Abstract
Acute myeloid leukemia (AML) is an aggressive bone marrow malignancy where the immature leukemia cells communicate with neighboring cells through constitutive cytokine release and through their cell surface adhesion molecules. The primary AML cells express various integrins. These heterodimeric molecules containing an α and a β chain are cell surface molecules that bind extracellular matrix molecules, cell surface molecules and soluble mediators. The β3 integrin (ITGB3) chain can form heterodimers only with the two α chains αIIb and αV. These integrins are among the most promiscuous and bind to a large number of ligands, including extracellular matrix molecules, cell surface molecules and soluble mediators. Recent studies suggest that the two β3 integrins are important for leukemogenesis and chemosensitivity in human AML. Firstly, αIIb and β3 are both important for adhesion of AML cells to vitronectin and fibronectin. Secondly, β3 is important for the development of murine AML and also for the homing and maintenance of the proliferation for xenografted primary human AML cells, and for maintaining a stem cell transcriptional program. These last effects seem to be mediated through Syk kinase. The β3 expression seems to be regulated by HomeboxA9 (HoxA9) and HoxA10, and the increased β3 expression then activates spleen tyrosine kinase (Syk) and thereby contributes to cytokine hypersensitivity and activation of β2 integrins. Finally, high integrin αV/β3 expression is associated with an adverse prognosis in AML and decreased sensitivity to the kinase inhibitor sorafenib; this integrin can also be essential for osteopontin-induced sorafenib resistance in AML. In the present article, we review the experimental and clinical evidence for a role of β3 integrins for leukemogenesis and chemosensitivity in AML.
Keywords: acute myeloid leukemia, integrin, beta3
1. Introduction
Acute myeloid leukemia (AML) is an aggressive malignancy characterized by the bone marrow infiltration of immature leukemia cells [1,2]. The median age at the time of first diagnosis is 65–70 years, and the only possibility for cure is intensive chemotherapy that may be followed by allogeneic stem cell transplantation [3]. However, even for patients receiving intensive treatment, there is a relatively high risk of chemoresistant relapse, and this treatment is not possible for unfit and elderly patients due to the unacceptable risk of treatment-related mortality. The acute promyelocytic leukemia (APL) variant is an exception, and has a much better prognosis. In this review, the term AML refers to the non-APL variants; for these patients, there is a need for new therapeutic strategies both for the younger and elderly patients.
The bone marrow stromal elements, i.e., extracellular molecules and nonleukemic stromal cells, support leukemogenesis in human AML [4,5,6,7]. The integrins are one of the major families of cell adhesion receptors [8], and may be important for these AML-supporting effects. In the present review, we focus on the β3 integrin subset and their possible role in human AML.
2. The Integrin Family
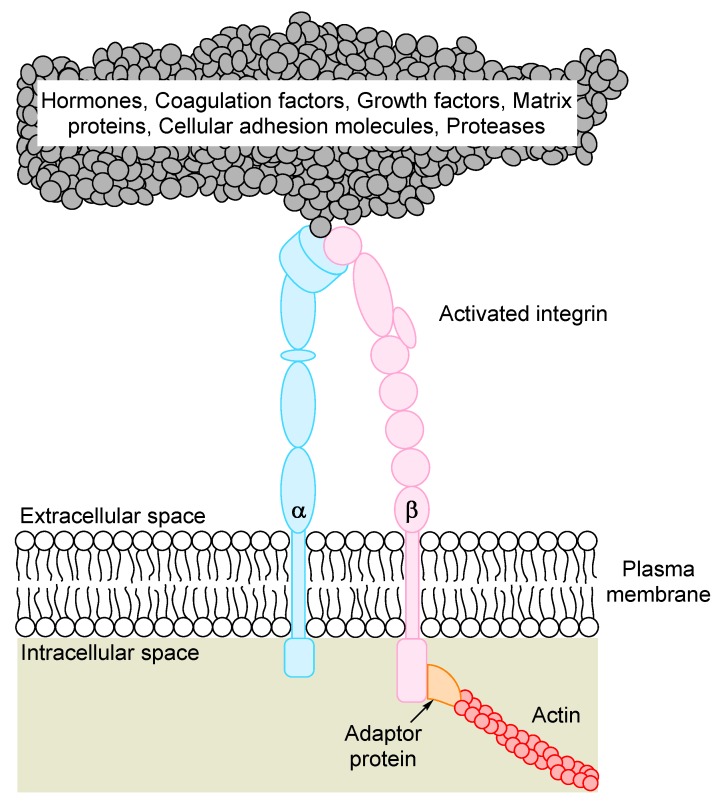
The integrins are non-covalently linked heterodimers containing an α and a β chain, and the dimers function as receptors for extracellular stromal molecules or cell surface molecules (Figure 1) [8,9,10,11,12]. Both subunits are transmembrane proteins containing large extracellular domains, a single transmembrane domain and a small cytoplasmic tail. Mammalian genomes contain 18 α and 8 β subunits, and 24 αβ-dimers have been identified at the protein level. Integrins coordinate the assembly of both cytoskeletal polymers and intracellular signaling complexes, and, on the cell surface, the integrins bind to extracellular matrix molecules or counter-receptors on neighboring cells. These linkages thereby integrate cells with their microenvironment, e.g., AML cells with the extracellular matrix or neighboring nonleukemic cells.
Figure 1.
The integrin heterodimer consisting of one α and one β chain. In its activated state, the heterodimer interacts with the extracellular matrix through binding to large structural proteins such as collagen or fibrinogen, or with receptors on neighboring cells. The short cytoplasmic tail interacts with a vast variety of ligands, with members of the cytoskeleton comprising the largest subgroup. The main classification of ligands is shown at the top of the figure (for details see Table 1).
Adhesion mediated by integrins comprises a diverse family of cellular contacts essential for the organization of individual cells into tissues. The integrin adhesome includes 232 scaffold, cytoskeletal and signaling proteins [41]; 148 of these molecules are referred to as intrinsic proteins that reside within the adhesion site, whereas the remaining 84 components associate transiently with the integrins. A classification of the involved molecules is given in Table 2; it can be seen that the downstream signaling from integrins involves a large number of intracellular molecules with various functions. Several of these molecules can also be involved in carcinogenesis/leukemogenesis, including the guanosine triphosphatase (GTPase) activating proteins and the GTPases.
Table 2.
The integrin adhesome.
| Actin and Actin Regulators (18 Members) |
|---|
| Closely related to the cytoskeleton |
| Adaptor proteins contain a variety of protein-binding modules that link protein-binding partners |
| together and facilitate formation of larger complexes. |
| The integrins are the largest subset of proteins in this group |
| Channel proteins (5 members) |
| Chaperones (3 members) |
| E3 ligases |
| GTPase activating proteins (14 members) |
| Guanine nucleotide exchange factor (16 members) |
| GTPases (6 members) |
| Proteases (4 members) |
| Phosphatidyl inositol (PtdIns) kinases (2 members) |
| PtdIns phosphatases (3 members) |
| RNA or DNA regulation (4 members) |
| Serine/Threonine (Ser/Thr) kinases (10 members) |
| Ser/Thr phosphatases (5 members) |
| Tyrosine (Tyr) kinases (10 members) |
| Tyr phosphatases |
3. The β3 Integrin (ITGB3) Associations with Clinico-Pathological Features in AML
3.1. Regulation of ITGB3 Expression in AML Cells; the Importance of Troponin, PI3K and Monocytic Differentiation
Experimental studies suggest that thrombopoietin increases the activation of αIIbβ3 integrin, and the adhesion of leukemic cells to fibrinogen is thereby increased [13]. This increased binding is caused by recognition of the Arg–Gly–Asp (RGD) sequence on the fibrinogen ligand. The effect is only seen for αIIbβ3, but not for αVβ3 integrins, and signaling through phosphatidylinositol-3-kinases (PI3K) is important for the increased integrin expression/binding. The number of receptors per AML cell seems to be comparable with the expression in carcinoma and endothelial cells, and the leukemia cell levels of both αV and β3 chains seem to increase further in response to induction of monocytic differentiation [42]. Finally, there seems to be a variation in the expression within AML cell populations and a two-fold variation of αIIbβ3 protein expression has been detected even within more homogeneous AML cell line populations [43].
3.2. Associations between ITGB3 Expression and Clinico-Pathological Features
A high expression of ITGB3 at the mRNA level is associated with higher age and chemoresistance, i.e., a higher fraction of these patients with high ITGB3 expression had cytogenetic abnormalities or Fms-like receptor tyrosine kinase 3 (FLT3)-internal tandem duplications (ITD) associated with adverse prognosis [44]. However, these patients had, in addition, lower peripheral blood blast counts, lower blast percentage in the bone marrow and higher peripheral blood platelet counts. Taken together, these observations suggest that high ITGB3 expression is part of a high-risk AML cell phenotype, also characterized by differences with regard to AML cell trafficking (i.e., lower peripheral blood blast count) as well as a different influence on the persisting normal hematopoiesis (i.e., higher levels of circulating platelets) compared with other patients.
αIIbβ3 dimers (i.e., CD41 and CD61) are regarded as markers of megakaryocytic differentiation, as these dimers are expressed by megakaryocytes and platelets [45,46]. This integrin seems to have an increased expression in the uncommon acute megakaryoblastic variant of AML. However, the functional importance of αIIbβ3 may not be limited to the megakaryoblastic variant because αIIb together with α5, β1 and β3 are all important for adhesion of the erythroleukemia cell line (HEL) to vitronectin and fibronectin [47].
4. The Promiscuity of β3 Integrin Ligand Binding
A characteristic of most integrins is their ability to bind a wide variety of ligands; at the same time, many matrix molecules and cell surface adhesion molecules can bind multiple integrin receptors [48]. A classification of the various integrins based on their binding characteristics has been described in detail in a previous review [9], and integrins can be classified into four subsets based on their ligand binding. Both β3 integrins belong to the subgroup of RGD binding integrins, i.e., integrins recognizing ligands containing an RGD tripeptide sequence. These integrins are among the most promiscuous and bind to a large number of ligands, including extracellular matrix and soluble vascular ligands [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Important ligands for the β3 integrins are given in Table 1. It can be seen from the table that many of these ligands are expressed in the bone marrow by various AML-supporting stromal cells, including cells in the stem cell niches. Many of these ligands are known to affect AML cells, but for several of them it is not known whether these effects are mediated through ligation of β3 integrins, other integrins or different receptors.
Table 1.
Classification of β3 integrin ligands and an overview of the importance ligands, their important functions and their integrin binding; for additional details see [9] and the Gene database [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40].
| Ligand | Integri Binding | Function of the Ligand in Human Acute Myeloid Leukemia (AML) | Key References |
|---|---|---|---|
| ADAM family members | αVβ3 | ADAMTS-13, see von Willebrand factor (vWF) below. | |
| Androgens | αVβ3 | A recent study described improved survival of elderly patients when androgens maintenance treatment was combined with intensive chemotherapy. | [14] |
| BSP | αVβ3 | Bone sialo protein (BSP). No known effect in AML. | |
| Collagen | α10β3 | Collagen IV promotes the migration and adhesion of primary human AML cells, MMP-9 is also increased. Collagen and collagen IV is present in human bone marrow. It is not known whether binding to integrins contributes to these effects or whether other receptors are responsible (e.g., the diskoid domain receptor 1). | [15] |
| COMP | αVβ3 | Cartilage oligomeric matrix protein(COMP) This mediator is synthesized by osteoblasts and may thus be expressed in the bone marrow niches. |
[16] |
| Connective tissue growth factor | αVβ3, αIIbβ3 | Connective tissue growth factor (CTGF) is expressed in bone marrow stromal cells; it is regarded as a regulator of adipocyte differentiation and may influence leukemogenesis both through direct effects on the AML cells and through indirect effects on AML-supporting stromal cells. AML cells induce its expression in bone marrow mesenchymal cells. | [17,18] |
| Cyr61 | αIIbβ3, αVβ3 | Cystein-rich 61(Cyr61) is released by stromal cells, it is released as a matricellular protein and it increases the proapoptotic effects of mitoxantrone in AML-stromal cell cocultures. | [19] |
| Del-1 | αVβ3 | The secreted glycoprotein Developmental endothelial locus-1 (Del-1) is expressed endothelial cell, becomes associated with extracellular matrix or cell surfaces and regulates hematopoiesis in the bone marrow stem cell niche. | [20] |
| Fibrillin | αVβ3 | Murine studies have demonstrated that the extracellular matrix protein, fibrillin, is expressed in the bone marrow and functions as a regulator of normal hematopoiesis. | [21] |
| Fibrinogen | αIIbβ3, αVβ3 | The plasma fibrinogen levels at the time of diagnosis seem to have a prognostic impact and are associated with an adverse outcome in AML patients. This impact is not caused by increased early mortality, but it is not known whether this long-term effect is caused by a direct effect of fibrinogen on the AML cells. Both soluble and solid-phase fibrinogen induces Syk signaling in human megakaryoblastic cell lines. | [13,22] |
| Fibronectin | αIIbβ3, αVβ3 | Experimental studies suggest that AML cell adhesion to fibronectin increase leukemia cell proliferation, accelerate S-phase entry and cause accumulation of the cell cycle inhibitor CDC25A. This CDC25A accumulation was caused by decreased degradation. Activation of PI3K-Akt-mTOR seemed to be important for this adhesion-dependent growth enhancement. Fibronectin adhesion inhibited the proliferation of normal CD34+ bone hematopoietic cells. | [23] |
| ICAM-4 | αVβ3, αIIbβ3 | Intercellular adhesion molecule-4 (ICAM-4) is expressed by erythroid cells and seems important in erythropoiesis, but it is not known whether it is important in AML. | [24] |
| L1 | αVβ3, αIIbβ3 | L1 is expressed by human monocytes and may thus be expressed in the bone marrow stem cell niches. | [25] |
| MFG-E8 | αVβ3, αVβ5 | The Milk fat globule-EGF-factor 8 protein (MFG-E8) is expressed and released by bone marrow macrophages and is thus present in the AML cell microenvironment. | [26] |
| MMP-2 | αVβ3 | Matrix metalloprotease 2 (MMP-2) is constitutively released by primary human AML cells for most patients and is involved in AML cell migration; it may even be important for the extracellular migration of leukemic cells. An adverse prognostic impact of constitutive MMP-2 release has been suggested. | [27,28,29] |
| Osteopontin | αVβ3 | Monocytic differentiation in human AML cells seems to be associated with increased expression of both ITGαV and osteopontin. High osteopontin serum levels seem to be associated with an adverse prognosis in human AML, but this impact differs among patients and is most clearly seen for patients with intermediate risk factors. | [30,31,32] |
| PCAM | αVβ3 | Mesenchymal stem cells express Platelet cell adhesion molecule (PCAM); this ligand is thus expressed in the bone marrow stem cell niches where leukemic stem cells locate. | [33] |
| SPARC | αVβ3? | Secreted-Protein-Acidic-Cysteine Rich (SPARC) Seems to induce β3-catenin signaling at least in subsets of human AML. |
[34] |
| Thyroid hormones | αVβ3 | A matched case-control study with 28 children/patients with AML showed that extreme Thyroid stimulating hormone (TSH) levels, both high and low at neonatal screening, were associated with decreased risk of AML | [35] |
| Trombospondin | αVβ3, αIIbβ3 | Thrombospondin induces apoptosis in AML cell lines and also in primary human AML cells, but this effect may be due to ligation of CD36. The effect is antagonized by thrombopoietin, a mediator that is often increased in AML patients receiving intensive chemotherapy. | [36,37] |
| Vitronectin | αIIbβ3, αVβ3 | Adhesion of Mixed lineage leukemia-Eleven-nineteen lysine-rich leukemia (MLL-ELL) murine myeloid progenitor cells to vitronectin activates/phosphorylates β3 integrins and Syk kinase. | [38] |
| vWf | αVβ3, αIIbβ3 | ADAMTS-13 is essential for maintaining the keeping normal sized of the vWF; it cleaves the multimer into smaller forms. Low plasma levels of ADAMTS-13 seems to be associated with an adverse outcome in human AML, but it is not known whether this is due to an effect of ADAMTS-13/vWF directly on the AML cells or whether it represents a secondary reactive mechanism. | [39,40] |
5. β3 Integrins and Spleen Tyrosine Kinase (SYK) Activation in Murine Models of AML
5.1. ITGB3 Shows High Expression in the MLL-AF9 Mouse Model of AML
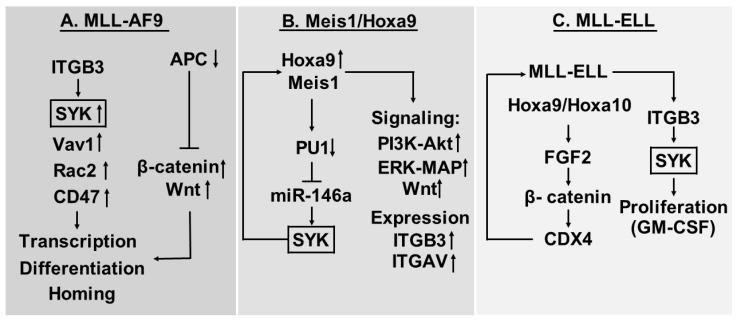
Several MLL translocations transform committed hematopoietic progenitors; one of them, MLL-AF9, is the basis for the MLL-AF9 mouse model of AML (Figure 2A). This leukemia variant depends on Wnt-β-catenin; the negative β-catenin regulator Apc is decreased [49] and at the same time this leukemia is also characterized by high expression of ITGB3 as well as β-catenin (Ctnnb1) and High mobility group box 3 (Hmgb3) [50]. Studies of the intracellular signaling downstream to β3 integrins suggest that Syk, Vav1, Rac2 and CD47 are all activated. However, Syk activation seems to be of particular importance for the effects of ITGB3 on AML cell homing, transcriptional regulation in leukemic stem cells and differentiation induction of the leukemic cells.
Figure 2.
Animal models of AML—a summary of the MLL-AF9 (A), Meis1-HoxA9 (B) and MLL-ELL (C) murine models. For additional details and references, see the text.
As described above, this leukemia is based on an MLL-translocation and is dependent on Wnt-β-catenin signaling. However, several studies have demonstrated that Wnt-β-catenin is important also in AML with other genetic abnormalities, including del(5) [51], t(8;21) [52], normal karyotype AML [53], as well as FLT3-driven AML [52]. This pathway seems important for the survival of AML stem cells, and overexpression of this pathway has been associated with a poor prognosis in human AML [54]. Targeting of Wnt-β-catenin has also been suggested as a possible therapeutic strategy in human AML [55]. Thus, the Wnt-β-catenin pathway seems important for various subsets of AML and not only patients with MLL-translocations, and the possible role of ITGB3 suggested by the observations in this murine AML models may therefore be relevant also for several other AML subsets and not only this specific MLL-variant.
5.2. Myeloid Ectopic (Viral) Insertion Site-1 (Meis1)/Hoxa9 Driven AML Cells Depend on Meis1-Induced Syk Expression and ITGAV/ITGB3 Induced Syk Activation
The importance of Syk was also investigated in another murine AML model where the transcription factor Meis1 drives myeloid leukemogenesis in the context of HomeboxA9 (HoxA9) overexpression (Figure 2B) [56]. In this model Meis1, increased Syk overexpression through a Meis1 dependent feed-back loop: Meis1 acts through downregulation of transcription factor PU1 to increase the expression of mirR-146a that directly increases Syk expression. Syk signaling then induces Meis1 and thereby recapitulates leukemogenic features of the HoxA9/Meis1 driven leukemia. Syk inhibition with disruption of the Meis1/PU1/miR-146a/Syk loop has antileukemic effects and prolongs survival of these mice, even though activation of Wnt is also involved in the cell transformation, and Meis1 also enhances signaling through PI3K/Akt and Mitogen activated protein/extracellular signal-regulated kinase (Erk/MAP) kinase pathways in addition to Syk activation. Finally, additional studies showed that Meis1 increased the expression of both ITGB3 and integrin αV (ITGAV) and thereby upregulates the cell surface levels of this integrin heterodimer [56]. Knock-out studies suggested that the Syk activation was at least partly dependent on ITGB3 also in this model. Thus, a combined action of ITGB3 expression, Wnt signaling and Syk activation seems to be important both in MLL-AF9 and Meis1/HoxA9 driven disease.
Several studies suggest that Meis1/HoxA9 are also important in human AML. Overexpression of HoxA9 is associated with an adverse prognosis and high expression is associated with a variety of genetic abnormalities not only including MLL translocations, but also Nucleoporin98 (NUP98) fusion, Nucleophosmin 1 (NPM1) mutations isocitrate dehydrogenaseIDH mutations, CDX deregulation, MYST translocations, c-AMP response element-binding protein (CREBBP) involving abnormalities and monocytic leukemia zinc finger protein (MOZ) fusions [57,58,59,60]. Meis1/HoxA9 then seem to belong to a set of homeodomain transcription factors associated with adverse prognosis [58,61]. Taken together, these observations suggest that Meis1/HoxA9 are important for various subsets of human AML; the observations in this animal model of AML suggesting a role of β3 integrins in the pathogenesis and in the development of clinical chemoresistance, may therefore be relevant also for human AML.
5.3. Proliferation of AML Cells Expressing the MLL-ELL Fusion Protein is Increased by Cooperation between Fibroblast Growth Factor (FGF) 2 and ITGAV/ITGB3 Integrins
In another experimental murine AML model, the MLL-ELL fusion protein activates aberrant expression of HOX genes (Figure 2C) [38,62]. HoxA9 and HoxA10 then increase the expression of the FGF2 gene, and the autocrine stimulation by FGF2 stabilizes β-catenin that increases the expression of CDX4; this last mediator targets HoxA9 and HoxA10 and thereby augments the effect of the MLL-ELL fusion protein. Thus, the autocrine FGF2 stimulation is a part of a MLL-ELL initiated loop including MLL-ELL, HoxA9 and HoxA10/FGF2/β-catenin/CDX4 and then back to HoxA9 and HoxA10. The MLL-ELL fusion protein also increased ITGB3 expression and activation of the αVβ3 integrin that caused integrin-mediated Syk activation leading to increased proliferative responsiveness to Granulocyte macrophage colony stimulating factor (GM-CSF). Taken together, the observations in this experimental model also support a role of the αVβ3 integrin and its activation of Syk in leukemogenesis.
6. The Role of αVβ3 Integrins Human AML
6.1. HOX Genes and β-Catenin
The M9 cells are a human model of MLL-AML; these cells were derived from umbilical cord blood cells transduced with the MLL-ELL oncogene [56]. These cells express β3 integrins, and transplantation of these cells into immunocompromised mice showed that β3 integrins were important for later development of leukemia. Furthermore, ITGB3/ITGAV is also expressed by primary human AML cells both with and without MLL-rearrangement [56], and xenografting experiments suggest that the β3 integrins were then important for engraftment and thereby disease development both in patients with and without MLL rearrangements. These observations suggest that β3 integrins are important also for human disease development both in MLL and non-MLL variants of AML.
Previous studies of murine AML suggest that HoxA9/HoxA10 are involved in leukemogeneisis through their effects on the expression/activation of αVβ3 integrins and Syk (Figure 2B,C) [38]. Furthermore, studies of human AML suggest that HOX genes can be important in human leukemogenesis, and high HOX expression seems to identify a distinct subset of patients [63,64]. Similar to the murine AML models described above [38], HOX expression seems to be associated with increased expression of FGF2, αVβ3 integrins and CDX4 compared with normal hematopoietic cells. The AML patients showing the highest HOX expression also show the highest levels of FGF2, αVβ3 and CDX4, and this subset of patients with the highest expression are also characterized by a higher proliferative response to exogenous GM-CSF and a stronger antiproliferative effect of FGF2/Syk inhibition [38]. Thus, the HOX/FGF2/β-catenin/CDX4 and the HOX/αVβ3/Syk cooperation first identified in murine models of AML seems important also in human leukemogenesis at least for a subset of AML patients that mainly includes patients with intermediate cytogenetics [63].
The role of β-catenin was further investigated in a recent study [44] describing an association between ITGB3 expression and survival in human AML (see Figure 2A,B). This association was seen especially for patients with normal cytogenetics and FLT3-ITD. The authors also presented experimental evidence for a role of αVβ3 in osteopontin-induced chemoresistance in FLT3-ITD AML, and this seemed to be caused by activation of the αVβ3/PI3K/Akt/glycogen synthase kinase-3 β (GSK3-β)/β-catenin pathway. These observations further support that the cooperation between HOX/FGF2/β-catenin/CDX4, HOX/αVβ3/Syk and αVβ3/PI3K/Akt/GSK3-β/β-catenin is important for leukemogenesis and probably also chemosensitivity in human AML.
6.2. Modulation of Syk and Focal Adhesion Kinase (FAK) Activation by β3 Ligation
The two β3 integrins can bind a wide range of ligands, and the downstream activation of the nonreceptor protein tyrosine kinases Syk and FAK is in addition dependent on how the ligand is presented to the integrin [13]. This has been clearly demonstrated by fibrinogen; an experimental study of a megakaryoblastic leukemic cell line showed that soluble fibrinogen caused tyrosine-phosphorylation of Syk but a dephosphorylation of FAK whereas solid-phase fibrinogen caused immediate FAK phosphorylation followed by delayed Syk phosphorylation. A combined soluble and solid phase fibrinogen exposure caused tyrosine phosphorylation of the β3 and at the same time complex formation with Syk; the further translocation of Syk to the cytoskeleton seems to be a two-step process and one of these later steps is also β3 dependent [65].
The importance of FAK in human AML is summarized in Table 3. Several studies have described a role of FAK in the regulation of proliferation, chemoresistance and migration of human AML cells [66,67,68,69,70]. Even though these studies suggest that the functional interactions between upstream β3 integrins and FAK has a clinical relevance, additional studies are definitely needed to clarify the possible importance of β3 integrins initiated signaling for the role of FAK expression and activation in human AML. However, the observed association between FAK activation and β3 integrin expression suggest that these integrins contribute involved in FAK activation.
Table 3.
The role of the non-receptor tyrosine kinase, focal adhesion kinase (FAK), in human AML.
|
6.3. Clinical Evidence for a Role of β3 Integrins in Human AML; the Stories of SPARC and TRIM62
The secreted-protein-acidic-cysteine-rich (SPARC) encodes the matricellular protein osteonectin that has both intracellular and extracellular functions including regulation of the growth factor families transforming growth factor β (TGFβ), FGF, vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF); a recent study described that the overexpression of this protein independently predicted an adverse outcome in patients with normal karyotype AML [34]. However, its prognostic impact may depend on the biological or genetic context because AML with MLL rearrangements is also associated with an adverse prognosis, but shows downregulated SPARC, and increased levels have been described for the favorable AML variants with t(8;21) and inv(16) (for references see [34]). Experimental studies suggested that the increased SPARC expression was mediated by SP1/NFκB/miR-29b, and the secreted SPARC activated the integrin-linked kinase-Akt-GSK3β pathway. GSK3β will induce degradation of β-catenin, and GSK3β inactivation through the Akt-mediated phosphorylation will thereby increase β-catenin levels. Thus, these observations also support the hypothesis that integrin/β-catenin signaling is important for leukemogenesis and/or chemosensitivity at least in subsets of AML patients.
Tripartite motif-62 (TRIM62) is a putative tumor suppressor gene, and low expression of this mediator has been associated with adverse prognosis and shorter remission duration, event-free survival and overall survival in patients with intermediate-risk cytogenetics [71]. In this study, age and TRIM62 levels were the most powerful independent prognostic factors. However, among the proteins that were most strongly downregulated in patients with low TRIM62 (i.e., adverse prognosis) were both the integrin-β3 dimers (associated with adverse prognosis previously [44]) and their ligand fibronectin.
Taken together these two studies suggest that β3 integrin expression has a prognostic impact in AML patients receiving intensive therapy, but this impact seems to differ between patient subsets.
7. β3-Integrins, Intracellular Signaling and Transcriptional Regulation—A Summary of Our Current Evidence
The present evidence from animal models as well as human studies described above suggest that β3-integrin initiates downstream signaling that alters transcriptional regulation. Several pathways seem to be involved, and the most important observations are summarized below:
The extracellular SPARC molecule may be important for regulation of cytokine responses (e.g., FGF2 and possibly GM-CSF responses) and thereby interact with the functional effects of β3-integrin signaling.
Several cell surface molecules seem to be important for the signaling, including CD47 and β-catenin; this last protein has a dual function and is important both for cell adhesion and transcriptional regulation. Another cell surface proteins being important for the signaling is CD47.
Syk seems to be an important downstream mediator, possibly the most important.
However, several pathways seem to be involved, including Wnt-signaling, PI3K-Akt, and Erk-MAP. The importance of Vav1 (guanine nucleotide exchange factor) and Rac2 (a GTPase) in the MLL-AF9 model also suggest that G-protein dependent signaling may be involved.
Several transcriptional regulators also seem to be involved, including β-catenin, Meis1, miR-146a, PU1, HoxA9, HoxA10 and CDX4.
Thus, several cell surface molecules, intracellular pathways and transcriptional regulators are important for the function of β3 integrins in human AML. The contribution of each molecule/mediator seems to depend on the biological context/experimental model, and this last observation suggests that their importance may also differ between biologically heterogeneous AML patients.
8. The Soluble Isoform of β3 Integrins
Alternative splicing is an important mechanism to increase the functional diversity of integrins, and a soluble β3 (sβ3) variant has been detected in the serum for a subset of AML patients [72]. This variant represents an alternatively spliced and truncated variant. Additional studies showed that this sβ3 integrin increased natural killer (NK) cell proliferation, interleukin-2 (IL2)-induced NK cell release of interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α), NK cell expression of granzyme B and Fas ligand and NK cell cytotoxicity. This included increased cytotoxicity against AML cells that was probably caused by a combined effect of the cytokine release, Fas-induced apoptosis and increased cytotoxic capacity.
Antileukemic immune reactivity is especially important in AML patients treated with allogeneic stem cell transplantation, and the NK cells seem to contribute to this reactivity [73]. The capacity of primary AML cells to release sβ3 integrins may therefore be important for the posttransplant antileukemic effects mediated by the graft or donor NK cells, and it may also contribute to patient heterogeneity with regard to the efficiency of the posttransplant antileukemic immune reactivity.
9. The Possible Importance of Cooperation between Different Integrins
Experimental studies of normal leukocytes suggest that the function of one integrin can be regulated by another integrin. Several examples are known: α5β2 ligation activates α2β1 integrins in monocytes and β3 ligation can activate the function of αMβ2 integrin. However, αVβ3 can also inhibit the function of α5β1 in the human AML cell line K562 [74,75,76] and this last αVβ3 effect does not seem to be a direct interaction between the two types of integrins but rather a crosstalk at the intracellular signaling level. Most studies of integrins in human AML have focused on one or only a few integrins, and future studies should probably further address the question whether the integrin profile is more important than single integrin expression. Previous studies suggest that β1 integrins are important in human AML, and it will therefore be particularly important to investigate the possible crosstalk between β3 and β1 integrins in human AML [77,78,79,80].
10. Summarizing and Concluding Comments
Several integrins are expressed by primary human AML cells, and previous studies have shown that they can be used together with other molecules as markers for leukemia cell differentiation and thereby as markers for identification of patient subsets. More recent studies have lately shown that at least certain integrins or their downstream mediators are potential therapeutic targets in AML.
The integrin family consists of 24 heterodimers that can bind to a wide range of ligands expressed on the surface of neighboring cells or by extracellular matrix molecules. Many of them are expressed by primary human AML cells, including the two β3 integrins αIIbβ3 and αVβ3 integrins. β3 integrins and especially αVβ3 seem to be important for disease development and chemosensitivity in human AML at least for certain subsets of patients, including patients with MLL translocations. Furthermore, the integrin interactome consists of a large number of intracellular mediators, but especially β-catenin, the Syk kinase and several HoxA genes seem to be important together with the FGF2 receptor for the downstream signaling of β3 integrins in human AML cells. Thus, Syk inhibition as well as β3-specific antibody blocking may be a possible strategy for inhibition of AML-supporting signaling circuits.
The β3 integrins show downstream crosstalk with other integrins as well as other intracellular signaling pathways. This includes both PI3K-Akt and NFκB signaling as well as certain β1 integrins. Thus, combination of β3-inhibition and other targeted therapies may become possible. There may also be a crosstalk with the chemokine system and intracellular signaling initiated by chemokine receptors [70,78].
Integrins seem to be important for the development of chemoresistance in human AML. Firstly, galectin 1 seems to induce sorafenib-resistance in hepatocellular carcinoma through induction of αvβ3 integrin expression and activation of PI3K-Akt signaling [81]. Galectin-1 is also expressed in human AML bone marrow both by the leukemic cells and by stromal cells in the stem cell niches [82,83]. A recent study could not find any association between galectin expression in primary human AML cells and prognosis after conventional chemotherapy, but further studies are needed to clarify whether galectin-1 dependent chemoresistance is important for subsets of patients or for kinase inhibitory strategies. Secondly, α3 integrins as well as expression of the downstream FAK seem to be important for development of sorafenib resistance in hepatocellular carcinomas and mantle cell lymphoma [84,85]; αvβ3 integrin may then influence these mechanisms through the crosstalk between various integrin heterodimers (see above).
The possibility of using inhibition of β3 integrins in future AML treatment should thus be considered. However, a further characterization especially of patient heterogeneity with regard to integrin expression profile and integrin crosstalk is needed to clarify whether this therapeutic strategy will be effective only in certain patients. The β3 integrins are very promiscuous with regard to binding of various ligands (Table 1), and future studies have to address whether the binding of certain ligands is especially important in AML. Finally, it will be necessary to further investigate whether this therapeutic approach can be combined with conventional cytotoxic therapy or other targeted therapies before an optimal design of future clinical studies will be possible.
Acknowledgments
The study was supported by Øyvinn Mølbach-Petersen’s foundation, Helse Vest, University of Bergen and the Norwegian Cancer Society.
Abbervations
| AML | Acute myelogen leukemia |
| APL | Acute promyelocytic leukemia |
| COMP | Cartilage oligomeric matrix protein |
| CREBBP | CREB binding protein |
| CTGF | Connective tissue growth factor |
| Cyr61 | Cystein-rich61 |
| Ctnnb1 | β–catenin |
| CXCR4 | CXC chemokine receptor 4 |
| Del-1 | Developmental endothelial locus-1 |
| ELL | Eleven-nineteen lysine-rich leukemia |
| FAK | Focal adhesion kinase |
| FLT3 | Fms-like receptor tyrosin kinase 3 |
| GSK3-β | Glycogen synthase kinase-3 β |
| GTPase | Guanosine triphosphatase |
| GM-CSF | Granulocyte-macrophage colony-stimulatingfactor |
| HEL | Erythroleukemia cell line |
| HoxA9 | Homebox A9 |
| Hmgb3 | High mobility group box 3 |
| ICAM-4 | Intercellular adhesion molecule-4 |
| IL2 | Interleukin-2 |
| IFN-γ | Interferon-γ |
| ITD | Internal tandem duplications |
| ITGAV | Integrin αV |
| ITGB3 | Beta3 intergrin |
| MAP/ERK | Mitogen activated protein/extracellular signal-regulated kinase |
| MEIS1 | Myeloid ectopic (viral) insertion site-1 |
| MFG-E8 | Milk fat globule-EGF-factor 8 protein |
| MLL | Mixed lineage leukemia |
| MMP-2 | Matrixmetalloprotease 2 |
| MOZ | Monocytic leukaemia zinc finger protein |
| NK | Natural killer (cell) |
| NPM1 | Nucleophosmin 1 |
| NUP98 | Nucleoporin98 |
| PDGF | Platelet derived growth factor |
| PCAM | Platelet cell adhesion molecule |
| PtdIns | Phosphatidyl inositol |
| PI3K | Phosphatidylinositol-3-kinases |
| RGD | Arg-Gly-Asp |
| Ser/Thr | Serine/Threonine |
| S β3 | Soluble β3 |
| SPARC | Secreted-Protein-Acidic-Cysteine Rich |
| STAT5 | Signal transducer and activator of transcription-5 |
| SYK | Spleen tyrosin kinase |
| TGF-β | Transforming growth factor-β |
| TNF-α | Tumor necrosis factor-α |
| TRIM62 | Tripartite motif-62 |
| TSH | Thyroid stimulating hormon |
| Tyr | Tyrosine |
| VEGF | Vascular endothelial growth factor |
| vWF | Von Willebrand Factor |
Conflict of Interests
The authors report none conflict of potential interest.
References
- 1.Arber D.A., Orazi A., Hasserjian R., Thiele J., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 revision to the world health organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 2.Döhner H., Weisdorf D.J., Bloomfield C.D. Acute myeloid leukemia. N. Engl. J. Med. 2015;373:1136–1152. doi: 10.1056/NEJMra1406184. [DOI] [PubMed] [Google Scholar]
- 3.Döhner H., Estey E., Grimwade D., Amadori S., Appelbaum F.R., Buchner T., Dombret H., Ebert B.L., Fenaux P., Larson R.A., et al. Diagnosis and mrnaanagement of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–447. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenner A.K., Nepstad I., Bruserud O. Mesenchymal stem cells support survival and proliferation of primary human acute myeloid leukemia cells through heterogeneous molecular mechanisms. Front. Immunol. 2017;8:106. doi: 10.3389/fimmu.2017.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reikvam H., Brenner A.K., Hagen K.M., Liseth K., Skrede S., Hatfield K.J., Bruserud O. The cytokine-mediated crosstalk between primary human acute myeloid cells and mesenchymal stem cells alters the local cytokine network and the global gene expression profile of the mesenchymal cells. Stem Cell Res. 2015;15:530–541. doi: 10.1016/j.scr.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Ito S., Barrett A.J., Dutra A., Pak E., Miner S., Keyvanfar K., Hensel N.F., Rezvani K., Muranski P., Liu P., et al. Long term maintenance of myeloid leukemic stem cells cultured with unrelated human mesenchymal stromal cells. Stem Cell Res. 2015;14:95–104. doi: 10.1016/j.scr.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim J.A., Shim J.S., Lee G.Y., Yim H.W., Kim T.M., Kim M., Leem S.H., Lee J.W., Min C.K., Oh I.H. Microenvironmental remodeling as a parameter and prognostic factor of heterogeneous leukemogenesis in acute myelogenous leukemia. Cancer Res. 2015;75:2222–2231. doi: 10.1158/0008-5472.CAN-14-3379. [DOI] [PubMed] [Google Scholar]
- 8.Hynes R.O. Integrins: Bidirectional, allosteric signaling machines. Cell. 2002;110:673–687. doi: 10.1016/S0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 9.Humphries J.D., Byron A., Humphries M.J. Integrin ligands at a glance. J. Cell Sci. 2006;119:3901–3903. doi: 10.1242/jcs.03098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnaout M.A., Mahalingam B., Xiong J.P. Integrin structure, allostery, and bidirectional signaling. Annu. Rev. Cell Dev. Biol. 2005;21:381–410. doi: 10.1146/annurev.cellbio.21.090704.151217. [DOI] [PubMed] [Google Scholar]
- 11.Springer T.A., Wang J.H. The three-dimensional structure of integrins and their ligands, and conformational regulation of cell adhesion. Adv. Protein Chem. 2004;68:29–63. doi: 10.1016/S0065-3233(04)68002-8. [DOI] [PubMed] [Google Scholar]
- 12.Barczyk M., Carracedo S., Gullberg D. Integrins. Cell Tissue Res. 2010;339:269–280. doi: 10.1007/s00441-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tohyama Y., Tohyama K., Tsubokawa M., Asahi M., Yoshida Y., Yamamura H. Outside-in signaling of soluble and solid-phase fibrinogen through integrin alphaiibbeta3 is different and cooperative with each other in a megakaryoblastic leukemia cell line, cmk. Blood. 1998;92:1277–1286. [PubMed] [Google Scholar]
- 14.Pigneux A., Bene M.C., Guardiola P., Recher C., Hamel J.F., Sauvezie M., Harousseau J.L., Tournilhac O., Witz F., Berthou C., et al. Addition of androgens improves survival in elderly patients with acute myeloid leukemia: A goelams study. J. Clin. Oncol. 2017;35:387–393. doi: 10.1200/JCO.2016.67.6213. [DOI] [PubMed] [Google Scholar]
- 15.Favreau A.J., Vary C.P., Brooks P.C., Sathyanarayana P. Cryptic collagen IV promotes cell migration and adhesion in myeloid leukemia. Cancer Med. 2014;3:265–272. doi: 10.1002/cam4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C.J., Prazak L., Fajardo M., Yu S., Tyagi N., Di Cesare P.E. Leukemia/lymphoma-related factor, a POZ domain-containing transcriptional repressor, interacts with histone deacetylase-1 and inhibits cartilage oligomeric matrix protein gene expression and chondrogenesis. J. Biol. Chem. 2004;279:47081–47091. doi: 10.1074/jbc.M405288200. [DOI] [PubMed] [Google Scholar]
- 17.Battula V.L., Chen Y., Cabreira Mda G., Ruvolo V., Wang Z., Ma W., Konoplev S., Shpall E., Lyons K., Strunk D., et al. Connective tissue growth factor regulates adipocyte differentiation of mesenchymal stromal cells and facilitates leukemia bone marrow engraftment. Blood. 2013;122:357–366. doi: 10.1182/blood-2012-06-437988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheung L.C., Strickland D.H., Howlett M., Ford J., Charles A.K., Lyons K.M., Brigstock D.R., Goldschmeding R., Cole C.H., Alexander W.S., et al. Connective tissue growth factor is expressed in bone marrow stromal cells and promotes interleukin-7-dependent B lymphopoiesis. Haematologica. 2014;99:1149–1156. doi: 10.3324/haematol.2013.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Long X., Yu Y., Perlaky L., Man T.K., Redell M.S. Stromal CYR61 confers resistance to mitoxantrone via spleen tyrosine kinase activation in human acute myeloid leukaemia. Br. J. Haematol. 2015;170:704–718. doi: 10.1111/bjh.13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitroulis I., Chen L.S., Singh R.P., Kourtzelis I., Economopoulou M., Kajikawa T., Troullinaki M., Ziogas A., Ruppova K., Hosur K., et al. Secreted protein Del-1 regulates myelopoiesis in the hematopoietic stem cell niche. J. Clin. Investig. 2017;127:3624–3639. doi: 10.1172/JCI92571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smaldone S., Bigarella C.L., Del Solar M., Ghaffari S., Ramirez F. Fibrillin-1 microfibrils influence adult bone marrow hematopoiesis. Matrix Biol. 2016;52–54:88–94. doi: 10.1016/j.matbio.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger M.D., Heini A.D., Seipel K., Mueller B., Angelillo-Scherrer A., Pabst T. Increased fibrinogen levels at diagnosis are associated with adverse outcome in patients with acute myeloid leukemia. Hematol. Oncol. 2016 doi: 10.1002/hon.2307. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez-Vidal A., Ysebaert L., Didier C., Betous R., De Toni F., Prade-Houdellier N., Demur C., Contour-Galcera M.O., Prevost G.P., Ducommun B., et al. Cell adhesion regulates CDC25A expression and proliferation in acute myeloid leukemia. Cancer Res. 2006;66:7128–7135. doi: 10.1158/0008-5472.CAN-05-2552. [DOI] [PubMed] [Google Scholar]
- 24.Lee G., Lo A., Short S.A., Spring F., Parsons S.F., Yazdanbakhsh K., Mohandas N., Anstee D.J., Chasis J.A. Targetes gene deletion demonstrates that the cell adhesion molecule ICAM-4 is critical for erythroblastic island foramtion. Blood. 2006;15:2064–2071. doi: 10.1182/blood-2006-03-006759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ebeling O., Duczmal A., Aigner S., Geiger C., Schollhammer S., Kemshead J.T., Moller P., Schwartz-Albiez R., Altevogt P. L1 adhesion molecule on human lymphocytes and monocytes: Expression and involvement in binding to alpha v beta 3 integrin. Eur. J. Immunol. 1996;26:2508–2516. doi: 10.1002/eji.1830261035. [DOI] [PubMed] [Google Scholar]
- 26.Lee J., Choi B.I., Park S.Y., An S.Y., Han J., Kim J.H. Fetal hematopoietic stem cells express MFG-E8 during mouse embryogenesis. Exp. Mol. Med. 2015;47:e174. doi: 10.1038/emm.2015.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reikvam H., Hatfield K.J., Oyan A.M., Kalland K.H., Kittang A.O., Bruserud O. Primary human acute myelogenous leukemia cells release matrix metalloproteases and their inhibitors: Release profile and pharmacological modulation. Eur. J. Haematol. 2010;84:239–251. doi: 10.1111/j.1600-0609.2009.01382.x. [DOI] [PubMed] [Google Scholar]
- 28.Jiang L., Yu G., Meng W., Wang Z., Meng F., Ma W. Overexpression of amyloid precursor protein in acute myeloid leukemia enhances extramedullary infiltration by MMP-2. Tumour Biol. 2013;34:629–636. doi: 10.1007/s13277-012-0589-7. [DOI] [PubMed] [Google Scholar]
- 29.Song J.H., Kim S.H., Cho D., Lee I.K., Kim H.J., Kim T.S. Enhanced invasiveness of drug-resistant acute myeloid leukemia cells through increased expression of matrix metalloproteinase-2. Int. J. Cancer. 2009;125:1074–1081. doi: 10.1002/ijc.24386. [DOI] [PubMed] [Google Scholar]
- 30.Liersch R., Gerss J., Schliemann C., Bayer M., Schwoppe C., Biermann C., Appelmann I., Kessler T., Lowenberg B., Buchner T., et al. Osteopontin is a prognostic factor for survival of acute myeloid leukemia patients. Blood. 2012;119:5215–5220. doi: 10.1182/blood-2011-11-389692. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y.B., Ren S.M., Li S.D., Du Z. Prognostic significance of osteopontin in acute myeloid leukemia: A meta-analysis. Mol. Clin. Oncol. 2017;7:275–280. doi: 10.3892/mco.2017.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somerman M.J., Berry J.E., Khalkhali-Ellis Z., Osdoby P., Simpson R.U. Enhanced expression of alpha v integrin subunit and osteopontin during differentiation of hl-60 cells along the monocytic pathway. Exp. Cell Res. 1995;216:335–341. doi: 10.1006/excr.1995.1042. [DOI] [PubMed] [Google Scholar]
- 33.Ayatollahi M., Geramizadeh B., Zakerinia M., Ramzi M., Yaghobi R., Hadadi P., Rezvani A.R., Aghdai M., Azarpira N., Karimi H. Human bone marrow-derived mesenchymal stem cell: A source for cell-based therapy. Int. J. Organ Transplant. Med. 2012;3:32–41. [PMC free article] [PubMed] [Google Scholar]
- 34.Alachkar H., Santhanam R., Maharry K., Metzeler K.H., Huang X., Kohlschmidt J., Mendler J.H., Benito J.M., Hickey C., Neviani P., et al. Sparc promotes leukemic cell growth and predicts acute myeloid leukemia outcome. J. Clin. Investig. 2014;124:1512–1524. doi: 10.1172/JCI70921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lei U., Wohlfahrt J., Hjalgrim H., Hjalgrim L.L., Simonsen H., Melbye M. Neonatal level of thyroid-stimulating hormone and acute childhood leukemia. Int. J. Cancer. 2000;88:486–488. doi: 10.1002/1097-0215(20001101)88:3<486::AID-IJC24>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 36.Li K., Yang M., Yuen P.M., Chik K.W., Li C.K., Shing M.M., Lam H.K., Fok T.F. Thrombospondin-1 induces apoptosis in primary leukemia and cell lines mediated by CD36 and caspase-3. Int. J. Mol. Med. 2003;12:995–1001. doi: 10.3892/ijmm.12.6.995. [DOI] [PubMed] [Google Scholar]
- 37.Foss B., Nesthus I., Bergheim J., Bruserud O. Serum levels of thrombopoietin and stem cell factor in acute leukemia patients with chemotherapy-induced cytopenia and complicating infections. Platelets. 1999;10:17–23. doi: 10.1080/09537109976301. [DOI] [PubMed] [Google Scholar]
- 38.Shah C.A., Bei L., Wang H., Altman J.K., Platanias L.C., Eklund E.A. Cooperation between alphavbeta3 integrin and the fibroblast growth factor receptor enhances proliferation of hox-overexpressing acute myeloid leukemia cells. Oncotarget. 2016;7:54782–54794. doi: 10.18632/oncotarget.10189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang W.J., Han Y., Ma Z.N., Wang Q., Tang Y.Q., Wang J., Su J., Sun A.N., Wang Z.Y., Ruan C.G., et al. Changes of adamts13 activity and VWF antigen level in patients with acute myelogenous leukemia and their significance. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2014;22:1503–1507. doi: 10.7534/j.issn.1009-2137.2014.06.001. (in Chinese) [DOI] [PubMed] [Google Scholar]
- 40.Liu C., Zhao L., Zhao J., Xu Q., Song Y., Wang H. Reduced adamts-13 level negatively correlates with inflammation factors in plasma of acute myeloid leukemia patients. Leuk. Res. 2017;53:57–64. doi: 10.1016/j.leukres.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Winograd-Katz S.E., Fassler R., Geiger B., Legate K.R. The integrin adhesome: From genes and proteins to human disease. Nat. Rev. Mol. Cell Biol. 2014;15:273–288. doi: 10.1038/nrm3769. [DOI] [PubMed] [Google Scholar]
- 42.Benedetto S., Pulito R., Crich S.G., Tarone G., Aime S., Silengo L., Hamm J. Quantification of the expression level of integrin receptor alpha(v)beta3 in cell lines and mr imaging with antibody-coated iron oxide particles. Magn. Reson. Med. 2006;56:711–716. doi: 10.1002/mrm.21023. [DOI] [PubMed] [Google Scholar]
- 43.Zhai J., Wang Y., Xu C., Zheng L., Wang M., Feng W., Gao L., Zhao L., Liu R., Gao F., et al. Facile approach to observe and quantify the alpha(IIb)beta3 integrin on a single-cell. Anal. Chem. 2015;87:2546–2549. doi: 10.1021/ac504639u. [DOI] [PubMed] [Google Scholar]
- 44.Yi H., Zeng D., Shen Z., Liao J., Wang X., Liu Y., Zhang X., Kong P. Integrin alphavbeta3 enhances beta-catenin signaling in acute myeloid leukemia harboring FMS-like tyrosine kinase-3 internal tandem duplication mutations: Implications for microenvironment influence on sorafenib sensitivity. Oncotarget. 2016;7:40387–40397. doi: 10.18632/oncotarget.9617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu C.C., Chou Y.L., Ch’ang L.Y. Down-regulation of human NDR gene in megakaryocytic differentiation of erythroleukemia K562 cells. J. Biomed. Sci. 2004;11:104–116. doi: 10.1159/000075293. [DOI] [PubMed] [Google Scholar]
- 46.Helleberg C., Knudsen H., Hansen P.B., Nikolajsen K., Kjaersgaard E., Ralfkiaer E., Johnsen H.E. CD34+ megakaryoblastic leukaemic cells are CD38-, but CD61+ and glycophorin A+: Improved criteria for diagnosis of AML-M7? Leukemia. 1997;11:830–834. doi: 10.1038/sj.leu.2400648. [DOI] [PubMed] [Google Scholar]
- 47.Ylanne J., Cheresh D.A., Virtanen I. Localization of beta 1, beta 3, alpha 5, alpha v, and alpha IIb subunits of the integrin family in spreading human erythroleukemia cells. Blood. 1990;76:570–577. [PubMed] [Google Scholar]
- 48.Plow E.F., Haas T.A., Zhang L., Loftus J., Smith J.W. Ligand binding to integrins. J. Biol. Chem. 2000;275:21785–21788. doi: 10.1074/jbc.R000003200. [DOI] [PubMed] [Google Scholar]
- 49.Wang Y., Krivtsov A.V., Sinha A.U., North T.E., Goessling W., Feng Z., Zon L.I., Armstrong S.A. The wnt/beta-catenin pathway is required for the development of leukemia stem cells in aml. Science. 2010;327:1650–1653. doi: 10.1126/science.1186624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miller P.G., Al-Shahrour F., Hartwell K.A., Chu L.P., Jaras M., Puram R.V., Puissant A., Callahan K.P., Ashton J., McConkey M.E., et al. In vivo RNAi screening identifies a leukemia-specific dependence on integrin beta 3 signaling. Cancer Cell. 2013;24:45–58. doi: 10.1016/j.ccr.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li L., Sheng Y., Li W., Hu C., Mittal N., Tohyama K., Seba A., Zhao Y.Y., Ozer H., Zhu T., et al. Beta-catenin is a candidate therapeutic target for myeloid neoplasms with del(5q) Cancer Res. 2017;77:4116–4126. doi: 10.1158/0008-5472.CAN-17-0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ugarte G.D., Vargas M.F., Medina M.A., Leon P., Necunir D., Elorza A.A., Gutierrez S.E., Moon R.T., Loyola A., De Ferrari G.V. Wnt signaling induces transcription, spatial proximity, and translocation of fusion gene partners in human hematopoietic cells. Blood. 2015;126:1785–1789. doi: 10.1182/blood-2015-04-638494. [DOI] [PubMed] [Google Scholar]
- 53.Griffiths E.A., Golding M.C., Srivastava P., Povinelli B.J., James S.R., Ford L.A., Wetzler M., Wang E.S., Nemeth M.J. Pharmacological targeting of beta-catenin in normal karyotype acute myeloid leukemia blasts. Haematologica. 2015;100:e49–e52. doi: 10.3324/haematol.2014.113118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Garg S., Shanmukhaiah C., Marathe S., Mishra P., Babu Rao V., Ghosh K., Madkaikar M. Differential antigen expression and aberrant signaling via PI3/AKT, MAP/ERK, JAK/STAT, and WNT/beta catenin pathways in Lin-/CD38-/CD34+ cells in acute myeloid leukemia. Eur. J. Haematol. 2016;96:309–317. doi: 10.1111/ejh.12592. [DOI] [PubMed] [Google Scholar]
- 55.Li K., Hu C., Mei C., Ren Z., Vera J.C., Zhuang Z., Jin J., Tong H. Sequential combination of decitabine and idarubicin synergistically enhances anti-leukemia effect followed by demethylating wnt pathway inhibitor promoters and downregulating wnt pathway nuclear target. J. Transl. Med. 2014;12:167. doi: 10.1186/1479-5876-12-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohr S., Doebele C., Comoglio F., Berg T., Beck J., Bohnenberger H., Alexe G., Corso J., Strobel P., Wachter A., et al. Hoxa9 and Meis1 cooperatively induce addiction to syk signaling by suppressing miR-146a in acute myeloid leukemia. Cancer Cell. 2017;31:549–562 e511. doi: 10.1016/j.ccell.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Collins C.T., Hess J.L. Deregulation of the hoxa9/Meis1 axis in acute leukemia. Curr. Opin. Hematol. 2016;23:354–361. doi: 10.1097/MOH.0000000000000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Eklund E. The role of hox proteins in leukemogenesis: Insights into key regulatory events in hematopoiesis. Crit. Rev. Oncog. 2011;16:65–76. doi: 10.1615/CritRevOncog.v16.i1-2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ferreira H.J., Heyn H., Vizoso M., Moutinho C., Vidal E., Gomez A., Martinez-Cardus A., Simo-Riudalbas L., Moran S., Jost E., et al. DNMT3A mutations mediate the epigenetic reactivation of the leukemogenic factor MEIS1 in acute myeloid leukemia. Oncogene. 2016;35:3079–3082. doi: 10.1038/onc.2015.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ogawara Y., Katsumoto T., Aikawa Y., Shima Y., Kagiyama Y., Soga T., Matsunaga H., Seki T., Araki K., Kitabayashi I. IDH2 and NPM1 mutations cooperate to activate Hoxa9/Meis1 and hypoxia pathways in acute myeloid leukemia. Cancer Res. 2015;75:2005–2016. doi: 10.1158/0008-5472.CAN-14-2200. [DOI] [PubMed] [Google Scholar]
- 61.Liu J., Qin Y.Z., Yang S., Wang Y., Chang Y.J., Zhao T., Jiang Q., Huang X.J. Meis1 is critical to the maintenance of human acute myeloid leukemia cells independent of MLL rearrangements. Ann. Hematol. 2017;96:567–574. doi: 10.1007/s00277-016-2913-6. [DOI] [PubMed] [Google Scholar]
- 62.Shah C.A., Bei L., Wang H., Platanias L.C., Eklund E.A. The leukemia-associated MLL-ell oncoprotein induces fibroblast growth factor 2 (FGF2)-dependent cytokine hypersensitivity in myeloid progenitor cells. J. Biol. Chem. 2013;288:32490–32505. doi: 10.1074/jbc.M113.496109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roche J., Zeng C., Baron A., Gadgil S., Gemmill R.M., Tigaud I., Thomas X., Drabkin H.A. Hox expression in aml identifies a distinct subset of patients with intermediate cytogenetics. Leukemia. 2004;18:1059–1063. doi: 10.1038/sj.leu.2403366. [DOI] [PubMed] [Google Scholar]
- 64.Argiropoulos B., Humphries R.K. Hox genes in hematopoiesis and leukemogenesis. Oncogene. 2007;26:6766–6776. doi: 10.1038/sj.onc.1210760. [DOI] [PubMed] [Google Scholar]
- 65.Tohyama Y., Yanagi S., Sada K., Yamamura H. Translocation of p72syk to the cytoskeleton in thrombin-stimulated platelets. J. Biol. Chem. 1994;269:32796–32799. [PubMed] [Google Scholar]
- 66.Despeaux M., Chicanne G., Rouer E., De Toni-Costes F., Bertrand J., Mansat-De Mas V., Vergnolle N., Eaves C., Payrastre B., Girault J.A., et al. Focal adhesion kinase splice variants maintain primitive acute myeloid leukemia cells through altered WNT signaling. Stem Cells. 2012;30:1597–1610. doi: 10.1002/stem.1157. [DOI] [PubMed] [Google Scholar]
- 67.Recher C., Ysebaert L., Beyne-Rauzy O., Mansat-De Mas V., Ruidavets J.B., Cariven P., Demur C., Payrastre B., Laurent G., Racaud-Sultan C. Expression of focal adhesion kinase in acute myeloid leukemia is associated with enhanced blast migration, increased cellularity, and poor prognosis. Cancer Res. 2004;64:3191–3197. doi: 10.1158/0008-5472.CAN-03-3005. [DOI] [PubMed] [Google Scholar]
- 68.Carter B.Z., Mak P.Y., Wang X., Yang H., Garcia-Manero G., Mak D.H., Mu H., Ruvolo V.R., Qiu Y., Coombes K., et al. Focal adhesion kinase as a potential target in AML and MDS. Mol. Cancer Ther. 2017;16:1133–1144. doi: 10.1158/1535-7163.MCT-16-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chatterjee A., Ghosh J., Ramdas B., Mali R.S., Martin H., Kobayashi M., Vemula S., Canela V.H., Waskow E.R., Visconte V., et al. Regulation of STAT5 by FAK and PAK1 in oncogenic FLT3- and KIT-driven leukemogenesis. Cell Rep. 2014;9:1333–1348. doi: 10.1016/j.celrep.2014.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tavernier-Tardy E., Cornillon J., Campos L., Flandrin P., Duval A., Nadal N., Guyotat D. Prognostic value of CXCR4 and fak expression in acute myelogenous leukemia. Leuk. Res. 2009;33:764–768. doi: 10.1016/j.leukres.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 71.Quintas-Cardama A., Zhang N., Qiu Y.H., Post S., Creighton C.J., Cortes J., Coombes K.R., Kornblau S.M. Loss of TRIM62 expression is an independent adverse prognostic factor in acute myeloid leukemia. Clin. Lymphoma Myeloma Leuk. 2015;15:115–127 e115. doi: 10.1016/j.clml.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Skaik Y., Vahlsing S., Goudeva L., Eiz-Vesper B., Battermann A., Blasczyk R., Figueiredo C. Secreted beta3-integrin enhances natural killer cell activity against acute myeloid leukemia cells. PLoS ONE. 2014;9:e98936. doi: 10.1371/journal.pone.0098936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ruggeri L., Mancusi A., Burchielli E., Aversa F., Martelli M.F., Velardi A. Natural killer cell alloreactivity in allogeneic hematopoietic transplantation. Curr. Opin. Oncol. 2007;19:142–147. doi: 10.1097/CCO.0b013e3280148a1a. [DOI] [PubMed] [Google Scholar]
- 74.Blystone S.D., Lindberg F.P., LaFlamme S.E., Brown E.J. Integrin beta 3 cytoplasmic tail is necessary and sufficient for regulation of alpha 5 beta 1 phagocytosis by alpha v beta 3 and integrin-associated protein. J. Cell Biol. 1995;130:745–754. doi: 10.1083/jcb.130.3.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pacifici R., Roman J., Kimble R., Civitelli R., Brownfield C.M., Bizzarri C. Ligand binding to monocyte alpha 5 beta 1 integrin activates the alpha 2 beta 1 receptor via the alpha 5 subunit cytoplasmic domain and protein kinase c. J. Immunol. 1994;153:2222–2233. [PubMed] [Google Scholar]
- 76.Jiang B.H., Liu L.Z. Pi3k/pten signaling in angiogenesis and tumorigenesis. Adv. Cancer Res. 2009;102:19–65. doi: 10.1016/j.bbapap.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Becker P.S., Kopecky K.J., Wilks A.N., Chien S., Harlan J.M., Willman C.L., Petersdorf S.H., Stirewalt D.L., Papayannopoulou T., Appelbaum F.R. Very late antigen-4 function of myeloblasts correlates with improved overall survival for patients with acute myeloid leukemia. Blood. 2009;113:866–874. doi: 10.1182/blood-2007-12-124818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bae M.H., Oh S.H., Park C.J., Lee B.R., Kim Y.J., Cho Y.U., Jang S., Lee J.H., Kim N., Park S.H., et al. VLA-4 and CXCR4 expression levels show contrasting prognostic impact (favorable and unfavorable, respectively) in acute myeloid leukemia. Ann. Hematol. 2015;94:1631–1638. doi: 10.1007/s00277-015-2442-8. [DOI] [PubMed] [Google Scholar]
- 79.Matsunaga T., Takemoto N., Sato T., Takimoto R., Tanaka I., Fujimi A., Akiyama T., Kuroda H., Kawano Y., Kobune M., et al. Interaction between leukemic-cell VLA-4 and stromal fibronectin is a decisive factor for minimal residual disease of acute myelogenous leukemia. Nat. Med. 2003;9:1158–1165. doi: 10.1038/nm909. [DOI] [PubMed] [Google Scholar]
- 80.Walter R.B., Alonzo T.A., Gerbing R.B., Ho P.A., Smith F.O., Raimondi S.C., Hirsch B.A., Gamis A.S., Franklin J.L., Hurwitz C.A., et al. High expression of the very late antigen-4 integrin independently predicts reduced risk of relapse and improved outcome in pediatric acute myeloid leukemia: A report from the children's oncology group. J. Clin. Oncol. 2010;28:2831–2838. doi: 10.1200/JCO.2009.27.5693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang P.F., Li K.S., Shen Y.H., Gao P.T., Dong Z.R., Cai J.B., Zhang C., Huang X.Y., Tian M.X., Hu Z.Q., et al. Galectin-1 induces hepatocellular carcinoma EMT and sorafenib resistance by activating FAK/PI3K/AKT signaling. Cell Death Dis. 2016;7:e2201. doi: 10.1038/cddis.2015.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang Y., Ge X.H., Guo X.J., Guan S.B., Li X.M., Gu W., Xu W.G. Bone marrow mesenchymal stem cells inhibit the function of dendritic cells by secreting galectin-1. Biomed. Res. Int. 2017;2017:3248605. doi: 10.1155/2017/3248605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.El Leithy A.A., Helwa R., Assem M.M., Hassan N.H. Expression profiling of cancer-related galectins in acute myeloid leukemia. Tumour Biol. 2015;36:7929–7939. doi: 10.1007/s13277-015-3513-0. [DOI] [PubMed] [Google Scholar]
- 84.Azzariti A., Mancarella S., Porcelli L., Quatrale A.E., Caligiuri A., Lupo L., Dituri F., Giannelli G. Hepatic stellate cells induce hepatocellular carcinoma cell resistance to sorafenib through the laminin-332/alpha3 integrin axis recovery of focal adhesion kinase ubiquitination. Hepatology. 2016;64:2103–2117. doi: 10.1002/hep.28835. [DOI] [PubMed] [Google Scholar]
- 85.Xargay-Torrent S., Lopez-Guerra M., Montraveta A., Saborit-Villarroya I., Rosich L., Navarro A., Perez-Galan P., Roue G., Campo E., Colomer D. Sorafenib inhibits cell migration and stroma-mediated bortezomib resistance by interfering B-cell receptor signaling and protein translation in mantle cell lymphoma. Clin. Cancer Res. 2013;19:586–597. doi: 10.1158/1078-0432.CCR-12-1935. [DOI] [PubMed] [Google Scholar]