Abstract
The anterior cruciate ligament suture augmentation technique is a method to augment anterior cruciate ligament reconstruction (ACLR) with autologous hamstring tendons using a braided ultrahigh–molecular weight polyester or polyethylene suture or suture tape and fixed on both the femoral and tibial sides independent of the graft to act as a backup or secondary stabilizer until complete integration and ligamentization of the graft take place. The technique is proposed to allow early rehabilitation and return to sports after ACLR and may be advantageous in patients with a high body mass index and in cases with small grafts (7 or 7.5 mm in diameter). In such situations the technique is supposed to decrease the risk of reinjury, as well as the degree of postoperative lengthening or stretching of the graft, in the early postoperative avascular phase. We describe graft preparation with the internal suture augmentation technique in arthroscopic ACLR using a cortical button system on the femoral side and a Bio-Interference Screw (Arthrex, Naples, FL) on the tibial side.
Anterior cruciate ligament (ACL) reconstruction failure occurs in different forms and as a result of many causes in both the early and late postoperative period. Primary ACL rupture recently has been reported to approach an incidence of 60.9 per 100,000 persons.1, 2, 3, 4, 5
Instability after ACL reconstruction resulting from an acute traumatic incident has been reported by some authors to comprise as many as 43% of the cases of ACL reconstruction failure.6 In animal studies, it has been shown that the ACL graft undergoes increasing incorporation into the bony tunnels, as well as vascularization, between 6 and 12 weeks and that vigorous activities or inappropriately aggressive rehabilitation can lead to graft elongation or rupture.7 The same fact has been confirmed in human patients, in whom the strength of the ACL graft during the first year after reconstruction was found to be only 30% and the resistance of the graft was found to be only 50% of that of the original ACL.7, 8 Acute and chronic loads exceeding the loads that the graft has the capacity to withstand can result in plastic deformation, elongation, loosening, or even rupture of the graft. Repetitive trauma was found to be the cause of failure in 24% to 100% of cases.3
Secondary stiffness or arthrofibrosis resulting from delayed or inappropriate postoperative rehabilitation occurs in 5.5% to 24% of cases and can be decreased if an earlier and more intensive rehabilitation protocol is adopted. However, full extension causes high stress on the graft that may result in its injury. Current early rehabilitation protocols also can produce higher stress on the graft in flexion that may lead to graft failure.9 This is particularly important in patients after ACL revision surgery, in whom a more conservative rehabilitation protocol is recommended.
With our technique, it is possible to achieve full extension as well as flexion to at least 90° within a few days thanks to the strong augmentation and backup fixation. Recent advances in ACL graft fixation techniques have evolved in the past few years, aiming at better fixation and thus yielding fewer incidences of failure and stiffness. None of these techniques is known to prevent relaxation or stretching of the graft fibers.
In this Technical Note we present our technique that augments the graft until complete ligamentization and vascularization occur, when stretching and elongation of the graft are then unlikely to occur. The technique relies on bridging the graft with a strong nonabsorbable suture (No. 2 FiberTape or No. 5 FiberWire; Arthrex, Naples, FL) that is fixed on the femoral side in an extracortical manner and on the tibial side with a Bio-Interference Screw (Arthrex) for both the graft and the internally placed suture, followed by additional extracortical backup fixation of the internal sutures with a mega-button, staple, or screw and washer. The technique also allows early and secure postoperative rehabilitation, thus decreasing the possibility of stiffness and the need for prolonged physiotherapy, with an earlier return to work and activities. The technique represents an easy addition to the standard techniques for graft preparation and can be practically adopted with modification by all techniques for ACL graft fixation.
The idea of augmenting ligamentous repair as well as reconstruction has recently been proposed by many authors and in different anatomic sites.10, 11, 12 Augmentation may be indicated with variable degrees of chronicity with different techniques, particularly with the use of allografts to protect them until complete healing and ligamentization take place. Early promising results in ACL reconstruction in canine models have been reported.10, 11, 12, 13 However, there is no published technique that describes augmenting an ACL hamstring autograft fixed with a femoral cortical button and Bio-Interference Screw on the tibial side.
Surgical Technique
The indications for our technique are patients either with an ACL rupture in the acute postinjury period or with chronic instability (Video 1). The special indications are patients with a high body mass index (>30), professional and competitive contact athletes, patients undergoing revision ACL reconstruction, and patients with relatively soft bone.
A graft preparation station (Arthrex) is used for preparation and tensioning of the hamstring tendon graft (Fig 1). According to the surgeon's preference, a strong nonabsorbable suture (No. 0 Ethibond Excel [Ethicon (Johnson & Johnson), Miami, FL] or No. 0 or No. 2 FiberWire) is used for graft preparation. The graft can be prepared with 3 or 4 folds according to its length. Both the semitendinosus and gracilis tendons are needed if the semitendinosus tendon is less than 28 cm in length, which is the minimum length needed to prepare a quadruple graft of 7 cm in length. In most cases the semitendinosus alone is not sufficient to produce a triple-folded graft of adequate diameter (minimum of 8 mm).
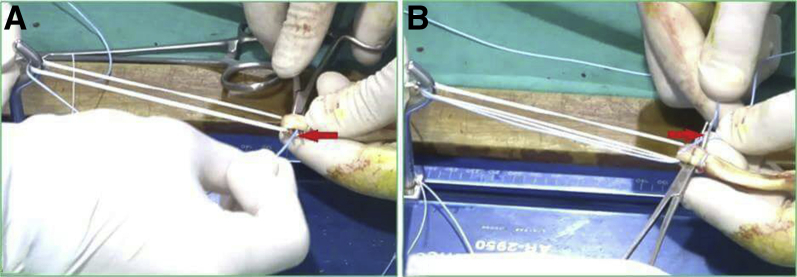
Fig 1.
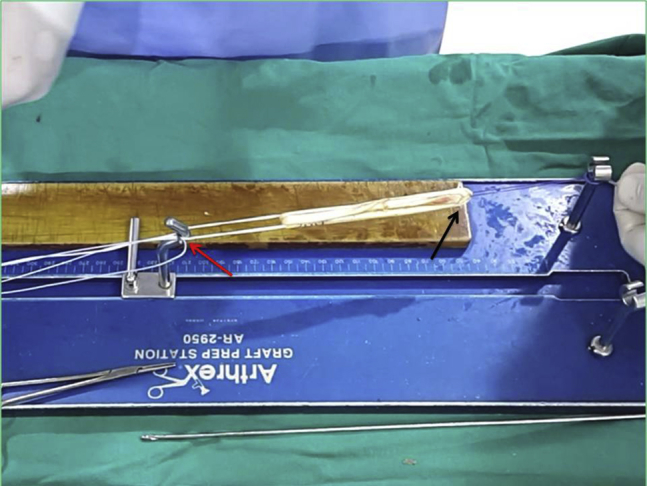
A graft preparation station is used for preparation and tensioning of the hamstring tendon graft. The femoral button is placed on the traction post (red arrow), and traction on the tibial end of the prepared graft is applied with strong suture on the station's second traction post (black arrow).
The described technique is based on the use of a cortical suspensory device (TightRope; Arthrex) on the femoral side and a Bio-Interference Screw on the tibial side. The graft is folded over the loop of the TightRope system. A braided ultrahigh–molecular weight polyethylene or polyester suture or suture tape is threaded into the holes of the femoral cortical button so that both suture ends are directed inferiorly in line with the graft (Fig 2).
Fig 2.
A braided ultrahigh–molecular weight polyester or polyethylene suture is passed through the holes of the femoral cortical button so that both suture ends are directed inferiorly in line with the graft (arrows).
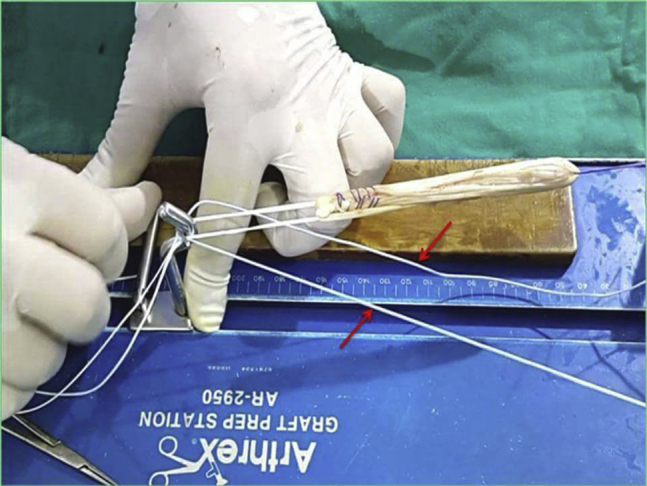
The tibial end of the graft, after folding, is whipstitched with a strong nonabsorbable suture (No. 2 FiberWire). The graft is then tensioned on the graft preparation station. The femoral button is loaded on 1 post of the preparation station, and the 2 ends of the tibial-side sutures are tied to the other post. The graft should be at least 70 mm in length. The graft is stitched in a loop fashion about 1 cm from the femoral end with a strong No. 2 FiberWire suture, starting from the central strand in an inside-out fashion, then making a complete loop around the graft, and finally passing from outside-in so that the knot is tied and buried inside the graft material (Fig 3).
Fig 3.
The graft is stitched in a loop fashion about 1 cm from the femoral end with a strong FiberWire suture (No. 2) starting from the central strand in an inside-out fashion, then making a complete loop around the graft, and finally passing from outside-in so that the knot is tied and buried inside the graft material (arrow).
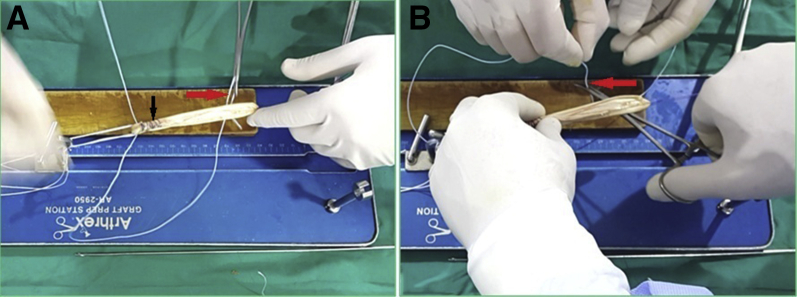
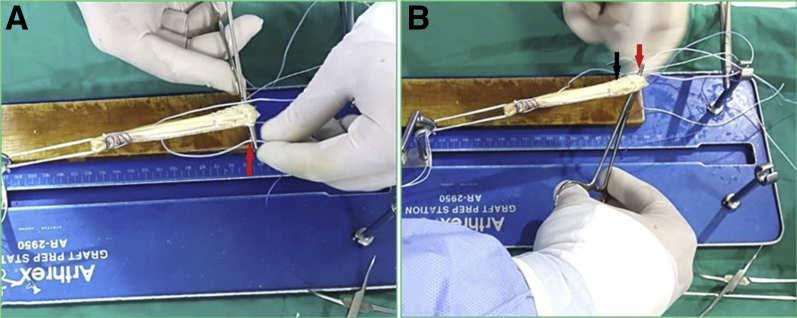
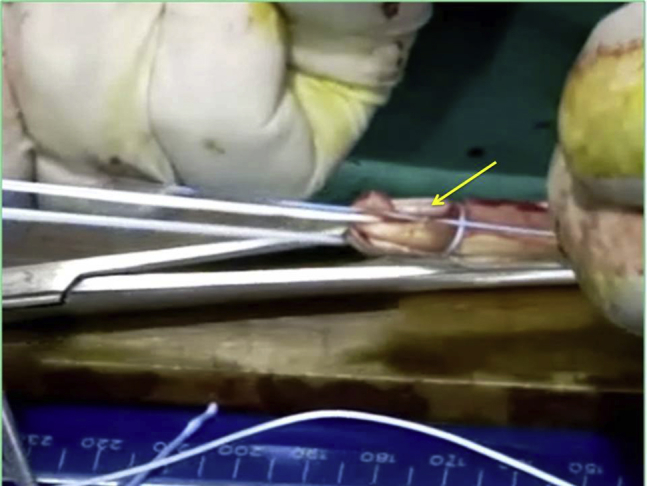
One end of the No. 5 FiberWire (which had been passed through the femoral button) is passed through the graft in the interval between the femoral end and the loop stitch already made about 1 cm from the femoral end to exit on the other side, and the other suture limb is passed from the other side so that they cross each other inside the proximal 1-cm interval of the graft (Fig 4). The same process is repeated, and both suture limbs are passed through the graft from each side to the other, crossing each other in the interval distal to the loop stitch (Fig 5). The process is repeated a third time at the tibial end of the graft. This is aided by a mosquito forceps passed through the whipstitches about 8 to 10 mm from the tibial end to pull 1 suture limb from each side to the other, crossing each other a third time inside the graft (Fig 6).
Fig 4.
One end of the No. 5 FiberWire (which had been passed through the femoral button) is passed through the graft in the interval between the femoral end and the loop stitch already made about 1 cm from the femoral end to exit on the other side (A, arrow), and the other suture limb is passed from the other side (B, arrow) so that they cross each other inside the proximal 1-cm interval of the graft.
Fig 5.
(A, B) Both suture limbs are passed through the graft from each side to the other (red arrows), crossing each other in the interval distal to the loop stitch (black arrow).
Fig 6.
(A, B) A mosquito forceps is passed through the whipstitches about 8 to 10 mm from the tibial end of the graft (black arrow) to pull 1 suture limb from each side to the other (red arrows), crossing each other for a third time inside the graft.
The femoral end of the graft is marked at a distance corresponding to the desired graft length to be placed inside the femoral socket. This is usually 15 to 25 mm according to the available length of the graft.
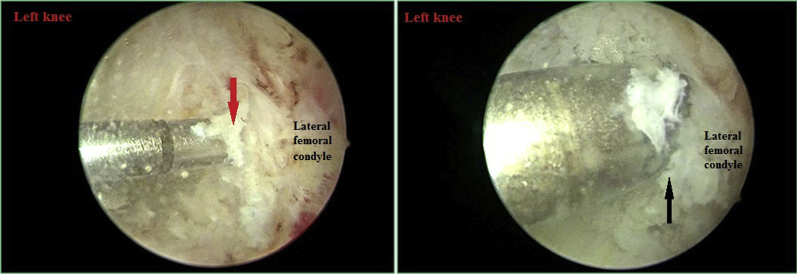
The technique for anatomic single-bundle ACL reconstruction is performed as described before.14 A femoral guide pin aided by a femoral offset guide (Arthrex) is inserted through the deep anteromedial portal and placed at the center of the femoral footprint, resting carefully against the posterior aspect of the lateral femoral condyle. Overdrilling follows with a cannulated femoral reamer corresponding to the measured diameter of the graft and to the desired depth (Fig 7). A looped suture is passed through the femoral tunnel for later traction of the graft.
Fig 7.
A guide pin is drilled at the center of the femoral footprint (red arrow) in the left knee, and after the tunnel length is checked, overdrilling follows with a cannulated femoral reamer corresponding to the measured diameter of the graft and to the desired depth (black arrow).
Next, a tibial guide is used to insert a guide pin in the center of the tibial ACL footprint; the position is checked by performing the impingement test, after which overdrilling is performed.14 The suture loop is retrieved through the tibial tunnel and used to pull the traction passing sutures of the TightRope system through both tunnels from below upward until the sutures, followed by the button itself, exit the lateral femoral cortex; the button is then flipped by countertraction on the graft (Fig 8).
Fig 8.
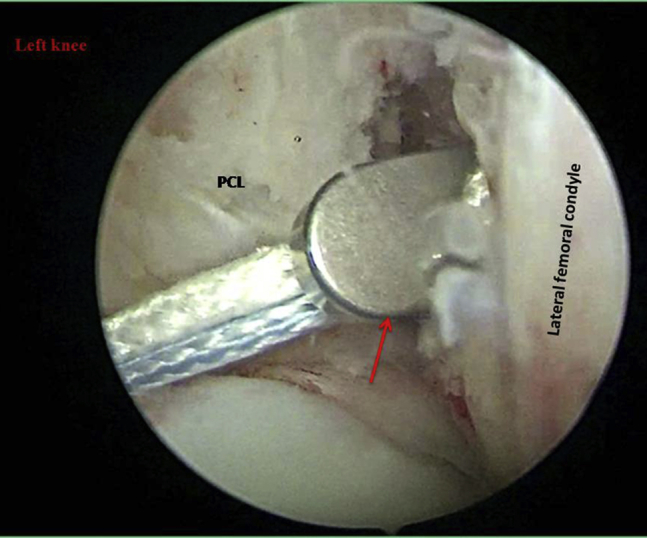
The suture loop is retrieved through the tibial tunnel (left knee) and used to pull the traction passing sutures of the TightRope system through both tunnels (arrow) from below upward until the sutures, followed by the button itself, exit the lateral femoral cortex; the button is then flipped by countertraction on the graft. (PCL, posterior cruciate ligament.)
The shortening white sutures are tightened alternately to pull the graft to fill the femoral socket. The internal suture augmentation is pulled and tensioned carefully downward to ensure that it is not redundant inside the graft after the TightRope loop is tightened. All sutures including the internal suture augmentation are tightened under 80 N of traction while the interference screw is inserted into the tibial tunnel with the knee in 30° of flexion. Arthroscopic confirmation of the graft position and tension in the full range of motion should follow. The ends of the internal suture augmentation are then fixed outside the tibial tunnel orifice. Many options are available including a Bio-SwiveLock (Arthrex), a cortical button, staples, or—as we prefer to use—a 6.5-mm cancellous fully threaded screw with a metal washer (Fig 9). Final tightening of the internal sutures is performed with the knee in full extension to avoid any possible limitation of final extension.
Fig 9.
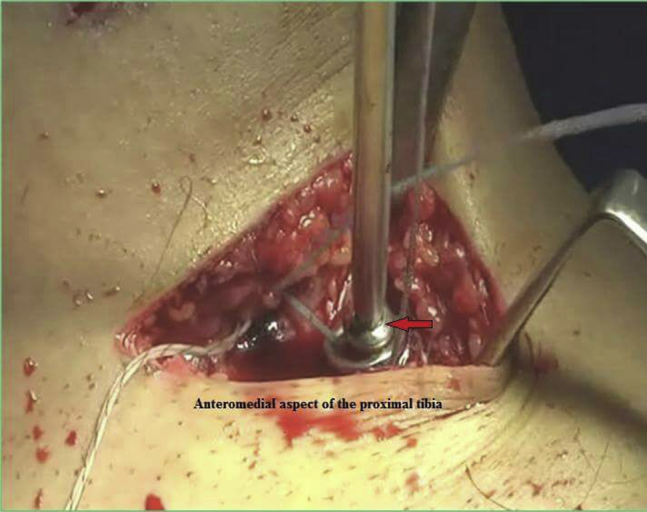
The ends of the internal sutures are fixed outside the tibial tunnel orifice (left knee) using a 6.5-mm cancellous fully threaded screw with a metal washer. The sutures are passed through the hole of the washer and then tied securely around and below it (arrow).
Postoperative Rehabilitation
A hinged knee brace with 0° to 120° extension-flexion range of motion is recommended for a minimum of 3 months. With this technique, immediate weight bearing as tolerated is recommended from the second postoperative day.
Discussion
ACL graft protection from excessive stress during the early postoperative period is essential to prevent postoperative stretching and failure.3 We believe that internally supporting the hamstring tendon graft with the described technique is beneficial to allow an early postoperative rehabilitation program that can also prevent arthrofibrosis and dissatisfaction with the results (Table 1). The technique needs further clinical evaluation to assess the long-term results and the effect of protection of the graft on the actual ligamentization of the graft, as well as the clinical behavior of the resultant collagen fibers. Radiologic evaluation of the tunnels may be beneficial to assess the effect of the internal brace material on the femoral and tibial tunnel diameters.
Table 1.
Advantages and Disadvantages of Internal Suture Augmentation Technique
| Advantages |
| Protection of the ACL graft during the early postoperative period, preventing early failure due to implant failure. |
| Protection of the ACL graft later on, preventing relaxation and stretching of the graft. |
| The technique allows earlier and more secure rehabilitation. |
| The technique is potentially advantageous in professional athletes and patients with a high BMI, as well as patients with osteoporosis. |
| The technique may be of special value in patients with smaller graft diameters because of thin tendons and with no available allograft. |
| Disadvantages |
| There is a potential for stress shielding if the tension of the internal suture augmentation is higher than the tension of the graft; however, this needs further research. |
| The costs are higher than those with the standard technique. |
ACL, anterior cruciate ligament; BMI, body mass index.
An important point that needs further clarification is the effect of reduction of stress on the graft through the internal brace on healing and whether it may cause a phenomenon such as stress shielding (Table 1). This requires laboratory animal clinical and histologic studies. To decrease this potential, we tighten the whipstitch sutures of the tibial end of the graft and the suture of the internal brace at the same time and to the same degree during fixation with the interference screw (Table 2).
Table 2.
Pearls and Pitfalls
| Good and meticulous preparation of the graft is needed so that the sutures are completely buried inside the graft in its intra-articular part, thus reducing potential irritation at the articular surface or synovitis. |
| The 2 ends of the internal sutures should be pulled separately, independent of the graft, after the TightRope is tightened to ensure there are no lax sutures inside the graft material. |
| Over-tightening should be avoided during backup cortical fixation outside the tibial tunnel while the knee is in full extension to avoid any potential limitation of range of motion or pulling the Bio-Interference Screw outside the tibial tunnel. |
Footnotes
The authors report the following potential conflict of interest or source of funding: A.B.I. receives support from Arthrex, Arthrosurface, medi Bayreuth. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Internal suture augmentation technique for anterior cruciate ligament reconstruction graft and method of fixation in both femoral and tibial tunnels. A No. 5 FiberWire suture is used as an internal brace to augment the hamstring tendon autograft. The suture is passed through and suspended on the femoral button proximally. Distally, the suture ends are passed and completely buried within the graft by crossing each other 3 times. The internal augmentation sutures are fixed first with the graft using a Bio-Interference Screw and then with secondary backup cortical fixation (screw and washer).
References
- 1.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Baer G.S., Harner C.D. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26:661–681. doi: 10.1016/j.csm.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Kamath G.V., Redfern J.C., Greis P.E., Burks R.T. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 4.Noyes F.R., Barber-Westin S.D. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131–1143. doi: 10.2106/00004623-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Wright R.W., Huston L.J., Spindler K.P. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979–1986. doi: 10.1177/0363546510378645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harner C.D., Giffin J.R., Dunteman R.C., Annunziata C.C., Friedman M.J. Evaluation and treatment of recurrent instability after anterior cruciate ligament reconstruction. Instr Course Lect. 2001;50:463–474. [PubMed] [Google Scholar]
- 7.Clancy W.G., Jr., Narechania R.G., Rosenberg T.D., Gmeiner J.G., Wisnefske D.D., Lange T.A. Anterior and posterior cruciate ligament reconstruction in rhesus monkeys. J Bone Joint Surg Am. 1981;63:1270–1284. [PubMed] [Google Scholar]
- 8.Drez D.J., Jr., DeLee J., Holden J.P., Arnoczky S., Noyes F.R., Roberts T.S. Anterior cruciate ligament reconstruction using bone-patellar tendon-bone allografts. A biological and biomechanical evaluation in goats. Am J Sports Med. 1991;19:256–263. doi: 10.1177/036354659101900308. [DOI] [PubMed] [Google Scholar]
- 9.Getelman M.H., Friedman M.J. Revision anterior cruciate ligament reconstruction surgery. J Am Acad Orthop Surg. 1999;7:189–198. doi: 10.5435/00124635-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Cook J.L., Smith P., Stannard J.P. A canine arthroscopic anterior cruciate ligament reconstruction model for study of synthetic augmentation of tendon allografts. J Knee Surg. 2017;30:704–711. doi: 10.1055/s-0036-1597618. [DOI] [PubMed] [Google Scholar]
- 11.Mackay G.M., Blyth M.J., Anthony I., Hopper G.P., Ribbans W.J. A review of ligament augmentation with the InternalBrace: The surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239–255. [PubMed] [Google Scholar]
- 12.Smith P.A., Bley J.A. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. doi: 10.1016/j.eats.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nancoo T.J., Lord B., Yasen S.K., Smith J.O., Risebury M.J., Wilson A.J. Transmedial all-inside posterior cruciate ligament reconstruction using a reinforced tibial inlay graft. Arthrosc Tech. 2013;2:e381–e388. doi: 10.1016/j.eats.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feucht M., Hinterwimmer S. ACL reconstruction. In: Imhoff A.B., Feucht M.J., editors. Surgical atlas of sports orthopaedics and sports traumatology. Ed 1. Springer; New York: 2015. pp. 213–220. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Internal suture augmentation technique for anterior cruciate ligament reconstruction graft and method of fixation in both femoral and tibial tunnels. A No. 5 FiberWire suture is used as an internal brace to augment the hamstring tendon autograft. The suture is passed through and suspended on the femoral button proximally. Distally, the suture ends are passed and completely buried within the graft by crossing each other 3 times. The internal augmentation sutures are fixed first with the graft using a Bio-Interference Screw and then with secondary backup cortical fixation (screw and washer).