Chondromyxoid fibroma (CMF) is the rarest benign chondroid tumor, constituting around 0.5% of all bone tumors.[1] CMF is characterized by incomplete cartilaginous differentiation with chondroid, fibrous, and myxoid areas in varying proportions.[1,2] It is found most often in the metaphysis around the knee in the proximal tibia, proximal fibula, or distal femur of patients in their first or second decade of life.[3] The diagnosis becomes difficult if it occurs at unusual sites such as small bones of foot.[4]
A 26-year-old male presented with a painful swelling of the right foot. The swelling had been gradually increasing in size for the last six years. On local examination, there was tenderness over the first metatarsal region of the right foot. There was no discharging sinus.
Radiograph of the right foot showed a well-circumscribed lytic lesion in the head of the first metatarsal bone [Figure 1a]. T1-weighted magnetic resonance imaging of the right foot revealed a lesion with low intensity in the first metatarsal. Fine needle aspiration biopsy (FNAB) was done from the lesion under ultrasound guidance. Smears were moderately cellular with round to ovoid cells embedded in a chondromyxoid matrix [Figure 1b]. The cells had moderate amount of cytoplasm, mild nuclear atypia, and bland chromatin. Few cells with indented nuclei were noted entrapped in the matrix suggestive of chondroblast. Stellate cells and spindle-shaped fibroblast-like cells were also seen [Figure 1c]. Occasional scattered binucleate cells and multinucleated giant cells were observed [Figure 1d]. Based on the cytological findings, a diagnosis of CMF was suggested.
Figure 1.
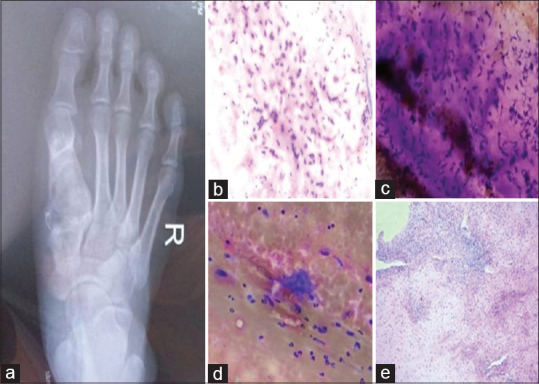
(a) Radiograph of the right foot showed a lytic lesion in the head of the first metatarsal bone. (b) Smears were moderately cellular with round to ovoid cells embedded in a chondromyxoid matrix (H and E, ×100). (c) Stellate cells and spindle-shaped fibroblast-like cells were also seen (MGG stain, ×100). (d) Occasional scattered multinucleated giant cells were observed (MGG stain, 100×). (e) Biopsy showed pseudolobules of myxoid and chondroid tissue separated by zones of fibrous tissue (H and E, ×40)
The patient underwent curettage of the lesion followed by bone grafting. Histopathology of the curettage sample showed pseudolobules of myxoid and chondroid tissue separated by zones of fibrous tissue [Figure 1e]. Mitotic figures were not seen. Thus, the histopathological diagnosis of CMF was confirmed.
The postoperative period was uneventful and the patient was discharged on the sixth postoperative day. The patient had no recurrence after 10 months of follow-up.
CMF is a commonly asymptomatic lesion that is discovered incidentally on radiography.[2] Symptomatic patients present with pain, swelling or tenderness, restrictions of movement, and rarely with pathological fracture.[2,4,5]
The cytological differential diagnosis of CMF includes chondroblastoma, enchondroma, and low-grade chondrosarcoma.[3] Chondroblastomas are epiphyseal, unlike metaphyseal location of CMF.[2] Cytologically, chondroblastomas have a more uniform population of mononuclear cells with round to ovoid nuclei and nuclear grooves compared with a more polymorphic population of ovoid, stellate, and spindle cells found in CMF.[3] Chondromyxoid matrix is also more commonly found in CMF compared with chondroblastomas.[3] True lacunar spaces with chondrocytes are present in enchondroma and chondrosarcoma.[3] The individual cells in chondrosarcoma can be uninucleate or binucleate and show nuclear pleomorphism and frequent mitosis.[4] Immunomarkers are not useful in distinguishing CMF from these entities.[3]
Treatment of CMF in most reported cases consists of intralesional curettage.[5] The recurrence rate after thorough curettage is approximately 25%.[5] Therefore, excision with or without bone grafting is preferred by many investigators.[5]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Siddiqui B, Faridi SH, Faizan M, Sherwani RK. Cytodiagnosis of chondromyxoid fibroma of the metatarsal head: A case report. Iran J Pathol. 2016;11:272–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Armah HB, McGough RL, Goodman MA, Gollin SM, Surti U, Parwani AV, et al. Chondromyxoid fibroma of rib with a novel chromosomal translocation: A report of four additional cases at unusual sites. Diagn Pathol. 2007;2:44. doi: 10.1186/1746-1596-2-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergman S, Madden CR, Geisinger KR. Fine-needle aspiration biopsy of chondromyxoid fibroma: An investigation of four cases. Am J Clin Pathol. 2009;132:740–5. doi: 10.1309/AJCPFJZ8AKMFUAFP. [DOI] [PubMed] [Google Scholar]
- 4.Walke VA, Nayak SP, Munshi MM, Bobhate SK. Cytodiagnosis of chondromyxoid fibroma. J Cytol. 2010;27:96–8. doi: 10.4103/0970-9371.71873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dürr HR, Lienemann A, Nerlich A. Chondromyxoid fibroma of bone. Arch Orthop Trauma Surg. 2000;120:42–7. doi: 10.1007/pl00021214. [DOI] [PubMed] [Google Scholar]


