Abstract
Hip arthroscopy is a technically demanding procedure that is currently characterized by a “steep” learning curve. Therefore, achieving an advanced technical level is often challenging, especially for the amateur hip arthroscopist. Hand laterality when training in hip arthroscopy is an aspect that has been omitted. In addition, the technical differences regarding the handling of the surgical instruments when performing hip arthroscopy on the left versus right hip can influence the technical excellence. This Technical Note summarizes our preferred hip arthroscopy technique by comparing the surgeon's hand position when operating on the left versus right hip. We also emphasize how the surgeon's hand laterality affects the instrument manipulation during the procedure and potentially the clinical outcomes.
The arthroscopic approach to treat hip pathology has increased dramatically during the past 2 decades.1, 2, 3 Symptomatic chondrolabral pathology and bony deformities can be successfully treated by arthroscopy because of the development of techniques and a deeper understanding of the pathophysiological mechanisms behind femoroacetabular impingement (FAI).4 In addition, improvements in surgical instrumentation and imaging techniques have significantly contributed to the advancement of arthroscopic hip surgery.2 Correspondingly, the numbers of procedures performed and surgeons trained in hip arthroscopy have risen exponentially during the past several years.2, 3
Hip arthroscopy is considered a technically challenging procedure, and its learning curve has been described as “steep,” despite the limited validated data on this subject.5 Several aspects contribute to the characterization of hip arthroscopy as a highly demanding and complex procedure, including the following: deep joint location, thickness of the capsule, long distance of the surgeon's hands from the working area, limited working space because of inelastic adjacent structures, and high congruency between the femoral head and acetabulum.5 On the basis of our experience, we have observed that surgeon handedness may pose different challenges for surgeons during their training in hip arthroscopy. For example, when a right-handed surgeon holds the shaver blade or electrothermal probe with the dominant hand and the arthroscope with the nondominant hand, it allows for better manipulation of the surgical instruments and thus facilitates the procedures performed. On the basis of this, a right-handed surgeon may feel more comfortable when operating on a left hip because he or she can hold the instruments with the dominant hand through the anterolateral (AL) portal while holding the camera with the nondominant hand through the midanterior (MA) portal. However, when a right-handed surgeon operates on a right hip (mirror image), this would result in holding the instruments with the nondominant hand (left) through the AL portal and the arthroscope with the dominant hand (right) through the MA portal. We believe that holding the surgical instruments with the dominant hand during hip arthroscopy would result in improved surgical technique and decrease complication rates.
The purpose of this Technical Note is to describe our preferred hip arthroscopy technique by emphasizing the use of surgical instruments with the dominant hand and the arthroscope with the nondominant hand. We highlight the basic technical differences in instrument and arthroscope holding in correspondence with the actual arthroscopic view when operating on the left versus right hip, provided that the surgeon is right handed (senior author [M.J.P.]). This will be a valuable tool for hip arthroscopy beginners to achieve expertise in this field.
Surgical Technique
This section describes the surgical approach when performing hip arthroscopy on the left versus right side (Video 1). The previously described labral repair technique6 is used as an example.
Patient Preparation and Positioning
By use of a fracture table, the patient is placed in a modified supine position. To achieve adequate muscle relaxation and hip joint traction, a combination of spinal-epidural injection with general or conscious anesthesia is administered. Traction is applied to the operative hip until the vacuum sign is present on the fluoroscopic image. Slight traction is also applied to the contralateral leg, which is abducted at 45°. The table is tilted toward the nonoperative side by 10° to facilitate joint exposure during the procedure. The operative leg is internally rotated so that the femoral neck is parallel to the floor. An extra-wide perineal post is placed against the perineum to avoid soft-tissue compression injury.
Surgeon Positioning
The surgeon's orientation differs based on whether the hip arthroscopy is performed on the left or right side. When operating on the right hip, the surgeon is facing toward the feet of the patient. In contrast, when operating on the left hip, the surgeon is facing toward the patient's head (Fig 1). The surgeon should set up the surgical room (patient position, arthroscopic screen position) based on his or her predilection to accomplish technical perfection during the operation.
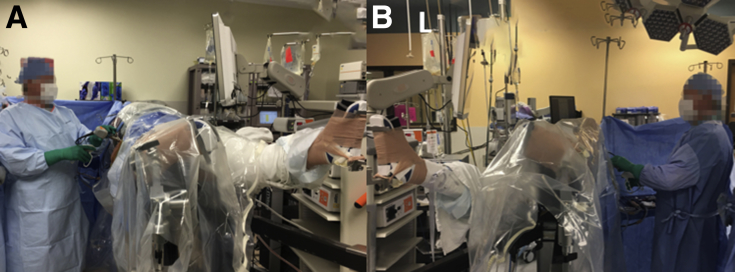
Fig 1.
Surgeon's orientation during hip arthroscopy. (A) When operating on the right side, the surgeon is facing toward the patient's feet. (B) When operating on the left hip, the surgeon is facing toward the patient's head.
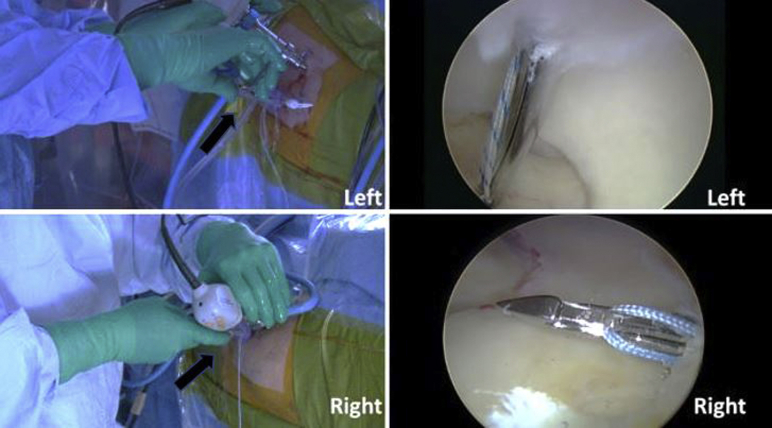
Acetabular Labrum Preparation and Rim Trimming
Whether the surgeon is operating on a left or right hip, the MA portal is used as the viewing portal (arthroscope insertion) whereas the AL portal is the working portal (instrument insertion). After the identification of a reparable acetabular labrum using direct visualization and the hip dynamic examination,7 an arthroscopic knife (Beaver Blade; Smith & Nephew) and/or shaver (Dyonics; Smith & Nephew) is used to detach the labrum from the adjacent tissues (Fig 2). Attention should be paid to protecting the healthy native labrum. The rim-trimming procedure is performed on the acetabular bone to create a bleeding bed to potentiate the healing of the repaired labrum (Fig 3). For this purpose, a 4.5-mm round, prebent polishing burr (Linvatec, Largo, FL) is used. If a pincer deformity is present, it should be addressed before the labral repair.
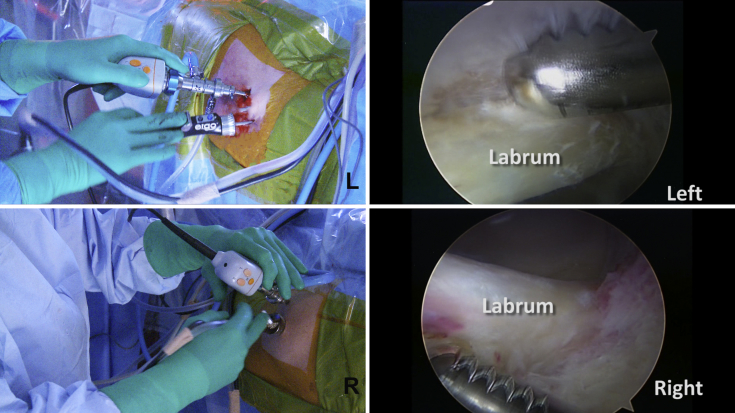
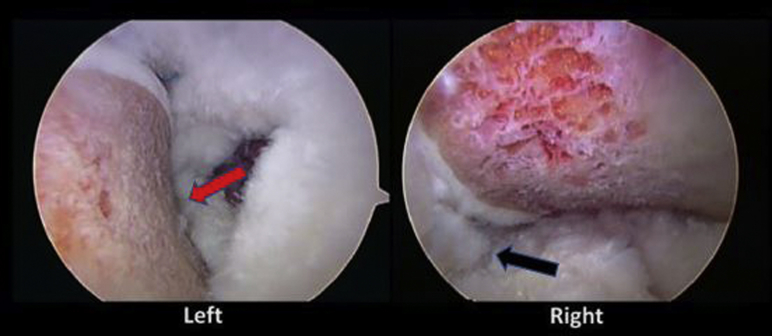
Fig 2.
When the surgeon is operating on the left hip (L), the upper portion of the screen corresponds to the superior aspect of the surgical field. When the surgeon is operating on the right hip (R), the upper portion of the screen is reversed and corresponds to the inferior aspect of the surgical field.
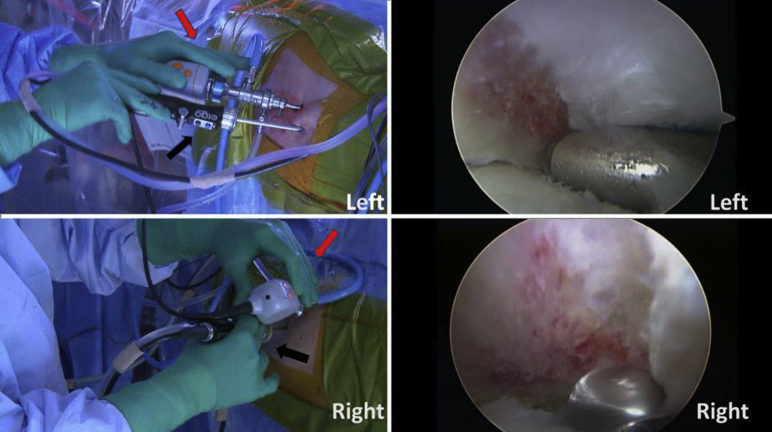
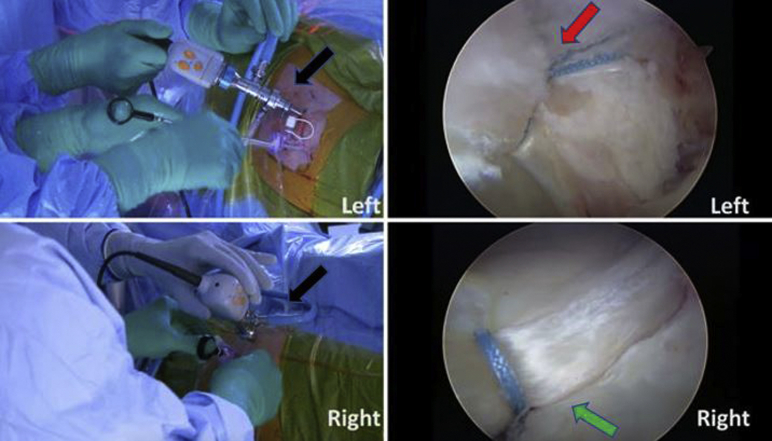
Fig 3.
Rim trimming. The surgeon holds the arthroscope with the nondominant hand (red arrows) through the midanterior portal and the burr with the dominant hand (black arrows) through the anterolateral portal for both a left hip operation and a right hip operation.
Labral Repair
The MA portal is used to place the arthroscope in the joint, whereas anchor placement is performed through the AL portal. Although the portal use is the same in both a right hip and a left hip, the position of the surgeon's hands is adjusted to insert the anchors using the dominant hand and hold the arthroscope with the nondominant hand. To stabilize the torn labrum against the acetabulum, suture anchors are placed on the acetabular rim beginning medially and moving laterally (Fig 4). At the 3-o'clock position on the acetabulum, a 1.5-mm suture anchor is usually used, whereas at the 12-o'clock position or laterally, a 2.3-mm anchor is placed most of the time. The number and size of anchors depend on the length as well as the position of the labral tear. The distance between the anchors is approximately 10 mm. The angle for anchor placement is critical to avoid bony penetration, which on the medial side results in future irritation of the adjacent psoas tendon and pain.8 The arthroscopic sutures can be passed through (if remnant tissue is adequate) or in a loop fashion around the labrum to stabilize it against the acetabular rim (Fig 5). The arthroscopic knot is placed toward the capsular side to avoid cartilage damage (Fig 6).
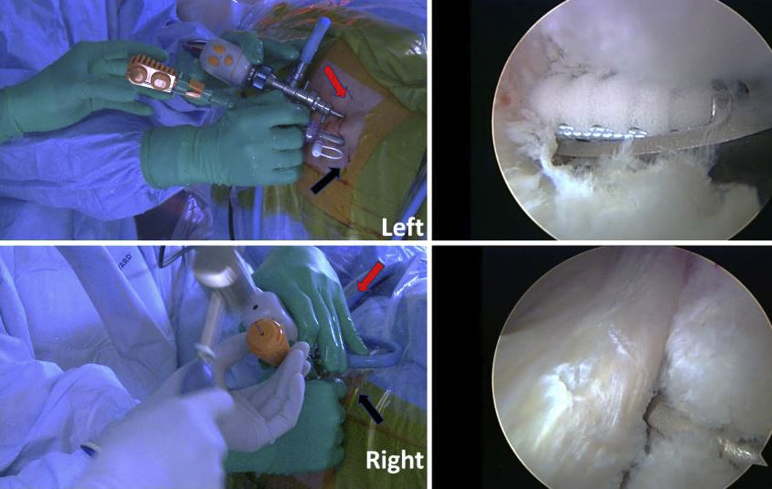
Fig 4.
Anchor placement. The surgeon holds the arthroscope with the nondominant hand (red arrows) through the midanterior portal and the burr with the dominant hand (black arrows) through the anterolateral portal for anchor placement in both a left hip and a right hip.
Fig 5.
Suture passage to stabilize labrum against acetabulum. The dominant hand (arrows) should always be used to manipulate the instrument, which is inserted through the anterolateral portal.
Fig 6.
Knot placement on capsular side of labrum (red arrow) to avoid future cartilage damage. The midanterior portal is the viewing portal (black arrows). When the surgeon is operating on the right hip, the arthroscopic image shows the surgical field in upside-down fashion (green arrow).
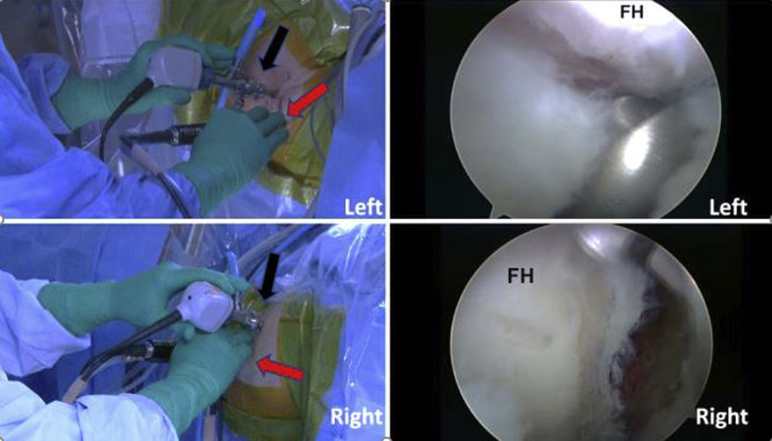
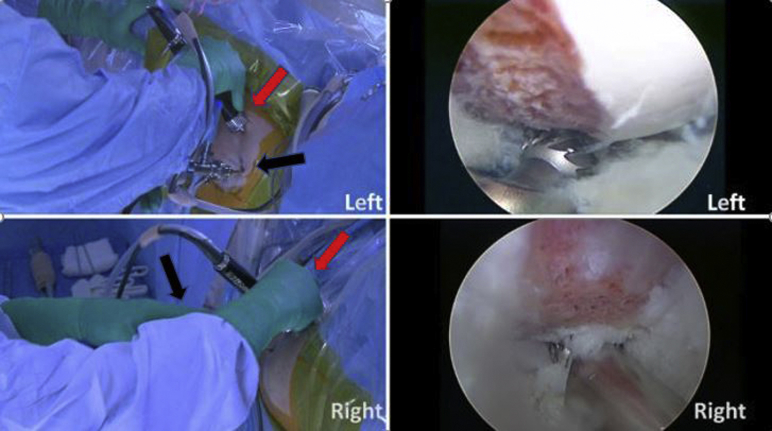
Femoral Osteochondroplasty
Correction of cam impingement is usually performed after dynamic evaluation of the hip to localize the cam deformity and area of impingement. A 5.5-mm round burr (Smith & Nephew) is used to resect the “bump” from the femoral bone (Fig 7). Cam resection begins from the AL portion of the lesion and extends to the posterolateral portion (Fig 8). For both left and right hips, when the surgeon is resecting the AL portion of the cam lesion, the arthroscope is inserted through the MA portal and the burr using the AL portal. In contrast, when the surgeon is resecting the posterolateral portion of the cam lesion, the AL portal is used as the viewing portal (arthroscope) whereas the MA portal becomes the working portal (burr). The lateral epiphyseal vessels should be protected throughout the resection. Hip dynamic examination is performed7 to assess the restoration of the hip seal mechanism,9 as well as the bone congruency (adequate cam and/or pincer resection), and to ensure adequate labral stabilization (Fig 9).
Fig 7.
Anterolateral femoral osteochondroplasty. The burr is gripped with the dominant hand through the anterolateral portal (working portal, red arrows). The midanterior portal is the viewing portal (black arrows). (FH, femoral head.)
Fig 8.
Posterolateral femoral osteochondroplasty. The burr is gripped with the dominant hand through the midanterior portal (working portal, red arrows). The anterolateral portal is the viewing portal (arthroscope, black arrows).
Fig 9.
Final look of cam osteochondroplasty. The seal of the labrum and femoral head (black arrow) and a smooth head-neck offset (red arrow) prevent femoroacetabular impingement recurrence.
Discussion
Good to excellent clinical outcomes have been reported using hip arthroscopy to address FAI and chondrolabral pathology.10, 11, 12 Unfortunately, a systematic review recently showed that the learning curve for this procedure has been repeatedly characterized as steep, with a significantly higher complication rate occurring early on the curve.5 According to the systematic review's authors, although the cutoff value at which the learning curve plateaus has been set at 30 cases, this result should be interpreted with caution because it was not based on a validated study tool specifically for this purpose. Apart from the surgical technique, patient selection is important for hip arthroscopy to achieve a satisfactory clinical outcome. The presence of severe osteoarthritis or dysplasia precludes hip arthroscopy as the ideal procedure to address hip pathology.13, 14 Postoperative adhesions and residual FAI are common intraoperative findings in patients undergoing revision hip arthroscopy.15
About 10% of the population is left handed, and male persons have higher rates of left handedness than female persons.16 Medical school training is identical regardless of the intention of each medical student to pursue a surgical versus nonsurgical specialty. Therefore, little attention is given to the surgical skills of the student, as well as hand laterality. In addition, most surgical instruments are designed for right-handed surgeons.17 However, the impact of hand dominance on surgical outcomes has not been investigated in hip arthroscopy. Moloney et al.18 showed that malpositioning of the sliding hip screw occurred significantly more frequently on the left than on the right when the surgical procedure was performed by right-handed surgeons. Mehta and Lotke19 examined the impact of surgeon handedness on total knee arthroplasty outcomes. Total knee arthroplasty on the right knee yielded superior 1-year outcomes compared with the left knee when performed by a single right-handed orthopaedic surgeon. On the basis of this finding, the effect of dexterity and proprioception on patient outcomes was highlighted.
Given the aforementioned findings and considering the fact that hip arthroscopy is generally associated with a steep learning curve,5 the handedness of the amateur surgeon might affect the surgical technique and potentially the patient outcome. A previous study on psychomotor skills in endoscopic surgery evaluated the surgical performance of medical students based on different variables: hand-eye coordination, spatial perception, perceptual processing of indirect image information, and balance or manipulation of the probe within a magnified field.20 Statistically significant differences in the error rate and first-time accuracy between the dominant and nondominant hands were observed. An interesting finding was that these 2 parameters did not significantly change with practice, contrary to execution time and the degree of angular deviations, which improved with training. This finding shows the influence of handedness on endoscopic and arthroscopic procedures.
This Technical Note summarizes the basic steps of our preferred hip arthroscopy technique using the AL and MA portals, with emphasis on the hand positions when performing right- versus left-side hip arthroscopy. The senior author (M.J.P.) is a right-handed surgeon and prefers to use shaver blades and electrothermal probes with his dominant hand while holding the arthroscope with the nondominant hand. This allows for better instrument manipulation and improved tactile sensation during the procedure. Right-handed surgeons may feel more comfortable performing hip arthroscopy on left hips. This is because they are able to hold the surgical instruments with the dominant hand (AL portal) while using the nondominant hand (left hand) only for visualization (MA portal). On the basis of the aforementioned theory, when operating on the right hip, the right-handed surgeon would hold the surgical instruments with the nondominant hand through the AL portal while using his or her dominant hand for visualization. This could result in rough instrumentation handling, reduced tactile feedback, and higher perceptual processing of each surgical maneuver. This phenomenon may be exaggerated for surgeons on the learning curve.21 Therefore, the senior author suggests using the dominant hand for the instruments for all surgical procedures, whether one is operating on the left or right hip (Video 1). This is crucial to accomplish the maximum technical accuracy based on each surgeon's skills. Another key point is the standing position of the surgeon relative to the operating hip. When performing hip arthroscopy on the left side, the senior author stands parallel to the extremity or slightly facing toward the patient's head. In contrast, when operating on the right hip, the surgeon stands in a position facing slightly toward the patient's feet while the surgeon's left elbow is elevated. This position allows for better arm-hand maneuverability and arm-hand steadiness (Table 1).
Table 1.
Pearls and Pitfalls
| Pearls |
| Using the instrument with the dominant hand and the arthroscope with the nondominant hand allows better instrument manipulation and improved tactile sensation. |
| For right-handed surgeons, facing toward the patient's feet with a slightly elevated left elbow results in better arm-hand maneuverability and arm-hand steadiness during right hip surgery. |
| Pitfalls |
| Gripping instruments close to the portals allows precise control of instruments, particularly during cam osteochondroplasty. |
| Control of the light source can be maintained with the ring finger and small finger to change the angle of vision frequently to obtain multiple perspectives to optimize the procedure. |
Hip arthroscopy is a demanding procedure, and young surgeons often struggle to become proficient. Apart from the basic surgical training, emphasizing the impact of hand laterality on the surgical technique is useful during the learning process (Table 2). Highlighting the technical differences between left and right hip arthroscopy based on the approach of an experienced surgeon further contributes to the learning experience.
Table 2.
Surgical Tips on Hand Laterality and Instrument Use During Labral Repair
| Procedure | Surgical Tips |
|---|---|
| Acetabular labrum preparation and rim trimming | Arthroscope: nondominant hand (MA) Working instrument: dominant hand (AL) |
| Labral repair | Arthroscope: nondominant hand (MA) Working instrument: dominant hand (AL) |
| Femoral osteochondroplasty | |
| Anterolateral cam resection | Arthroscope: nondominant hand (MA) Burr: dominant hand (AL) |
| Posterolateral cam resection | Arthroscope: nondominant hand (AL) Burr: dominant hand (MA) |
AL, anterolateral portal; MA, midanterior portal.
Although a similar technique article would be ideal for left-handed surgeons, we strongly encourage them to use their dominant hand for manipulating instruments. The standing position can also be altered based on their handedness to facilitate the surgical technique.
Acknowledgment
The authors thank Chris Jacobsen and Shannen McNamara for their contribution to the preparation of this article.
Footnotes
The authors report the following potential conflict of interest or source of funding: K.K.B. receives support from Smith & Nephew. Research grant. Smith & Nephew, Ossur, Siemens, Vail Valley Medical Center. M.J.P. receives support from Smith & Nephew, ISHA, MIS, Ossur, Siemens, Vail Valley Medical Center, Arthrosurface, DonJoy, Slack, Elsevier, Linvatec, MJP Innovations. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Comparison of surgeon's position, utilization of surgical instruments, and arthroscopic visualization between right and left hip arthroscopy.
References
- 1.Clohisy J.C., Baca G., Beaule P.E. Descriptive epidemiology of femoroacetabular impingement: A North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41:1348–1356. doi: 10.1177/0363546513488861. [DOI] [PubMed] [Google Scholar]
- 2.Colvin A.C., Harrast J., Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. doi: 10.2106/JBJS.J.01886. [DOI] [PubMed] [Google Scholar]
- 3.Maradit Kremers H., Schilz S.R., Van Houten H.K. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32:750–755. doi: 10.1016/j.arth.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Philippon M.J., Bolia I., Locks R., Utsunomiya H. Treatment of femoroacetabular impingement: Labrum, cartilage, osseous deformity, and capsule. Am J Orthop (Belle Mead NJ) 2017;46:23–27. [PubMed] [Google Scholar]
- 5.Hoppe D.J., de Sa D., Simunovic N. The learning curve for hip arthroscopy: A systematic review. Arthroscopy. 2014;30:389–397. doi: 10.1016/j.arthro.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Philippon M.J., Faucet S.C., Briggs K.K. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2:e73–e76. doi: 10.1016/j.eats.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Locks R., Chahla J., Mitchell J.J., Soares E., Philippon M.J. Dynamic hip examination for assessment of impingement during hip arthroscopy. Arthrosc Tech. 2016;5:e1367–e1372. doi: 10.1016/j.eats.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lertwanich P., Ejnisman L., Torry M.R., Giphart J.E., Philippon M.J. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011;39(suppl):111s–116s. doi: 10.1177/0363546511413746. [DOI] [PubMed] [Google Scholar]
- 9.Philippon M.J., Nepple J.J., Campbell K.J. The hip fluid seal—Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22:722–729. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 10.Sawyer G.A., Briggs K.K., Dornan G.J., Ommen N.D., Philippon M.J. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43:1683–1688. doi: 10.1177/0363546515581469. [DOI] [PubMed] [Google Scholar]
- 11.Geyer M.R., Philippon M.J., Fagrelius T.S., Briggs K.K. Acetabular labral reconstruction with an iliotibial band autograft: Outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41:1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 12.McDonald J.E., Herzog M.M., Philippon M.J. Performance outcomes in professional hockey players following arthroscopic treatment of FAI and microfracture of the hip. Knee Surg Sports Traumatol Arthrosc. 2014;22:915–919. doi: 10.1007/s00167-013-2691-9. [DOI] [PubMed] [Google Scholar]
- 13.Skendzel J.G., Philippon M.J., Briggs K.K., Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42:1127–1133. doi: 10.1177/0363546514526357. [DOI] [PubMed] [Google Scholar]
- 14.Kirsch J.M., Khan M., Bedi A. Does hip arthroscopy have a role in the treatment of developmental hip dysplasia? J Arthroplasty. 2017;32:S28–S31. doi: 10.1016/j.arth.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Newman J.T., Briggs K.K., McNamara S.C., Philippon M.J. Revision hip arthroscopy: A matched-cohort study comparing revision to primary arthroscopy patients. Am J Sports Med. 2016;44:2499–2504. doi: 10.1177/0363546516650888. [DOI] [PubMed] [Google Scholar]
- 16.McManus I.C. Cambridge University Press; Cambridge: 2009. The history and geography of human handedness. [Google Scholar]
- 17.Adusumilli P.S., Kell C., Chang J.H., Tuorto S., Leitman I.M. Left-handed surgeons: Are they left out? Curr Surg. 2004;61:587–591. doi: 10.1016/j.cursur.2004.05.022. [DOI] [PubMed] [Google Scholar]
- 18.Moloney D., Bishay M., Ivory J., Pozo J. Failure of the sliding hip screw in the treatment of femoral neck fractures: ‘Left-handed surgeons for left-sided hips.’. Injury. 1994;25(suppl 2):B9–B13. doi: 10.1016/0020-1383(94)90194-5. [DOI] [PubMed] [Google Scholar]
- 19.Mehta S., Lotke P.A. Impact of surgeon handedness and laterality on outcomes of total knee arthroplasties: Should right-handed surgeons do only right TKAs? Am J Orthop (Belle Mead NJ) 2007;36:530–533. [PubMed] [Google Scholar]
- 20.Hanna G.B., Drew T., Clinch P. Psychomotor skills for endoscopic manipulations: Differing abilities between right and left-handed individuals. Ann Surg. 1997;225:333–338. doi: 10.1097/00000658-199703000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tendick F., Jennings R.W., Tharp G., Stark L. Sensing and manipulation problems in endoscopic surgery: Experiment, analysis, and observation. Presence Teleoperators Virtual Env. 1993;2:66–81. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of surgeon's position, utilization of surgical instruments, and arthroscopic visualization between right and left hip arthroscopy.