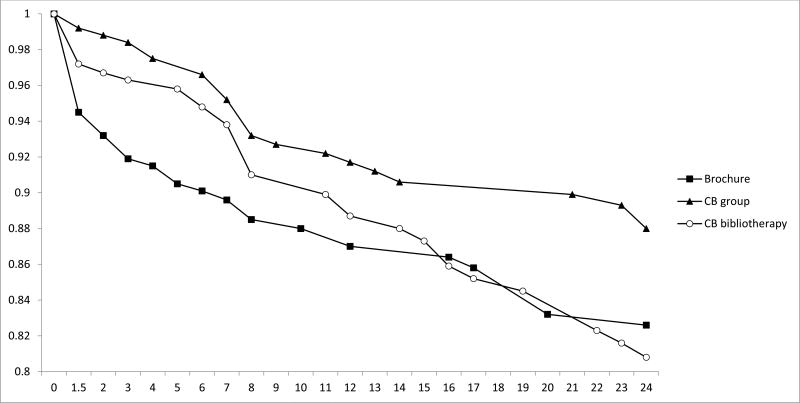
We also conducted secondary analyses comparing conditions on the time to MDD onset. Figure 1 shows the survival rates over a two-year period for the three conditions (MDD onset percentages differ slightly from Table 2 due to differences in handling missing data). An overall comparison between the three curves approached but did not reach significance (Breslow generalized Wilcoxon χ2 = 5.268, df = 2, p = .07) and one of the three pairwise comparisons was significant; CB group vs. Brochure control (Breslow χ2 = 5.163, df = 1, p = .02). We computed hazard ratios (HR) comparing time to MDD incidence rates in CB group prevention relative to the two alternate conditions at the five examined time-points, adjusting for trial. The effects of CB Group relative to Brochure were significant at posttest (HR = 10.0, 95% CI = 2.6 – 38.9, p < .001) and remained significant up to 3-month follow-up (HR = 2.8 [1.2-7.0], p < .05]; hazard rate effects were nonsignificant at subsequent time-points. Effects of CB Group relative to CB bibliotherapy were significant at posttest only (HR = 4.7 [1.1-20.4], p < .05]. Thus, results suggest that the gains produced by CB group are mostly derived from delaying the onset of MDD during receipt of the intervention and, relative to brochure controls, for the first three months post-intervention.
Figure 1. Survival curves illustrating time to MDD onset in the three intervention conditions.
Note: Cumulative survival (i.e., remaining MDD-free) shown on X-axis; months shown on the Y-axis. Cox regression models found that the effect of CB group interacted statistically with time following a cubic trend (i.e., effects of CB group relative to the two alternate conditions tended to be stronger initially, then weakened in the middle of the follow-up period before increasing near the final phase of follow-up).
Discussion
The goal of this report was to merge MDD incidence data across four RCTs evaluating a brief group-based CB indicated depression prevention program for adolescents to provide a more sensitive and reliable description of the preventive effect of this approach up to 2-years post-intervention, using IPD meta-analysis. Three of the trials also included CB bibliotherapy, which provided another CB-based active intervention comparison condition. CB group resulted in significantly lower MDD incidence rates relative to Brochure control that persisted to 6-month follow-up; a similar pattern was seen in the survival analyses examining time to MDD onset, suggesting that the CB group had its strongest effect in delaying the time to MDD in the early assessments. The incidence data effects of CB group versus CB bibliotherapy differed across trials at the 1- and 2-year follow-up points. In one study (Trial 2), CB group significantly reduced the longterm MDD incidence compared to CB bibliotherapy, but this effect was nonsignificant in Trial 1. Regarding time to MDD onset in the survival analyses, the CB group was superior to the CB bibliotherapy condition only immediately post-intervention. Although bibliotherapy is easier and less expensive to implement than CB group, we found no consistent evidence supporting its use in this merged data analysis.
It might be helpful to translate the CB group results into an actual school situation. The Blues Program is an indicated prevention program targeting adolescents with subthreshold depressive symptoms. Two of the 4 RCTs used a screening threshold of CES-D greater than or equal to 20, which applies to approximately one-third of the typical high school population (Roberts, Lewinsohn, & Seeley, 1991). If all students in a high school of 1000 were screened and 80% of the eligible adolescents (i.e., elevated CES-D score but not currently in an MDD episode) agreed to participate, approximately 250 adolescents could receive the prevention intervention. Providing the CB group in that hypothetical scenario would result in an MDD incidence of 8 MDD cases 6 months later, versus 25 new MDD cases in a comparison school that provided educational brochure (of course there would also be some MDD onset for the remaining 750 students at each school). This translates into a 68% absolute reduction in MDD onset across that period that roughly reflects one academic year.
For the four contrasts in which the odds of MDD incidence significantly differed, the number needed to treat (NNT) ranged from 10 to 21, suggesting that for every 10 to 21 adolescents who received the CB group rather than either the educational brochure or CB bibliotherapy, one less adolescent would develop MDD over the respective time period. The NNT statistic examines the effect of a binary rather than continuous outcome (i.e., MDD onset versus changes in depressive symptoms) and depends on the comparison condition, the avoided negative outcome, and the timeframe; an NNT of 5 or even 10 for a treatment intervention is often considered acceptable but NNT values for prevention are less established and sometimes much larger (e.g., Kraemer & Kupfer, 2006). In the first standard meta-analysis to synthesize results regarding the efficacy of preventive interventions across the lifespan in reducing the incidence of depressive disorders, Cuijpers, van Straten, Smit, Mihalopoulos, and Beekman (2008) found a 22% reduction of depressive disorders (which included MDD, dysthymia, postpartum depression, and depressive disorder-not otherwise specified) incidence compared with control groups, which corresponded to an NNT of 22. In an update of this body of research, Van Zoonen and colleagues (2014) conducted a standard meta-analysis of 32 RCTs examining the effects of preventive interventions in participants (from early adolescents to old age) with no diagnosed depressive disorders at baseline on the incidence of diagnosed depressive disorders at follow-up. The relative risk of developing a depressive disorder was an incidence rate ratio = 0.79 (95% confidence interval: 0.69–0.91), indicating a 21% decrease in incidence in prevention groups compared control groups. The NNT to prevent one new case of depressive disorder was 20 for the total sample, with subgroup analyses reporting NNTs of 22 for studies with adolescent samples. This larger analysis provides evidence that is consistent with the present report, increasing confidence in the findings supporting a brief CB group as an indicated depression prevention intervention.
As noted, NNT values depend on incidence, which is low for MDD onset, especially early in a post-intervention follow-up period. That is why odds ratios in Table 2 need to be fairly high early in follow-up to be significant. Looking at Table 2, although there is not a statistically significant difference between CB group and Brochure control at two-years follow-up, the pattern of results and NNT = 14 with a higher MDD incidence rate suggest that a clinically meaningful longer-term reduction in MDD is plausible.
One unique aspect of this report is its reliance on MDD incidence data. Most depression prevention trials have focused on depressive symptoms, which is easier and cheaper to collect and, as a continuous measure, have greater power to detect differences. One confusion with symptom-level data is that there are often significant acute phase effects immediately post-intervention, which have been more appropriately conceptualized as “treatment” effects rather than prevention per se (Gillham, Shatté, & Freres, 2000). These immediate treatment effects often quickly reverse with the intervention condition shower greater initial reductions in symptom levels but then reductions in the control group “catching up” with time. This reversal in the direction of effects does not occur in the prevention of future MDD incidence even when the odds ratios become nonsignificant.
It is noteworthy that CB Bibliotherapy did not significantly lower MDD onset versus educational brochure in the analyses of the combined data, as bibliotherapy had significantly reduced MDD onset in Trial 1 out to 2-year follow-up. This likely explains the heterogeneity in results regarding bibliotherapy in this combined analyses. It is possible that the efficacy trial had a stronger placebo effect because the books were distributed by the research team or the research team was able to achieve stronger engagement and use of the self-help book. In the present report, CB Bibliotherapy appeared, relative to brochure control, to be somewhat effective for the first 6-months post-intervention and given its ease of dissemination, we believe it warrants additional study. The present results provide no evidence suggesting that CB bibliotherapy is an effective stand-alone prevention intervention for at-risk adolescents in general but it could be a successful and inexpensive intervention for a subset of at-risk youth or as an augmentation to CB group.
Study limitations should be noted. First, our analyses focus exclusively on MDD incidence and future research should examine changes in depressive symptom levels (including levels indicating subthreshold disorders), functional status, comorbid psychiatric disorders (especially anxiety), and differences in MDD duration and severity as a result of prevention programs. Second, the Blues Program was examined as an indicated prevention program and results may not function as a selective prevention program, in which group members are selected on the basis of risk factors, such as parental depression. Third, the number of conditions and follow-up duration varied across trials.
In sum, a brief CB-based group depression prevention intervention for at-risk adolescent appears to be achieving clinically meaningful effects compared to both an active, credible control intervention and to a minimal control. However, the magnitude and durability of outcomes can certainly be improved. We conclude with two research directions we believe will most strongly improve the MDD prevention effects of this approach. First, improved screening for recruiting the most appropriate students should produce better effects. This includes identifying and not including adolescents with elevated depressive symptoms who are “spontaneous remitters” perhaps by using a serial screening approach. Also, identifying youth who have consistently elevated depressive symptoms but are inclined to not benefit from the intervention for other reasons (e.g., those with high baseline levels of substance use or negative life events; Gau, Stice, Rohde, & Seeley, 2012) would focus this prevention program more directly on those most likely to benefit. Second, CB group effects relative to control were nonsignificant at the 1-year follow-up, suggesting it would be useful to determine how to produce more persistent effects. Possible solutions may include the use of booster sessions (e.g., Beardslee et al., 2013), periodic re-screening of participants for a return of depressive symptoms, tiered interventions (e.g., Fazel, Hoagwood, Stephan, & Ford, 2014), or even perhaps bibliotherapy for a subset of young people. An effective prevention program for this common and debilitating condition among adolescents is currently available but needs to be both enhanced and broadly implemented.
Highlights.
-
-
Merged MDD incidence data across 4 trials evaluating indicated CB prevention group
-
-
Participants were 766 high school or college students with elevated depressive symptoms
-
-
Compared to brochure, CB group had lower MDD incidence rates out to 6-mo follow-up
-
-
For significant contrasts, the number needed to treat (NNT) ranged from 10 to 21
-
-
We found no evidence supporting use of CB bibliotherapy in this merged data analysis
Footnotes
This work was partially supported by NIMH grants MH067183 and MH080852. The authors declare no conflicts of interest and have no additional financial disclosures related to this publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Paul Rohde, Oregon Research Institute, Eugene, USA.
Frédéric N. Brière, Université de Montréal, Québec, Canada
Eric Stice, Oregon Research Institute, Eugene, USA.
References
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey–adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54:37–44. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Brent DA, Weersing VR, Clarke GN, Porta G, Hollon SD, Gladstone TR, et al. Prevention of depression in at-risk adolescents: longer-term effects. JAMA Psychiatry. 2013;70:1161–1170. doi: 10.1001/jamapsychiatry.2013.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns DD. Feeling Good: The New Mood Therapy. New York: William Morrow & Company; 1980. [Google Scholar]
- Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman ATF. Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. American Journal of Psychiatry. 2008;165:1272–1280. doi: 10.1176/appi.ajp.2008.07091422. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Druss BG. Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:160–170. doi: 10.1016/j.jaac.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools in high-income countries. The Lancet Psychiatry. 2014;1:377–387. doi: 10.1016/S2215-0366(14)70312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gau JM, Stice E, Rohde P, Seeley JR. Negative life events and substance use moderate cognitive behavioral adolescent depression prevention intervention. Cognitive Behaviour Therapy. 2012;41:241–250. doi: 10.1080/16506073.2011.649781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Shatté AJ, Freres DR. Preventing depression: A review of cognitive–behavioral and family interventions. Applied and Preventive Psychology. 2000;9:63–88. [Google Scholar]
- Gregory RJ, Schwer-Canning S, Lee TW, Wise JC. Cognitive bibliotherapy for depression: A meta-analysis. Professional Psychology: Research and Practice. 2004;35:275–280. [Google Scholar]
- Hetrick SE, Cox GR, Witt KG, Bir JJ, Merry SN. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database of Systematic Reviews. 2016;(8) doi: 10.1002/14651858.CD003380.pub4. Art. No.: CD003380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry. 2006;59:990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- Malouff J, Rooke S. Empirically supported self-help books. Behavior Therapist. 2007;30:129–131. [Google Scholar]
- Puig-Antich J, Chambers WJ. Schedule for Affective Disorders and Schizophrenia for School-Age Children (6-18 years) Pittsburgh: Western Psychiatric Institute; 1983. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science. 2013;1:41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Cognitive-behavioral group depression prevention compared to bibliotherapy and brochure control: Nonsignificant effects in pilot effectiveness trial with college students. Behaviour Research and Therapy. 2014;55:48–53. doi: 10.1016/j.brat.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Effectiveness trial of an indicated cognitive-behavioral group adolescent depression prevention program versus bibliotherapy and brochure control at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2015;83:736–747. doi: 10.1037/ccp0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Cognitive-behavioral group depression prevention compared to bibliotherapy and brochure control: Nonsignificant effects in pilot effectiveness trial with college students. Behaviour Research and Therapy. 2014;55:48–53. doi: 10.1016/j.brat.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Pilot trial of a dissonance-based cognitive-behavioral group depression prevention with college students. Behaviour Research and Therapy. 2016;82:21–27. doi: 10.1016/j.brat.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behaviour Research and Therapy. 2007;45:863–876. doi: 10.1016/j.brat.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010;78:856–867. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. Clinician-led, peer-led, and Internet-delivered dissonance-based eating disorder prevention programs: Acute effectiveness of these delivery modalities. Journal of Consulting and Clinical Psychology. doi: 10.1037/ccp0000211. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D, Radji S, Benedetti A. Systematic review of methods for individual patient data meta-analysis with binary outcomes. BMC: Medical Research Methodology. 2014;14:79. doi: 10.1186/1471-2288-14-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF, Beekman ATF, Cuijpers P. Preventing the onset of major depressive disorder: A meta-analytic review of psychological interventions. International Journal of Epidemiology. 2014;43:318–329. doi: 10.1093/ije/dyt175. [DOI] [PMC free article] [PubMed] [Google Scholar]