Abstract
The present study investigated the expression and clinical significance of flavin-containing monooxygenase 5 (FMO5) in colorectal cancer (CRC). The expression of FMO5 was detected by immunohistochemistry in 208 colon cancer tissues and 8 normal colon tissues. Then, the correlations of FMO5 expression with several clinicopathological features were evaluated. FMO5 mRNA expression from The Cancer Genome Atlas dataset was assessed for further validation. In addition, the association of the expression of FMO5 with prognosis was further evaluated by Kaplan-Meier survival curves and Cox proportional hazards model. The FMO5 protein level in colon cancer tissues was significantly higher than that in normal colon tissues (P<0.001). Overexpression of FMO5 was associated with an advanced clinical stage of cancer (P=0.018) and lymph node metastasis (P=0.03). The TCGA dataset also demonstrated that FMO5 was upregulated in CRC with advanced clinical stage (P=0.047), lymph node metastasis (P=0.045) and distant metastasis (P=0.030). The Kaplan-Meier survival curves showed that higher FMO5 mRNA indicated a shorter overall survival in patients with CRC compared with a low expression of FMO5 (P=0.029). Cox proportional hazards regression revealed that a high FMO5 mRNA level served as an independent prognostic factor for patients with CRC (hazard ratio, 2.865; 95% confidence interval, 1.116–7.355; P=0.029). A high expression of FMO5 may serve roles in colorectal carcinogenesis and distant metastasis. FMO5 may be an independent predictive factor for the prognosis of CRC.
Keywords: colorectal cancer, flavin-containing monooxygenase 5, prognosis
Introduction
Colorectal cancer (CRC) is the 3rd most commonly diagnosed cancer and the fourth leading cause of death worldwide (1). The routine prognostic factors for patient survival are histological grade and tumor staging (1,2), which is depending on the depth of tumor invasion, involvement of regional lymph nodes, and metastatic spread to other organs (3). Distinct molecular drivers and prognosis may be implicated in the same stage of CRC patients. Therefore, it is imperative to better understand the carcinogenic and molecular markers of CRC and to identify new therapeutic targets for the treatment of this disease.
The flavonoid monooxygenase family (FMO) includes a large variety of endogenous and exogenous substrates (4). FMO-catalyzed oxygenation usually produces polar and relatively stable, nontoxic products that are easily excreted from the body, allowing FMOs to become an important part of metabolic detoxification (5). Flavin-containing monooxygenase 5 (FMO5) is classified as an oxidoreductase, and it is possible that its effects are mediated through regulation of the cellular redox state. The ability of FMO5 to catalyze a Baeyer-Villiger oxidation reaction was demonstrated in a study of an anticancer therapeutic (6). Bièche et al found that overexpression of FMO5 significantly associated with longer relapse-free survival (RFS) among postmenopausal patients with breast carcinoma (7). Miller et al showed that the overexpression of FMO5 upregulated the expression of progesterone receptor B; Consequently, progesterone enhanced the carcinogenicity of tamoxifen in breast cancer (8). However, the roles of FMO5 in CRC remain to be explored and discussed.
This study aimed to detect the expression of FMO5 in CRC and investigate the correlations between FMO5 expression and clinicopathological characteristics, including prognosis.
Materials and methods
Tissue samples
Tissue microarray (TMA, no. CO2161) was purchased from Alenabio Biotechnology Co., Ltd. (Xian, China), which was constructed from 208 histologically confirmed CRC samples and 8 normal colon tissues. The clinical information of these samples was collected. All human tissues were collected under IRB and HIPPA approved protocols. All samples had tested negative for HIV and hepatitis B and were approved for commercial product development. In addition, we used a publically available dataset: The Cancer Genome Atlas (TCGA) dataset with 192 primary CRC tissues and mRNA sequences.
Immunohistochemistry analysis
Dako Envision Systems (Dako Diagnostics AG, Zug, Switzerland) were applied for immunohistochemistry (IHC) analysis. In short, TMA specimens were blocked with proteolytic digestion and using peroxidase, followed by incubation with 1:50 anti-FMO5 monoclonal antibody (ab189516; Abcam, Cambridge, MA, USA) at 4°C overnight. After washing in PBS, peroxidase-labeled antibodies and substrate chromogen applied to visualize the staining of the target proteins.
Evaluation of immunostaining
TMA slides were scanned using a ScanScope and analyzed using ImageScope v11 software (Aperio Technologies, Vista, CA, USA). Immunostaining was scored by two independent experienced pathologists, who were blinded to the clinicopathological data and clinical outcomes of the patients. Antigen expression was evaluated in a semi-quantitative manner. Each specimen was assessed for staining intensity as follows: Non-significant brown, weak brown, moderate brown, and strong brown staining intensities were scored as 0, 1, 2, and 3, respectively. The percentage of immunoreactive cells was rated as follows: 1 points, <25%; 2 point, 25–50%; 3 points, 50–75%; 4 points, >75%. The immunoreactivity score (IRS) was determined by multiplying intensity and and extent of positivity scores of stained cells. The final scores from the pathologists were compared, and any inconsistencies were were resolved by discussion between these two pathologists. The samples were classified as high (based on an IRS value >4) and low (based on an IRS value ≤4) levels per FMO5 protein expression (Wang et al, 2013).
Statistical analysis
Statistical analyses were performed by means of SPSS 21.0 software (SPSS, Inc., Chicago, IL, USA). Statistical analysis was performed using Pearson's Chi-squared and Fisher's exact tests to compare the relativity of FMO5 expression with clinicopathological characteristics. The Kaplan-Meier method was used to calculate the actual survival rate and to plot survival curves, followed by the log-rank test for clinical and histological variables. Univariate and multivariate Cox proportional hazards models were performed to obtain prognostic factors and corresponding hazard ratios (HRs) for different factors with 95% confidence intervals (CIs). P<0.05 was considered to indicate a statistically significant difference.
Results
High FMO5 protein was associated with aggressive CRC
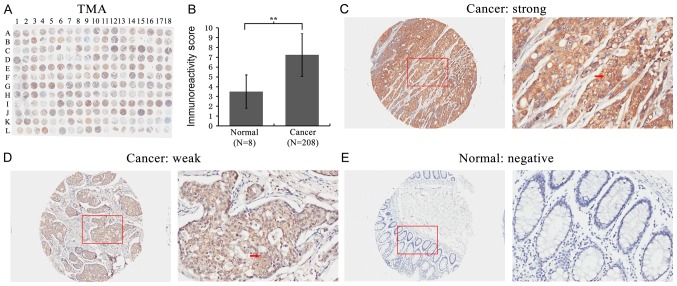
First, FMO5 expression was detected in a TMA using IHC staining (Fig. 1A). We found that the expression of FMO5 significantly increased in CRC compared to that in normal colon tissues (P<0.001) (Fig. 1B). The staining of FMO5 was localized within the cytoplasm of colorectal and normal glandular epithelial cells (Fig. 1C-E).
Figure 1.
Immunohistochemical staining for FMO5 in colon cancer and normal colon tissues. (A) Staining pattern of the TMA section. (B) Immunoreactive score in cancerous tissues was higher than in normal colon tissues (IRS: Normal: 3.50±1.69 vs. cancer: 7.24±2.20, P=0.000). **P<0.01. (C) Images showing a strong FMO5 staining in the cytoplasm of tumor cells. The C is enlarged images of L04 spot. (D) FMO5 expression was weak in the cytoplasm of cancer cells. The D is enlarged images of K04 spot. (E) FMO5 expression was negative in the normal colon tissues. The E is enlarged images of L18 spot. The red arrows in C and D show positively stained cells. Original magnifications, ×100 and ×400. FMO5, flavin-containing monooxygenase 5.
The study further analyzed the correlation between FMO5 expression and clinical or pathological characteristics of the tissues in patients with CRC. Table I showed that the high FMO5 protein expression was associated with older age (P=0.015), advanced clinical stage (P=0.018) and lymph node metastasis (P=0.030). However, no relationship was observed between FMO5 expression and other clinical features, such as gender, pathological grade, tumor invasion, and distant metastasis (all P>0.05). These findings indicated that high levels of FMO5 expression correlated with aggressive clinical features in CRC.
Table I.
Correlation of FMO5 expression with clinico-pathological characteristics of colon cancer.
| TMA | TCGA | ||||||
|---|---|---|---|---|---|---|---|
| Clinical features | Case | Low, n (%) | High, n (%) | P-value | Case | Mean ± SD | P-value |
| Tissue | |||||||
| Cancer | 208 | 44 (21.2) | 164 (78.8) | <0.001 | 192 | 297.70±218.89 | – |
| Normal | 8 | 7 (87.5) | 1 (12.5) | – | |||
| Age (years) | |||||||
| <25 | 2 | 10 (37.0) | 17 (63.0) | 0.015 | 0 | – | 0.529 |
| 25–40 | 27 | 23 (22.6) | 70 (77.4) | 3 | 204.00±26.47 | ||
| 41–60 | 93 | 10 (11.6) | 76 (88.4) | 38 | 52.36±205.20 | ||
| >60 | 86 | 10 (37.0) | 17 (63.0) | 151 | 306.00±224.02 | ||
| Sex | |||||||
| Male | 118 | 23 (19.5) | 95 (80.5) | 0.501 | 94 | 288.88±213.95 | 0.586 |
| Female | 90 | 21 (23.3) | 69 (76.7) | 98 | 306.16±224.30 | ||
| Pathological grade | |||||||
| ≤2 | 150 | 26 (17.3) | 124 (82.7) | 0.090 | – | – | – |
| >2 | 41 | 12 (29.3) | 29 (70.7) | – | – | – | |
| Clinical stage | |||||||
| I–II | 150 | 38 (25.3) | 112 (74.7) | 0.018 | 108 | 326.62±246.68 | 0.047 |
| III–IV | 58 | 6 (10.3) | 52 (89.7) | 81 | 262.37±173.24 | ||
| Tumor invasion | |||||||
| T1-T2 | 23 | 4 (17.4) | 19 (82.6) | 0.790 | 172 | 298.73±256.84 | 0.988 |
| T3-T4 | 185 | 40 (21.6) | 145 (78.4) | 4 | 298.15±208.42 | ||
| Lymph node metastasis | |||||||
| N0 | 153 | 38 (24.8) | 115 (75.2) | 0.030 | 114 | 324.77±242.47 | 0.045 |
| N1–2 | 55 | 6 (10.9) | 49 (89.1) | 77 | 260.16±173.12 | ||
| Distant metastasis | |||||||
| M0 | 197 | 44 (22.3) | 153 (77.7) | 0.125 | 158 | 313.67±230.88 | 0.030 |
| M1 | 11 | 0 (0.0) | 11 (100.0) | 30 | 218.50±131.43 | ||
−, indicates a lack of related information for the patient. The pathological grade of 17 CRC patients from TCGA were unavailable. FMO5, flavin-containing monooxygenase 5; TMA, tissue microarray; TCGA, The Cancer Genome Atlas.
Overexpression of FMO5 mRNA was associated with aggressive CRC in TCGA
FMO5 mRNA expression data of 192 primary CRC patients from TCGA was used to validate the findings of TMA. As shown in Table I, FMO5 was upregulated in CRC with advanced clinical stage (P=0.047), lymph node metastasis (P=0.045), and distant metastasis (P=0.030).
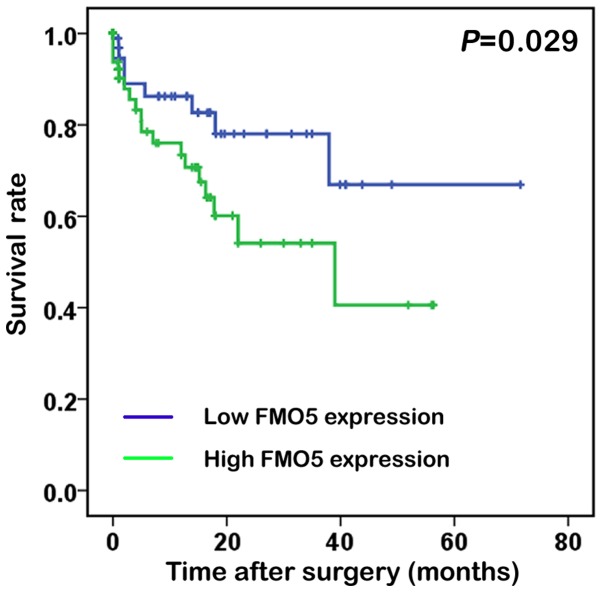
To reveal whether high FMO5 mRNA expression was a prognostic factor in patients with CRC, the Kaplan-Meier survival analysis was performed and K-M curve was plotted for groups classified by high and low FMO5 expression levels (Fig. 2). The mean FMO5 mRNA level in the TCGA dataset was used as a cutoff to segregate patients into high- and low-FMO5 expression groups (9). Interestingly, the overall survival after surgery in the high-FMO5 expression groups were 7.81±12.5 months while in the low-FMO5 expression groups were 8.21±14.1 months. Actually, high FMO5 expression in CRC patients indicated a shorter survival compared with those having low expression (log rank=4.776; P=0.029).
Figure 2.
OS curves of CRC patients with high and low FMO5. OS, overall survival; CRC, colorectal cancer; FMO5, flavin-containing monooxygenase 5.
FMO5 was an independent prognostic factor for the survival of patients with CRC
The study analyzed whether FMO5 expression could predict the prognosis of patients with CRC. Univariate analysis revealed that FMO5 could serve as a valuable prognostic factor for the overall survival rate of patients with CRC (HR, 2.326; 95% CI, 1.062–5.091; P=0.035). Multivariate analysis further revealed that high FMO5 expression served as independent prognostic factor for the overall survival rate of patients with CRC (HR, 2.865; 95% CI, 1.116–7.355; P=0.029), as shown in Table II.
Table II.
Prognostic value of FMO5 expression in OS.
| OS | ||
|---|---|---|
| Variables | HR (95% CI) | P-value |
| Univariate analysis | ||
| Sex (male vs. female) | 0.722 (0.294–1.770) | 0.476 |
| Age, years (≥60 vs. <60) | 2.698 (0.625–11.652) | 0.184 |
| Clinical stage (I–II vs. III–IV) | 1.809 (0.735–4.453) | 0.197 |
| T stage (T1-2 vs. T3-4) | 2.408 (0.555–10.437) | 0.240 |
| N stage (N0 vs. N1-2) | 1.633 (0.674–3.956) | 0.278 |
| M stage (M0 vs. M1) | 2.706 (1.023–7.162) | 0.045 |
| FMO5 expression (low vs. high) | 2.326 (1.062–5.091) | 0.035 |
| Multivariate analysis | ||
| Sex (male vs. female) | 0.573 (0.231–1.426) | 0.231 |
| Age, years (≥60 vs. <60) | 2.451 (0.710–8.464) | 0.156 |
| FMO5 expression (low vs. high) | 2.865 (1.116–7.355) | 0.029 |
FMO5, flavin-containing monooxygenase 5; OS, overall survival; HR, hazard ratio; CI, confidence interval.
Discussion
Research has helped us accumulate extensive knowledge about FMOs since they were founded by Ziegler in the early 1970s (10). FMOs family consists of a group of important drug-metabolizing enzymes, which catalyze oxidation reactions that are complementary to cytochrome P450-mediated biotransformations (11). Among all the isoforms, FMO3 is the primary enzyme in human hepatic metabolism and helps to the metabolism of a variety of common drugs (12). However, recent studies have shown that FMO5 mRNA is almost the same as FMO3 in adult liver and occupy the leading position in the small intestine in humans (13). FMO5 is classified as an oxidoreductase, whose effects are quite likely to be mediated by means of adjusting the cellular redox state. Although highly expression of FMO5 is found in the liver of mice (14) and humans (15), but very little is known about the function of this protein. The knowledge on FMO5 substrates is limited (16–18): Known catalysis of FMO5 are the N-oxygenation of short-chain aliphatic primary amines such as N-octylamine (19) and the S-oxygenation of S-methyl-esonarimod, an active metabolite of the antirheumatic esonarimod (17,20). Sandra found that interindividual variation in FMO5 expression (8,16,21,22) might make contribution to diversity in fat deposits and plasma cholesterol, and some therapeutic agents induced FMO5 expression may have an adverse effect on the patient's metabolic health (23,24). The development of CRC is known to be closely related to diet, lifestyle, and metabolic syndrome. However, the relationship between FMO5 and CRC remains unclear.
This study showed that FMO5 was primarily located in the cytoplasm of CRC epithelial cells, and upregulated in CRC tissues in comparison with that in normal colon tissues by a human TMA containing 208 primary CRCs and 8 normal colon tissues. Moreover, it was found that FMO5 upregulation was associated with advanced clinical stage and lymph node metastasis. Further, these detections were acknowledged in the TCGA dataset, in which significant correlations between FMO5 overexpression and advanced clinical stage, lymph node involvement and distant metastasis were procured. However, no association was found between high FMO5 protein expression and distant metastasis by TMA, which may due to the small sample size as there were only 11 M1 patients. In general, these findings strongly recommended that FMO5 was associated with CRC progression.
Moreover, the correlation between FMO5 mRNA expression and overall survivals of patients were analyzed. The results indicated that patients with high FMO5 expression were found to have a shorter overall survival (P=0.029). The Cox proportional hazards model further showed that overexpression of FMO5 was an independent prognostic factor of poor prognosis for patients with CRC.
The expression of FMO5 should be compared among normal, benign and cancer tissues, which will do help to better and further explore the roles of FMO5 in CRC. And we also expect to investigate the correlations of FMO5 with other putative markers like Kras, p53, Braf, TS. However, these data were unavailable, and we could not investigate these features and relationships. In our future study, we will further investigate such aspects and the molecular characteristics of FMO5.
In conclusion, high FMO5 was associated with aggressive CRC, and may predict shorter survival for patients with CRC. The molecular activities of FMO5 in CRC still require further investigation.
Acknowledgements
This study was supported by the grants from National Natural Science Foundation of China (81272556), Science and Technology Project of Guangdong Province (2014A020212614) and Science and Technology Program of Guangzhou, China (2014Y2-00137).
Glossary
Abbreviations
- FMO5
flavin-containing monooxygenase 5
- CRC
colorectal cancer
- TMA
tissue microarray
- TCGA
The Cancer Genome Atlas
References
- 1.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, Allen C, Hansen G, Woodbrook R, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eyking A, Reis H, Frank M, Gerken G, Schmid KW, Cario E. miR-205 and miR-373 are associated with aggressive human mucinous colorectal cancer. PLoS One. 2016;11:e0156871. doi: 10.1371/journal.pone.0156871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Compton CC. Colorectal carcinoma: Diagnostic, prognostic, and molecular features. Mod Pathol. 2003;16:376–388. doi: 10.1097/01.MP.0000062859.46942.93. [DOI] [PubMed] [Google Scholar]
- 4.Lai WG, Farah N, Moniz GA, Wong YN. A Baeyer-Villiger oxidation specifically catalyzed by human flavin-containing monooxygenase 5. Drug Metab Dispos. 2011;39:61–70. doi: 10.1124/dmd.110.035360. [DOI] [PubMed] [Google Scholar]
- 5.Siddens LK, Krueger SK, Henderson MC, Williams DE. Mammalian flavin-containing monooxygenase (FMO) as a source of hydrogen peroxide. Biochem Pharmacol. 2014;89:141–147. doi: 10.1016/j.bcp.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henderson MC, Siddens LK, Krueger SK, Stevens JF, Kedzie K, Fang WK, Heidelbaugh T, Nguyen P, Chow K, Garst M, et al. Flavin-containing monooxygenase S-oxygenation of a series of thioureas and thiones. Toxicol Appl Pharmacol. 2014;278:91–99. doi: 10.1016/j.taap.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biéche I, Girault I, Urbain E, Tozlu S, Lidereau R. Relationship between intratumoral expression of genes coding for xenobiotic-metabolizing enzymes and benefit from adjuvant tamoxifen in estrogen receptor alpha-positive postmenopausal breast carcinoma. Breast Cancer Res. 2004;6:R252–R263. doi: 10.1186/bcr784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller MM, James RA, Richer JK, Gordon DF, Wood WM, Horwitz KB. Progesterone regulated expression of flavin-containing monooxygenase 5 by the B-isoform of progesterone receptors: Implications for tamoxifen carcinogenicity. J Clin Endocrinol Metab. 1997;82:2956–2961. doi: 10.1210/jcem.82.9.4239. [DOI] [PubMed] [Google Scholar]
- 9.Wang GH, Yao L, Xu HW, Tang WT, Fu JH, Hu XF, Cui L, Xu XM. Identification of MXRA5 as a novel biomarker in colorectal cancer. Oncol Lett. 2013;5:544–548. doi: 10.3892/ol.2012.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cai C, Chen JY, Han ZD, He HC, Chen JH, Chen YR, Yang SB, Wu YD, Zeng YR, Zou J, et al. Down-regulation of dual-specificity phosphatase 5 predicts poor prognosis of patients with prostate cancer. Int J Clin Exp Med. 2015;8:4186–4194. [PMC free article] [PubMed] [Google Scholar]
- 11.Pettit FH, Orme-Johnson W, Ziegler DM. The requirement for flavin adenine dinucleotide by a liver microsmal oxygenase catalyzing the oxidation of alkylaryl amines. Biochem Biophys Res Commun. 1964;16:444–448. doi: 10.1016/0006-291X(64)90373-0. [DOI] [PubMed] [Google Scholar]
- 12.Uetrecht J, Trager W. Drug metabolism chemical and enzymatic aspects. New York: Crc Press; 2007. [DOI] [Google Scholar]
- 13.Zhang J, Cashman JR. Quantitative analysis of FMO gene mRNA levels in human tissues. Drug Metab Dispos. 2006;34:19–26. doi: 10.1124/dmd.105.006171. [DOI] [PubMed] [Google Scholar]
- 14.Krueger SK, Williams DE. Mammalian flavin-containing monooxygenases: Structure/function, genetic polymorphisms and role in drug metabolism. Pharmacol Ther. 2005;106:357–387. doi: 10.1016/j.pharmthera.2005.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janmohamed A, Hernandez D, Phillips IR, Shephard EA. Cell-, tissue-, sex- and developmental stage-specific expression of mouse flavin-containing monooxygenases (Fmos) Biochem Pharmacol. 2004;68:73–83. doi: 10.1016/j.bcp.2004.02.036. [DOI] [PubMed] [Google Scholar]
- 16.Cashman JR, Zhang J. Human flavin-containing monooxygenases. Annu Rev Pharmacol Toxicol. 2006;46:65–100. doi: 10.1146/annurev.pharmtox.46.120604.141043. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez Malagon SG, Melidoni AN, Hernandez D, Omar BA, Houseman L, Veeravalli S, Scott F, Varshavi D, Everett J, Tsuchiya Y, et al. The phenotype of a knockout mouse identifies flavin-containing monooxygenase 5 (FMO5) as a regulator of metabolic ageing. Biochem Pharmacol. 2015;96:267–277. doi: 10.1016/j.bcp.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang J, Cerny MA, Lawson M, Mosadeghi R, Cashman JR. Functional activity of the mouse flavin-containing monooxygenase forms 1, 3 and 5. J Biochem Mol Toxicol. 2007;21:206–215. doi: 10.1002/jbt.20176. [DOI] [PubMed] [Google Scholar]
- 19.Motika MS, Zhang J, Ralph EC, Dwyer MA, Cashman JR. pH dependence on functional activity of human and mouse flavin-containing monooxygenase 5. Biochem Pharmacol. 2012;83:962–968. doi: 10.1016/j.bcp.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Lang DH, Yeung CK, Peter RM, Ibarra C, Gasser R, Itagaki K, Philpot RM, Rettie AE. Isoform specificity of trimethylamine N-oxygenation by human flavin-containing monooxygenase (FMO) and P450 enzymes: Selective catalysis by FMO3. Biochem Pharmacol. 1998;56:1005–1012. doi: 10.1016/S0006-2952(98)00218-4. [DOI] [PubMed] [Google Scholar]
- 21.Ohmi N, Yoshida H, Endo H, Hasegawa M, Akimoto M, Higuchi S. S-oxidation of S-methyl-esonarimod by flavin-containing monooxygenases in human liver microsomes. Xenobiotica. 2003;33:1221–1231. doi: 10.1080/00498250310001624627. [DOI] [PubMed] [Google Scholar]
- 22.Rae JM, Johnson MD, Lippman ME, Flockhart DA. Rifampin is a selective, pleiotropic inducer of drug metabolism genes in human hepatocytes: Studies with cDNA and oligonucleotide expression arrays. J Pharmacol Exp Ther. 2001;299:849–857. [PubMed] [Google Scholar]
- 23.Krusekopf S, Roots I. St. John's wort and its constituent hyperforin concordantly regulate expression of genes encoding enzymes involved in basic cellular pathways. Pharmacogenet Genomics. 2005;15:817–829. doi: 10.1097/01.fpc.0000175597.60066.3d. [DOI] [PubMed] [Google Scholar]
- 24.Overby LH, Carver GC, Philpot RM. Quantitation and kinetic properties of hepatic microsomal and recombinant flavin-containing monooxygenases 3 and 5 from humans. Chem Biol Interact. 1997;106:29–45. doi: 10.1016/S0009-2797(97)00055-0. [DOI] [PubMed] [Google Scholar]