Abstract
The use of hip arthroscopy to treat various forms of hip pathology continues to grow. As part of a standard evaluation for eligibility for hip arthroscopy, we routinely obtain standard radiographs to assess the hip joint. These include orthogonal projections of the acetabulum and proximal femur, which can be obtained with a standing false profile, supine anteroposterior pelvis, and a lateral view of the proximal femur (either Dunn 45° or 90°, frog-leg lateral, or cross-table lateral). A comprehensive analysis of the radiographs is of utmost importance in order to indicate a patient for hip arthroscopy, for preoperative planning, and to determine prognosis. The purpose of this Technical Note is to provide a comprehensive guide of how our group performs qualitative and quantitative analysis of hip radiographs in a potential candidate for hip arthroscopy.
Hip-related pathologies and pain should be evaluated with a thorough physical examination and a standard set of radiographs to identify anatomic abnormalities and potential sites of pain generators. With an increased understanding of hip pathologies, hip arthroscopic procedures have increased. A 25-fold increase in hip arthroscopic procedures was reported between 2006 and 2013.1
Radiographic evaluation of the hip requires several views for comprehensive characterization prior to hip arthroscopy. Routine hip radiographs must include orthogonal projections of the acetabulum and proximal femur, which can be accomplished with standing false profile, supine anteroposterior (AP) pelvis, and a lateral view of the proximal femur (either Dunn 45° or 90°, frog-leg lateral, or cross-table lateral). Assessment of the studies for quality and positioning of the patient is essential for radiographic assessment of the hip. Quality radiographs are paramount for obtaining accurate measurements necessary for the comprehensive and quantitative assessment of a potential hip arthroscopy patient and to allow comparison with validated measurements, which are important for appropriate surgical indications and predicting prognosis.
A reliable radiographic technique and accurate measurements are of utmost importance when objectively evaluating a patient, indicating a certain procedure, and predicting the prognosis of the joint-preserving arthroscopic surgery. The purpose of this Technical Note is to provide a comprehensive guide to how our group performs qualitative and quantitative analysis of hip radiographs and associated pathology in a potential candidate for hip arthroscopy.
Radiographic Assessment of Hip Osteoarthritis
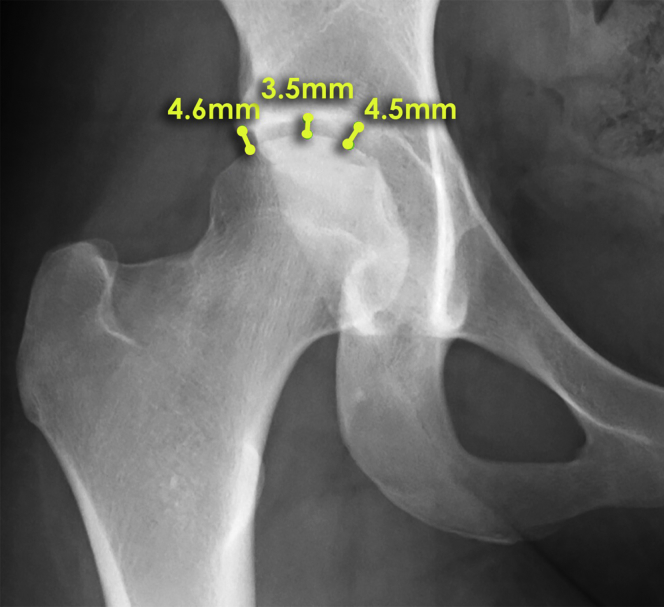
Severe hip osteoarthritis has been reported to negatively affect the outcome of hip arthroscopy and is readily assessed with plain radiographs.2, 3, 4 Tonnis and Heinecke described a classification graded 0 through 3 for least to most severe, respectively.5 The hip is assessed for features of arthritis that include joint space narrowing (Fig 1), subchondral cystic changes, and femoral head sphericity. Joint space narrowing <2 mm may preclude successful hip arthroscopy and should be considered for alternative treatment.4 Radiographs without evidence of osteoarthritis are classified as Tönnis grade 0, whereas Tönnis grade 1 represents mild osteoarthritis characterized by maintenance of femoral head sphericity, increased sclerosis, and slight narrowing of the hip joint space. Moderate and severe hip osteoarthritis are characterized by Tönnis grades 2 and 3, respectively. Tönnis grade 2 represents moderate hip osteoarthritis, which is characterized by moderate loss of head sphericity, moderate joint space narrowing, and small subchondral cysts. Tönnis grade 3 is characterized by severe osteoarthritis with severe femoral head deformity, obliteration of the hip joint space, and large subchondral cystic changes.5
Fig 1.
Hip joint space measurement in an anteroposterior hip radiograph. Patients with <2 mm of joint space remaining can be considered to have arthritis and are typically recommended for nonarthroscopic management. Joint space measurements should be performed at 3 locations in the hip joint. Medial point: measure joint space of acetabulum to femoral head at a 90° angle to the most medial aspect of the acetabular sourcil line. Central point: measure joint space of acetabulum to femoral head at a 90° angle to the center of the superior articular surface. Lateral point: measure joint space of the acetabulum to femoral head at a 90° angle to the most lateral weight-bearing aspect of the femoral head joint space narrowing <2 mm may preclude successful hip arthroscopy and should be considered for alternative treatment.
Several findings of hip osteoarthritis on an AP pelvis radiograph have been described by Howse and Stubbs, including the “saber tooth” sign, “seagull” sign, “hammock” sign, posterior superior femoral head-neck junction remodeling sign, and interior femoral neck remodeling sign.3 The saber tooth sign is when osteophytes form in the central, non-weight-bearing, portion of the acetabulum, which may sometimes result in lateralization of the femoral head. The seagull sign is degeneration and remodeling of the superolateral acetabulum, and the hammock sign is remodeling of the inferior acetabulum.3
Metrics to Quantify Femoral and Acetabular Morphology
A variety of measurements are used to assess radiographs of patients being evaluated prior to hip arthroscopy (Video 1). These radiographic metrics include the alpha angle, Tönnis angle, lateral center edge angle of Wiberg, and Sharp angle. Additionally, the radiographs should be evaluated for the presence of coxa profunda, coxa protrusion, coxa magna, coxa breva, femoroacetabular impingement (e.g. cam, pincer, or mixed), or acetabular retroversion (e.g. crossover sign, ischial spine sign, posterior wall sign). Each of the measurements and conditions are subsequently described in greater detail herein.3
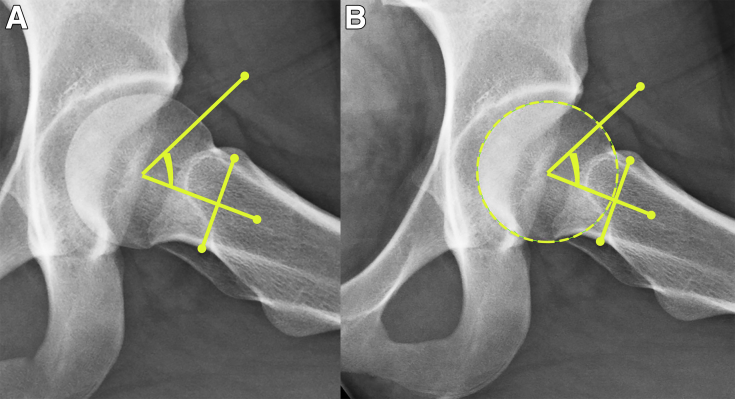
Alpha Angle (and Beta Angle)
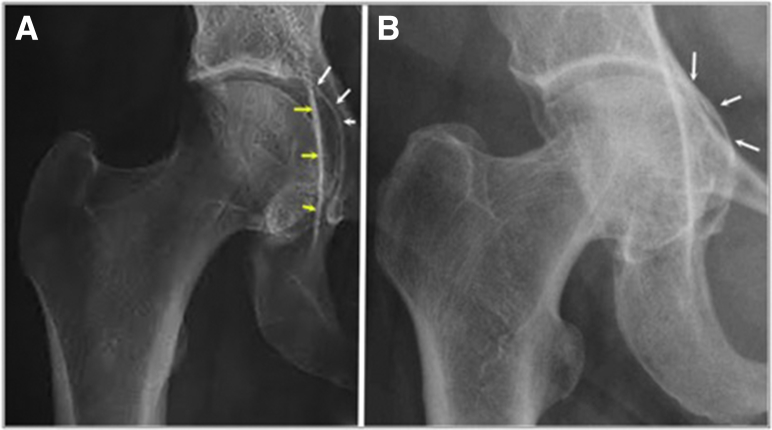
The Dunn view can be obtained at 45° or 90° and is used to evaluate the femoral head sphericity and contour of the femoral head neck junction. The alpha angle allows quantitative characterization of the degree of anterior deformity associated with cam-type femoroacetabular impingement. An alpha angle is obtained by drawing a line from the center of the narrowest point of the femoral neck to the center of the femoral head using a best-fit circle. The alpha angle is between the line down the axis of the femoral neck and a line drawn to the location where the femoral head becomes “out of round” (i.e. extends beyond the best-fit circle; Fig 2). This analogous measurement performed at the posterior hip at the location of the abnormal femoral head-neck junction is the beta angle.3
Fig 2.
(A and B) Radiographic imaging of a left hip demonstrating the alpha angle measurement. In order to accurately measure the alpha angle, a line should be drawn from the center of the narrowest point of the femoral neck to the center of the femoral head using a best-fit circle. The alpha angle is between the line down the axis of the femoral neck and a line drawn to the location where the femoral head loses its sphericity. Alpha angles >55° are indicative of cam femoroacetabular impingement deformity, and normal alpha angles are typically considered to be <55°.
Alpha angles greater than 55° are indicative of cam femoroacetabular impingement deformity, and normal alpha angles are typically considered to be <55°.6 Articular surface damage should be suspected when alpha angles are large.7
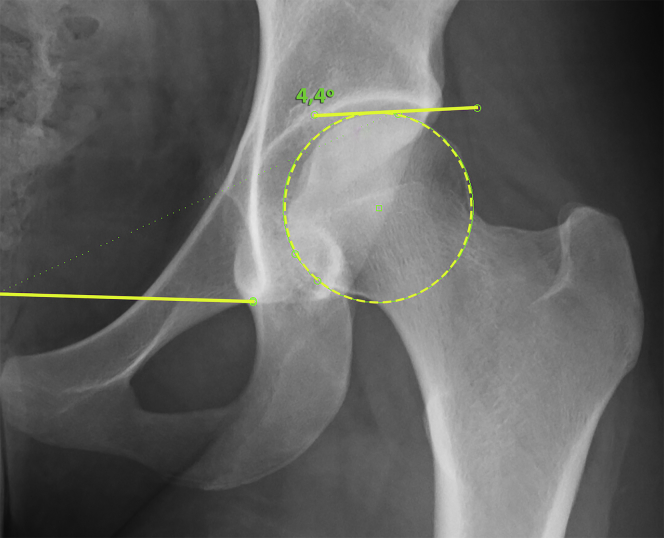
Tönnis Angle
The Tönnis angle is derived off a horizontal line drawn from teardrop to teardrop (or 2 other reference points on each hemipelvis) and a line tangential to the weight-bearing dome (i.e. sourcil) of the acetabulum. The reference range for normal Tönnis angle is −10° to 10°. A Tönnis angle >10° is indicative of acetabular dysplasia, and a Tönnis angle ≤10° is indicative of a pincer lesion.3 Tönnis angle is the most representative radiographic measurement of acetabular volume and femoral head coverage, as demonstrated by a study that related radiographic measurements with computed tomography volumetric measurements (Fig 3).8
Fig 3.
Anteroposterior radiograph of a left hip showing a Tönnis angle measurement where a horizontal teardrop-to-teardrop line has been drawn and a line tangential to the weight-bearing dome of the acetabulum depicts the Tönnis angle. The reference range for normal Tönnis angle is −10° to 10°. A Tönnis angle >10° is indicative of acetabular dysplasia, and a Tönnis angle ≤10° is indicative of a pincer lesion.
Neck-Shaft Angle
The femoral neck to shaft angle is measured by the angle created by a line from the center of the femoral head down the axis of the femoral neck and a second line drawn down the shaft of the femur. Standard femoral neck-shaft angles range from 125° to 145°. A femoral neck-shaft angle >145° indicates coxa valga, and a neck-shaft angle <125° indicates the presence of coxa vara. Abnormal femoral neck to shaft angles may be associated with injury or greater strain upon the hip secondary to abnormal hip development and biomechanics.3
Sharp Angle
Sharp developed a method for quantifying acetabular development known as the acetabular angle or Sharp angle. The basis of the Sharp angle measurement is the theory that underdeveloped or dysplastic hips may concentrate increased force on the weight-bearing acetabular dome, predisposing this location to early articular cartilage degeneration and resulting in premature development of osteoarthritis.9
The Sharp angle is measured by a horizontal line drawn between the bilateral teardrops (inferior end projection of the acetabular fossa floor) and an additional line to the lateral acetabular roof.9 A modification of the Sharp angle measurement by Agus et al. defines the Sharp angle as the angle between the horizontal line connecting the bilateral teardrops and the most lateral aspect of the acetabular sourcil (the acetabular condensation of subchondral bone).10
A normal Sharp angle is between 33° and 38°. An abnormal Sharp angle is defined as an angle <32°, defined as insignificant; between 39° and 42°, defined as borderline; and final >42°, defined as dysplastic (Fig 4).9
Fig 4.
Sharp's angle measurement on a left anteroposterior hip radiograph. The acute angle measured between the projection of the horizontal teardrop line and the line connecting the teardrop to the lateral acetabulum is performed. A normal Sharp angle is between 33° and 38°. An abnormal Sharp angle is defined as an angle <32°, defined as insignificant; between 39° and 42°, defined as borderline; and final >42°, defined as dysplastic.
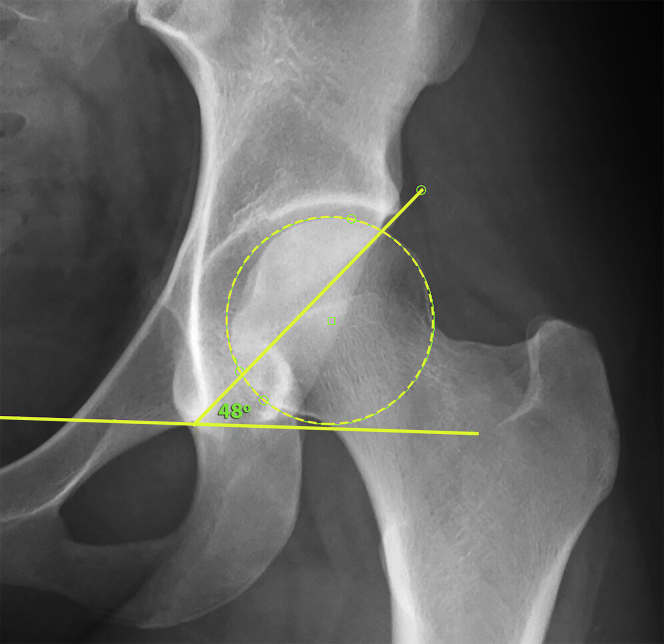
Lateral Center Edge Angle of Wiberg
Acetabular coverage can also be quantitatively assessed with the lateral center edge angle of Wiberg. This angle is between a line drawn from the center of the femoral head to the lateral edge of the acetabulum and a second line that is parallel to the longitudinal pelvic axis.3, 11 There is inconsistency in the literature about whether the angle is best measured at the most lateral aspect of the acetabulum rather than the sourcil.11 The normal lateral center edge of Wiberg is between 26° and 42°. Angles <26° are indicative of hip dysplasia.3 Specifically, a lateral center edge angle <20° is considered dysplastic, ≥20° and ≤25° is considered borderline dysplastic, ≥26° and ≤40° is considered normal, and ≥40° is considered overcovered (Fig 5).11
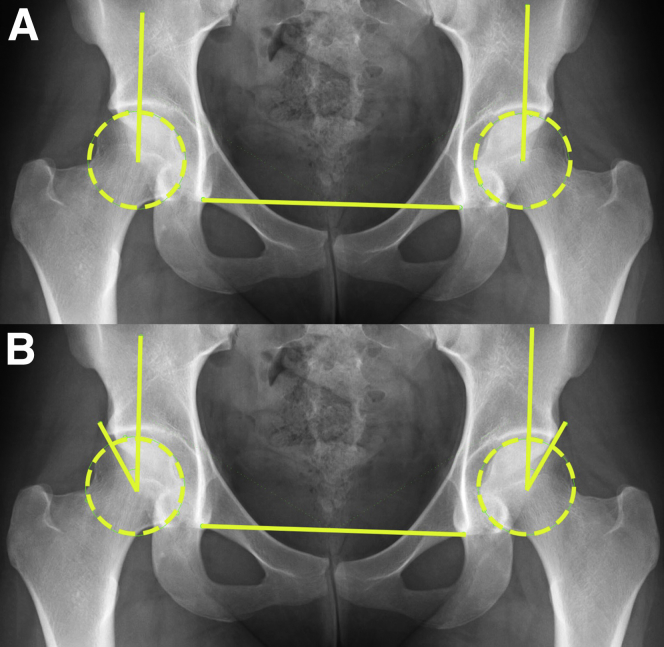
Fig 5.
Anteroposterior radiographic assessment of both hips. In order to measure the lateral center edge angle (LCE) (A), determine the center of the femoral head using a circle tool. Using an angle measurement, a line is drawn from the center of the femoral head vertically that parallels the longitudinal pelvic axis. (B) The LCE is created by an intersection angle between the first line and one drawn from the outermost weight-bearing aspect of the lateral edge of the acetabular socket or pincer lesion.
Acetabular Depth
Standard AP pelvis radiographs can be used to determine whether protrusio acetabuli is present, which is defined as the femoral head projecting medial to the ilioischial line.3 This view can also be used to determine coxa profunda—defined as the femoral head lying medial to the posterior wall of the acetabulum and the acetabular fossa protruding medial to the ilioischial line (Fig 6).3, 12
Fig 6.
Anteroposterior radiographic assessment of the right hip demonstrating protrusion acetabuli. The femoral head projects medial to the ilioischial line as demonstrated by the arrows in panel A. In other instances, there is medialization of the femoral head and protrusion acetabuli with the femoral head projecting medial to the ilioischial and the iliopectineal lines as indicated by the arrows in panel B.
Characterization of Femoroacetabular Impingement Conditions
Patients with the clinical condition of femoroacetabular impingement usually present with groin pain and limited hip motion, although the imaging findings differ depending on the anatomic type of impingement. This may result in clinically identifiable limitations in hip range of motion and ultimately may lead to chondral and labral injury. The 3 main types of femoroacetabular impingement recognized on radiographic evaluation include pincer, cam, and combined/mixed impingement.
Pincer Impingement
Pincer impingement is related to acetabular anatomy. It may occur at the site of acetabular retroversion as demonstrated by the crossover sign on an AP pelvis radiograph. It may also be secondary to excessive coverage of the femoral head by the acetabulum as demonstrated by the anterior or lateral center edge angle. Pincer impingement is more common in females.
Acetabular retroversion can have several radiographic features that allow the arthroscopic hip surgeon to identify this variation of normal anatomy. The posterior wall of the acetabulum can project medial to the center of hip rotation, thus resulting in femoral head undercoverage. Typically, the posterior wall of the acetabulum intersects the center of the femoral head of the hip joint. Another indicator of acetabular retroversion is the ischial spine projecting medial to the quadrilateral plate—known as the ischial spine sign. The crossover sign is the projection of the anterior and posterior walls on an AP pelvis radiograph crossing caudally to the lateral edge of the acetabulum. The positive crossover sign coupled with a lateral center edge angle <35° may suggest acetabular retroversion.3, 13, 14
Cam Impingement
Cam impingement is characterized by asphericity of the femoral head resulting in abnormal contour of the femoral head-neck junction. This is best identified on the 45° Dunn view radiograph and quantified by measurement with the alpha angle. Cam impingement is more commonly identified in males.
Mixed Impingement
Mixed impingement refers to both femoral head-neck junction, as well as acetabular dysmorphisms, resulting in abnormal contact between the femoral and acetabular anatomy.15 This is the most common presentation, occurring at the anterior femoral neck and anterosuperior acetabular rim.16
Discussion
Each of the radiographic views allow for measurement or evaluation of certain aspects of the hip joint (Table 1). The AP pelvis radiograph allows for evaluation of coxa profunda, coxa magna, protrusion acetabulii, and femoral head sphericity. Additionally, the AP pelvis radiograph allows for evaluation of a saber tooth sign, posterior wall sign, measurement of the lateral center edge angle, assessment of overall joint health including quantitative joint space measurements, and application of the Tönnis classification.2, 3, 14, 15, 17 The false-profile radiograph allows for evaluation of the anterior center edge angle, hip articular joint space, and anterior inferior iliac spine morphology.4, 18 The cross-table lateral and the Dunn/frog-leg lateral views allow for assessment of the alpha angle and cam morphology.2, 7, 14 The cross-table lateral also facilitates assessment of the posterior hip joint space.3
Table 1.
Pearls and Pitfalls of Qualitative and Quantitative Analysis of Hip Radiographs Prior to Hip Arthroscopy
| Pearls | Pitfalls |
|---|---|
| Standardizing the radiographic views taken on all hip arthroscopy patients allows for consistent quantitative measurements during preoperative assessment. | Radiographic views of the hip joint demonstrate osseous anatomy but do not provide the soft-tissue detail of magnetic resonance imaging (MRI) |
| Radiographic views must be performed in a similar manner and by a similar protocol to ensure quantitative measurements are accurate. | Nonstandardized or incomplete x-ray protocols may result in the inability to perform a thorough evaluation of the hip joint. |
| X-ray evaluation of the hip joint is an affordable and cost-effective methodology of radiographic assessment. | X-ray evaluation does expose the patient to ionizing radiation. |
| Radiographs can be taken relatively quickly during or prior to an orthopaedic clinic appointment, thereby not disrupting the flow of clinic. | Standard radiographs are often required prior to insurance approval of more advanced imaging modalities, such as computed tomography scan or MRI. |
Radiographs are often a standard part of an orthopaedic evaluation of hip pain. Despite the use of 3-dimensional imaging, such as computed tomography scanning (CT scan) and magnetic resonance imaging, evaluation with plain radiographs remains a gold standard for initial evaluation.8 Further, radiographic assessment of the hip joint is a more economical initial screening than many 3-dimensional imaging modalities.4, 8
A drawback of radiographs of the pelvis and hip joint, especially in young patients, is the exposure to ionizing radiation. Radiation exposure from standard imaging of the hip and pelvis was reported by Nepple et al.; exposure from a standard AP pelvis is 0.24 mSv; from Dunn or frog-leg lateral, 0.12 mSv; and from a cross-table lateral, 0.89 mSv.19 Traditional CT scans of the hip and pelvis result in exposure of 5 to 7 mSv, although newer techniques have limited this value to 2.5 mSv.19
Radiographs must have sufficient quality for standardizing the various measurements detailed in this manuscript. In our experience, there can be some interpretation and measurement error when performing these quantitative techniques; however, these types of measurements become more accurate and reproducible with experience. Whereas measurement of angles does not require calibration, measurement of joint space requires calibration with a radiodense sphere of a defined size and automated software or manual techniques.
This manuscript details a systematic approach for radiographic evaluation of the hip to quantify various hip pathologies. Radiographs provide the surgeon with a valuable and economic assessment of the hip joint. Despite newer imaging techniques, standard radiographic views of the hip joint allow for meaningful assessment that may guide in the treatment of various hip joint disorders. However, radiographic assessment in isolation is not sufficient for making clinical recommendations, and the orthopaedic surgeon must put the quantitative measurements and assessment of hip radiographs in the context of the medical history, the patient's work and lifestyle demands, physical examination, and other advanced imaging modalities. Only after merging the careful assessment of all of these factors can treatment recommendations be rendered (Table 2).
Table 2.
Quantification of Hip Radiographic Measurements
| Measurement | Range for Measurements |
|---|---|
| Sharp angle | 33°-38°, normal |
| <32°, insignificant | |
| 39°-42°, borderline | |
| >42°, dysplastic | |
| Tönnis angle | −10° to 10°, normal |
| >10°, acetabular dysplasia | |
| <10°, pincer lesion | |
| Lateral center edge angle of Wiberg | 22°-42°, normal |
| <20°, dysplastic | |
| ≥20° and ≤25°, borderline dysplastic | |
| ≥40°, overcovered | |
| Arthritis | <2-mm joint space indicative of arthritis best managed nonarthroscopically |
| Alpha angle | <55°, normal |
| >55°, cam femoroacetabular impingement |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.M. receives American Board of Medical Specialties (ABMS)-American Board of Orthopaedic Surgeons (ABOS) Visiting Scholars Grant; he was also awarded with US Patent 08926626. M.J.P. receives support from ISHA, Smith & Nephew, MIS, MJP Innovations, LLC, Ossur, Siemens, Vail Valley Medical Center, Arthrosurface, DonJoy, Slack, Elsevier, and Linvatec. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A standard anterior posterior radiograph of the hip is quantitatively assessed. The Sharp angle is created between a horizontal from 2 separate radiographic equivalent points on the pelvis (such as the teardrop) and a line drawn from the teardrop to the lateral portion of the acetabulum. The Sharp angle helps to radiographically define dysplasia in the hip. Anteroposterior radiograph of a left hip showing a Tönnis angle measurement where a horizontal teardrop-to-teardrop line has been drawn and a line tangential to the weight-bearing dome of the acetabulum depicts the Tönnis angle. A Tönnis angle >10° is indicative of acetabular dysplasia, and a Tönnis angle ≤10° is indicative of a pincer lesion. In order to measure the lateral center edge angle (LCE), first determine the center of the femoral head using a circle tool. Using an angle measurement, a line is drawn from the center of the femoral head vertically that parallels the longitudinal pelvic axis. The LCE is created by an intersection angle between the first line and one drawn from the outermost weight-bearing aspect of the lateral edge of the acetabular socket or pincer lesion. The LCE helps quantify the spectrum of acetabular dysplasia versus overcoverage of the acetabulum. A measurement of joint space is also performed at 3 separate locations. A joint space of <2 mm may indicate arthritis that is too severe for arthroscopic intervention. The Dunn view can be obtained at 45° or 90° and is used to evaluate the femoral head sphericity and contour of the femoral head neck junction. In order to accurately measure the alpha angle, a line should be drawn from the center of the narrowest point of the femoral neck to the center of the femoral head using a best-fit circle on the Dunn view. The alpha angle is between the line down the axis of the femoral neck and a line drawn to the location where the femoral head loses its sphericity. Alpha angles >50.5° are indicative of cam femoroacetabular impingement deformity, and normal alpha angles are typically considered to be <50.5°.
References
- 1.Cvetanovich G.L., Chalmers P.N., Levy D.M. Hip arthroscopy surgical volume trends and 30-day postoperative complications. Arthroscopy. 2016;32:1286–1292. doi: 10.1016/j.arthro.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 2.Bardakos N.V., Villar R.N. Predictors of progression of osteoarthritis in femoroacetabular impingement: A radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 3.Howse E.A., Stubbs A.J. Imaging in hip preservation surgery—plain x-rays, computed tomography, and magnetic resonance imaging. In: Byrd J.W.T., Bedi A., Stubbs A.J., editors. AANA advanced arthroscopic surgical techniques: the hip. SLACK; Thorofare, NJ: 2016. p. 340. [Google Scholar]
- 4.Philippon M.J., Briggs K.K., Carlisle J.C., Patterson D.C. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013;471:2492–2496. doi: 10.1007/s11999-012-2779-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tonnis D., Heinecke A. Acetabular and femoral anteversion: Relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 6.de Sa D., Urquhart N., Philippon M., Ye J.E., Simunovic N., Ayeni O.R. Alpha angle correction in femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:812–821. doi: 10.1007/s00167-013-2678-6. [DOI] [PubMed] [Google Scholar]
- 7.Johnston T.L., Schenker M.L., Briggs K.K., Philippon M.J. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669–675. doi: 10.1016/j.arthro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Stubbs A.J., Anz A.W., Frino J., Lang J.E., Weaver A.A., Stitzel J.D. Classic measures of hip dysplasia do not correlate with three-dimensional computer tomographic measures and indices. Hip Int. 2011;21:549–558. doi: 10.5301/HIP.2011.8696. [DOI] [PubMed] [Google Scholar]
- 9.Sharp I.K. Acetabular dysplasia: The acetabular angle. J Bone Joint Surg Br. 1961;43:268–272. [Google Scholar]
- 10.Agus H., Bicimoglu A., Omeroglu H., Tumer Y. How should the acetabular angle of Sharp be measured on a pelvic radiograph? J Pediatr Orthop. 2002;22:228–231. [PubMed] [Google Scholar]
- 11.Hanson J.A., Kapron A.L., Swenson K.M., Maak T.G., Peters C.L., Aoki S.K. Discrepancies in measuring acetabular coverage: Revisiting the anterior and lateral center edge angles. J Hip Preserv Surg. 2015;2:280–286. doi: 10.1093/jhps/hnv041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nepple J.J., Lehmann C.L., Ross J.R., Schoenecker P.L., Clohisy J.C. Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg Am. 2013;95:417–423. doi: 10.2106/JBJS.K.01664. [DOI] [PubMed] [Google Scholar]
- 13.Siebenrock K.A., Kalbermatten D.F., Ganz R. Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin Orthop Relat Res. 2003:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 14.Boone G., Pagnotto M.R., Walker J.A., Trousdale R.T., Sierra R.J. Radiographic features associated with differing impinging hip morphologies with special attention to coxa profunda. Clin Orthop Relat Res. 2012;470:3368–3374. doi: 10.1007/s11999-012-2539-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 16.Philippon M., Schenker M., Briggs K., Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: Associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. doi: 10.1007/s00167-007-0332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sakai T., Nishii T., Sugamoto K., Yoshikawa H., Sugano N. Is vertical-center-anterior angle equivalent to anterior coverage of the hip? Clin Orthop Relat Res. 2009;467:2865–2871. doi: 10.1007/s11999-009-0802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chosa E., Tajima N. Anterior acetabular head index of the hip on false-profile views. New index of anterior acetabular cover. J Bone Joint Surg Br. 2003;85:826–829. [PubMed] [Google Scholar]
- 19.Nepple J.J., Prather H., Trousdale R.T. Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(Suppl 1):S20–S26. doi: 10.5435/JAAOS-21-07-S20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A standard anterior posterior radiograph of the hip is quantitatively assessed. The Sharp angle is created between a horizontal from 2 separate radiographic equivalent points on the pelvis (such as the teardrop) and a line drawn from the teardrop to the lateral portion of the acetabulum. The Sharp angle helps to radiographically define dysplasia in the hip. Anteroposterior radiograph of a left hip showing a Tönnis angle measurement where a horizontal teardrop-to-teardrop line has been drawn and a line tangential to the weight-bearing dome of the acetabulum depicts the Tönnis angle. A Tönnis angle >10° is indicative of acetabular dysplasia, and a Tönnis angle ≤10° is indicative of a pincer lesion. In order to measure the lateral center edge angle (LCE), first determine the center of the femoral head using a circle tool. Using an angle measurement, a line is drawn from the center of the femoral head vertically that parallels the longitudinal pelvic axis. The LCE is created by an intersection angle between the first line and one drawn from the outermost weight-bearing aspect of the lateral edge of the acetabular socket or pincer lesion. The LCE helps quantify the spectrum of acetabular dysplasia versus overcoverage of the acetabulum. A measurement of joint space is also performed at 3 separate locations. A joint space of <2 mm may indicate arthritis that is too severe for arthroscopic intervention. The Dunn view can be obtained at 45° or 90° and is used to evaluate the femoral head sphericity and contour of the femoral head neck junction. In order to accurately measure the alpha angle, a line should be drawn from the center of the narrowest point of the femoral neck to the center of the femoral head using a best-fit circle on the Dunn view. The alpha angle is between the line down the axis of the femoral neck and a line drawn to the location where the femoral head loses its sphericity. Alpha angles >50.5° are indicative of cam femoroacetabular impingement deformity, and normal alpha angles are typically considered to be <50.5°.