Abstract
Breakthroughs in our global fight against cancer have been achieved. However, this progress has been unequal. In low- and middle-income countries and for specific populations in high-income settings, many of these advancements are but an aspiration and hope for the future. This review will focus on health disparities in cancer within and across countries, drawing from examples in Kenya, Brazil, and the United States. Placed in context with these examples, the authors also draw basic recommendations from several initiatives and groups that are working on the issue of global cancer disparities, including the US Institute of Medicine, the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries, and the Union for International Cancer Control. From increasing initiatives in basic resources in low-income countries to rapid learning systems in high-income countries, the authors argue that beyond ethics and equity issues, it makes economic sense to invest in global cancer control, especially in low- and middle-income countries.
INTRODUCTION
In the last 50 years, major breakthroughs in our global fight against cancer have been achieved. However, in low- and middle-income countries and for specific populations in high-income settings, many of these advancements are but an aspiration.1 This review will focus on health disparities in cancer within and across countries. Using examples that cover the income spectrum from low to high, we will describe the challenges faced by public health officials, physicians, and patients at each level. We will then summarize the most important steps needed to improve global cancer control.
Several definitions for health disparities have been proposed.2 In the United States, the Healthy People 2020 program defines health disparities as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage.”3 Two observations should be noted regarding these definitions. First, a common theme is that race and ethnicity are not the only determinants of disparities. Other avoidable inequalities in social determinants of health, such as socioeconomic status, geographic location, and sex, also play a role. Second, it is mandatory to distinguish between disparities in cancer care and disparities in cancer outcomes, acknowledging of course that outcomes are inextricably linked to care.
ECONOMIC CASE FOR INVESTING IN CANCER CONTROL: ADDRESSING CANCER DISPARITIES ACROSS COUNTRIES
Cancer control is defined by the Union for International Cancer Control (UICC) as a public health approach aimed at reducing the burden of cancer in a population. This concept includes the planning of integrated, evidence-based, and cost-effective interventions across the cancer continuum (research, prevention, early detection, treatment, and palliative care). In 2012, there were 14.1 million new cancer cases and 8.2 million cancer deaths worldwide; 57% of cases and 65% of deaths occurred in lower income countries. Aggregate data show that the ratio of yearly mortality and incidence is 0.475 in more developed regions, whereas it is 0.644 in less developed ones. In the United States and European Union, the mortality-to-incidence ratios are 0.36 and 0.48, respectively. In contrast, these ratios range from 0.66 to 0.7 in the WHO's Western Pacific, Southeast Asia, and Africa regions.1 Furthermore, 5-year survival rates for most cancers are higher in richer countries than in low- and middle-income countries. These data demonstrate wide disparities in cancer outcomes,4-6 reflecting, in part, different relative investments in cancer control in countries around the world. The gap is striking when comparing the 5-year age-standardized net survival rates for breast cancer (2005 to 2009) of 88.6% in the United States and 87.4% in Brazil versus 59.8% in Algeria, 53.4% in South Africa, and 43.1% in Jordan. Further, although the annual economic burden of each patient with cancer in the United States, the United Kingdom, and Japan falls between US$183 and US$460, it ranges from a paltry US$0.54 to US$7.92 in South America, India, and China. Overall, high-income regions spend five to 10 times more on cancer control on a per capita basis than low- and middle-income countries.1
At the 2014 World Cancer Leaders' Summit,7 cancer advocates, including one of the authors of this article (G.L.), argued that it makes economic sense to invest in global cancer control, especially in low- and middle-income countries. In 2010, taking into consideration the direct costs related to the prevention and treatment of the disease and the economic value of lives lost and disability caused, cancer had an impact of approximately US$1.16 trillion worldwide. Further estimates, which add the longer term costs of patients and their families, bring the annual global cost of cancer to US$2.5 trillion.8
The implementation of prevention, early detection, and treatment strategies could potentially save between 2.4 and 3.7 million lives annually. The vast majority of these lives would be saved in low- and middle-income countries, yielding an economic benefit in excess of US$400 billion. Moreover, it has been estimated that an investment of US$11.4 billion in a set of core prevention strategies in less wealthy regions of the world can lead to savings of up to US$100 billion in future cancer treatment costs.8,9 The measures with the highest potential for clinical and economic impact are those geared toward tobacco and obesity control, vaccines, early detection and treatment, palliative care, and health systems planning, with the creation of cancer registries. Table 1 discusses these measures in detail.
Table 1.
| Priorities | Facts | Initiatives |
|---|---|---|
| Tobacco control | The cost of tobacco-related cancers exceeds US$200 billion a year. The WHO estimates that by increasing tobacco taxes by 50%, there could be a reduction in the number of smokers by 49 million within the next 3 years. It has then been suggested that it would ultimately save 11 million lives, without a decrease in government revenues. | The average low- and middle-income country could, for a cost of approximately US$0.11 per capita, implement the most active control measures, including education campaigns; higher excise taxes on tobacco; smoking bans in public places; and bans on advertising, promotion, and sponsorship. |
| Obesity, diet, and exercise | Obesity and other diet- and physical activity–related risk factors contribute to approximately 20% of cancer cases globally and will soon be the most common modifiable causes of the disease. The Organization for Economic Cooperation and Development has predicted that the implementation of strategies to improve diets, increase physical activity, and tackle obesity in Europe would lead to gains of > 3 million years of life free of cancer over 10 years, a benefit that could increase to 11.8 million in another decade. | A recent report by McKinsey, a business consultancy, drawing on data from the United Kingdom, showed that a series of interventions to curb overweight and obesity are cost effective, costing society less than the economic benefits they bring. These included public health campaigns, portion control, and limiting media exposure and price promotions. |
| Vaccines | Chronic infections are responsible for approximately 15% of all cancers around the world, but in some regions, such as in sub-Saharan Africa, nearly a third of all cancers are secondary to infections, compared with < 3% in developed countries. Vaccines to prevent hepatitis B (HBV) and human papillomavirus (HPV) have a significant impact in the prevention of liver and cervical cancer, respectively. The HPV vaccine can prevent up to 70% of cervical cancers, and HBV vaccines have had a significant impact in Asian countries that implemented immunization programs in the 1980s, such as Taiwan and Singapore. | GAVI, a public-private partnership formerly known as the Global Alliance for Vaccines and Immunization, has had a major impact in reducing the price of HBV and HPV vaccines to US$0.20 and US$4.50 per dose, respectively. By providing funding and creating a working market where previously there was none, it has improved access in eligible low-income countries and potentially averted hundreds of thousands of cancer deaths. |
| Prevention, early detection, and treatment | The prevention, early detection, and treatment of common cancers would have a major impact worldwide. Global investment in cervical cancer prevention could save up to 230 million years of life free of disability, with an economic value of US$1 trillion in 2010. The estimated cost of new breast cancers in the same year was US$26.6 billion. As examples, the treatment of late-stage breast cancer is three times more expensive than the management of early-stage disease. The estimated cost of death and disability caused by colorectal cancer was US$99 billion in 2008, excluding direct treatment costs. | In high-resource settings, colorectal cancer screening has been shown to be a cost-effective or cost-saving measure. Worldwide, there are nearly 300,000 new cases of oral cancer every year. Studies in India, where a third of global cases occur, show that oral cancer screening by visual inspection is cost effective and that early detection can reduce the associated morbidity and mortality. Oral cancer visual inspection by trained health workers can be carried out for < US$6.00 per person. The incremental cost per life-year saved was US$835 for all individuals eligible for screening and US$156 for high-risk individuals. |
| Palliative care | The WHO defines palliative care as an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness through the prevention and relief of suffering by means of early identification and assessment and treatment of pain and other physical, psychosocial, and spiritual problems. | Several studies have quantified that hospital-based palliative care visits can reduce hospital costs by up to US$7,500 for patients who die during their last admission. Home-based palliative care is also important and can reduce the overall cost of care by up to US$7,500 per cancer patient. |
| Cancer control planning and registries | Investing in national cancer control planning is vital to plan and deliver cost-effective programs aimed at reducing cancer incidence and mortality, to improve patients' quality of life and well-being, and to decrease the economic impact of cancer globally. Cancer registries cover < 10% of the world's population, and the available ones are predominantly located in high- and middle-income countries. In Africa, < 1% of the population is covered. | The Centers for Disease Control and Prevention, in collaboration with the International Agency for Research on Cancer, is supporting research to test pilot and develop a standardized instrument—the International Cancer Registry Costing tool (InCanRegCosting tool). This project aims to systematically assess the cost of cancer registration in LMICs. Moreover, the Global Initiative for Cancer Registries, a multipartner initiative led by the International Agency for Research in Cancer, estimates that with an investment of US$15 million over 5 years, it can establish four regional capacity building hubs that would significantly improve cancer data collection around the world. |
| Universal health care | Aiming to improve access to health care, many LMICs in Asia and Latin America have introduced universal coverage, the fundamental element of functional health care systems because it allows pooling of resources and the provision of financial protection from the costs of illness. As an example, not just Brazil, but also Chile, Colombia, Costa Rica, Mexico, Malaysia, South Korea, Taiwan, Thailand, and others have enacted legislation creating comprehensive insurance systems over the last few decades. | A majority of LMICs, many of which are in Africa, however, still lack universal coverage programs. A study of 192 nations revealed that even though 75 of these countries had a mandate for universal access to health care, only 58 of them met stricter criteria of > 90% access of the population to skilled birth attendance (doctors, midwives, or both) and insurance. Universal coverage also brings challenges, because it often increases public expenditure (and therefore taxation) and increases bureaucratic and administrative demands. In China, for instance, public expenditure increased from 35.6% in 2001 to nearly 60% of the total health care spending in 2012. Moreover, in low-resource settings, institutions might be weaker, and problems with corruption as well as management and accountability incentives may result in underfunding and misallocation of expenditures. |
Abbreviations: HBV, hepatitis B virus; HPV, human papillomavirus; LMICs, low- and middle-income countries.
To further justify such investments, this article will describe case studies on the challenges and opportunities in different countries. It will further draw from the authors' previous experience and work published by the US Institute of Medicine,10 the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries,11 and the UICC.7
LOW-INCOME COUNTRIES: KENYA AS AN EXAMPLE
Kenya is a low-income East African country in sub-Saharan Africa with a population of 44 million and a gross domestic product (GDP) per capita of US$1,245.12 In 2012, total health expenditures were 4.7% of GDP.11 Life expectancy is 58 years for men and 61 years for women. Population-based registry data are not available in the country, but it is estimated that the annual incidence of cancer is approximately 28,000 cases and 22,000 deaths. Cancer is the third leading cause of mortality, after infections and cardiovascular diseases, causing 7% of deaths annually. As in most low-income countries, noncommunicable diseases are not the predominant burden in Kenya. However, the most common cancers are cervical and breast cancers,13 preventable diseases that would highly benefit from a cancer control policy. Highlighting these differences in outcomes, the estimated age-standardized mortality rates per 100,000 persons per year for cervical cancer is 2.7 in the United States, 7.4 in Brazil, and 21.8 in Kenya.
Kenya's health care financing, initially predominantly tax funded, evolved to include user fees in 1992 as a result of budgetary constraints.12 Modifications in 2004 mandated free basic health care at the primary level for all citizens, yet out-of-pocket health care expenditures still account for most of health care financing. The government-funded insurance scheme, known as the National Hospital Insurance Fund, does not cover outpatient screening, diagnostics, or treatment of cancer. Although health insurance coverage in the formal workforce is high as a result of compulsory registration, less than 16% of the population in the informal sector (> 80% of Kenya's workforce) is covered.12,14 Overall, only 4.5 million people (11% of the Kenyan population) had health care coverage in 2013.
In 2011, the National Cancer Prevention and Control Programme stipulated provisions for “efficient and evidence-based preventive, curative and palliative care services accessible to all Kenyans.”12 Some collaborative programs between academic institutions and treatment centers, such as the Academic Model Providing Access to Healthcare15 in western Kenya, provide education, free screening for cervical cancer (using visual inspection with acetic acid), and clinical breast exams. However, as in many low- and middle-income countries, implementation of such ambitious programs has remained challenging, and cancer screening occurs in a few selected sites and disjointed projects rather than as a fully fledged, national-level, comprehensive program.16 Therefore, coverage is negligible. In addition to implementation issues, access to cervical, breast, and colon cancer screening is also impaired as a result of lack of community awareness on the importance of screening, as well as low health literacy. Human papillomavirus (HPV) and hepatitis B vaccines are not provided as part of the national vaccine and immunization program. Other factors include inadequate skills among service providers; lack of equipment and supplies (eg, no mammography is available for breast cancer screening in the public national referral systems); inadequate monitoring and evaluation of existing programs, especially for data collection and management; and low prioritization of screening among policymakers and opinion leaders.
Related to available resources, there are more than 50 palliative care centers in Kenya, including free-standing hospices, rural community palliative and hospice centers, religious mission hospitals, public tertiary referral centers, government hospitals, and private hospitals.17 Pain control remains a major challenge as a result of the cost of narcotics (morphine costs approximately US$3 per gram18), the lack of availability of pain medications, and the variable level of awareness of pain management among health care workers. Although surgical services for patients with cancer are usually available, the cost of such services is prohibitive to most patients. There are only two cobalt radiation machines available for public patients at one of the two tertiary referral centers in Kenya. These machines are overstretched, and appointments for radiotherapy are booked up to 8 months away. For private patients, there are four linear accelerators in Nairobi. Those who can pay out of pocket or with private insurance coverage are able to get prompt radiotherapy when needed.
Finally, chemotherapy is available, but because of the high cost of drugs and the consequent inability of the National Hospital Insurance Fund to cover the cost of cancer treatments, it is inaccessible to most patients. Most drugs in the WHO essential medicines list19 are not available, and there is no national or regional purchasing arrangement. Rather, hospitals and other providers procure drugs directly from industry, decreasing the purchasers' bargaining power. For cancer drugs, of 52 present in the UICC's revision of the WHO essential medicines list, only 18 are present in Kenya's essential list.20
In summary, Kenya, like most low-income countries, struggles with the foundation of a health care financing and delivery system that can tackle cancer control. Following this example, we can conclude that in low-income settings, several factors affect our ability to control cancer. There are low levels of awareness of cancer in the general population and among health professionals. As a result, it takes longer than it should for patients to seek medical attention and for physicians to make a diagnosis. There is often misapplication and misallocation of scarce resources and limited population data and access to health care. There is a lack of viable business models for cancer care, either public or private, and no well-established funding mechanism for cancer services. Furthermore, health infrastructure, such as oncology clinics, biochemistry and pathology laboratories, and imaging services, is often nonexistent, and there are inadequate numbers of well-trained personnel. Above all, there is a lack of political will within many countries to mobilize resources for cancer planning and control, because health care systems are still focused on acute care of infectious diseases.21
MIDDLE-INCOME COUNTRIES: BRAZIL AS AN EXAMPLE
Brazil is a federative republic with a population of approximately 200 million. It is a middle-income country with a GDP per capita of US$11,208 in 201322 and a life expectancy of 70 years for men and 77 years for women. The population is covered by a public, tax-funded, universal health scheme called Sistema Único de Saúde, and 25% of the population has private medical insurance. Total health expenditures reach 9.3% of GDP, with 46% coming from public sources. The most common cancers in men (in order from most to least frequent) are those of the prostate, lungs and airway, colon and rectum, stomach, and oral cavity; and in women, the most common cancers are those of the breast, colon and rectum, cervix, lungs and airway, and thyroid.
A national cancer control plan has been in place since 2005. Subnational population- and hospital-based registries are available and supply local data for cancer control planning. Smoking is banned in public places, as is its advertising. Taxes on tobacco exceed 60% of the final price. With these measures and educational campaigns, less than 12% of Brazilians are current smokers, as compared with a rate of 32% in 1989.23,24 As for other risk factors, 17.4% of adults are obese, 14.9% are not physically active, and only 34% of Brazilians eat an adequate amount of fresh fruits and vegetables. HPV prevalence was 40% in a survey of pregnant women, and 18.4% of Brazilians drink alcohol at least sporadically. To address these risk factors, there are federal policies to prevent and control overweight and harmful use of alcohol. Hepatitis B virus vaccination was introduced in 1998 and covers 97% of the target population (newborns). HPV vaccination of girls between the ages of 11 and 13 became freely available to the public in 2014 and will be extended to girls age 9 and 10 in 2015.25 In the first 6 months after the program initiation, 4.3 million girls between the ages of 11 and 13 were vaccinated, covering 87.3% of the target population. Through a technology transfer program with Merck/MSD, Instituto Butantan (São Paulo, Brazil) will produce the HPV vaccine in Brazil, at potentially lower costs.
Screening for cervical and breast cancer is available through the public health care system. Pap smear is recommended for women between the ages of 25 and 64 years, every 3 years, after two consecutive normal Pap tests done annually. It is estimated that nearly 80% of the target population has been covered. For breast cancer, breast clinical examination is recommended for women age 40 to 69 years, and mammography screening is recommended for those age 50 to 69 years (every 2 years). In women with a family history of breast cancer, mammography screening is indicated annually starting at 35 years of age. Surveys suggest that 50% of women age ≥ 50 years have had at least one screening mammogram.26
Radiation services are usually available in the public system, but there are disparities in access based on geography and income. Although there are more than 250 radiation machines in the country, with average waiting times of up to 3 months in areas with the least access to care, an extra 130 radiation machines are needed to fill the gap.25 The government announced the purchase of 80 machines from Varian at a combined cost of R$120 million (approximately US$645,000 per machine at the time of the deal) in 2014, but implementation has been delayed. This exemplifies not only how a large middle-income country (and possibly consortia of smaller countries or regions) can use volume to negotiate better prices with industry, but also the difficulties lower income nations have in terms of bureaucracy and in developing the required human resources.
Pathology, imaging, and surgical services are available, although delays are common, and molecular tests are not always available. In a survey of patients who presented with mammographic abnormalities at a public hospital in the state of São Paulo, for instance, the average time between mammography and a diagnostic biopsy was 72 days.27 In another study, male patients presenting with symptoms compatible with oral cancer waited an average of more than 5 months to seek medical care. Once they saw a physician, it took an average of 41 days to start treatment.28 Palliative care is available in clinics and hospitals, but there is little or no home care in the public and private settings.
Once an intravenous anticancer drug is approved by the local regulatory agency, Agência Nacional de Vigilância Sanitária, coverage is mandatory in the private health care system. The Brazilian essential medicines list is called Relacão Nacional de Medicamentos Essenciais (2014),29 and it covers most of the WHO essential list. New legislation enforced the coverage of oral drugs in the private system in January 2014.30 Finally, citizens are able to sue the federal government for access to cancer medications and most often win. From a health system perspective, this can worsen disparities, because richer patients are usually the ones who can afford to hire lawyers. Therefore, there has been an active debate related to how to prioritize relatively scarce resources in the public system.
Like most middle-income countries, Brazil has been able to develop a basic health care system and a cancer control plan, leading to improved outcomes and a decrease in cancer mortality over the last decade.31 Nevertheless, the country still struggles with more advanced technologies, such as molecular tests and targeted agents. In addition, there are clear regional disparities, with decreased access and availability of resources as one moves away from the state capitals and richest cities into the vast countryside and less developed regions.32 In this regard, travel distance to cancer centers is a particular challenge in Brazil. For example, although there was a decline in lung cancer mortality among Brazilian men in in the state capitals, there was an increase in the smaller cities, mainly in the north and northeast regions.33
Middle-income countries not only have more resources than low-income ones, but also usually spend a higher proportion of GDP on health care. This leads to greater success in establishing systems to fight cancer. Many have been able to establish relatively adequate universal coverage schemes.34,35 Upper-middle-income countries have been able to use the volume of services purchased or hired to obtain lower prices for radiation machines and chemotherapy drugs and serve as an example for other countries or consortia of countries for purchasing or hiring services.
HIGH-INCOME COUNTRIES: THE UNITED STATES AS AN EXAMPLE
The United States is a federative presidential republic with an ethnically diverse, multicultural population of approximately 300 million. The GDP of the United States is $15 trillion ($50,000 per person), 17% of which is spent on health care.36 The health care system is dual with public and private financing and delivery of care, with approximately 60% to 65% of financing coming from the government through programs such as Medicare, Medicaid, the Children's Health Insurance Plan, and the Veterans Health Administration. There are an estimated 1,658,370 cases and 589,430 deaths from cancer annually in the United States, with a mortality-to-incidence ratio of 0.36.37
A national cancer control plan has been in place since 2010, and a countrywide population-based cancer registry is available. Smoking is banned in public places. Taxes on tobacco exceed 40% of the final price in most states. Less than 19% of Americans are current smokers. As for other risk factors, 26.9% of adults are obese, 40.5% are not physically active, 65.4% drink alcohol at least sporadically, and only 23.4% eat an adequate amount of fresh fruits and vegetables. HPV prevalence is less than 14%.38,39
There are policies to prevent and control overweight and harmful use of alcohol. Hepatitis B virus vaccination was introduced in 1991 and covers 91% of the target population (newborns). The HPV vaccination plan is to immunize boys and girls age 11 to 12 years; however, only 32% of the target population has been vaccinated. Screening for cervical and breast cancer is available through the public and private health care systems through Pap smear and HPV testing with coverage of 83% of the target population. More than 70% of women age 50 to 74 years have undergone at least one mammogram in the last 2 years. Nearly 60% of eligible individuals undergo screening for colorectal cancer.
Radiation services are available, with more than 2,700 radiation machines in the country. There are adequate amounts of radiation oncologists and physicists. Advanced pathology, imaging, and surgical services are available to patients with health care coverage, as is chemotherapy, including newer and more expensive IV and oral treatments. Home palliative care is available in most regions.
Factors that contribute to health disparities in cancer in the United States include socioeconomic status, access to health care services, individual behaviors, the social and built environments, exposure to carcinogens, and treatment.40,41 Among men, the highest cancer incidence rate is observed among blacks, with overall rates 15% higher than those of whites and nearly twice the rates among Asian Pacific Islanders. Prostate, lung, and colorectal cancers are the three most commonly diagnosed cancers among men in each racial and ethnic group. The exception is Hispanic men, for whom colorectal cancer incidence was slightly higher than lung cancer incidence. Among women, the highest overall cancer incidence rates are observed among non-Hispanic and white women. Breast cancer is the most commonly diagnosed cancer in each racial and ethnic group. For white, black, and American Indian/Alaska Native women, incident lung and colorectal cancers rank second and third, respectively. In addition to differences in incidence, there are also large differences in the all-cancer mortality rates by race/ethnicity; the highest rate is seen among non-Hispanic blacks (208.8 per 100,000 population), followed by whites (176.5), Hispanics (119.7), and Asians (108.9).42
In addition, initiatives at the state level have provided evidence that a reduction in cancer disparities is possible if resources are properly allocated. For example, the state of Delaware recently undertook an experiment to reduce disparities in colorectal cancer among its residents.43 The key elements of this program included a colorectal cancer screening program, which promoted colonoscopy as the preferred screening tool and used nurse navigators and care coordinators to recruit and navigate patients; a cancer treatment program, which, in combination with existing insurance coverage, provides universal screening and treatment; and an emphasis on a reduction in the African American cancer disparity. Between 2002 and 2009, this program eliminated screening disparities, equalized incidence rates, reduced the percentage of African Americans with regional and distant disease from 79% to 40%, and nearly eliminated mortality differences.
Most recently, the Patient Protection and Affordable Care Act revolved around expanding access to care mainly through Medicaid, usually seen as health care coverage for the nonelderly low-income population. It has been estimated that under the Medicaid and Children's Health Insurance Program, 16 to 20 million additional people will have health coverage,18 with 160,000 having a cancer diagnosis. Also, families with household incomes up to 400% of the federal poverty level (approximately $45,000 for an individual or $97,000 for a family of four) are eligible for financial assistance to help lower total out-of-pocket insurance costs.14 This increased access to care has the potential to decrease disparities in cancer care. However, it has also been suggested that the Patient Protection and Affordable Care Act may result in health insurance premium increases for patients younger than 40 years, mainly young men.44 This is particularly important because young uninsured adults are more likely to present with advanced disease, be undertreated, or die after a diagnosis of cancer compared with those who are insured.44 Finally, there is ongoing debate in both the political and clinical arenas regarding how the increasing costs of new cancer treatments will impact disparities. To bring attention to this issue, the impact of costs experienced by patients (on access, quality of life, or survival) over the continuum of cancer care (from screening to survivorship) has recently been termed financial toxicity.45,46
The major challenge in high-income settings is to ensure that minorities and vulnerable populations have adequate access to health coverage and services. Moreover, the challenges of increasingly expensive cancer drugs and the impact of costs on patients are universal and need to be tackled. To create truly high-quality care through the continuum of care, these countries can lead the way by developing learning systems that promote patient engagement, better coordination of care, and the use of evidence-based oncology, quality measurement, and performance improvement. In addition, the American Society of Clinical Oncology has promoted the development of learning systems and decision tools that promote the so-called value of cancer care.47,48 These tools have the potential to both identify gaps in disparities research and prioritize resources in an evidence-based way. Table 2 lists the commonalities in low-, middle-, and high-income countries.
Table 2.
Summary of Common Challenges in Low-, Middle-, and High-Income Countries
| Challenge | Description |
|---|---|
| Poverty | Poverty is an obstacle to receiving cancer care. It forces people to concentrate on basic economic survival at the expense of good lifestyle habits, preventive medicine, cancer screening, and treatment in low-, middle-, and high-income countries. |
| Access | Availability of adequate and high-quality cancer care facilities varies geographically within low-, middle-, and high-income countries. Similarly, distance to high-quality cancer care has been shown to be an obstacle to cancer outcomes. |
| Financing for cancer care | Even with health care coverage, expenses may be unaffordable in low-, middle-, and high-income countries. |
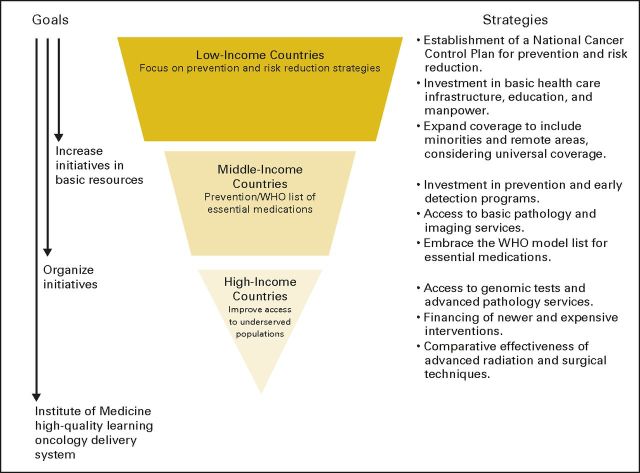
STEPPING STONES: A FRAMEWORK
The Institute of Medicine, the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries, the WHO, and other institutions and groups have created frameworks detailing the most important stepping stones in improving the fight against cancer in low-, middle-, and high-income countries. An extensive list of steps would include the following: the establishment of universal health care coverage; the development of health care infrastructure and well-trained human capital; the creation of national cancer control plans, including the establishment and improvement of cancer registries and data repositories on cancer risk factors and treatment outcomes; tobacco control; vaccination against the most common viruses that cause cancer, namely HPV and hepatitis B; promotion of healthy diets, exercise, and obesity control; resource-stratified evidence-based screening, diagnosis, and treatment of common cancers and the creation of reference cancer centers; access to essential cancer medicines; and access to palliative care, especially pain control. This list of stepping stones can be further improved by integration into a health information technology system that can help clinicians and researchers to translate best evidence into clinical practice and to develop quality measures leading to performance improvement. High- and middle-income countries have the resources to pave the way described earlier. Poverty is a major obstacle for medical care, especially in low-income countries. It impairs a patient's ability to seek help, reach medical facilities, and pay for appropriate interventions in systems in which health care provision is not free at the service point. Although economic development is likely to be the only measure that can improve this situation in the long run, policies such as conditional cash transfers and free access to health services in universal health schemes funded by taxation or contributions have been implemented with at least partial success in middle-income countries, such as Brazil and Mexico. For low-income countries, only with the support of the international community and the creation of a global fund to fight cancer will we see them passing those first stepping stones. In summary, the authors argue given the high population burden of preventable cancers in low-income countries, these are the cancers to be tackled first in these settings. In middle-income settings, risk reduction and fully embracing the WHO essential list of medications are warranted. For high-income countries, improving both prevention and treatment access to minorities should be a priority. Figure 1 summarizes the main building blocks in the creation of a high-quality cancer control system. It is out of the scope of this article to describe and discuss them in detail, but we urge the reader to access the original references for further information.
Fig 1.
Building blocks for addressing cancer disparities per income settings.
Since the United Nations high-level summit on noncommunicable diseases in 2011, the fight against cancer has become more visible in global public health. It should be clear to all of us that supporting the international fight against disparities in cancer is of paramount importance. This view is not only based in terms of curbing human suffering, but also in practical and economic grounds. To achieve this, it will take a global village. It is only through the engagement of all stakeholders, including governments, private companies, and nonprofits, that we will inch our way into making cancer history. The time is right for every nation to create or update its cancer control plan and invest more in decreasing cancer disparities. The authors hope that this summary paper will support the reader in taking action in their settings.
Footnotes
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: Jonas A. de Souza, Gilberto Lopes
Administrative support: Jonas A. de Souza, Gilberto Lopes
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Global Health Equity: Cancer Care Outcome Disparities in High-, Middle-, and Low-Income Countries
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Jonas A. de Souza
Honoraria: AstraZeneca
Bijou Hunt
No relationship to disclose
Fredrick Chite Asirwa
No relationship to disclose
Clement Adebamowo
No relationship to disclose
Gilberto Lopes
Honoraria: AstraZeneca, Roche/Genentech, Merck Serono, Merck Sharp & Dohme, Fresenius Kabi, Novartis
Consulting or Advisory Role: Pfizer, Bristol-Myers Squibb, Lilly/ImClone
Research Funding: Lilly/ImClone, Pfizer, AstraZeneca, Merck Sharp & Dohme, Eisai
Expert Testimony: Sanofi
REFERENCES
- 1.Lopes Gde L, Jr, de Souza JA, Barrios C: Access to cancer medications in low- and middle-income countries Nat Rev Clin Oncol 10:314–322,2013 [DOI] [PubMed] [Google Scholar]
- 2.Krieger N: Defining and investigating social disparities in cancer: Critical issues Cancer Causes Control 16:5–14,2005 [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services : The Secretary's Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: Recommendations for the framework and format of Healthy People 2020. Section IV. Advisory Committee findings and recommendations http://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf
- 4.International Agency for Research on Cancer, WHO : GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012 http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx
- 5.Torre LA Bray F Siegel RL, etal: Global cancer statistics, 2012 CA Cancer J Clin 65:87–108,2015 [DOI] [PubMed] [Google Scholar]
- 6.Allemani C Weir HK Carreira H, etal: Global surveillance of cancer survival 1995-2009: Analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet 385:977–1010,2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Union for International Cancer Control : World Cancer Leader's Summit 2014: The Economics of Cancer Prevention & Control Data Digest 2014 http://www.iccp-portal.org/sites/default/files/resources/WCLS2014_economics_of_cancer_FINAL-2.pdf
- 8.WHO : Country profile: Brazil http://www.who.int/countries/bra/en/
- 9.Knaul FM Arreola-Ornelas H Atun R, etal: Knaul FM, Gralow JR, Atun R, et al.Investing in cancer care and control Closing the Cancer Divide: An Equity Imperative 2012. Boston, MA: Harvard Global Equity Initiative [Google Scholar]
- 10.Institute of Medicine : Cancer control opportunities in low and middle income countries, 2007 https://download.nap.edu/catalog.php?record_id=11797
- 11.Farmer P Frenk J Knaul FM, etal: Expansion of cancer care and control in countries of low and middle income: A call to action Lancet 376:1186–1193,2010 [DOI] [PubMed] [Google Scholar]
- 12.WHO : Kenya statistics summary. Global Health Observatory Data Repository, WHO 2002-2015 http://www.who.int/countries/Ken/en/
- 13.Republic of Kenya Ministry of Public Health and Sanitation and Ministry of Medical Services : National Cancer Control Strategy; 2011 http://www.ipcrc.net/pdfs/Kenya-National-Cancer-Control-strategy.pdf
- 14.Carrin G James C Adelhardt M, etal: Health financing reform in Kenya: Assessing the social health insurance proposal S Afr Med J 97:130–135,2007 [PubMed] [Google Scholar]
- 15.Strother RM Asirwa FC Busakhala NB, etal: AMPATH-Oncology: A model for comprehensive cancer care in sub-Saharan Africa J Cancer Policy 1:e42–e48,2013 [Google Scholar]
- 16.Ministry of Public Health and Sanitation and Ministry of Medical Services : National Cervical Cancer Prevention Program: Strategic plan 2012-2015 http://www.iccp-portal.org/sites/default/files/plans/National%20Cervical%20Cancer%20Prevention%20Plan%20FINALFeb%202012.pdf
- 17.The Kenya Hospice and Palliative Care Association : Annual Report 2013 http://kehpca.org/wp-content/uploads/Annual-Report-2013_-Final.pdf
- 18.Human Rights Watch 2010 : Needless pain: Government failure to provide palliative care for children in Kenya http://www.hrw.org/sites/default/files/reports/kenya0910webwcover.pdf
- 19.WHO : Proposed list of cancer medicines: Union for International Cancer Control 2014 review of cancer medicines on the WHO List of Essential Medicines http://www.who.int/selection_medicines/committees/expert/20/applications/LIST_CANCER_MEDS.pdf?ua=1
- 20.WHO : Kenya Essential Medicines List 2010 (KEML) http://apps.who.int/medicinedocs/documents/s18694en/s18694en.pdf
- 21.Fontham ET: Infectious diseases and global cancer control CA Cancer J Clin 59:5–7,2009 [DOI] [PubMed] [Google Scholar]
- 22.The World Bank : GDP per capita (current US$): Brazil http://data.worldbank.org/indicator/NY.GDP.PCAP.CD
- 23.Ministério da Saúde, Secretaria de Vigilância em Saúde : Vigitel Brasil 2013: Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico Brasília 2014. http://www.prefeitura.sp.gov.br/cidade/secretarias/upload/saude/arquivos/morbidade/Vigitel-2013.pdf [Google Scholar]
- 24.Malta DC Oliveira TP Luz M, etal: Smoking trend indicators in Brazilian capitals, 2006-2013 Cien Saude Colet 20:631–640,2015 [DOI] [PubMed] [Google Scholar]
- 25.Pan American Health Organization : Cancer in the Americas: Country profiles 2013 http://www.paho.org/hq/index.php?option=com_content&view=category&layout=blog&id=1866&Itemid=3904&lang=pt
- 26.Ferrigno R: Sociedade Brasileira de Radioterapia: Panorama da Radioterapia no Brasil, 2013 http://www.sbradioterapia.com.br/pdfs/panorama2013b.pdf
- 27.Trufelli DC Miranda Vda C Santos MB, etal: [Analysis of delays in diagnosis and treatment of breast cancer patients at a public hospital] Rev Assoc Med Bras 54:72–76,2008 [DOI] [PubMed] [Google Scholar]
- 28.Abdo EN Garrocho Ade A Barbosa AA, etal: Time elapsed between the first symptoms, diagnosis and treatment of oral cancer patients in Belo Horizonte, Brazil Med Oral Patol Oral Cir Bucal 12:E469–E473,2007 [PubMed] [Google Scholar]
- 29.Relacão Nacional de Medicamentos Essenciais : RENAME 2014. 9a edicão, Brasília, DF http://portalsaude.saude.gov.br/images/pdf/2015/maio/06/Rename2014-9ed-data-arquivo-05.05.2015.pdf
- 30.Agencia Nacional de Saúde Suplementar : Começam a valer as novas coberturas dos planos de saúde http://www.ans.gov.br/a-ans/sala-de-noticias-ans/consumidor/2331–a-partir-de-2012014-comecam-a-valer-as-novas-coberturas-dos-planos-de-saude
- 31.Girianelli VR, Gamarra CJ, Azevedo e Silva G: Disparities in cervical and breast cancer mortality in Brazil Rev Saude Publica 48:459–467,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzaga CM Freitas-Junior R Souza MR, etal: Disparities in female breast cancer mortality rates between urban centers and rural areas of Brazil: Ecological time-series study Breast 23:180–187,2014 [DOI] [PubMed] [Google Scholar]
- 33.Chatenoud L Bertuccio P Bosetti C, etal: Trends in cancer mortality in Brazil, 1980-2004 Eur J Cancer Prev 19:79–86,2010 [DOI] [PubMed] [Google Scholar]
- 34.Carrin G Mathauer I Xu K, etal: Universal coverage of health services: Tailoring its implementation Bull World Health Organ 86:857–863,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKee M Balabanova D Basu S, etal: Universal health coverage: A quest for all countries but under threat in some Value Health 16:S39–S45,2013 [DOI] [PubMed] [Google Scholar]
- 36.Diggs SN: Health disparities and healthcare financing: Restructuring the American health care system J Health Care Finance 38:76–90,2012 [PubMed] [Google Scholar]
- 37.Siegel RL, Miller KD, Jemal A: Cancer statistics, 2015 CA Cancer J Clin 65:5–29,2015 [DOI] [PubMed] [Google Scholar]
- 38.Murray CJ Atkinson C Bhalla K, etal: The state of US health, 1990-2010: Burden of diseases, injuries, and risk factors JAMA 310:591–608,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pan American Health Organization : Cancer in the Americas Country Profiles 2013 http://www.uicc.org/sites/main/files/private/Cancer-Country-Profiles-2013-ENG.pdf
- 40.Vineis P, Wild CP: Global cancer patterns: Causes and prevention Lancet 383:549–557,2014 [DOI] [PubMed] [Google Scholar]
- 41.Eheman C Henley SJ Ballard-Barbash R, etal: Annual Report to the Nation on the status of cancer, 1975-2008, featuring cancers associated with excess weight and lack of sufficient physical activity Cancer 118:2338–2366,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murphy SL, Xu JQ, Kochanek KD: Deaths: Final data for 2010. National vital statistics reports; vol 61 no 4. Hyattsville, MD, National Center for Health Statistics, 2013 http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf [PubMed]
- 43.Grubbs SS Polite BN Carney J Jr, etal: Eliminating racial disparities in colorectal cancer in the real world: It took a village J Clin Oncol 31:1928–1930,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aizer AA Falit B Mendu ML, etal: Cancer-specific outcomes among young adults without health insurance J Clin Oncol 32:2025–2030,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Souza JA Yap BJ Hlubocky FJ, etal: The development of a financial toxicity patient-reported outcome in cancer: The COST measure Cancer 120:3245–3253,2014 [DOI] [PubMed] [Google Scholar]
- 46.Ubel PA, Abernethy AP, Zafar SY: Full disclosure: Out-of-pocket costs as side effects N Engl J Med 369:1484–1486,2013 [DOI] [PubMed] [Google Scholar]
- 47.Schilsky RL Michels DL Kearbey AH, etal: Building a rapid learning health care system for oncology: The regulatory framework of CancerLinQ J Clin Oncol 32:2373–2379,2014 [DOI] [PubMed] [Google Scholar]
- 48.Schilsky RL: Moving from evaluation to value in cancer care Clin Cancer Res 21:947–949,2015 [DOI] [PubMed] [Google Scholar]