Abstract
Background and Objectives:
Patients with bipolar disorder (BD), despite recovering symptomatically, suffer from several functional impairments even in remission. The actual causes of impaired functioning are less known.
Materials and Methods:
The study aimed to examine the clinical and psychosocial determinants of functioning in patients with BD in remission. A cross-sectional single-group design was adopted (n = 150). Participants meeting the study criteria were screened with Mini-International Neuropsychiatric Interview Scale. The selected participants were administered various tools to assess the level of functioning and the clinical, psychosocial determinants of functioning.
Results:
The clinical characteristics of the sample included early age of onset of illness, presence of precipitating factors, fewer episodes, minimal comorbidities, history of psychotic episodes, family history of mental illness, good medication adherence, and low depression and mania scores. Psychosocial factors included higher stress and moderate social support and self-esteem in the sample. Poor functioning patients had a history of longer hospital stay and had greater scores on depression, mania, stress, and maladaptive coping styles than better functioning patients.
Conclusion:
Higher depression, mania, stress, and maladaptive coping strategies were related to poor functioning, while higher medication adherence, self-esteem, and social support were related to better functioning.
Keywords: Bipolar disorder in remission, clinical factors, functioning, psychosocial factors
INTRODUCTION
Bipolar disorder (BD) is a subtype of mood disorder, which is episodic, recurrent and causes significant disability.[1] It is estimated that 8.7 million people suffer from BD in India alone.[2] Poor recovery, risk for relapse, and disability characterize the longitudinal course of BD.[3] Contradicting earlier beliefs that individuals with BD were not symptomatic during their interepisodic period and had better functioning, recent studies have found its negative impact on functioning. The World Health Report (2001) considers BD as one of the ten major causes of functional impairment worldwide. Even though BD has generally been regarded as having a better prognosis than schizophrenia, a significant proportion of patients with BD show continual symptoms despite being remitted. Moreover, most individuals with BD are symptomatic, a significant part of their lifetime even after receiving adequate medication.[4] In fact, those who recover from clinical symptoms also face difficulties in functioning and find it difficult to attain their premorbid functioning.
Despite the gap between clinical and functional recovery, the factors that play a role in the functioning of BD were seldom studied. Psychological and social factors in patients with BD have altogether been less thought of, when compared to psychosis. Most patients with BD show only a partial clinical improvement during their interepisodic period as the residuals’ symptoms still persist although it may not amount to a diagnosable episode.[4,5] Research has also demonstrated functional impairment in several individuals with BD, who had recovered clinically with a lot of them, experiencing social and relational difficulties, as well as significant problems in occupational roles.[6,7,8]
The influencing factors that affect the functional outcome in BD differ from study to study and have been hard to replicate, because of varied methodologies and measures used. Several factors associated with low functioning are presented in the western literature; however, in India, such studies are rarely found. Still in the population of India where a vast majority struggles with disability, functioning of patients with BD has not been broadly studied as compared with studies targeting patients with schizophrenia. There is a dire need to look into the various clinical and psychosocial factors affecting the interepisodic functioning in Indian sample of remitted patients with BD. These factors can be incorporated in the psychological treatment of patients with BD so as to improve their psychosocial functioning during their remission phase.
MATERIALS AND METHODS
The aim of the study was to examine the clinical and psychosocial determinants of functioning in patients with BD in remission. The study was carried out at National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru, India. The study participants were 150 patients who met the International Classification of Diseases, Tenth Revision (ICD-10) criteria (F: 31.7) for BD in remission. They were recruited by convenient sampling from the psychiatric outpatient services of NIMHANS over a period of 12 months. Ethical clearance was obtained from the Institutional Ethics Committee. Before participation, all participants provided written informed consent in accordance with NIMHANS-I-approved consenting procedures. Diagnoses of participants with BD were determined using Mini-International Neuropsychiatric Interview (MINI)-6.0.[9] Participants with BD were included in the study if they (a) had low residual depressive symptoms (score of ≤7 in Hamilton Depression Rating Scale [HDRS]), (b) had low residual manic symptoms (score of ≤7 on Young Mania Rating Scale [YMRS]), (c) did not have an episode of a ICD-10 major depression and/or ICD-10 hypomania or mania in the 6 months preceding the study, (d) were on a stable dose of medication, (e) in the age range between 18 and 50 years, and (f) could read either English, Malayalam, Hindi, or Kannada language. The participants were excluded if they had (a) a history of organic or neurological illness, (b) primary diagnosis of unipolar disorder and other psychotic disorders, and (c) BD with mental retardation.
To recruit patients for the study, 258 patients from the psychiatric outpatient services with a diagnosis of BD in remission were contacted; 204 met the inclusion and exclusion criteria, of which 168 patients gave written informed consent for participation in the study. After screening using MINI, a clinically representative sample of 150 patients diagnosed with BD in remission was selected for the study. The clinical determinants of functioning were assessed using the Sociodemographic Sheet, Clinical Data Sheet, Brief Adherence Rating Scale (BARS),[10] YMRS,[11] and HDRS.[12] Brief Cope (BC),[13] Perceived Stress Scale,[14] Multidimensional Scale for Social Support,[48] and Rosenberg Self-Esteem Scale (RSES)[15] were used for assessing the psychosocial determinants.
Measurement of functioning
The Functioning Assessment Short Test (FAST) was used to measure their functioning. It was designed for ongoing assessment of functioning, especially in patients with BD.[16] The scale measures six specific areas of functioning: autonomy, occupational functioning, cognitive functioning, financial issues, interpersonal relationships, and leisure time. The scale was administered by an interviewer on patients, and their responses were corroborated with the caregivers. The studied time frame refers to the last 15 days before assessment. The total score across all domains is measured; higher the scores, poorer the functioning. The scale had high internal consistency with a Cronbach's alpha of 0.91.
Statistical analyses were performed using Statistical Package for the Social Sciences Version 16.0 software (Armonk, NY: IBM Corporation, NY, USA). The obtained data were analyzed using descriptive statistics such as frequency, percentage, mean, standard deviation, and cross-tabulation. Parametric statistics such as Student's t-test and nonparametric statistics such as Chi-square test were used to compare subgroups on variables being studied. Pearson's correlation coefficient was used to find the relationship between various variables. Stepwise linear regression analysis was carried out to determine variables that better predict the functioning of remitted patients with BD.
RESULTS
Mean age of the sample was 33 years. Their average number of episodes was around five, and the mean age of onset of illness was 22 years. Almost half of the sample was in the age group of 18–30 years (47%), followed by the age group of 31–40 years (31%). Representation of males was higher (64%) than females (36%). Majority were from Hindu (47%) and Muslim (41%) religious backgrounds. More than half of them were married (55%). One-third was graduates (33%) while 27% had only primary education. Majority were working full time (43%) and were from nuclear families (85%). Almost half of the patients were living with their spouse (47%), 46% of the patients were living with their parents, and 7% were staying alone.
The clinical characteristics of the sample (n = 150)
Half of the samples (51%) had onset of BD when they were between 10 and 20 years, while only 3% had a late onset between 41 and 50 years. Majority (67%) had a psychotic episode at least once during their illness. About half (53%) of the sample had their last episode within the last 6–12 months. Comorbid conditions were minimal in the sample. Substance use and abuse was the most prevalent comorbidity (9%), followed by other anxiety disorders (6%) and obsessive–compulsive disorder in remission (4%). Majority did not have family history of mental illness (60%). Precipitating factors were present in almost half of the cases (46%), while current stressors were absent in most of the cases (80%). Majority had not undergone psychotherapeutic intervention (92%), but most of them had responded to pharmacological treatment (85%).
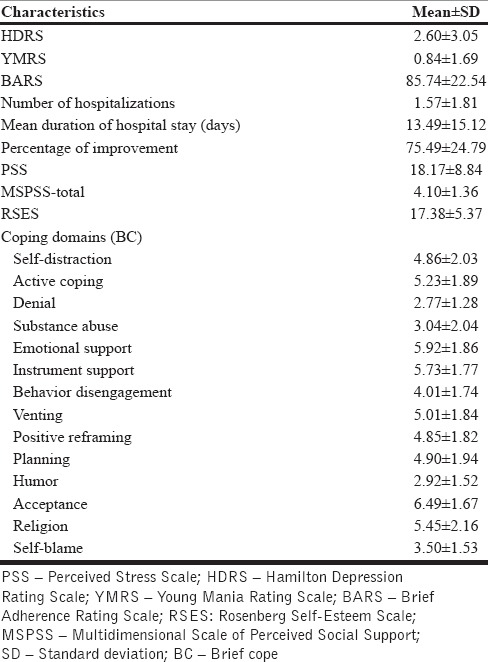
From Table 1, we can see that the mean depression and mania scores of the patients were within the normal range. Majority of the patients were adherent to medication (proportion of doses) in the past month, and the mean duration of hospital stays was around 2 weeks. The mean scores for the stress, coping domains, social support, and self-esteem are given in Table 1.
Table 1.
Mean and standard deviation scores of the sample on clinical and psychosocial characteristics (n=150)
Functioning of patients with bipolar disorder
Functioning was measured using FAST. The mean global functioning score was 20.71 ± 16.79. The authors of FAST scale suggested a cutoff point of ≥11 in subjects with BD as a measure of disability.[17] Based on the cutoff in FAST, 96 (64%) patients had a FAST score more than or equal to 11 indicating disability/poor functioning and 54 (36%) patients had scores below 11 indicating better functioning. More number of males had experienced poor functioning compared to females even though majority of both groups had poor functioning. Regardless of occupational status, most of the patients experienced poor functioning. Marital status and current living arrangements also did not show any role in functioning as both groups had majority of poor functioning patients.
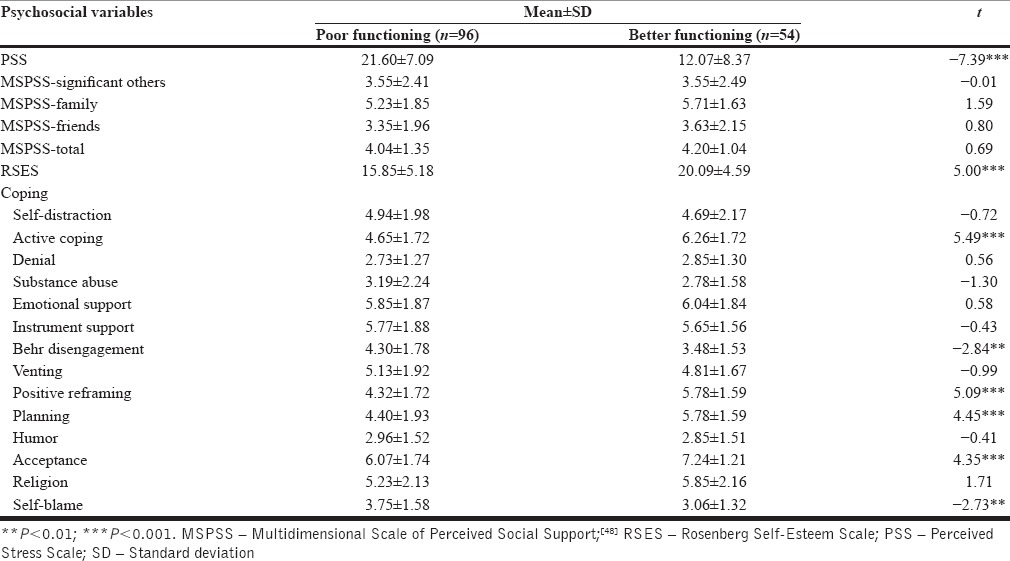
There was significant difference between the better and poor functioning groups on clinical variables. The poor functioning group had significantly higher scores in mean duration of hospital stay, HDRS, and YMRS scores [Table 2]. The better functioning group perceived more improvement (cross-sectionally). With respect to stress and self-esteem, poor functioning group reported more stress while better functioning group had higher self-esteem. Better functioning group had used more healthy coping strategies as compared to poor functioning group [Table 3].
Table 2.
Mean and standard deviation of clinical variables of the sample based on functioning
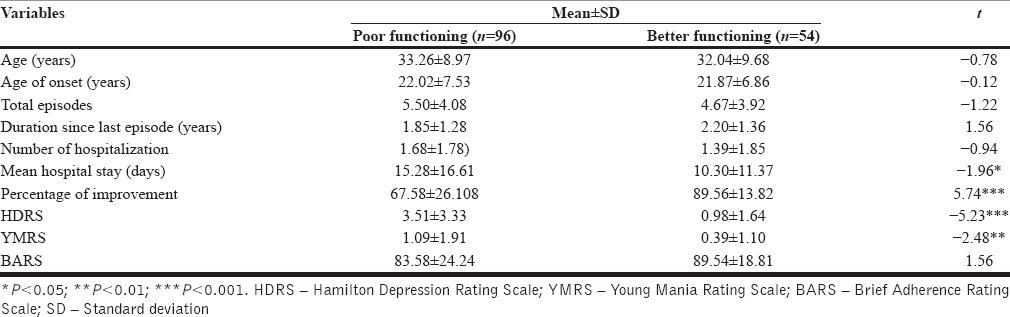
Table 3.
Mean and standard deviation of psychosocial variables of the sample based on functioning
Relationship between functioning and other variables
Correlation of FAST scores with clinical and psychosocial variables [Table 4] shows that Global FAST scores (poor functioning) were positively correlated with depression and mania scores. Further, poor functioning in financial and interpersonal domains of FAST was positively correlated with mania and depression. Stress had a positive correlation with all FAST domains, while perceived percentage of improvement was negatively correlated with all domains of FAST. Negative correlation was seen between functioning in financial and interpersonal domains and medication adherence, duration since the last episode, and prior psychotic episode. Social support from family was negatively correlated with FAST domains: occupational functioning and leisure, while social support from friends had negative correlation with leisure domain. Self-esteem had a significant negative correlation with the FAST Global score and all its domains.
Table 4.
Correlation of Functioning Assessment Short Test scores with clinical and psychosocial variables (n=150)
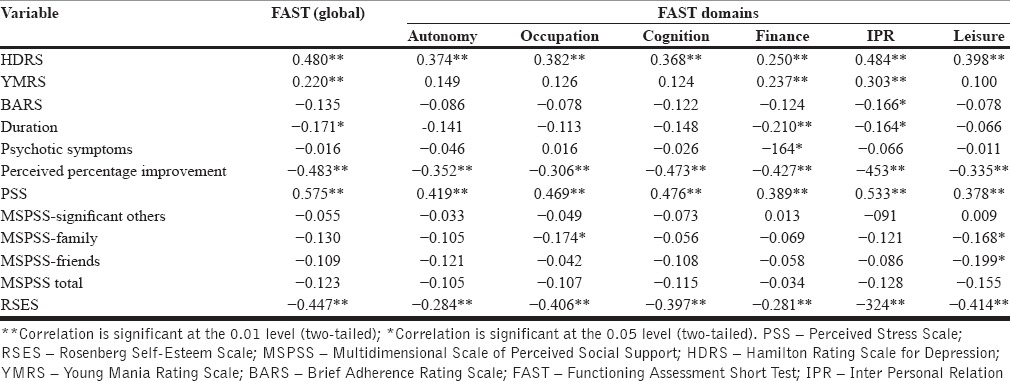
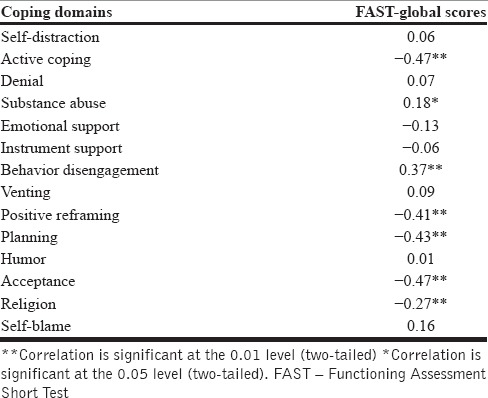
Table 5 shows that the poor functioning was significantly positively correlated with coping strategies such as behavior disengagement and substance abuse. The poor functioning was significantly negatively correlated with religion, positive reframing, planning, acceptance, and active coping strategies.
Table 5.
Correlation of global functioning with coping domains in the sample
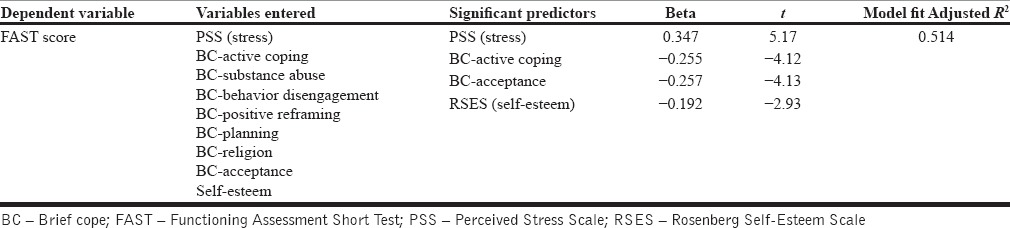
Predictors of functioning in patients with bipolar disorder
To determine the relative contribution of the variables that influence functioning, perceived stress, BC domains, and RSES scores were entered for the analysis as the independent variable and FAST score was taken as the dependent variable [Table 6]. Stepwise forward regression analysis found that stress, active coping, acceptance coping, and self-esteem accounted for a total of 51.4% of variance. Stress alone predicted 33%, active coping 11.5%, acceptance coping explained 5.4%, and self-esteem 2.8% of variance in functioning.
Table 6.
Stepwise (forward) linear regression analysis (n=150)
DISCUSSION
The study aimed to examine the interepisodic functioning of patients with BD. The impairment in functioning was greater in this study when compared to previous studies done in the West.[18] More than half of the sample had impaired functioning regardless of their occupational status. The earlier age of onset of illness in this sample, previous psychotic episodes, comorbidities, and subsyndromal symptoms might have contributed to the impaired functioning of patients in the study.
Clinical variables of the sample based on functioning
The study highlighted that patients who had longer hospital stay tend to have poorer functioning [Table 2]. This could be because such patients might have had more severe symptoms or were difficult to stabilize on treatment or due to severe cognitive deficits as also seen in previous studies.[19,20] Association of illness severity with cognitive impairment in BD could be due to allostatic overload described by Kapczinski et al., where greater stress can lead to more severe neurological damage and cognitive decline.[21] In this study, it could be possible that patients who required a longer hospital stay might have experienced a more stressful mood episode or greater acute allostatic load. Tohen et al. also found the association between functional recovery and shorter hospitalization.[7] Hence, we can understand that in Indian sample also, poor functioning is associated with longer hospital stay.
Poor functioning group also had significantly higher mean scores in HDRS and YMRS. This could be attributed to the subsyndromal symptoms which could affect their functioning. This is consistent with several studies done in the West.[22,23,24] Ozer et al. reported that the number of previous depressive episodes and the duration of hospitalization as well as the current subthreshold depressive and manic symptoms predicted overall functioning.[19]
Psychosocial variables of the sample based on functioning
The present study has come up with a newer understanding about the association between functioning and self-esteem. Most of the previous studies have examined self-esteem during an affective episode rather than during remission.[25,26] Meta-analysis by Nilsson et al. also revealed that the self-esteem of remitted BD patients was significantly lower than that of normal controls while significantly higher than that of remitted major depressive episode patients.[27] However, the studies could identify the association between self-esteem and functioning, while in this study, the association between higher self-esteem and better functioning was clearly depicted.
The study also points out that stress plays a major role in impaired functioning. This may be explained by the neurodegenerative hypothesis which holds that chronic mood instability produces physiological stress with neurotoxic effects, leading to neurological damage and cognitive decline over the course of illness. While most of the literature had focused on stress as a factor leading to onset and relapse of BDs, only few studies on remitted patients have shown consistent results.[28,29] How an individual manages stress can determine the effects of the stressor and ultimately affect their functioning.[30] Lam and Wong reported that functioning of BD patients in various areas of life was highly related to how well they coped with the prodromes of mania.[31] Better functioning group had better scores on active coping, positive reframing, planning, and acceptance coping dimensions. Adaptive coping was found to be an effective coping style in improving mood and self-esteem; thus, adaptive coping strategies were found to improve functioning.[32,33]
In the study, poor functioning group had adopted maladaptive coping strategies such as disengagement and self-blame. Disengagement coping item focuses on giving up hope, which may prevent the individual from doing something to change the way of approaching a stressor and they may develop learned helplessness which can increase affective symptoms and reduce functioning. Self-blame items involved criticizing and blaming oneself for things that happened. This could lead to guilty feeling and finally might end up in relapse. We have seen that poor functioning patients had more subsyndromal symptoms and subsyndromal depression also could increase hopelessness and self-blame making it difficult to concentrate and cope with life. They may withdraw socially and may feel suicidal. Thus, both disengagement and self-blame can cause and maintain poor functioning in the remitted patients. Studies on coping in remitted patients with BDs were seldom found. Thus, the results from this study would help plan treatment strategies for patients with BD in Indian population to achieve full recovery and prevent relapse.
The relationship between the clinical and psychosocial factors in determining functioning of patients with BD shows that greater scores in depression (HDRS Scores) was positively correlated to poorer functioning as a whole and specifically to functioning domains such as autonomy, occupational functioning, cognitive functioning, financial functioning, interpersonal relations, and leisure. Although the criteria for remission were very restrictive (HDRS <7; YMRS <7), higher HDRS scores had a negative impact on overall functioning. A wide search of the literature published from 1980 to December 2007 revealed that, even after the acute phase of the BD, patients suffered from impairments in work, family, and social life and subsyndromal symptoms appeared to increase the risk of low functioning and disability in bipolar patients.[34] Depressive symptoms along with premorbid neuroticism were the best determinants of the functioning quality explaining 33% of the variance in one study.[24] On similar lines, this study found that the depressive symptoms, although minimal, were still causing functional impairment. This throws light to the strong relationship between depressive symptoms and various domains of functioning even in patients with a low HDRS score. These findings clearly demonstrate the public health significance of subsyndromal depression in the BD. Subsyndromal mania scores also had a significant relationship with Global FAST score and its financial and interpersonal domain. Although the mean YMRS scores were negligible, its significant association with functioning indicates that similar to depression, residual manic symptoms may also interfere in day-to-day functioning. Most of the studies have focused on subsyndromal depression, and only very few studies have looked into subsyndromal mania in India.[35] Subsyndromal mania could negatively influence functioning by means of the attention deficits, irritability, and impaired judgment, which is an essential feature of mania.
Medication adherence was found to be negatively correlated with the impairment in interpersonal relation functioning. Studies have found that medication adherence is an indication of insight, remission and longer time to relapse.[36,37,38] Date of the last episode was negatively correlated with functional impairment. From this, one can infer that longer the duration since the last relapse, lesser the symptoms, and better the functioning. Hence, similar to the case of medication adherence, it may reduce functional impairment. Perceived percentage of improvement was negatively correlated with all domains of FAST scale, i.e., greater a person perceived his/her improvements during remission better the functioning in all domains. Although perceived improvement as such is not examined in other studies, studies on insight have shown that insight during remission is associated with functioning although not as much a contributor as depression.[39] In psychosocial variables, social support from the family was related to better occupational and leisure functioning. Various studies have reported the importance of social support in preventing relapse and reducing symptom severity.[40,41] This might be because supportive family members tends to give them the confidence and encourage them to go for work and engage in leisure activities rather than sitting idle. According to an Indian study, social support and stressful life events are significant correlates of response to medication.[42] The social support from friends also was found to be related to increase functioning in leisure activities. Thus, good social support from family and friends might have helped in better recovery and less symptomatic interepisodic period, which in turn might aid in better functioning.
An inverse relationship was found between self-esteem and impaired functioning. Inconsistent finding was found in literature regarding self-esteem in BD. Some studies found that in remission, patients with BD had poorer self-esteem than their control and other studies found unstable self-esteem in bipolar patients, even when their symptoms were in remission.[27,43,44,45] Only one study so far reported that functioning of patients in key life domains such as self-esteem, love and social life, family, physical well-being, and working capability was affected in mixed states of BD.[46] This study has found that the effect of the disorder per say on the self-esteem seems to be lasting even after illness is remitted.
Coming to the relationship between functioning and coping dimensions, behavior disengagement and substance abuse coping contributed to impairments in functioning, while religion, positive reframing, planning, acceptance, and active coping were inversely related to the same. They may find the stressors too difficult to cope as they may underestimate their ability to overcome, which may be due to the residual depressive symptoms or poor self-esteem. Functional impairment was also associated positively with the use of substances to cope. Lam et al. found that a significant number of patients who drank or used other passive strategies in the depression prodromal phase of BD had relapsed.[47]
Predictors of functioning in patients with bipolar disorder
Of all the predictors, stress predicted the maximum percentage of variance in impaired functioning. The role of stress in functioning of patients with BD was previously discussed. While most of the previous studies have focused on nonremitted patients and had predicted onset or recurrence of BD, while the current study uniquely focused on how stress predicted functioning during the remission period. The importance of stress as a major predictor of functioning even during remission can be very useful for preventing relapses. Therapies aimed at treating remitted BD should definitely include a component of stress management in their module for better relapse prevention.
Acceptance and active coping dimensions were also found to be significant predictors of functioning. Both active coping and planning are adaptive problem-focused coping strategies. Acceptance might improve insight and prevent avoidance due to which the patient could engage in activities which can facilitate their functioning, such as treatment adherence, regulating social rhythms, reducing cognitive biases, and increasing active coping. Ability to function seems to be dependent on what actions an individual take to overcome stress. To take such actions, one needs to accept their situation initially. Thus, we can see that acceptance and active coping work synchronously in predicting functioning. Coping as such has not been examined in the previous studies. Greater use of these two coping strategies during interventions may yield better functioning in remitted bipolar patients. Self-esteem is another predictive factor of functioning which is well supported in the literature.
Limitations of the study and future direction
The study has few limitations. First, as it was cross-sectional in nature, it could not capture changes if any in functioning or in clinical or psychosocial variables across time and situations. Second, absence of comparison group could affect the conclusions drawn for this sample. Third, the medication adherence as measured by the BARS assessed medication adherence in the past month. Assessment of adherence over the past 5 years or more could have seen many of the currently adherent people score low on adherence. Fourth, the stringent criteria for remission used to recruit participants led to the exclusion of cases who were remitted for <6 months; a comparison of the partially remitted and fully remitted groups would give us a better idea about the predictors of relapse and factors that determine the recovery. Finally, a higher age range could have brought forth several other issues faced by the patients even in old age after controlling for other health complications.
Implications of the study are many; this is one of the first Indian studies that have focused on an in-depth understanding of the functional correlates of remitted patients with BD. The study findings have implications in the theoretical understanding of determinants of functioning in remitted BD. The study had highlighted the effects of clinical factors such as subsyndromal depression, early onset of illness, presence of psychosis, and recent episodes, which had affected functioning even when medication adherence was good. The present study makes an important contribution to the understanding of the psychosocial and clinical determinants of BD in a cultural context.
From this study, one can also understand that genetic component is more or less constant and the only changes that one can make are with regard to the psychosocial environment of the patient. Even with effective therapeutic and pharmacological intervention to overcome the effects of the illness, overlooking psychosocial variables could lead to disability even in the absence of acute symptoms. Although cognitive behavior therapy and interpersonal social rhythm therapy are proved effective in treating BD, high disability during interepisodic period and increased relapse rates are common. The findings of the present study highlight the significance of the psychosocial factors and cultural factors that play a major role in causing disability. This factor can be utilized in involving family members as cotherapist for the effective management of symptoms. Based on the findings, it could be inferred that the therapy should include components that help individuals reduce stress, teach adaptive coping strategies, boost self-esteem, regulate mood swings, and build awareness about identifying prodromes and educating about the psychosocial and familial context of illness.
CONCLUSION
The sample was characterized by clinical factors such as earlier age of onset, greater amount of precipitating factors, lesser episodes, minimal comorbidities, history of psychotic episodes, family history, more recent episodes, good medication adherence, and low depression and mania scores. The psychosocial factors included higher stress, moderate social support and self-esteem, and greater use of problem-focused coping strategies. Poor functioning patients had a history of longer hospital stay and had greater scores in depression, mania, stress, and maladaptive coping styles than better functioning patients. Higher depression, mania, stress, and maladaptive coping strategies were related to poor functioning, while higher medication adherence, self-esteem, and social support were related to better functioning and the main predictors of functioning were stress, active coping, acceptance coping, and self-esteem.
Financial support and sponsorship
The study was supported by the University Grants Commission - Senior Research Fellowship.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Goodwin FK, Jamison KR. New York: Oxford University Press; 2007. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression. [Google Scholar]
- 2.Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241–51. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, et al. Psychosocial disability in the course of bipolar I and II disorders: A prospective, comparative, longitudinal study. Arch Gen Psychiatry. 2005;62:1322–30. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- 4.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–7. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 5.Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635–40. doi: 10.1176/ajp.152.11.1635. [DOI] [PubMed] [Google Scholar]
- 6.Hammen C, Gitlin M, Altshuler L. Predictors of work adjustment in bipolar I patients: A naturalistic longitudinal follow-up. J Consult Clin Psychol. 2000;68:220–5. doi: 10.1037//0022-006x.68.2.220. [DOI] [PubMed] [Google Scholar]
- 7.Tohen M, Hennen J, Zarate CM, Jr, Baldessarini RJ, Strakowski SM, Stoll AL, et al. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry. 2000;157:220–8. doi: 10.1176/appi.ajp.157.2.220. [DOI] [PubMed] [Google Scholar]
- 8.Tohen M, Zarate CA, Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, et al. The McLean-Harvard First-Episode Mania Study: Prediction of recovery and first recurrence. Am J Psychiatry. 2003;160:2099–107. doi: 10.1176/appi.ajp.160.12.2099. [DOI] [PubMed] [Google Scholar]
- 9.Sheehan D, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–41. [Google Scholar]
- 10.Byerly MJ, Nakonezny PA, Rush AJ. The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophr Res. 2008;100:60–9. doi: 10.1016/j.schres.2007.12.470. [DOI] [PubMed] [Google Scholar]
- 11.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 15.Rosenberg M. New Jersey: Princeton University Press; 1965. Society and the Adolescent Self-Image. [Google Scholar]
- 16.Cacilhas AA, Magalhães PV, Ceresér KM, Walz JC, Weyne F, Rosa AR, et al. Validity of a short functioning test (FAST) in Brazilian outpatients with bipolar disorder. Value Health. 2009;12:624–7. doi: 10.1111/j.1524-4733.2008.00481.x. [DOI] [PubMed] [Google Scholar]
- 17.Rosa AR, Bonnin CM, Mazzarini L, Amann B, Kapczinski FP, Vieta E. Clinical predictors of interpersonal functioning in patients with bipolar disorder. Rev Psiquiatr Salud Ment. 2009;2:83–8. doi: 10.1016/S1888-9891(09)72249-9. [DOI] [PubMed] [Google Scholar]
- 18.Rosa AR, Reinares M, Michalak EE, Bonnin CM, Sole B, Franco C, et al. Functional impairment and disability across mood states in bipolar disorder. Value Health. 2010;13:984–8. doi: 10.1111/j.1524-4733.2010.00768.x. [DOI] [PubMed] [Google Scholar]
- 19.Ozer S, Ulusahin A, Batur S, Kabakçi E, Saka MC. Outcome measures of interepisode bipolar patients in a Turkish sample. Soc Psychiatry Psychiatr Epidemiol. 2002;37:31–7. doi: 10.1007/s127-002-8211-z. [DOI] [PubMed] [Google Scholar]
- 20.Levy B, Stephansky MR, Dobie KC, Monzani BA, Medina AM, Weiss RD. The duration of inpatient admission predicts cognitive functioning at discharge in patients with bipolar disorder. Compr Psychiatry. 2009;50:322–6. doi: 10.1016/j.comppsych.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kapczinski F, Vieta E, Andreazza AC, Frey BN, Gomes FA, Tramontina J, et al. Allostatic load in bipolar disorder: Implications for pathophysiology and treatment. Neurosci Biobehav Rev. 2008;32:675–92. doi: 10.1016/j.neubiorev.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Drieling T, Scherer-Klabunde D, Schaerer LO, Biedermann NC, Post RM, Langosch JM. Interpersonal and instrumental functioning of patients with bipolar disorder depends on remaining depressive symptoms. Age. 2010;81:18. [Google Scholar]
- 23.Mur M, Portella MJ, Martinez-Aran A, Pifarre J, Vieta E. Influence of clinical and neuropsychological variables on the psychosocial and occupational outcome of remitted bipolar patients. Psychopathology. 2009;42:148–56. doi: 10.1159/000207456. [DOI] [PubMed] [Google Scholar]
- 24.Pope M, Dudley R, Scott J. Determinants of social functioning in bipolar disorder. Bipolar Disord. 2007;9:38–44. doi: 10.1111/j.1399-5618.2007.00323.x. [DOI] [PubMed] [Google Scholar]
- 25.Hayward P, Wong G, Bright JA, Lam D. Stigma and self-esteem in manic depression: An exploratory study. J Affect Disord. 2002;69:61–7. doi: 10.1016/s0165-0327(00)00380-3. [DOI] [PubMed] [Google Scholar]
- 26.Johnson SL, Meyer B, Winett C, Small J. Social support and self-esteem predict changes in bipolar depression but not mania. J Affect Disord. 2000;58:79–86. doi: 10.1016/s0165-0327(99)00133-0. [DOI] [PubMed] [Google Scholar]
- 27.Nilsson KK, Jørgensen CR, Craig TK, Straarup KN, Licht RW. Self-esteem in remitted bipolar disorder patients: A meta-analysis. Bipolar Disord. 2010;12:585–92. doi: 10.1111/j.1399-5618.2010.00856.x. [DOI] [PubMed] [Google Scholar]
- 28.Chand PK, Mattoo SK, Sharan P. Quality of life and its correlates in patients with bipolar disorder stabilized on lithium prophylaxis. Psychiatry Clin Neurosci. 2004;58:311–8. doi: 10.1111/j.1440-1819.2004.01237.x. [DOI] [PubMed] [Google Scholar]
- 29.Henry AD, Coster WJ. Predictors of functional outcome among adolescents and young adults with psychotic disorders. Am J Occup Ther. 1996;50:171–81. doi: 10.5014/ajot.50.3.171. [DOI] [PubMed] [Google Scholar]
- 30.Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129:216–69. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- 31.Lam D, Wong G. Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med. 1997;27:1091–100. doi: 10.1017/s0033291797005540. [DOI] [PubMed] [Google Scholar]
- 32.Meyer B. Coping with severe mental illness: Relations of the brief COPE with symptoms, functioning, and well-being. J Psychopathol Behav Assess. 2001;23:265–77. [Google Scholar]
- 33.Pavlickova H, Varese F, Smith A, Myin-Germeys I, Turnbull OH, Emsley R, et al. The dynamics of mood and coping in bipolar disorder: Longitudinal investigations of the inter-relationship between affect, self-esteem and response styles. PLoS One. 2013;8:e62514. doi: 10.1371/journal.pone.0062514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanchez-Moreno J, Martinez-Aran A, Tabarés-Seisdedos R, Torrent C, Vieta E, Ayuso-Mateos JL. Functioning and disability in bipolar disorder: An extensive review. Psychother Psychosom. 2009;78:285–97. doi: 10.1159/000228249. [DOI] [PubMed] [Google Scholar]
- 35.Ram D, Ram D. Subsyndromal states in bipolar disorder. Indian J Psychiatry. 2010;52:367–70. doi: 10.4103/0019-5545.74314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baldessarini RJ, Tondo L, Davis P, Pompili M, Goodwin FK, Hennen J. Decreased risk of suicides and attempts during long-term lithium treatment: A meta-analytic review. Bipolar Disord. 2006;8(5 Pt 2):625–39. doi: 10.1111/j.1399-5618.2006.00344.x. [DOI] [PubMed] [Google Scholar]
- 37.Colom F, Vieta E, Martínez-Arán A, Reinares M, Benabarre A, Gastó C. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549–55. doi: 10.4088/jcp.v61n0802. [DOI] [PubMed] [Google Scholar]
- 38.Col SE, Caykoylu A, Karakas Ugurlu G, Ugurlu M. Factors affecting treatment compliance in patients with bipolar I disorder during prophylaxis: A study from Turkey. Gen Hosp Psychiatry. 2014;36:208–13. doi: 10.1016/j.genhosppsych.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 39.Dias VV, Brissos S, Frey BN, Kapczinski F. Insight, quality of life and cognitive functioning in euthymic patients with bipolar disorder. J Affect Disord. 2008;110:75–83. doi: 10.1016/j.jad.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 40.Johnson SL, Winett CA, Meyer B, Greenhouse WJ, Miller I. Social support and the course of bipolar disorder. J Abnorm Psychol. 1999;108:558–66. doi: 10.1037//0021-843x.108.4.558. [DOI] [PubMed] [Google Scholar]
- 41.Johnson L, Lundström O, Aberg-Wistedt A, Mathé AA. Social support in bipolar disorder: Its relevance to remission and relapse. Bipolar Disord. 2003;5:129–37. doi: 10.1034/j.1399-5618.2003.00021.x. [DOI] [PubMed] [Google Scholar]
- 42.Kulhara P, Basu D, Mattoo SK, Sharan P, Chopra R. Lithium prophylaxis of recurrent bipolar affective disorder: Long-term outcome and its psychosocial correlates. J Affect Disord. 1999;54:87–96. doi: 10.1016/s0165-0327(98)00145-1. [DOI] [PubMed] [Google Scholar]
- 43.Blairy S, Linotte S, Souery D, Papadimitriou GN, Dikeos D, Lerer B, et al. Social adjustment and self-esteem of bipolar patients: A multicentric study. J Affect Disord. 2004;79:97–103. doi: 10.1016/S0165-0327(02)00347-6. [DOI] [PubMed] [Google Scholar]
- 44.Shapira B, Zislin J, Gelfin Y, Osher Y, Gorfine M, Souery D, et al. Social adjustment and self-esteem in remitted patients with unipolar and bipolar affective disorder: A case-control study. Compr Psychiatry. 1999;40:24–30. doi: 10.1016/s0010-440x(99)90072-x. [DOI] [PubMed] [Google Scholar]
- 45.Knowles R, Tai S, Jones SH, Highfield J, Morriss R, Bentall RP. Stability of self-esteem in bipolar disorder: Comparisons among remitted bipolar patients, remitted unipolar patients and healthy controls. Bipolar Disord. 2007;9:490–5. doi: 10.1111/j.1399-5618.2007.00457.x. [DOI] [PubMed] [Google Scholar]
- 46.Lee Mortensen G, Vinberg M, Lee Mortensen S, Balslev Jørgensen M, Eberhard J. Bipolar patients’ quality of life in mixed states: A preliminary qualitative study. Psychopathology. 2015;48:192–201. doi: 10.1159/000381479. [DOI] [PubMed] [Google Scholar]
- 47.Lam D, Wong G, Sham P. Prodromes, coping strategies and course of illness in bipolar affective disorder – A naturalistic study. Psychol Med. 2001;31:1397–402. doi: 10.1017/s003329170100472x. [DOI] [PubMed] [Google Scholar]
- 48.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]


