Abstract
Background
Atopic allergy is a widespread disease with increasing prevalence in the second half of the twentieth century and is most often associated with clinical symptoms, like rhinoconjunctivitis, asthma or eczema. This study explored the prevalence of atopy and polysensitization in nine cohorts of Swiss medical students during the period of 2007–2015. Furthermore, the self-reported allergic symptoms, such as rhinoconjunctivitis, asthma and eczema, among students with and without atopy were assessed.
Methods
Each cohort was assessed in the third study year. Students underwent an ImmunoCAP rapid test, a qualitative point-of-care test, and completed an anonymous questionnaire on age, gender and clinical symptoms including rhinoconjunctivitis, asthma and eczema. Statistical analyses assessed the overall prevalence of atopy in each group and estimated the average annual increase using a linear mixed model. We examined the frequency of occurrence of polysensitization and differences of reported symptoms among students with and without atopy.
Results
Data of 1513 students (mean age 22.4–23.3 years across cohorts) in nine cohorts (median cohort size 215 interquartile range IQR 193–222) were available for analysis. Test results consistent with atopy were present in 39.9% of students. Average increase of atopy over the 9 years of observation was 2.25% (95% CI 0.18–4.31%; p = 0.037). Main drivers for this increase were the ubiquitously available allergens, house dust mite, timothy grass and birch pollen. Atopy and polysensitization were more pronounced in male students: Polysensitization also increased in the observation period. The clinical symptoms, rhinoconjunctivitis, asthma and eczema were reported by 463 (76.7%) atopic and by 141 (15.5%) non-atopic students.
Conclusions
We observed a slight increase of atopy and polysensitization within 9 years of observation in Swiss medical students. The most frequent sensitization occurred with allergens with the highest chance of exposure. Rhinoconjunctivitis, asthma and eczema are a symptom complex associated with atopy but also found in non-atopic students.
Trial registration retrospectively registered by the Cantonal Ethics Committee Zurich on 22.01.2016; Nr: 08-2016
Keywords: Atopy, Time trends of sensitization, Polysensitization
Background
Atopic allergies belong to the most common diseases in the western world and their prevalence in the adult population in central and northern Europe and the United states ranges from about 30% to almost 50% [1–3].
Development of allergies is associated with genetic and environmental factors [4–12].
While atopy increased markedly in the second half of the twentieth century, [13–18] the development of atopy prevalence has been controversially discussed in recent years. Whereas some studies noted a plateauing of this trend for children and adolescents, [19–21] other data documented a further slight increase of atopy prevalence [2, 12, 22, 23]. The mechanism leading to these discordances remains unclear.
In this study we hypothesised that the observed variation was due to the composition of different risk profiles for sensitization of participants that were analysed in the various studies. To examine this hypothesis, the aim of this study was to document the time course of sensitization and polysensitization in a more homogenous selected young adult population with a probable accumulation of risk factors for allergic disorders including higher socio-economic status, good education and urban life [9, 11, 12]. We analyzed the temporal trend of atopy prevalence, sensitization/polysensitization pattern and associated clinical symptoms of 1683 Swiss medical students from nine 3rd year cohorts between 2007 and 2015.
Methods
The local Ethical Review Board of Zurich assessed the protocol of this study and offered a waiver (#8-2016). The study strictly adhered to the principles of good clinical practice and the ethical standards outlined in the Declaration of Helsinki [24]. The reporting guidelines for observational studies (STROBE) were applied [25]. All participants were verbally informed and gave their oral informed consent when in handing in the questionnaire and their blood test results.
Participants
From 2007 to 2015, all third year medical students at the University of Zurich attended the practical course in immunology and were included, forming nine annual cohorts. No exclusion criteria were imposed. In Switzerland, medical students usually study for 6 years after completing secondary school at an age of 18 years on average. Zurich University has the largest medical school in Switzerland with about 220 students per clinical year (followed by Berne, Basel and Lausanne). About 10% of the students come from abroad. The number of inhabitants living in the catchment area for medical students at the University of Zurich is approximately 3 million. This corresponds to about 40 percent of the Swiss population. The proportion of female students has steadily increased and surpassed the 50% margin in 2009.
Data collection
From all participants we secured information on age, gender and clinical symptoms, including rhinoconjunctivitis, asthma and eczema. Each student tested his or her blood during the practical course in immunology using the ImmunoCAP Rapid test kit, a semi-quantitative point-of-care test (Thermo Fisher Scientific Inc, Waltham MA, USA) according to the manufacturer’s instructions and a short film sequence (http://www.phadia.com/en/Products/Allergy-testing-products/ImmunoCAP-Rapid). In addition, senior staff of the University Clinic for Immunology supervised the testing. We entered anonymised personal data and the results from blood tests into an electronic database for statistical analysis.
Specific IgE antibodies against the 10 common aeroallergens cat dander (e1), birch (t3, Betula verrucosa), mugwort (w6, Artemisia vulgaris), timothy grass (g6, Phleum pratense), cockroach (i6, Blatella germanica), dog dander (e5), olive (t9, Olea europaea), wall pellitory (w21, Parietaria judaica), house dust mite (d1, Dermatophagoides pteronyssinus) and mould (m6, Alternaria alternata) were measured. The 2007 test (ImmunoCAP Rapid wheeze/rhinitis child) contained egg white (f1) and cow’s milk (f2) instead of cockroach and mould.
Definition of sensitization and allergic diseases
We define atopy as a sensitization to any of the tested allergens, monosensitization as sensitization to only one allergen, and polysensitization as sensitization to two or more of the tested allergens. Sensitization to olive pollen was interpreted as a sensitization to ash pollen due to a cross-reaction of the sIgE antibodies [26].
We evaluated the frequency of the most common IgE-mediated allergic diseases, namely rhinoconjunctivitis, asthma and eczema [27]. The occurrence of atopic diseases was assessed by self-reported answers to the questions: “Do you suffer from seasonal/perennial rhinoconjunctivitis, asthma or eczema?”. We expected that 3rd year medical students have the required medical knowledge to answer these questions.
Statistical analysis
Interval scaled variates were summarized with means and standard deviations or medians and interquartile ranges (IQR), where appropriate. Dichotomous variates were described as ratios and percentages. We assumed that the composition of students from rural and urban areas and the average socioeconomic status remained constant during the observation period. Under this premise, the nine cohorts were combined for further analysis and an indicator variate was created for each cohort.
The overall prevalence of atopy in each cohort and the average annual increase was assessed using a linear mixed model allowing a random intercept for each cohort. In exploratory analyses we then assessed the temporal changes of ten individual allergens.
We performed all analyses using the Stata 14.2 statistics software package (StataCorp LP, College Station, TX, USA).
Results
From 1683 third-year medical students, the questionnaire and the ImmunoCAP Rapid test result was available in 1513 participants (89.9% of the study population). The median cohort size were 215 students, (interquartile range 193–222) and the proportion of female students ranged from 43.7–62.2%. Mean age ranged from 22.4 to 23.3 years. In ten students, data about gender was missing.
Comparison of cohorts
Atopy was present in 604 (39.9%) participants. The most common allergen in our study population was timothy grass, with a prevalence of 27.5%, followed by house dust mite 17.5%, birch 15.3%, olive/ash 11.8% and cat dander 7%. Sensitization to mugwort, alternaria, parietaria, dog dander and cockroach were less common, with rates below 3% for each. More men than women were atopic (odds ratio (OR) 1.53 (95% CI 1.24–1.89), p < 0.001). Accordingly, males were significantly more sensitized against birch, timothy grass, olive/ash and house dust mite. Of all tested subjects, 22.8% (n = 345) were polysensitized and 17.1% (n = 259) monosensitized. Male subjects were significantly more polysensitized than females (see Tables 1, 3).
Table 1.
Results from the ImmunoCAP rapid test: frequency of atopy and sensitization to different allergens and distribution of non-, mono- and poly-sensitized participants
| Prevalence n = 1513 |
Women n = 856 |
Men n = 647 |
Missing n = 10 |
|
|---|---|---|---|---|
| Atopy | 604 (39.9%) | 305 (35.6%) | 297 (45.9%) | 2 |
| Monosensitization | 259 (17.1%) | 134 (15.7%) | 124 (19.2%) | 1 |
| Polysensitization | 345 (20.5%) | 171 (18.1%) | 173 (26.7%) | 1 |
| Two allergens | 128 (8.5%) | 67 (7.8%) | 61 (9.4%) | |
| Three allergens | 111 (7.3%) | 55 (6.4%) | 56 (8.7%) | |
| ≥ 4 allergens | 106 (7.0%) | 49 (5.7%) | 56 (8.7%) | 1 |
| Cat dander (e1) | 106 (7.0%) | 64 (7.5%) | 41 (6.3%) | 1 |
| Birch (t3) | 231 (15.3%) | 106 (12.4%) | 124 (19.2%) | 1 |
| Mugwort (w6) | 42 (2.8%) | 23 (2.7%) | 19 (2.9%) | |
| Timothy grass (g6) | 416 (27.5%) | 212 (24.8%) | 202 (31.2%) | 2 |
| Cockroach (i6) | 17 (1.1%) | 8 (0.9%) | 9 (1.4%) | 0 |
| Dog dander (e5) | 25 (1.7%) | 17 (2.0%) | 8 (1.2%) | 0 |
| Olive (t9) | 179 (11.8%) | 86 (10.1%) | 93 (14.4%) | 0 |
| Parietaria (w21) | 29 (1.9%) | 12 (1.4%) | 17 (2.6%) | 0 |
| House dust mite (d1) | 265 (17.5%) | 127 (14.8%) | 137 (21.2%) | 1 |
| Mold (Alternaria, m6) | 28 (1.9%) | 13 (1.5%) | 15 (2.7%) | 0 |
Gender information was missing in ten students
Table 3.
Proportion of sensitized students who are polysensitized per year cohort and gender
| Cohort year | Polysensitized male among sensitized male (%) | Polysensitized female among sensitized female (%) |
|---|---|---|
| 2007 | 14 (42.4) | 17 (54.8) |
| 2008 | 24 (61.5) | 16 (53.3) |
| 2009 | 18 (51.4) | 21 (55.3) |
| 2010 | 8 (42.1) | 6 (85.7) |
| 2011 | 32 (72.7) | 33 (60.0) |
| 2012 | 14 (46.7) | 13 (52.0) |
| 2013 | 21 (67.7) | 28 (59.6) |
| 2014 | 15 (68.2) | 9 (42.9) |
| 2015 | 27 (58.7) | 28 (54.9) |
From the 604 atopic students, 76.6% were symptomatic of allergic-related disorders, such as rhinoconjunctivitis, asthma or eczema. The most frequent clinical symptom was seasonal rhinoconjunctivitis (68.2%), followed by asthma (20.8%), eczema (17.9%) and perennial rhinoconjunctivitis (9.4%). From the 909 non-atopic students, 16.9% reported seasonal rhinoconjunctivitis, 3.6% perennial rhinoconjunctivitis, 5.7% asthma and 12.4% eczema (Table 2).
Table 2.
Comparison of reported symptoms among the group of students with vs. without atopy
| Subjects without atopy (n = 909) | Subjects with atopy (n = 604) | p value | |
|---|---|---|---|
| Symptomatic | 141 (15.5%) | 463 (76.6%) | < 0.001 |
| Eczema | 17 (12.4%) | 83 (17.9%) | 0.003 |
| Seasonal rhino-conjunctivitis | 24 (16.9%) | 316 (68.2%) | < 0.001 |
| Perennial rhino-conjunctivitis | 5 (3.6%) | 44 (9.4%) | < 0.001 |
| Asthma | 8 (5.7%) | 96 (20.8%) | < 0.001 |
Time trends
Overall, we observed an average annual 2.25% increase of sensitization (95% CI 2.13–2.36%), p < 0.001. House dust mite, timothy grass- and birch-pollen were responsible for the overall increase. For details, see Fig. 1. The proportion of polysensitization slightly increased during the 9 years of observation and was more pronounced in male subjects compared to women (Table 3; Fig. 2).
Fig. 1.
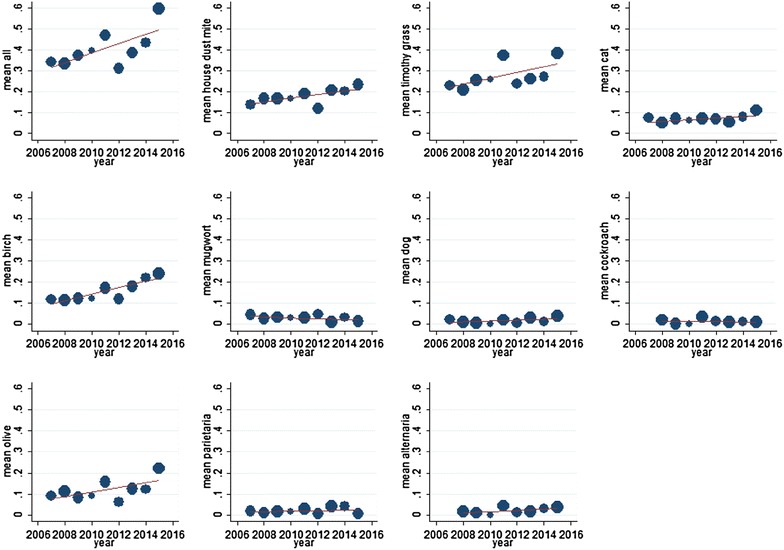
Overall (upper left) and allergen specific trend across the nine cohorts of students, in percentage of the sensitized population. House dust mites, timothy grass- and birch pollen are responsible for the overall increase
Fig. 2.
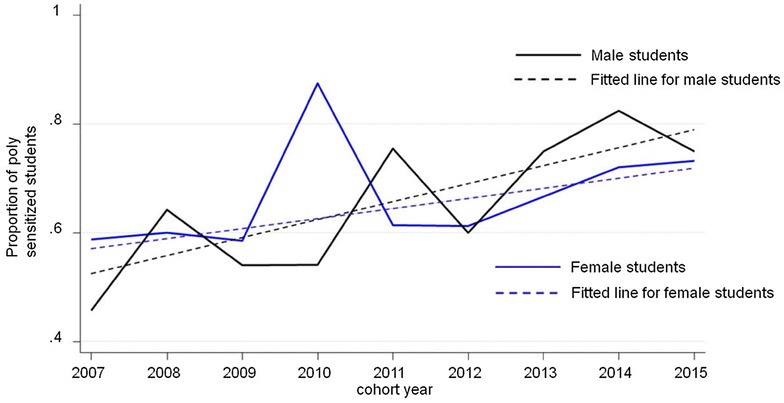
Overall and stratified trend for polysensitization among students with atopy across the nine cohorts from 2007 to 2015
Discussion
In this selected population of Swiss, 3rd year medical students, we were able to document a slight increase of sensitization and polysensitization for common aeroallergens during the 9 years of observation. Timothy grass pollen, house dust mites and tree pollen are the most prevalent allergens and they were the main drivers for the overall increase of sensitization in the described study-population. Compared to cohorts in northern Europe, prevalence of cat dander sensitivity is relatively low. The extent of sensitization in our cohort corresponds to the results found in Germany, the USA, and previous Swiss studies [2, 3, 23, 28, 29]. This is most probably due to climatic distinctions and exposure frequency.
While atopy increased markedly in the second half of the twentieth century, [13, 16–18] data about atopy prevalence have been more controversial in recent years. Some studies indicate a flattening and stabilization of atopy prevalence in Switzerland and other westernized countries [19–21, 30] whereas other data noted a further increase [12, 23, 31]. Our study describes a selected population of highly educated young adults, living predominantly in urban areas with a high social status. All these factors are described to have the potential to increase the risk of developing atopy and allergic diseases [9, 11, 12, 23, 32]. This exposure to several risk factors might explain the slight increase of atopy prevalence in our cohorts over 9 years.
The atopy prevalence of 39.9% and the gender distribution with male subjects suffering more often from atopy and being more often polysensitized than women, is in line with other studies from industrialized countries in central-, and northern Europe, and the United States [2, 3, 28, 29, 33–35]. As documented in other studies, polysensitization is more prevalent than monosensitization [36–38] and more pronounced in men (compare Tables 1, 3). Polysensitization is associated with clinical manifestation of allergic diseases, especially with asthma [38, 39]. Therefore, our findings with an increase of sensitization and polysensitization, in parallel, support an overall increase of symptomatic atopic patients in the described cohorts.
Rhinoconjunctivitis, asthma and eczema are a complex of disorders, which often coexist and therefore seem to have a causal relationship. Normally associated with atopy, this symptom complex also occurs in non-atopic subjects [40] as shown in Table 2.
Strength and limitations
In this study it was possible to compare cohorts with an accumulation of similar risk factors for the development of allergic sensitization and related disorders over several years. The lack of detailed information about the subjects’ genetic background, place of birth, and the time point when sensitization and/or allergic symptoms were first diagnosed is a downside of this study. Therefore, we were unable to explore the extent to which these parameters modified the effects reported here. Arguably, spurious differences in the composition of these parameters across cohorts, which we were unable to correct in the analysis, introduced bias. Nevertheless, due to the lack of an obvious mechanism leading to substantial changes in the composition of cohorts over time, we consider the results valid. Self-reporting of symptoms carry the risk of reporting bias. We cannot fully rule-out that such bias occurred in our study. On the other hand, it can be expected that 3rd year medical students have the necessary medical knowledge to indicate whether they are suffering from seasonal/perennial rhinoconjunctivitis, asthma or eczema.
Conclusions
Our findings suggest that the trend for an increase in atopy prevalence and polysensitization is still on the rise in young adults with certain risk factors. Further investigations in selected cohorts with defined risk factors for atopic diseases could help to elucidate the mechanisms of sensitization. Allergic diseases rhinoconjunctivitis, asthma and eczema are associated with atopy but also coexist in non-atopic subjects.
Authors’ contributions
LS: data collection, analysis and interpretation of the data; writing/critical revision of the manuscript; LMB: statistical analysis, analysis and interpretation of the data, writing/critical revision of the manuscript; SR: introduction of the ImmunoCAP Rapid test kit, data collection, analysis and interpretation of the data, writing/critical revision of the manuscript; EP: introduction of the ImmunoCAP Rapid test kit, analysis and interpretation of the data; writing/critical revision of the manuscript; US: carried out concept and design of the study, data collection; analysis and interpretation of the data, writing/critical revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data
Data are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The local cantonal Ethics Commission Zurich issued a clearance certificate for the publication of this study data.
Funding
No funding.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Elsbeth Probst and Urs C. Steiner shared last authorship
Contributor Information
Lukas Steinegger, Email: lukas.steinegger@spitaeler-sh.ch.
Stephan Regenass, Email: s.regenass@gmail.com.
Lucas M. Bachmann, Email: bachmann@medignition.ch
Elsbeth Probst, Email: Elsbeth.Probst-Mueller@usz.ch.
Urs C. Steiner, Phone: +41 44 255 11 12, Email: urs.steiner@usz.ch
References
- 1.Papadopoulos NG, Agache I, Bavbek S, Bilo BM, Braido F, Cardona V, Custovic A, Demonchy J, Demoly P, Eigenmann P, et al. Research needs in allergy: an EAACI position paper, in collaboration with EFA. Clin Transl Allergy. 2012;2:21. doi: 10.1186/2045-7022-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haftenberger M, Laussmann D, Ellert U, Kalcklosch M, Langen U, Schlaud M, Schmitz R, Thamm M. Prevalence of sensitisation to aeraoallergens and food allergens: results of the German Health Interview and Examination Survey for Adults (DEGS1) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:687–697. doi: 10.1007/s00103-012-1658-1. [DOI] [PubMed] [Google Scholar]
- 3.Salo PM, Arbes SJ, Jr, Jaramillo R, Calatroni A, Weir CH, Sever ML, Hoppin JA, Rose KM, Liu AH, Gergen PJ, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J Allergy Clin Immunol. 2014;134:350–359. doi: 10.1016/j.jaci.2013.12.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–1260. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanaka K, Miyake Y, Kiyohara C. Environmental factors and allergic disorders. Allergol Int. 2007;56:363–396. doi: 10.2332/allergolint.R-07-143. [DOI] [PubMed] [Google Scholar]
- 6.Braun-Fahrlander C, Gassner M, Grize L, Neu U, Sennhauser FH, Varonier HS, Vuille JC, Wuthrich B. Prevalence of hay fever and allergic sensitization in farmer’s children and their peers living in the same rural community. SCARPOL team. Swiss study on childhood allergy and respiratory symptoms with respect to air pollution. Clin Exp Allergy. 1999;29:28–34. doi: 10.1046/j.1365-2222.1999.00479.x. [DOI] [PubMed] [Google Scholar]
- 7.von Mutius E, Vercelli D. Farm living: effects on childhood asthma and allergy. Nat Rev Immunol. 2010;10:861–868. doi: 10.1038/nri2871. [DOI] [PubMed] [Google Scholar]
- 8.Gergen PJ, Turkeltaub PC, Kovar MG. The prevalence of allergic skin test reactivity to eight common aeroallergens in the US population: results from the second National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 1987;80:669–679. doi: 10.1016/0091-6749(87)90286-7. [DOI] [PubMed] [Google Scholar]
- 9.Schafer T, Ruhdorfer S, Weigl L, Wessner D, Heinrich J, Wichmann HE, Ring J. School education and allergic sensitization in adults. Allergy. 2001;56:1206–1210. doi: 10.1034/j.1398-9995.2001.00208.x. [DOI] [PubMed] [Google Scholar]
- 10.Schlaud M, Atzpodien K, Thierfelder W. Allergic diseases. Results from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:701–710. doi: 10.1007/s00103-007-0231-9. [DOI] [PubMed] [Google Scholar]
- 11.D’Amato G, Cecchi L, D’Amato M, Liccardi G. Urban air pollution and climate change as environmental risk factors of respiratory allergy: an update. J Investig Allergol Clin Immunol. 2010;20:95–102. [PubMed] [Google Scholar]
- 12.Bergmann KC, Heinrich J, Niemann H. Current status of allergy prevalence in Germany: position paper of the Environmental Medicine Commission of the Robert Koch Institute. Allergo J Int. 2016;25:6–10. doi: 10.1007/s40629-016-0092-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakagomi T, Itaya H, Tominaga T, Yamaki M, Hisamatsu S, Nakagomi O. Is atopy increasing? Lancet. 1994;343:121–122. doi: 10.1016/S0140-6736(94)90854-0. [DOI] [PubMed] [Google Scholar]
- 14.Linneberg A, Nielsen NH, Madsen F, Frølund L, Dirksen A, Jørgensen T. Increasing prevalence of allergic rhinitis symptoms in an adult Danish population. Allergy. 1999;54:1194–1198. doi: 10.1034/j.1398-9995.1999.00180.x. [DOI] [PubMed] [Google Scholar]
- 15.Downs SH, Marks GB, Sporik R, Belosouva EG, Car NG, Peat JK. Continued increase in the prevalence of asthma and atopy. Arch Dis Child. 2001;84:20–23. doi: 10.1136/adc.84.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Law M, Morris JK, Wald N, Luczynska C, Burney P. Changes in atopy over a quarter of a century, based on cross sectional data at three time periods. BMJ. 2005;330:1187–1188. doi: 10.1136/bmj.38435.582975.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linneberg A, Gislum M, Johansen N, Husemoen LL, Jorgensen T. Temporal trends of aeroallergen sensitization over twenty-five years. Clin Exp Allergy. 2007;37:1137–1142. doi: 10.1111/j.1365-2222.2007.02760.x. [DOI] [PubMed] [Google Scholar]
- 18.Ronmark E, Bjerg A, Perzanowski M, Platts-Mills T, Lundback B. Major increase in allergic sensitization in schoolchildren from 1996 to 2006 in northern Sweden. J Allergy Clin Immunol. 2009;124:357–363. doi: 10.1016/j.jaci.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braun-Fahrlander C, Gassner M, Grize L, Takken-Sahli K, Neu U, Stricker T, Varonier HS, Wuthrich B, Sennhauser FH, Swiss Study on Childhood A et al. No further increase in asthma, hay fever and atopic sensitisation in adolescents living in Switzerland. Eur Respir J. 2004;23:407–413. doi: 10.1183/09031936.04.00074004. [DOI] [PubMed] [Google Scholar]
- 20.Zollner IK, Weiland SK, Piechotowski I, Gabrio T, von Mutius E, Link B, Pfaff G, Kouros B, Wuthe J. No increase in the prevalence of asthma, allergies, and atopic sensitisation among children in Germany: 1992–2001. Thorax. 2005;60:545–548. doi: 10.1136/thx.2004.029561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grize L, Gassner M, Wuthrich B, Bringolf-Isler B, Takken-Sahli K, Sennhauser FH, Stricker T, Eigenmann PA, Braun-Fahrlander C. Trends in prevalence of asthma, allergic rhinitis and atopic dermatitis in 5–7-year old Swiss children from 1992 to 2001. Allergy. 2006;61:556–562. doi: 10.1111/j.1398-9995.2006.01030.x. [DOI] [PubMed] [Google Scholar]
- 22.Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, Williams H. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 23.Warm K, Lindberg A, Lundback B, Ronmark E. Increase in sensitization to common airborne allergens among adults—two population-based studies 15 years apart. Allergy Asthma Clin Immunol. 2013;9:20. doi: 10.1186/1710-1492-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.General Assembly of the World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81:14–18. [PubMed] [Google Scholar]
- 25.Cevallos M, Poole C, von Elm E, Altman D, Egger M. Response to Rezaeian: strengthening the reporting of observational studies in epidemiology (STROBE) extension for ecological studies. J Clin Epidemiol. 2014;67:837–838. doi: 10.1016/j.jclinepi.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Imhof K, Probst E, Seifert B, Regenass S, Schmid-Grendelmeier P. Ash pollen allergy: reliable detection of sensitization on the basis of IgE to Ole e 1. Allergo J Int. 2014;23:78–83. doi: 10.1007/s40629-014-0010-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8:483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 28.Wuthrich B, Schindler C, Leuenberger P, Ackermann-Liebrich U. Prevalence of atopy and pollinosis in the adult population of Switzerland (SAPALDIA study). Swiss study on air pollution and lung diseases in adults. Int Arch Allergy Immunol. 1995;106:149–156. doi: 10.1159/000236836. [DOI] [PubMed] [Google Scholar]
- 29.Pallasaho P, Ronmark E, Haahtela T, Sovijarvi AR, Lundback B. Degree and clinical relevance of sensitization to common allergens among adults: a population study in Helsinki, Finland. Clin Exp Allergy. 2006;36:503–509. doi: 10.1111/j.1365-2222.2006.02460.x. [DOI] [PubMed] [Google Scholar]
- 30.Henriksen L, Simonsen J, Haerskjold A, Linder M, Kieler H, Thomsen SF, Stensballe LG. Incidence rates of atopic dermatitis, asthma, and allergic rhinoconjunctivitis in Danish and Swedish children. J Allergy Clin Immunol. 2015;136(360–366):e362. doi: 10.1016/j.jaci.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Langen U, Schmitz R, Steppuhn H. Prevalence of allergic diseases in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:698–706. doi: 10.1007/s00103-012-1652-7. [DOI] [PubMed] [Google Scholar]
- 32.Lee KS, Rha YH, Oh IH, Choi YS, Choi SH. Socioeconomic and sociodemographic factors related to allergic diseases in Korean adolescents based on the Seventh Korea Youth Risk Behavior Web-based Survey: a cross-sectional study. BMC Pediatr. 2016;16:19. doi: 10.1186/s12887-016-0549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Von Linstow ML, Porsbjerg C, Ulrik CS, Nepper-Christensen S, Backer V. Prevalence and predictors of atopy among young Danish adults. Clin Exp Allergy. 2002;32:520–525. doi: 10.1046/j.0954-7894.2002.01326.x. [DOI] [PubMed] [Google Scholar]
- 34.PausJenssen ES, Cockcroft DW. Sex differences in asthma, atopy, and airway hyperresponsiveness in a university population. Ann Allergy Asthma Immunol. 2003;91:34–37. doi: 10.1016/S1081-1206(10)62055-8. [DOI] [PubMed] [Google Scholar]
- 35.Bousquet J, Anto JM, Bachert C, Bousquet PJ, Colombo P, Crameri R, Daeron M, Fokkens W, Leynaert B, Lahoz C, et al. Factors responsible for differences between asymptomatic subjects and patients presenting an IgE sensitization to allergens. A GA2LEN project. Allergy. 2006;61:671–680. doi: 10.1111/j.1398-9995.2006.01048.x. [DOI] [PubMed] [Google Scholar]
- 36.Arbes SJ, Jr, Gergen PJ, Elliott L, Zeldin DC. Prevalences of positive skin test responses to 10 common allergens in the US population: results from the third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2005;116:377–383. doi: 10.1016/j.jaci.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 37.Bousquet PJ, Castelli C, Daures JP, Heinrich J, Hooper R, Sunyer J, Wjst M, Jarvis D, Burney P. Assessment of allergen sensitization in a general population-based survey (European Community Respiratory Health Survey I) Ann Epidemiol. 2010;20:797–803. doi: 10.1016/j.annepidem.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 38.Toppila-Salmi S, Huhtala H, Karjalainen J, Renkonen R, Makela MJ, Wang DY, Pekkanen J. Sensitization pattern affects the asthma risk in Finnish adult population. Allergy. 2015;70:1112–1120. doi: 10.1111/all.12670. [DOI] [PubMed] [Google Scholar]
- 39.Valero A, Pereira C, Loureiro C, Martinez-Cocera C, Murio C, Rico P, Palomino R, Davila I. Interrelationship between skin sensitization, rhinitis, and asthma in patients with allergic rhinitis: a study of Spain and Portugal. J Investig Allergol Clin Immunol. 2009;19:167–172. [PubMed] [Google Scholar]
- 40.Pinart M, Benet M, Annesi-Maesano I, von Berg A, Berdel D, Carlsen KC, Carlsen KH, Bindslev-Jensen C, Eller E, Fantini MP, et al. Comorbidity of eczema, rhinitis, and asthma in IgE-sensitised and non-IgE-sensitised children in MeDALL: a population-based cohort study. Lancet Respir Med. 2014;2:131–140. doi: 10.1016/S2213-2600(13)70277-7. [DOI] [PubMed] [Google Scholar]


