Abstract
Importance
Documenting patients’ advance care planning wishes is essential to providing value-aligned care, as is having this documentation readily accessible. Little is known about advance care planning documentation practices in the electronic health record.
Objective
Describe advance care planning documentation practices and the accessibility of documented discussions in the electronic health record.
Design
Cross-sectional study between 2013-2015.
Setting
Primary care clinics at the San Francisco Veterans Affairs Medical Center.
Participants
Veterans ≥60 years of age with ≥2 chronic/serious health conditions, ≥2 primary care visits, and ≥2 additional clinic/hospital/emergency room visits in the prior year who were participating in an advance care planning trial.
Exposure
Documentation of advance care planning in the electronic health record.
Main Measures
Advance care planning documentation, including all prior legal forms/orders and documented discussions within the prior five years. For discussions, the author’s discipline and documentation location in the electronic health record were determined. Discussions were defined as “accessible” if documented in a designated electronic posting location or “not easily accessible” if recorded as free-text in progress notes. Percentages and means were used to describe these measures.
Key Results
The mean age of 414 participants was 71 years (SD ±8), 9% were women, 43% were non-white, and 51% had documented advance care planning including 149 (36%) with forms/orders and 138 (33%) with discussions. Seventy-four participants (50%) with forms/orders did not have accompanying documented discussions. Most (55%) discussions were not easily accessible. Twenty-seven participants had a subsequent discussion documenting changes in treatment preferences from a prior form/order; however, 70% of these discussions were not easily accessible.
Conclusions and Relevance
Half of chronically ill, older participants had documented advance care planning wishes, including one third with documented discussions. However, half of the patients with completed legal forms/orders had no accompanying explanatory discussions. The majority of documented discussions were not easily accessible in the electronic health record, including 70% of those documenting a change in treatment preferences. Ensuring that patients’ preferences are documented and easily accessible is an important patient safety and quality improvement target to ensure patients’ wishes are honored.
Introduction
Advance care planning (ACP) is a process that supports adults in understanding and sharing their personal values, life goals, and preferences regarding future care.1 Although the prevalence of ACP documentation is increasing2 and may continue to increase with both federal and local reimbursement programs for ACP,3 the rates of ACP documentation are still low,4 especially among older and disenfranchised populations. A lack of documented ACP can lead to medical interventions misaligned with patients’ wishes5 as well as worse quality of life and stress for patients and surrogate decision-makers.6–11 Furthermore, ACP is a dynamic process which should be revisited as patients’ wishes and clinical context changes. Having up-to-date ACP information at the point of care is essential to providing value aligned care, however, little is known about ACP documentation practices.
The Veterans Affairs (VA) healthcare system, which treats over 10 million Veterans over the age of 65 years,12 is a leader in ACP quality improvement.13 Prior studies at the VA have sought to improve patient education and preparation for informed decision-making as well as increase rates of advance directive completion.14–17 The VA has also created ACP note templates and a centralized posting section for ACP discussion documentation in the electronic health record (EHR) to better capture patient preferences.
While prior studies, and a recent Institute of Medicine report, have stressed the need for standardized and up-to-date documentation of ACP in the medical record,18–23 it is unknown how well clinicians are utilizing EHR documentation tools, which disciplines are documenting patients’ preferences, and whether this information is easily accessible in the medical record. Better understanding of ACP documentation practices will lead to quality improvement opportunities to ensure patient safety and patients’ wishes are honored. This study aimed to quantify the rates and timing of ACP documentation, which disciplines were documenting ACP discussions, and whether ACP discussion information was placed in an easily accessible EHR location that could be retrieved at the point of care. Based on our clinical experience and prior research,18 we hypothesized that the majority of documented discussions would not be easily accessible in the EHR.
Methods
This is a cross-sectional study of primary care patients at the San Francisco Veterans Affairs Medical Center (SFVAMC). Baseline data were obtained from records of patients enrolled in a randomized controlled trial from 2013-2015 comparing the efficacy of a patient-centered ACP website (www.prepareforyourcare.org) plus an easy-to-read advance directive versus an advance directive alone on ACP documentation. The methods and results of this trial have been published.24,25
Patient Population
Eligibility was defined by chart review, physician assessment, and study staff assessment. Patients at the SFVAMC were eligible if they were at least 60 years of age, fluent in English, had at least two serious/chronic health conditions (defined by ICD-9 codes matching conditions listed in validated measures of comorbidity),26,27 had been seen at least twice in the prior year by a primary care provider in the General Medicine, Geriatrics, or Women’s Clinics, and had two additional clinic/hospital/emergency visits in the past year. Patients with evidence of dementia, blindness, cognitive impairment, delirium, psychosis, or active substance abuse by chart review or screening were ineligible. We obtained permission from primary care providers to approach their patients and then recruited participants by letters, flyers, phone calls, and in-clinic recruitment. Participants provided informed written consent. The study was approved by the University of California, San Francisco (UCSF) and the SFVAMC institutional review boards.
Measures
Measures included the frequency of ACP documentation, defined as legal forms/orders and documented ACP discussions (Figure 1). Forms/orders included any prior scanned advance directives or living wills, durable power of attorney for healthcare (DPOAHC) forms, and orders including outpatient Do Not Resuscitate/Do Not Intubate (DNR/DNI) orders or Physician Orders for Life Sustaining Treatment (POLST). For ACP discussions, chart notes were reviewed within the prior five years. Two independent coders reviewed all medical records. Disagreements were resolved by consensus. To qualify as a documented ACP discussion, written evidence of participant engagement and input in a conversation was required; documentation that participants were only provided educational materials was not counted.
Figure 1. All study measures assessed by chart review.
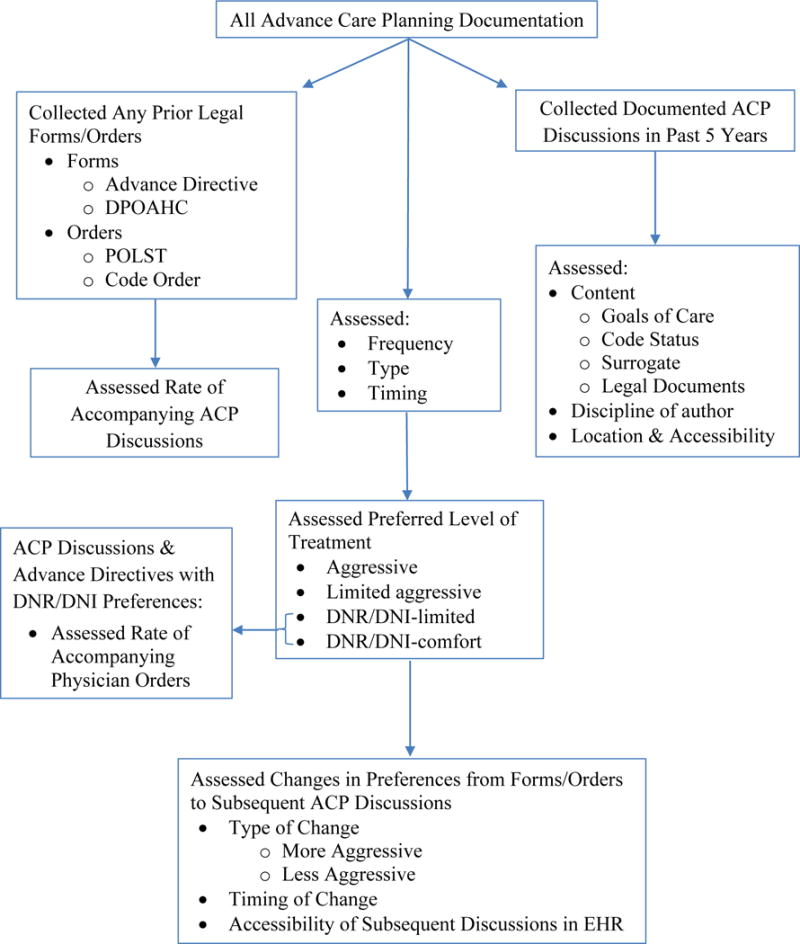
ACP indicates Advance Care Planning; DNR/DNI, Do Not Resuscitate/Do Not Intubate; DPOAHC, Durable Power of Attorney for Health Care; EHR, Electronic Health Record; POLST, Physician Orders for Life Sustaining Treatment.
For legal forms/orders, we assessed the type (e.g., advance directive, DPOAHC, POLST, and code order), overall frequency, and mean elapsed time between form/order completion and study enrollment. For participants with multiple forms/orders, all types were described and the most recent form/order was used to calculate overall frequency and timing. Also, because patients with completed legal forms/orders should ideally have accompanying ACP discussions to explain their decision-making process, we determined how many patients with a legal form/order had a documented ACP discussion.
For ACP discussions, we assessed the frequency, type, and timing of documented information, the author of the note, and location and accessibility in the EHR. Rates of discussion completion, as a percentage of all study participants, as well as mean elapsed time between discussion completion and study enrollment, were computed. For participants with multiple documented discussions, the most recent discussion was used. The type of documented discussions was categorized as follows: “goals of care” (i.e., a discussion describing participants’ wishes, reasoning, and thought processes), “code status only” (i.e., DNR/DNI or Full Code or Comfort Care noted in discussion documentation without documentation of participants’ reasoning or thought processes), “surrogate decision maker,” and discussions about “legal documents.” Discussions often included multiple categories. Data are presented for each content category as percentages of the total number of participants with discussions. Authorship was categorized by discipline: primary care provider, inpatient/outpatient social worker, inpatient medical team, or outpatient psychologist. The location of each ACP discussion was determined by the note type. The SFVAMC EHR uses note templates for ACP which are captured in a central posting area on the face page of the patients’ medical record. The accessibility of each ACP discussion was determined by whether it could be located in the centralized posting area. If it could, the discussion was deemed “easily accessible.” Documented discussions which could only be found by searching free-text from chart notes, including hospital admission, discharge, emergency department, outpatient primary care, specialty clinic, social work, and surgical/anesthesia pre-operative notes, were deemed “not easily accessible.”
For both ACP forms/orders and ACP discussions, we assessed preferred level of treatment using categories based on POLST and other scope-of-treatment documents.22 Preferences were categorized as “Aggressive” care (i.e., documented Full Code or affirmative to intubation, CPR, and all other life sustaining treatments without evidence of wanting to limit treatments in any situation), “Limited Aggressive” care (i.e., documented Full Code, affirmative to CPR and intubation but not indefinitely and not in every situation), “DNR/DNI-Limited” (i.e., negative response to intubation or CPR, but affirmative to surgery, antibiotics, or feeding tubes), or “DNR/DNI-Comfort” (i.e., negative responses to CPR and intubation with specific documentation of the term “comfort measures only”). The category of “No Wishes Documented” was used if preferences could not be categorized by these criteria. Rates of each desired level of treatment are presented as percentages of all participants with completed forms or discussions, respectively.
Once treatment preferences were categorized, we determined whether physician orders accompanied DNR/DNI documentation in advance directives or discussions. An accompanying DNR/DNI physician order or POLST is considered appropriate so that patients’ wishes can be honored across health settings.28 Thus, we assessed rates of POLST or outpatient DNR/DNI orders for participants whose advance directives and/or ACP discussions were categorized as DNR/DNI.
We also assessed changes in treatment preferences between forms/orders and subsequent ACP discussions with discernible levels of desired treatment (e.g., Aggressive, DNR/DNI-Comfort, etc.). Levels of desired treatment were categorized as “changed” if they differed between forms/orders and subsequent ACP discussions. For these participants, we categorized the changes as “more aggressive” or “less aggressive” based on how their preferences changed in more recent documented ACP discussions relative to prior forms. Determining the accessibility of ACP discussions that document changes in treatment preferences is important so that patients’ most updated wishes can be honored. Therefore, we assessed time between form completion and subsequent ACP discussions and the accessibility of the ACP discussion that documented the treatment change.
Statistical Analysis
To describe participant characteristics and our measures, we used percentages and means with standard deviations. Analyses were conducted using SAS statistical software (version 9.4; SAS Institute Inc.).
Results
Participants
The mean age of the 414 participants was 71 years (SD ±8) (Table 1). Participants were mostly men (91%), 43% were non-white by self-report, 18% had less than a high school education, 20% had limited health literacy, 29% self-rated their health as fair-to-poor on a 5-point Likert scale, and 92% reported having a potential surrogate decision maker. Of the 414 participants, 212 (51%) had some type of ACP documented in the EHR.
Table 1.
Demographic characteristics of study participants.
| Demographic Characteristics | |
|---|---|
| Age: N=414, mean (SD) | 71.1 (7.8) |
|
| |
| Sex: Women, N=414, No. (%) | 38 (9%) |
|
| |
| Race/Ethnicity: N=413, No. (%) | |
| White | 235 (57%) |
| African American | 88 (21%) |
| Latino/Hispanic | 33 (8%) |
| Native American | 5 (1%) |
| Asian/Pacific Islander | 26 (6%) |
| Multi-ethnic/Other | 26 (6%) |
|
| |
| Education ≤ high school: N=413, No. (%) | 74 (18%) |
|
| |
| Finances, not enough to make ends meet: N=412, No. (%) | 49 (12%) |
|
| |
| In a married/long term relationship: N=414, No. (%) | 187 (45%) |
|
| |
| Have a potential surrogate: N=414, No. (%) | 382 (92%) |
|
| |
| Self-Rated Health, fair-to-poor: N=412, No. (%) | 120 (29%) |
|
| |
| Limited Health Literacy, N=411, No. (%) | 83 (20%) |
ACP legal forms and Physician Orders
One hundred forty-nine participants (36%) had completed ACP legal forms at any time, including 130 advance directives/living wills and 103 DPOAHC forms. These forms were completed an average of 4.6 years (SD ±3.2) prior to study enrollment (Table 2). Three POLST forms were completed and two participants had outpatient DNR/DNI orders. Of 149 participants with ACP legal forms/orders, 75 (50%) had an accompanying documented ACP discussion.
Table 2.
ACP legal forms and physician orders.
| Type of ACP Forms/Orders | Completed Forms/Orders N=414, No. (%) | Time prior to study enrollment (mean years ± SD) |
|---|---|---|
| Advance Directive | 130 (31%) | 5.0 ± 3.3 |
| DPOAHC Form | 103 (25%) | 5.6 ± 3.7 |
| POLST | 3 (0.7%) | 1.9 ± 1.5 |
| DNR/DNI Order | 2 (0.5%) | 4.1 ± 0.7 |
| Any ACP Forms/Orders | 149 (36%) | 4.6 ± 3.2 |
ACP indicates Advance Care Planning; DNR/DNI, Do Not Resuscitate/Do Not Intubate; DPOAHC, Durable Power of Attorney for Health Care; POLST, Physician Orders for Life-Sustaining Treatment.
ACP discussions
In the five years prior to study enrollment, 138 (33%) study participants had documented ACP discussions. These discussions occurred 2.1 years (SD ±1.4) prior to study enrollment and focused on surrogate decision makers (n=115, 83% of participants with discussions), goals of care (n=45, 33%), legal documents (n=36, 26%), and code status (n=23, 17%).
Overall, discussions were documented predominantly by social workers (n=75, 54%) and outpatient primary care providers (n=49, 36%) (Table 3). Inpatient primary teams documented 12 discussions (9%), while one discussion each was documented by an outpatient palliative care provider, and an outpatient psychologist.
Table 3.
Location and authorship of documented ACP discussions in the EHRa
| Easily Accessible | N = 62 (45%) | |
|---|---|---|
| Author | Location in EHR | No. (%) |
|
|
||
| Inpatient Social Worker | ACP Postingb | 35 (25%) |
| Outpatient Social Worker | ACP Posting | 23 (17%) |
| Inpatient Medical Team | ACP Posting | 2 (1.4%) |
| Primary Care Provider | ACP Posting | 1 (0.7%) |
| Outpatient Palliative Care Provider | ACP Posting | 1 (0.7%) |
|
| ||
| Not Easily Accessible | N = 76 (55%) | |
| Author | Location in EHR | No. (%) |
|
|
||
| Primary Care Provider | Outpatient Progress Note | 48 (35%) |
| Inpatient Social Worker | Inpatient Social Work Note | 13 (9.4%) |
| Inpatient Medical Team | Admission Note | 5 (3.6%) |
| Outpatient Social Worker | Outpatient Social Work Note | 4 (2.9%) |
| Inpatient Medical Team | Discharge Summary | 2 (1.4%) |
| Inpatient Medical Team | Inpatient Progress Note | 1 (0.7%) |
| Inpatient Medical Team | Inpatient Progress Note Addendum | 1 (0.7%) |
| Inpatient Medical Team | Inpatient Pre-Operative Note | 1 (0.7%) |
| Outpatient Psychologist | Outpatient Progress Note | 1 (0.7%) |
|
| ||
| Time between ACP discussion documentation and study enrollment (mean years ± SD) | 2.1 ± 1.4 | |
n = 138 documented advance care planning discussions.
The ACP posting location is a centralized, easily accessible location on the face page of a participant’s electronic health record. ACP indicates Advance Care Planning; EHR, Electronic Health Record.
Of 138 ACP discussions, 62 (45%) were easily accessible and 76 (55%) were not easily accessible from the EHR. Of the easily accessible discussions, 58 (94%) were documented by social workers, two by inpatient primary teams, and one each by a primary care provider and an outpatient palliative care provider. Of the not easily accessible discussions, 48 (63%) were documented as free-text by primary care providers in progress notes and 17 (22%) were documented in social work notes. By provider type, 58 (77%) of 75 discussions documented by social workers were easily accessible, while one (2%) of 49 discussions documented by primary care providers was easily accessible.
Treatment Preferences and Physician Orders
Participants expressed preferences for desired level of treatment in 83% of completed ACP forms/orders and 39% of discussions (Table 4). In legal forms/orders, the most frequently desired level of treatment was DNR/DNI-Limited (56%). Among ACP discussions, the most frequently desired level of treatment was Limited Aggressive (46% of those with discernible wishes). Among the 88 participants with DNR/DNI wishes in advance directives, two (2%) had active DNR/DNI orders and two (2%) had completed POLST forms. Of the 15 participants with DNR/DNI wishes in discussions, no participants had active DNR/DNI orders and two (13%) had completed POLST forms.
Table 4.
Desired level of treatment documented in legal forms and ACP discussions.
| Level of Treatment Desired | ACP legal forms N = 149, No. (%) | ACP discussions N = 138, No. (%) |
|---|---|---|
| Aggressive | 9 (6%) | 14 (10%) |
| Limited Aggressive | 26 (17%) | 25 (18%) |
| DNR/DNI-Limited | 83 (56%) | 10 (7%) |
| DNR/DNI-Comfort | 5 (3%) | 5 (3%) |
| No Wishes Documented | 26 (17%) | 84 (61%) |
ACP indicates Advance Care Planning; DNR/DNI, Do Not Resuscitate/Do Not Intubate.
Changes in Preferences
During the 5-year retrospective review of the EHR, 34 participants had completed a legal form/order and then had a subsequent ACP discussion where levels of preferred treatment were documented. Discussions occurred an average of 3.9 years (SD ±3.4) after form/order completion. For 27 (79%) of these participants, discussions documented a change in participants’ treatment preferences: nine (33%) to more aggressive treatment and 18 (67%) to less aggressive treatment. For 19/27 (70%) participants with changed preferences, the documented ACP discussions were not easily accessible in the EHR: nine (100%) of those documenting more aggressive treatment preferences and 10 (56%) of those documenting less aggressive treatment preferences.
Discussion
To our knowledge, this is the first study to describe the comprehensive type, authorship, location, and accessibility of ACP documentation through detailed electronic chart review. The VA is an exceptional national model of ACP documentation in that it includes a centralized posting section in the EHR for ACP, is dedicated to ACP initiatives,13–17,25,29 and half of chronically ill, older Veterans in this study had documented ACP wishes, well above national norms.30 However, given that many non-VA health systems do not have similar established EHRs and dedicated ACP programs, these study findings point to a likely widely generalizable quality improvement gap for patient safety in ACP. For example, 50% of patients with a completed form or physician order in this study did not have an accompanying documented ACP discussion about that form/order in the EHR. In addition, the majority of ACP discussions were not easily accessible, though they were more up-to-date (i.e., on average two years versus five years prior) and often represented changes in wishes from prior forms/orders. A majority of ACP discussions, including those which were easily accessible, were also documented by social workers rather than primary care providers.
These results are similar to a Canadian study of hospitalized patients demonstrating that patients’ and families’ wishes were not being documented correctly in the medical record.22 Lack of accurate and accessible ACP documentation represents an important patient safety issue that could have devastating ramifications on patients’ care.23 Having up-to-date, easily accessible descriptions of patients’ wishes for medical care in an ACP discussion note in the EHR is essential to ensuring patients engage in fully informed shared decision-making about their preferences, interpreting the meaning behind legal forms/orders, conveying important information to other treating physicians about real-time and ongoing changes in patients’ preferences, and ensuring that patients’ wishes are honored. The insight provided by documented discussions also provides crucial context for future discussions with additional medical providers.
However, in this study, half of participants with completed ACP legal forms had no accompanying documented discussions. Ensuring all forms/orders are accompanied by a corresponding ACP note may be an important quality improvement metric in addition to advance directive or form/order completion. In addition, the majority of ACP discussions were not easily accessible and were documented as free-text in progress notes without any associated notification or flag in the central posting section of the EHR. This minimizes the likelihood that a future clinician would notice and be able to use this information in an actionable way at the bedside. Although many providers are having detailed ACP discussions with patients, the lack of standardized documentation practices limits the clinical utility of these discussions.
The lack of standardization was most concerning when documented preferences changed between legal forms/orders and subsequent discussions, especially as 70% of these changes in preferences were not easily accessible in the EHR. Future providers who do not notice or cannot find subsequent free-text discussions in the EHR are likely to default to more easily located forms/orders which may contain outdated patient preferences. These forms/orders were, on average, completed five years prior to study enrollment, and more frequent updates are needed as demonstrated by the high rate of changed preferences among those with subsequent discussions. Use of such out-of-date documentation may lead to care misaligned with patients’ preferences. When extrapolated on a population level, these misaligned documented wishes could affect many patients.
ACP discussions were most frequently documented by social workers followed by primary care providers. The involvement of social workers in this process is a strength of the integrated Patient Aligned Care Teams (PACT) in the VA system and likely positively impacts ACP documentation overall. However, in some cases, the additional involvement of the primary care provider to provide context regarding patients’ medical conditions and prognoses may also be important. Primary care providers documented only 2% of ACP discussions in an easily accessible location compared to 77% of social workers’ documentation. This discrepancy may reflect differences between training curricula and could likely be improved with educational interventions. The extremely low use of POLST and DNR/DNI orders for the subset of patients with preferences for DNR/DNI also reveals an opportunity for improvement of the ACP documentation process.
While prior research has focused on increasing rates of legal form completion31–33 or techniques to conduct effective ACP discussions,34–36 interventions focusing on appropriate documentation of ACP discussions are less prevalent.14 Such an intervention could have a large impact on clinical care and patient safety23 and may require minimal behavioral change from clinicians since our study demonstrated that many are already having and recording rich ACP discussions. In addition, changes to the EHR that would allow clinicians to easily flag goals of care conversations within other progress notes, to be placed in important central EHR posting areas, may negate the need for remembering specific note titles.
The strengths of this study include the comprehensive nature of chart review performed by two independent reviewers. Limitations include the predominantly older and male population of Veterans recruited from a single medical center who were participating in a study of ACP, which may restrict generalizability. However, the study population was diverse in other demographic characteristics. In this cross-sectional study, we were unable to assess changes in behavior over time, nor determine whether patients received care consistent with their most up-to-date preferences. However, our data provide an assessment of the current state of practice which can be used to inform future studies.
Conclusions
These results suggest potential areas for EHR redesign and quality improvement to ensure patient safety and patient-centered care in ACP. Quality improvement targets include clinician education concerning documentation of ACP discussions in an easily accessible location in the EHR, especially to help explain preferences for patients with completed ACP legal forms and changes to patients’ preferences over time. More frequent updating of patient’s wishes and completion of physician orders for patients with clear and stable DNR/DNI wishes may also be needed. Further study, including the design of the EHR, is needed to better understand how to improve ACP documentation practices and help ensure patients’ wishes are honored.
Key Points.
Question
What are the current advance care planning documentation practices at a VA Medical Center and how accessible are documented advance care planning discussions in the electronic health record?
Findings
In this cross-sectional study of 414 chronically ill Veterans, half had documented advance care planning wishes, including one third with documented discussions. Most (55%) discussions were not easily accessible in the medical record, including 70% of those documenting treatment wishes which had changed from prior legal forms/orders.
Meaning
Efforts to improve standardization and accessibility of advance care planning documentation are imperative to ensure patient safety and patients’ wishes are honored.
Acknowledgments
Drs. Walker and Sudore had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding/Support: The U.S. Department of Veterans Affairs
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study, data collection, management, analysis, and interpretation of data, or in preparation, review, or approval of the manuscript.
Footnotes
Author Contributions:
Study concept and design: Sudore, Barnes
Acquisition, analysis, or interpretation of data: All authors
Drafting of the manuscript: All authors
Critical revision of the manuscript for important intellectual content: All authors
Statistical analysis: Walker, Sudore
Obtained funding: Sudore
Administrative, technical, or material support: Sudore, Katen, McMahan
Study supervision: Sudore
Conflict of Interest Disclosures: None reported.
Neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere.
Additional Contributions: None
References
- 1.Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary delphi panel. J Pain Symptom Manage. 2017;53(5):821–832.e1. doi: 10.1016/j.jpainsymman.2016.12.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silveira MJ, Wiitala W, Piette J. Advance directive completion by elderly Americans: a decade of change. J Am Geriatr Soc. 2014;62(4):706–710. doi: 10.1111/jgs.12736. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Details for title: CMS-1654-F. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1654-F.html. Accessed February 9, 2017. [PubMed]
- 4.Harrison KL, Adrion ER, Ritchie CS, Sudore RL, Smith AK. Low completion and disparities in advance care planning activities among older medicare beneficiaries. JAMA Intern Med. 2016;176(12):1872–1875. doi: 10.1001/jamainternmed.2016.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477–489. doi: 10.1016/j.jamda.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried TR, O’Leary JR. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. J Gen Intern Med. 2008;23(10):1602–1607. doi: 10.1007/s11606-008-0748-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heyland DK, Cook DJ, Rocker GM, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29(1):75–82. doi: 10.1007/s00134-002-1569-y. [DOI] [PubMed] [Google Scholar]
- 10.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29(1):197–201. doi: 10.1097/00003246-200101000-00040. [DOI] [PubMed] [Google Scholar]
- 11.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Veterans Analysis and Statistics. Profile of Veterans. 2015 https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2015.pdf. Accessed December 15, 2016.
- 13.National Center for Ethics in Health Care. The Life-Sustaining Treatment Decisions Initiative. https://www.ethics.va.gov/LST.asp. Accessed June 2, 2017.
- 14.Lindner SA, Ben Davoren J, Vollmer A, Williams B, Seth Landefeld C. An electronic medical record intervention increased nursing home advance directive orders and documentation. J Am Geriatr Soc. 2007;55(7):1001–1006. doi: 10.1111/j.1532-5415.2007.01214.x. [DOI] [PubMed] [Google Scholar]
- 15.Sudore RL, Seth Landefeld C, Barnes DE, et al. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns. 2007;69(1-3):165–195. doi: 10.1016/j.pec.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Volicer L, Cantor MD, Derse AR, et al. Advance care planning by proxy for residents of long-term care facilities who lack decision-making capacity. J Am Geriatr Soc. 2002;50(4):761–767. doi: 10.1046/j.1532-5415.2002.50175.x. [DOI] [PubMed] [Google Scholar]
- 17.Pearlman RA, Starks H, Cain KC, Cole WG. Improvements in advance care planning in the Veterans Affairs System: results of a multifaceted intervention. Arch Intern Med. 2005;165(6):667–674. doi: 10.1001/archinte.165.6.667. [DOI] [PubMed] [Google Scholar]
- 18.Cox K, Moghaddam N, Almack K, Pollock K, Seymour J. Is it recorded in the notes? Documentation of end-of-life care and preferred place to die discussions in the final weeks of life. BMC Palliat Care. 2011;10:18. doi: 10.1186/1472-684X-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson CJ, Newman J, Tapper S, et al. Multiple locations of advance care planning documentation in an electronic health record: are they easy to find? J Palliat Med. 2013;16(9):1089–1094. doi: 10.1089/jpm.2012.0472. [DOI] [PubMed] [Google Scholar]
- 20.Turley M, Wang S, Meng D, Kanter M, Garrido T. Impact of a care directives activity tab in the electronic health record on documentation of advance care planning. Perm J. 2016;20(2):43–48. doi: 10.7812/TPP/15-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Academy of Sciences. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. http://www.nationalacademies.org/hmd/Reports/2014/Dying-In-America-Improving-Quality-and-Honoring-Individual-Preferences-Near-the-End-of-Life.aspx. Accessed June 2, 2017. [PubMed]
- 22.Heyland DK, Barwich D, Pichora D, et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. 2013;173(9):778–787. doi: 10.1001/jamainternmed.2013.180. [DOI] [PubMed] [Google Scholar]
- 23.Allison TA, Sudore RL. Disregard of patients’ preferences is a medical error: comment on “Failure to engage hospitalized elderly patients and their families in advance care planning”. JAMA Intern Med. 2013;173(9):787–787. doi: 10.1001/jamainternmed.2013.203. [DOI] [PubMed] [Google Scholar]
- 24.Sudore R, Le GM, McMahan R, Feuz M, Katen M, Barnes DE. The advance care planning PREPARE study among older Veterans with serious and chronic illness: study protocol for a randomized controlled trial. Trials. 2015;16:570. doi: 10.1186/s13063-015-1055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE website vs an easy-to-read advance directive on advance care planning documentation and engagement among Veterans: a randomized clinical trial [published online May 18, 2017] JAMA Intern Med. doi: 10.1001/jamainternmed.2017.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 27.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42(4):355–360. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 28.Bomba PA, Kemp M, Black JS. POLST: An improvement over traditional advance directives. Cleve Clin J Med. 2012;79(7):457–464. doi: 10.3949/ccjm.79a.11098. [DOI] [PubMed] [Google Scholar]
- 29.Lum HD, Jones J, Matlock DD, et al. Advance care planning meets group medical visits: the feasibility of promoting conversations. Ann Fam Med. 2016;14(2):125–132. doi: 10.1370/afm.1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yadav KN, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff (Millwood) 2017;36(7):1244–1251. doi: 10.1377/hlthaff.2017.0175. [DOI] [PubMed] [Google Scholar]
- 31.Jezewski MA, Meeker MA, Sessanna L, Finnell DS. The effectiveness of interventions to increase advance directive completion rates. J Aging Health. 2007;19(3):519–536. doi: 10.1177/0898264307300198. [DOI] [PubMed] [Google Scholar]
- 32.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277–283. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 33.Morrison RS, Chichin E, Carter J, Burack O, Lantz M, Meier DE. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc. 2005;53(2):290–294. doi: 10.1111/j.1532-5415.2005.53116.x. [DOI] [PubMed] [Google Scholar]
- 34.Quill TE. Initiating end-of-life discussions with seriously ill patients: addressing the elephant in the room. JAMA. 2000;284(19):2502–2507. doi: 10.1001/jama.284.19.2502. [DOI] [PubMed] [Google Scholar]
- 35.Jacobsen J, Robinson E, Jackson VA, Meigs JB, Billings JA. Development of a cognitive model for advance care planning discussions: results from a quality improvement initiative. J Palliat Med. 2011;14(3):331–336. doi: 10.1089/jpm.2010.0383. [DOI] [PubMed] [Google Scholar]
- 36.Modan G, Brill SB. Engaging death: narrative and constructed dialogue in advance care planning discussions. Commun Med. 2014;11(2):153–165. doi: 10.1558/cam.v11i2.18616. [DOI] [PubMed] [Google Scholar]


