Abstract
Background:
People who deliberately ingest poisons commonly present to emergency departments of hospitals in India. However, there is a dearth of information on poisoning using nonorganophosphorus pesticides.
Methods:
This prospective, hospital-based study attempted to examine the nonorganophosphorus poisons used to attempt suicide. Data on sociodemographic characteristics of patients, site and source of poisons, co-ingested substances, premeditation, and reason for poisoning were collected. A multinomial logistic regression was performed to determine association between poison class and these exposure characteristics.
Results:
Three hundred and forty-one cases of attempted suicide presented during the 6-month period (1.7% of all emergency room admissions). The majority was predominantly male and was young adults. Poisoning was the most common mode (91.7%), followed by hanging (7.3%) and self-injury (3, 0.9%). Pesticides (44.3%) including organophosphates (25.5%) were the predominant poisons, followed by pharmaceuticals (27.9%), caustics/chemicals (12.0%), and plant poisons (7.0%). One hundred and nine were available for prospective interview as the others who presented were not detained for prolonged observation the emergency department. Most patients who ingested such poisons were women, from rural backgrounds and were educated. The majority sourced the poisons from home, consumed poison at home, and mixed the poison with water; these attempts were impulsive and seemed to be in response to relationship conflicts. In the multivariate analysis, education (P = 0.08) and poison source (outside the home) were significant predictors of pesticide ingestion.
Conclusions:
Suicidal poisoning results from a complex synthesis of socioeconomic and psychological factors; certain patterns of poisoning are likely to be more prevalent in demographic niche groups.
Keywords: Nonorganophosphate, poisoning, suicide
INTRODUCTION
Suicide and deliberate self-harm are major public health problems, particularly in low-income and middle-income countries.[1] Reports on suicide in the developing countries suggest that the act is poorly contemplated with the choice of agent determined impulsively. Availability rather than lethality of poison determines the agent chosen.[2] Moreover, major psychopathology is often absent in people who kill themselves.[3] While certain poisons, such as organophosphate poisonings in farmers, are well reported,[4] the multitude of other poisonings encountered and the socioenvironmental characteristics around their use is unknown. This study describes the sociodemographic characteristics, the setting of the suicide attempt, choice of poison, co-ingested substances, planning and premedication of people who presented to the emergency department of a tertiary hospital with nonorganophosphorus poisoning.
METHODS
Site and duration
This study was performed a tertiary referral hospital in Tamil Nadu, South India, serving a mixed rural/urban population (approximately 1,000,000 people, over a 100 km radius). The hospital has a 24-h emergency department, which manages a wide variety of serious illnesses.
Method of patient selection
A once daily cross-sectional screening of the inpatients in the emergency ward was performed, and patients satisfying the following criteria were included: (i) suicidal poisoning with nonorganophosphorus poison, (ii) above 16 years, and (iii) attended hospital within 4 days of ingestion. Informed consent was obtained. Patients and their relatives were interviewed in detail using a semi-structured pro forma to collect the following information: (i) Sociodemographic characteristics, (ii) social, occupational, and environmental characteristics, (iii) the motives and circumstances of the poisoning event, and (iv) the nature of the ingested poison.
Analysis
Mean and standard deviation were used to describe continuous variables, while frequency and percentages were obtained for categorical data. ANOVA and Chi-square test were employed to test the statistical significance of bivariate associations.
To identify factors determining the type of poison class chosen, a multinomial logistic regression was performed with the patient characteristics as risk factors for poison class chosen. Caustics were chosen as the reference group, to which pesticides and pharmaceuticals were compared respectively. The risk attributable to a patient characteristic toward a poison choice was calculated. Those with P ≤ 0.10 were included in the multivariate analysis. Mixed poisonings involving two or more groups were excluded from the analysis. The Institutional Review Board (IRB) approved the study protocol [IRB no. 7209].
RESULTS
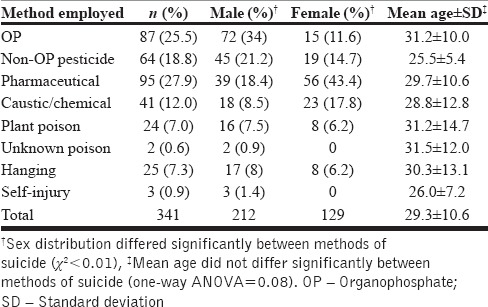
During the 6-month study, there were 341 patients with suicide attempts presented to the emergency department. This represented 1.7% of the total number of patient seen (n = 19,946). The sociodemographic details of patients who presented with attempted suicide are documented in Table 1. The majority was males and was young adults. Poisoning was the commonest mode (91.7%), followed by hanging (7.3%) and self-injury (3, 0.9%). Pesticides (44.3%) including organophosphates (25.5%) were the predominant poisons, followed by pharmaceuticals (27.9%), caustics/chemicals (12.0%), and plant poisons (7.0%). Pesticide, plant poisons, and hangings saw a statistically significant male predominance while females were more common among pharmaceutical and caustic/chemical poisons. Age did not differ significantly between groups.
Table 1.
Description and comparative analysis of the total sample (n=341)
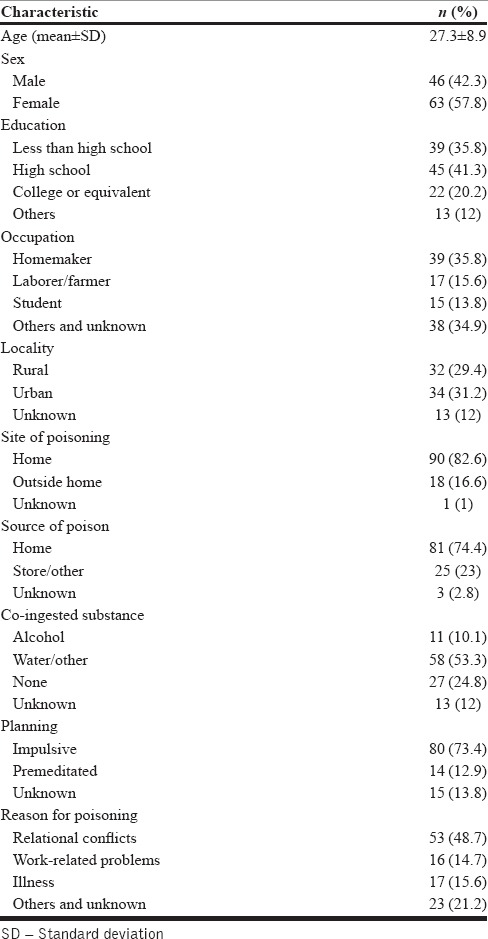
Two hundred patients ingested nonorganophosphate pesticide, corrosive, and pharmaceutical poisons. One hundred and nine were available for prospective interview by the once-daily sampling methodology; others had been discharged/referred based on the clinical judgment of the medical officers and were not available for interview in the emergency ward. The patients who were discharged did not differ from those who were detained regarding the overall poison class distribution (333,919 vs. 315,622, P = 0.424) and in the age distribution (P = 0.158). However, there were more females among those present and interviewed at emergency department, who belonged predominantly to the pharmaceutical and corrosive groups (64.3% vs. 35.7%, P = 0.006). The most commonly encountered poison in those was as follows: (1) Nonorganophosphate pesticide group - pyrethroids (n = 12, 38.7%), endosulfan (n = 3, 9.7%), rodenticides (including phosphides and superwarfarins, n = 4, 12.9%), carbamates (n = 1, 3.4%), with unknown insecticides being 7 (22.6%). (2) Pharmaceuticals: Paracetamol (n = 11, 19.6%), antipsychotics (n = 9.13, 1%), hypnotics (including benzodiazepines, n = 8, 14.3%), antihistamine (n = 58, 9%), antiepileptic (n = 4, 4.2%), oral hypoglycemic agents (n = 3, 5.4%), and antidepressants (n = 3, 5.4%). (3) Caustics/chemical poisons: Inorganic acid (n = 9, 40.9%), phenol (4, 18.2%), ammonium compounds (3, 13.6%), vasmol hair dye (n = 2, 9.1%), and organic solvents (n = 2, 9.1%). Most patients were from rural backgrounds and were educated [Table 2]. The majority sourced the poisons from home, consumed poison at home, and mixed the poison with water. Most these attempts were impulsive and seemed to be in response to relationship conflicts.
Table 2.
Sociodemographic and details of poisoning (n=109)
In the bivariate analysis, differences among the various classes of poisons were as follows: males were 4.5 times as likely consume pesticide than chemicals (P = 0.010). Those with college education were 90% less likely to be poisoned by pesticide than with caustics (P = 0.015). Pesticides were 90% more likely to be obtained from outside the home (P = 0.010). Pharmaceuticals were 6.6 times more likely to be co-ingested with water (0.036). Students were 90% more likely to consume caustics than pharmaceuticals (P = 0.014). Comorbid medical illnesses showed a nonsignificant increased risk of pharmaceutical poisonings by 8.5 times (P = 0.071). The following associations did not differ statistically among the classes of poisoning: Age, locality (rural vs. urban), poisoning site (home vs. outside), impulsivity, reason for poisoning [Table 3].
Table 3.
Multinomial logistic regression analysis of detailed sample (n=107, 2 mixed poisons excluded)
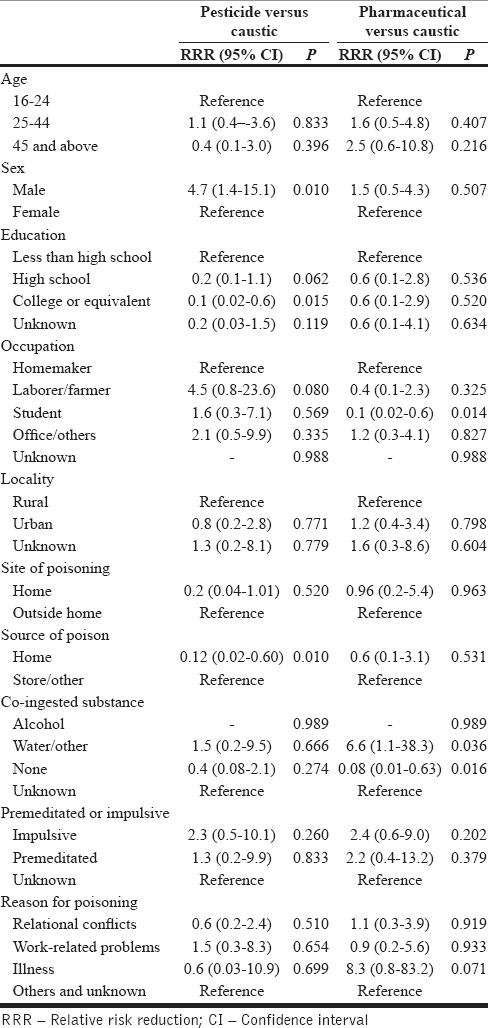
In the multivariate analysis, low education (relative risk [RR] = 0.36, 95% confidence interval [CI]: -0.16 to 0.76, P = 0.008) and poisoning outside the home (RR = 0.11, 95% CI: −0.14 to 0.81, P = 0.03) were significant predictors of pesticide usage (over caustics).
DISCUSSION
The significance of this study is the fact that it focuses on nonorganophosphorus poisons. While nonorganophosphorus poisons are commonly used for attempted suicide, they are much less often studied in detail compared to organophosphorus poisons.
Suicide is a complex phenomenon determined by heterogeneous factors affecting individuals and populations.[5] Using the Haddon matrix model, an interplay of host, agent, and environmental factors is described as determinants of completed suicide. Host factors include psychopathology, substance abuse, and chronic medical comorbidity. Agent factors include the potency and dosage of the poison, and environmental factors include social, economic pressures and healthcare availability.[6]
In the developing world, suicide prevalence is disparately higher than in the West; verbal autopsies report rates of 158/1000 in South India,[7] seventy times higher than the UK average in 1998;[8] one-fourth of deaths in the 20–30 age group and up to 67% of female deaths are suicides.[7] A single factor such as socioeconomic disadvantage cannot account for this, as suicide rates vary among regions with equal human development index.[9] While certain risk factors, such as severe psychopathology,[10] unemployment,[11] medical comorbidities[12] and deprivation of social privileges,[13] are pervasive, and improvement in suicide rates occurs after these are remedied,[14] certain host, agent, and environmental factors are peculiar to the developing world. Poor education and economic disadvantage are among these while certain methods of suicide, such as hanging and poisoning with pesticides, being common in the developing world,[7,15] are uncommon in the West.[8] A previous community-based survey of this geographical population had shown a variation in suicide method according to the age and demographic factors; while poisoning and hanging were the commonest methods, women often chose drowning or burning while men more often chose poisoning or hanging. People younger than 44 years used poison while older people tended to choose hanging.[16]
In this context, the findings of the present hospital-based survey of suicide show that males were at higher risk for pesticide poisonings, whereas women were comparatively more prone to caustic/chemicals poisons. Pesticide poisons were obtained from outside the home. College education or beyond was 90% less likely to consume pesticides. Those identifying as students were more 90% more likely to attempt caustic/chemical poisons than homemakers. Poorer education emerged as a significant risk factor for pesticide poisoning. This pattern may suggest the choice of poison reflects proximity and immediate availability during periods of vulnerability. In agricultural societies, males typically work at the field during daytime, whereas women care for the home. Therefore, the choice of pesticides among men and drugs/chemicals among women may be explained by occupational proximity. The reason for preference of caustics among students is less clear. One possibility is the increased exposure and conditioning by mass media influences such as movies and television serials upon this group, which dramatize morbid suicide methods.
Poorer education emerged as the significant risk factor for pesticide usage on multivariate analysis. Low education is a discriminative factor between the developed and developing world and can be linked to multiple direct and indirect stressors for suicide. Indirect stressors would include economic disadvantage, unemployment, poor opportunity for expression and redressal of grievances, and poor healthcare access. More direct risks would arise from lack of awareness of the dangers of pesticide poisons and their correct storage and use. Since pharmaceuticals poisonings are reportedly less lethal than pesticides,[17] it seems that the least educationally privileged is also vulnerable to severest of suicidal implements.
Pesticide poisons accounted for 30% of suicidal deaths globally in 2007[18] and for the majority of suicidal hospital emergency admissions in developing countries.[19,20] The West, despite having higher volume of pesticide sales, had several-fold lower pesticide mortality rates than in the developing world,[18] suggesting unsafe usage, and increased toxicity of the agents employed in the developing world. Consuming pesticide is a response to a stressful event, as a directed personal message or situational manipulation for advantage rather than actual desire to end life.[21] Relationship conflict, domestic abuse, and alcoholism are the common precipitants.[21] Introduction of a minimum pesticide list[22] and banning unethical distribution of toxic poisons[23] has reduced the prevalence of suicidal death by pesticides in Sri Lanka.[24]
Measures to target suicide would therefore require both population scale macroeconomic interventions, such as education, provision of basic human needs, and community-based psychosocial interventions for social support, as well as targeted interventions aimed at vulnerable populations, such as restriction of pesticide availability among rural centers with a minimum pesticides list, and restricting media influences that voyeuristically portray suicide.[5]
The generalization of the results of this hospital-based investigation to the community would necessarily require caution. In patriarchal societies like India, men are more often brought to hospital early in the course of their illness when compared with women. Consequently, the duration of stay in the emergency room will affect recruitment of patients. More women, especially among corrosive and pharmaceutical poisons, were detained in the emergency room than nonorganophosphate pesticides thereby increasing their numbers in the sample. Another possible reason for early discharge among patients who ingest pesticides may be the presence of a biomarker of nonseverity, like normal serum butyrylcholinesterase levels for pesticides, which may selectively facilitate early release from the emergency room among this group.
CONCLUSIONS
Suicidal poisoning death results from a synthesis of host, agent and environmental factors, including as education and poison availability. Certain patterns of poisoning are more prevalent in demographic niche groups, being contingent on these. Addressing suicide requires both population scale and individualized measures.
Financial support and sponsorship
From Research Grant, Christian Medical College, Vellore, Tamil Nadu, India.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jacob KS. Suicide prevention in low-income and middle-income countries: Part perceptions, partial solutions. Br J Psychiatry. 2017 doi: 10.1192/bjp.bp.117.198150. InPress. [DOI] [PubMed] [Google Scholar]
- 2.Eddleston M, Karunaratne A, Weerakoon M, Kumarasinghe S, Rajapakshe M, Sheriff MH, et al. Choice of poison for intentional self-poisoning in rural Sri Lanka. Clin Toxicol (Phila) 2006;44:283–6. doi: 10.1080/15563650600584444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manoranjitham SD, Rajkumar AP, Thangadurai P, Prasad J, Jayakaran R, Jacob KS. Risk factors for suicide in rural South India. Br J Psychiatry. 2010;196:26–30. doi: 10.1192/bjp.bp.108.063347. [DOI] [PubMed] [Google Scholar]
- 4.Sainath P, The Hindu. The Hindu. Nearly 2 lakh farm suicides since 1997. Jan 22, 2010 00:23 IST Updated: Dec 17, 2016 03:22 IST [Google Scholar]
- 5.Jacob KS. The prevention of suicide in India and the developing world: The need for population-based strategies. Crisis. 2008;29:102–6. doi: 10.1027/0227-5910.29.2.102. [DOI] [PubMed] [Google Scholar]
- 6.Eddleston M, Buckley NA, Gunnell D, Dawson AH, Konradsen F. Identification of strategies to prevent death after pesticide self-poisoning using a Haddon matrix. Inj Prev. 2006;12:333–7. doi: 10.1136/ip.2006.012641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aaron R, Joseph A, Abraham S, Muliyil J, George K, Prasad J, et al. Suicides in young people in rural Southern India. Lancet. 2004;363:1117–8. doi: 10.1016/S0140-6736(04)15896-0. [DOI] [PubMed] [Google Scholar]
- 8.McClure GM. Suicide in children and adolescents in England and Wales 1970-1998. Br J Psychiatry. 2001;178:469–74. doi: 10.1192/bjp.178.5.469. [DOI] [PubMed] [Google Scholar]
- 9.Vijayakumar L, Nagaraj K, Pirkis J, Whiteford H. Suicide in developing countries (1): Frequency, distribution, and association with socioeconomic indicators. Crisis. 2005;26:104–11. doi: 10.1027/0227-5910.26.3.104. [DOI] [PubMed] [Google Scholar]
- 10.Vijayakumar L, Rajkumar S. Are risk factors for suicide universal. A case-control study in India? Acta Psychiatr Scand. 1999;99:407–11. doi: 10.1111/j.1600-0447.1999.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 11.Blakely TA, Collings SC, Atkinson J. Unemployment and suicide. Evidence for a causal association? J Epidemiol Community Health. 2003;57:594–600. doi: 10.1136/jech.57.8.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris EC, Barraclough BM. Suicide as an outcome for medical disorders. Medicine (Baltimore) 1994;73:281–96. doi: 10.1097/00005792-199411000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Värnik A, Kõlves K, Wasserman D. Suicide among Russians in Estonia: Database study before and after independence. BMJ. 2005;330:176–7. doi: 10.1136/bmj.38328.454294.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pritchard C, Hansen L. Comparison of suicide in people aged 65-74 and 75+ by gender in England and Wales and the major Western countries 1979-1999. Int J Geriatr Psychiatry. 2005;20:17–25. doi: 10.1002/gps.1213. [DOI] [PubMed] [Google Scholar]
- 15.Abraham VJ, Abraham S, Jacob KS. Suicide in the elderly in Kaniyambadi block, Tamil Nadu, South India. Int J Geriatr Psychiatry. 2005;20:953–5. doi: 10.1002/gps.1385. [DOI] [PubMed] [Google Scholar]
- 16.Joseph A, Abraham S, Muliyil JP, George K, Prasad J, Minz S, et al. Evaluation of suicide rates in rural India using verbal autopsies, 1994-9. BMJ. 2003;326:1121–2. doi: 10.1136/bmj.326.7399.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henderson A, Wright M, Pond SM. Experience with 732 acute overdose patients admitted to an Intensive Care Unit over six years. Med J Aust. 1993;158:28–30. doi: 10.5694/j.1326-5377.1993.tb121644.x. [DOI] [PubMed] [Google Scholar]
- 18.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: Systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gargi J, Rai H, Chanana A, Rai G, Sharma G, Bagga IJ. Current trend of poisoning – A hospital profile. J Indian Med Assoc. 2006;104:72–3, 94. [PubMed] [Google Scholar]
- 20.Singh B, Unnikrishnan B. A profile of acute poisoning at Mangalore (South India) J Clin Forensic Med. 2006;13:112–6. doi: 10.1016/j.jcfm.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Konradsen F, Hoek W, Peiris P. Reaching for the bottle of pesticide – A cry for help. Self-inflicted poisonings in Sri Lanka. Soc Sci Med. 2006;62:1710–9. doi: 10.1016/j.socscimed.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 22.Eddleston M, Karalliedde L, Buckley N, Fernando R, Hutchinson G, Isbister G, et al. Pesticide poisoning in the developing world – A minimum pesticides list. Lancet. 2002;360:1163–7. doi: 10.1016/s0140-6736(02)11204-9. [DOI] [PubMed] [Google Scholar]
- 23.Jayasinghe S, de Silva D. Minimum pesticide list for the developing world. Lancet. 2003;361:259. doi: 10.1016/S0140-6736(03)12291-X. [DOI] [PubMed] [Google Scholar]
- 24.Gunnell D, Fernando R, Hewagama M, Priyangika WD, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol. 2007;36:1235–42. doi: 10.1093/ije/dym164. [DOI] [PMC free article] [PubMed] [Google Scholar]


