Abstract
Hereditary fibrinogen Aα-chain amyloidosis (Aα-chain amyloidosis) is a type of autosomal dominant systemic amyloidosis caused by mutations in fibrinogen Aα-chain gene (FGA). Patients with Aα-chain amyloidosis have been mainly reported in Western countries but have been rarely reported in Asia, with only five patients with Aα-chain amyloidosis being reported in Korea, China, and Japan. Clinically, the most prominent manifestation in Asian patients with Aα-chain amyloidosis is progressive nephropathy caused by excessive amyloid deposition in the glomeruli, which is similar to that observed in patients with Aα-chain amyloidosis in Western countries. In molecular features in Asian Aα-chain amyloidosis, the most common variant, E526V, was found in only one Chinese kindred, and other four kindred each had a different variant, which have not been identified in other countries. These variants are located in the C-terminal region (amino acid residues 517–555) of mature Aα-chain, which was similar to that observed in patients with Aα-chain amyloidosis in other countries. The precise number of Asian patients with Aα-chain amyloidosis is unclear. However, patients with Aα-chain amyloidosis do exist in Asian countries, and the majority of these patients may be diagnosed with other types of systemic amyloidosis.
Keywords: fibrinogen Aα-chain amyloidosis, hereditary renal amyloidosis, Ostertag-type amyloidosis, laser microdissection, proteomics analysis
1. Introduction
Different types of hereditary systemic amyloidosis without peripheral neuropathy are often referred to as “Ostertag-type amyloidosis” in reference to Ostertag’s description in 1950 of a German family in which several members died due to renal amyloidosis [1,2]. At present, hereditary non-neuropathic renal amyloidosis (also referred to as Ostertag-type amyloidosis) comprises a group of diseases associated with the variants of apolipoprotein AI [3], fibrinogen Aα-chain [4], lysozyme [5], apolipoprotein AII [6], apolipoprotein C2 [7], and apolipoprotein C3 [8].
Hereditary fibrinogen Aα-chain amyloidosis (Aα-chain amyloidosis) is a systemic disease caused by the extracellular deposition of amyloid fibrils comprising fibrinogen Aα-chain variants induced by mutations in fibrinogen Aα-chain gene (FGA) [4]. To date, 16 amyloidogenic FGA mutations have been identified [4,9,10,11,12,13,14,15,16] (Table 1). The majority of patients with Aα-chain amyloidosis have been reported in European countries and the Unites States [2,17]. Although Aα-chain amyloidosis has also been reported in some Asian patients [12,13,14], it is still recognized as a rare disease in Asia. Aα-chain amyloidosis was not reported in Japan until we recently identified a sporadic case of a patient who was initially diagnosed with primary AL amyloidosis [14]. This indicates that some patients with Aα-chain amyloidosis who have not been correctly diagnosed may exist in Asia because of the low recognition of the disease and clinical similarity of this disease to other types of amyloidosis. Here, we describe the clinical and genetic features of Aα-chain amyloidosis by paying special attention to Asian patients with Aα-chain amyloidosis, particularly the clinical and molecular characteristics of the first Japanese patient diagnosed with Aα-chain amyloidosis [14].
Table 1.
Sixteen amyloidogenic FGA mutations.
| FGA Mutations | Protein Variants | Clinical Features | Geographic Origin/Ethnicity | References |
|---|---|---|---|---|
| Missense Mutations | ||||
| c.1627G > A | E524K | Nephropathy | Scottish | Rowczenio et al. [15] |
| c.1633G > A | E526K | Nephropathy | Russian | Rowczenio et al. [15] |
| c.1634A > T | E526V | Nephropathy | US, Europe, Brazil, China | Uemichi et al. [9] |
| c.1670C > A | T538K | Nephropathy | Chinese | Gillmore et al. [13] |
| c.1676A > T | E540V | Nephropathy | German | Gillmore et al. [13] |
| c.1712C > A | P552H | Nephropathy | Afro-Caribbean | Gillmore et al. [13] |
| c.1718G > T | R554L | Nephropathy | Mexico, Europe, US (Afro-American) | Benson et al. [4] |
| Deletion Mutations | ||||
| c.1611delA (4886delA) | G519EfsX548 | Nephropathy | French | Rowczenio et al. [15] |
| c.1619_1622delTTGT (4894_4897delTTGT) | F521SfsX547 | Nephropathy | North African | Rowczenio et al. [15] |
| c.1620delT (4895delT) | F521LfsX548 | Nephropathy | French | Garnie et al. [16] |
| c.1622delT (4897delT) | V522AfsX548 | Nephropathy | French | Hamidi et al. [11] |
| c.1624_1627delAGTG (4899_4902delAGTG ) | S523RfsX547 | Nephropathy | Japanese | Yazaki et al. [14] |
| c.1629delG (4904delG) | E524EfsX548 | Nephropathy | US | Uemichi et al. [10] |
| c.1632delT (4907delT) | T525TfsX548 | Nephropathy | Chinese | Gillmore et al. [13] |
| Insertion-Deletion | ||||
| c.1606_1620del, 1619_1620insCA (4881_4895del, 4894_4895insCA) |
M517_F521del insQSfsX548 | Nephropathy | Korean | Kang et al. [12] |
| c.1720_1721delGGinsTT (5445_5446delGGinsTT) | G555F | Nephropathy | Norwegian | Rowczenio et al. [15] |
Number of amino acids denotes the position in mature fibrinogen Aα-chain.
2. Fibrinogen Aα-Chain Amyloidosis
The first case of Aα-chain amyloidosis was described by Benson et al. [4] in 1993 in a Peruvian-Mexican population, segregating with a mutation in FGA as R554L. Aα-chain amyloidosis is characterized by excessive amyloid deposition preferentially in the renal glomeruli and clinically presents as proteinuria, hypertension, and azotemia [2]. Involvement of the liver and spleen may be observed in advanced cases of Aα-chain amyloidosis; however, excessive amyloid accumulation in the glomeruli is the most remarkable feature of this disease [2]. Moreover, amyloid deposits result in atherosclerosis or cardiomyopathy in some patients [17,18]. A previous study reported that clinical symptoms of Aα-chain amyloidosis usually begin from the fourth to the ninth decade of life and that the median time from the progression of proteinuria to end-stage renal disease (ESRD) is 4.6 years [13]. However, some patients develop Aα-chain amyloidosis symptoms from the first or the second decade of life [11,12]. Most patients with Aα-chain amyloidosis do not have any family history of renal disease or amyloidosis because of the variable penetrance of this disease [13]. Therefore, a sporadic case of Aα-chain amyloidosis may be frequently misdiagnosed as primary AL amyloidosis [19]. To date, 16 amyloidogenic FGA variants have been reported, of which seven are missense mutations and nine are deletion or insertion-deletion mutations (Table 1) [4,9,10,11,12,13,14,15,16]. Of the nine deletion or insertion-deletion mutations, eight result in an out-frameshift mutation. E526V is the most common variant detected in patients across the world [2,9,13,17,20,21] (Table 1). Most patients with Aα-chain amyloidosis are heterozygous for the E526V variant; however, a recent study reported a Portuguese patient who was homozygous for the E526V variant [22]. While a genotype-phenotype correlation has not been investigated in detail, all described amyloidogenic mutations have been found to be associated with renal amyloidosis [2,13]. In addition, patients with Aα-chain amyloidosis having frameshift variants seem to show earlier disease onset (median age, 30 years) than those with single amino acid substitutions (median age, 59 years) [15].
3. Aα-Chain Amyloidosis in Asia
Aα-chain amyloidosis is the leading cause of hereditary non-neuropathic systemic amyloidosis in Western countries [17]. However, only a few cases of Aα-chain amyloidosis have been reported in Asia [12,13,14,23]. In 2005, Kang et al. [12] reported a sporadic case of a patient with Aα-chain amyloidosis in Korea who showed very early onset of the disease (at the age of 7 years) and rapid deterioration of renal function. The patient developed ESRD within 2 years after the disease onset. Renal biopsy showed severe glomerular enlargement with excessive amyloid deposits. Moreover, this patient had a unique frameshift mutation (c.1606_1620del,1619_1620insCA) in FGA, which was the first insertion-deletion mutation to be reported in patients with Aα-chain amyloidosis. Later, Gillmore et al. [13] detected two novel variants, T538K and c.1632delT (a frameshift variant), in Chinese patients with Aα-chain amyloidosis. In contrast, Yao et al. [23] reported the case of a Chinese patient with Aα-chain amyloidosis who had the most common mutation, i.e., E526V, and who presented with proteinuria, hypertension, and renal failure.
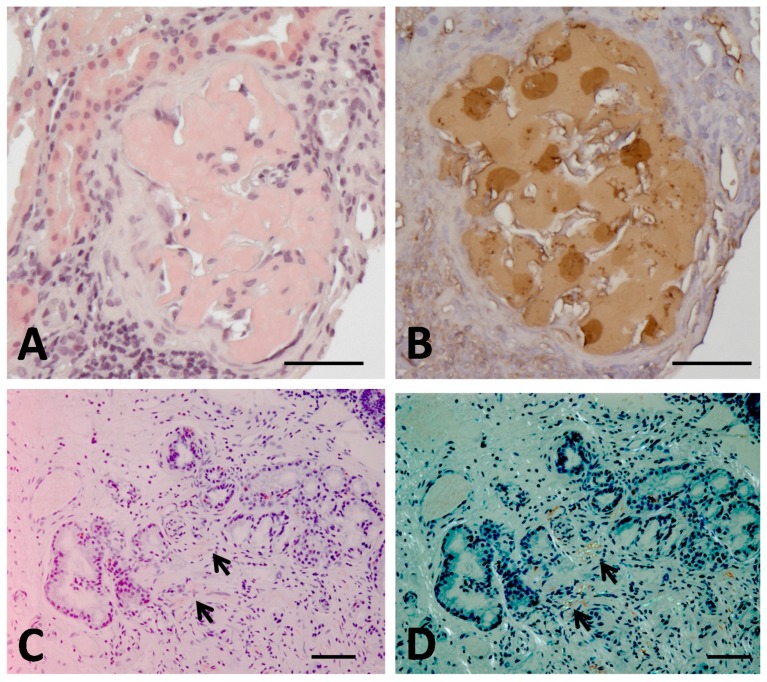
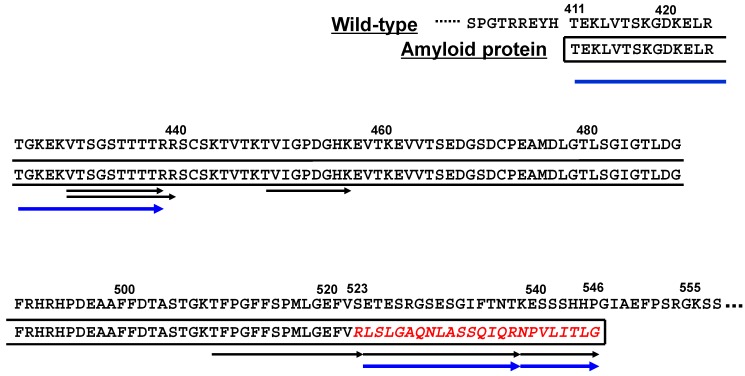
4. The First Case of Aα-Chain Amyloidosis in Japan: Clinical and Molecular Features
In Japan, the vast majority (over 90%) of patients with hereditary systemic amyloidosis are transthyretin-related familial amyloid polyneuropathy (hereditary ATTR amyloidosis). More than 300 patients are assumed to exist in Japan, and those patients usually present with severe peripheral and autonomic neuropathy, cardiomyopathy gastroenteropathy, and/or oculopathy. However, no patient with hereditary non-neuropathic renal amyloidosis (Ostertag-type amyloidosis) had been reported in Japan until we reported the sporadic case of a patient with Aα-chain amyloidosis having a novel frameshift variant (4899_4902delAGTG) in 2015 [14]. This patient was a 40-year-old woman with rapidly deteriorating nephropathy [14]. The patient developed proteinuria at the age of 32 years, and renal biopsy showed excessive amyloid deposits in her glomeruli (Figure 1A,B). The patient did not have any overt signs of neuropathy, cardiomyopathy, oculopathy, or gastroenteropathy; however, gastroduodenal biopsy showed small amount of amyloid accumulation in the duodenal mucosa (Figure 1C,D). The plasma fibrinogen level of the patient was within the normal range (254 mg/dL; normal range, 180–350 mg/dL), and she did not show coagulopathy. Abdominal fat pad biopsy and liver biopsy did not show the presence of amyloid deposits (data not shown). Initially, the patient was diagnosed with primary AL amyloidosis. However, her renal function deteriorated rapidly despite treatment with combined chemotherapies, and she developed ESRD at 18 months after the detection of proteinuria. Eight years after the onset, a definite diagnosis of Aα-chain amyloidosis was made by proteomics analysis of glomerular amyloid on renal sample biopsied at 32 years, using laser microdissection (LMD) and liquid chromatography tandem mass spectrometry (LC-MS/MS) [14]. Proteomics analysis detected several tryptic peptides in accordance with the C-terminal region of Aα-chain (Figure 2). In addition, proteomics analysis detected two tryptic peptides, namely, LSLGAQNLASSQIQR and NPVLITLG, that corresponded to the previously described sequences of the C-terminal region of a fibrinogen variant (position 525–547) induced by a frameshift mutation (4904delG [10]) (Figure 2). Proteomics analysis did not detect a wild-type Aα-chain sequence after position 523, indicating that amyloid fibrils in our patient were only composed of the variant Aα-chain fragment. Moreover, proteomics analysis did not detect other tryptic peptides before position 430, suggesting that the N-terminus of the amyloid protein was present around position 430 (Figure 2). To obtain more information on the N-terminus of the amyloid protein, we biochemically investigated the amyloid fibril protein isolated from frozen duodenal mucosa samples by performing methods reported previously [24] and detected several peptides generated by Arg-C peptidase (Figure 2). We also detected a fragment starting with the amino acid residue Thr at position 411, but could not detect peptides before position 410. Therefore, we assumed that Thr411 was the N-terminus and that the amyloid protein was composed of Aα-chain fragments with wild-type (positions 411–522) and abnormal sequences (position 523–546) (Figure 2). However, we did not detect any wild-type sequence after residue 523. This result indicated that the wild-type Aα-chain sequence did not contribute to amyloid formation in our patient, as that observed in another patient with 4897delT [11]. SDS-PAGE showed that the molecular weight of the amyloid fibril protein was approximately 12 kDa (unpublished observation).
Figure 1.
Findings of renal biopsy (A,B) and duodenal mucosal biopsy (C,D) in a Japanese Aα-chain amyloidosis patient [14]. (A,C) Congo red staining. (B) Immunohistochemical staining with anti-human fibrinogen antibody. (D) Congo red staining under polarized light. Renal biopsy at the age of 32 years shows heavy amyloid deposits mainly in glomerulus with almost complete obliteration of the normal glomerular architecture (A). The positive staining is observed in immunohistochemistry (B). Duodenal mucosal biopsy at the age of 40 years demonstrates a small amount of amyloid deposits (arrows, (C)), showing typical apple-green birefringence under polarized light (arrows, (D)). Bars = 50 μm.
Figure 2.
Putative primary structure of amyloid fibril protein in a Japanese Aα-chain amyloidosis patient [14]. Amyloid protein in this patient is assumed to be composed of both wild-type sequence (residues 411–522) and an additional fragment (red italic letters) induced by the frameshift variant (residues 523–546). Black arrows denote tryptic peptides detected at laser microdissection (LMD) isolation of glomerular amyloid, and blue arrows denote Arg-C peptides detected at in-gel digestion on SDS-PAGE analysis of duodenal amyloid.
5. Discussion
One of the most notable clinical features of Aα-chain amyloidosis in Asia is that it may still be a quite rare disease, as mentioned above, and only a few Asian patients have been found to date, solely in East Asian countries [12,13,14,23]. Nephropathy is the main clinical manifestation in Asian patients with Aα-chain amyloidosis, which is similar to that observed in patients with Aα-chain amyloidosis in other countries. Moreover, Asian and Western patients with Aα-chain amyloidosis show similar renal pathological findings, including excessive amyloid deposits in the glomeruli [12,14]. Genetically, the five Asian patients with Aα-chain amyloidosis had five different genetic mutations, of which four were novel (Table 1). E526V, the most common variant in patients with Aα-chain amyloidosis in Western countries, was detected in only one Chinese patient with Aα-chain amyloidosis [23]. The other four mutations detected in the remaining Asian patients with Aα-chain amyloidosis have not been reported in patients with Aα-chain amyloidosis in other countries to date.
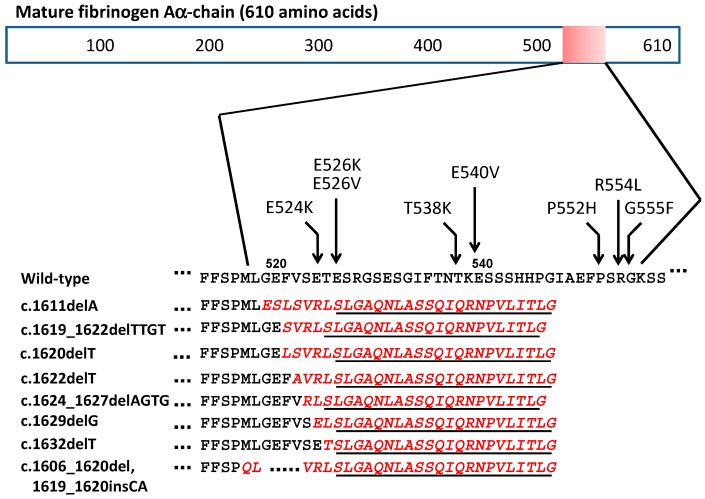
Fibrinogen is a 340-kDa plasma glycoprotein that plays a major role in blood coagulation by converting to fibrin [25,26]. It is composed of two identical subunits, each of which contains an Aα-, Bβ-, and γ-chain and is produced by hepatocytes. Mature Aα-chain contains 610 amino acids and has a molecular weight of approximately 66 kDa [27]. The detailed pathomechanism underlying amyloid formation from the Aα-chain remains unclear. Interestingly, all amyloidogenic variants, including the eight frameshift mutations, are present in a specific region of the Aα-chain from residues 517 to 555 (Figure 3). These data clearly suggest that the location of FGA mutations is a key factor in amyloid formation. However, because five single amino acid substitutions (Available online: www.geht.org/databaseang/fibrinogen/), such as R554C [28] and R554H [15] at position 517–555, do not induce amyloid formation, it is likely that amyloid formation strongly depends on both the location of the variants and the type of replaced amino acids. In addition, of particular interest in the eight frameshift variants is that the C-terminal sequences resulting from all mutations bear a close resemblance to each other (Figure 3). In fact, C-terminal peptides containing 24 amino acids (SLGAQNL.....VLITLG) are identical among all of the frameshift variants, suggesting that this common sequence may be essential for amyloid formation. A recent study reported the importance of the C-terminal sequence composed of five amino acids (VLITL) in amyloidogenesis [16]. This common sequence may be attributed to the number of deleted nucleotides explained by arithmetical progression (1 + 3[n − 1]). In addition, it seems to be important that the location of nucleotide deletion should be after TAG within Leu518 (TTA) and Gly519 (GGA), or all nucleotides at position 518 and 519 are deleted, according to the mutation reported by Kang et al. [12]. Indeed, one nucleotide deletion (delC) at position Ala499 (GCC) generated a premature stop codon (TAG) at position 518, and this mutation was non-amyloidogenic [29]. On the other hand, in amyloid proteins associated with frameshift mutations, the length of the wild-type amino acid sequence in the N-terminus seems to vary in each case. In our patient, the presumable start point was Thr411 and the amyloid protein was assumed to contain 136 amino acids (411–546), with a molecular weight of approximately 12 kDa (Figure 2). In contrast, the putative starting point in an amyloid protein associated with 4897delT was assumed to be around Ala499, and its molecular weight was found to be 5 kDa [11]. Therefore, the production of a fragment containing an appropriate length of the wild-type Aα-chain sequence and an additional 24 common C-terminal residues seems to be important for amyloid formation. It was assumed that the variant Aα-chain containing 546 amino acid residues, which was detected in our patient with a 4-bp deletion [14], was more unstable and could be more easily degraded than the normal Aα-chain, as reported in other frameshift variants [10]. However, because no amyloid deposits were seen within or outside hepatocytes in our patient, it is possible that the variant Aα-chain was secreted by hepatocytes without intracellular aggregation. Therefore, at least in our patient, amyloid formation seemed to be strongly dependent on some proteolytic events after secretion from hepatocytes. In the variant Aα-chain with a single amino acid substitution (R554L), the amyloid protein consisted of a fragment containing variant Aα-chain residues 500–580 [4]. Serpell et al. [30] described the importance of residues 500–521 in amyloidogenesity because this portion was also present in a frameshift variant (4897delT) [11]. This portion was also detected in our patient (Figure 2). This suggests that an amyloidogenic fragment of an appropriate length for fibril formation generated from a variant Aα-chain through an aberrant proteolytic event is important for amyloid formation. However, mechanisms underlying the generation of amyloidogenic fragments or their escape from further processing are unclear, and further in vivo or in vitro investigations should be performed to address these questions.
Figure 3.
The location of 16 amyloidogenic FGA variants. All amyloidogenic variants crowd in a quite limited portion from residue 517 to 555 of the mature Aα-chain. In eight frameshift variants, the C-terminal sequences resulted from frameshift variants (red italic letters) bear a close resemblance to each other, and the C-terminal peptides consisting of 24 amino acids (underline) are identical.
Thus, more patients with Aα-chain amyloidosis may be present in Asia. However, the majority of these patients may have been misdiagnosed with other types of systemic amyloidosis. Asian and European patients with Aα-chain amyloidosis do not show remarkable differences with respect to clinical manifestations; however, the most prevalent genetic variant E526V in European patients may not be common in Asian patients. Recently, several effective therapies have been established for treating different types of systemic amyloidosis; however, the therapeutic strategy for treating each type of amyloidosis is different [13,17,31,32,33,34,35,36,37,38,39,40,41,42] (Table 2), highlighting the importance of the correct diagnosis of the disease at an early stage. Moreover, the possibility of Aα-chain amyloidosis should always be considered in sporadic cases of amyloid nephropathy, even in Asian countries. In our patient, proteomic analysis by performing LMD and LC-MS/MS not only helped in making the correct diagnosis, but also helped in obtaining information on the whole sequence of the amyloid fibril protein by using small sections of an old formalin-fixed, paraffin-embedded tissue sample obtained from the patient [14].
Table 2.
Therapeutic options in major systemic amyloidoses.
| Types of Systemic Amyloidosis | Precursor Proteins | Therapeutic Options | References |
|---|---|---|---|
| Hereditary ATTR amyloidosis | Transthyretin | Liver transplant, tafamidis, diflunisal, gene therapies | [31,32,33,34,35] |
| Primary AL amyloidosis | Immunoglobulin light chain | Chemotherapies, stem cell transplantation | [36,37,38] |
| Reactive AA amyloidosis | Serum amyloid A (SAA) | Control of underlying diseases, biologic agents | [39,40] |
| Fibrinogen Aα-chain amyloidosis | Fibrinogen Aα-chain | Renal transplant, liver and renal transplant | [13,17] |
| Apolipoprotein A-I amyloidosis | Apolipoprotein A-I | Renal transplant, liver and renal transplant | [41] |
| Apolipoprotein A-II amyloidosis | Apolipoprotein A-II | Renal transplant | [42] |
6. Conclusions
Clinical pictures in Asian Aα-chain amyloidosis patients are almost similar to those in Western counties. While the features of genotype in FGA may be different between Asian and European patients, it is common that all amyloidogenic variants are located in the C-terminal region (amino acid residues 517–555) of mature Aα-chain. The precise number of Asian patients with Aα-chain amyloidosis is unclear. However, patients with Aα-chain amyloidosis do exist in Asian countries, and the majority of these patients may be diagnosed with other types of systemic amyloidosis.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research in Japan (Kaken, 16K21066 to Tsuneaki Yoshinaga) and a grant from the Hokuto Foundation for Bioscience (Masahide Yazaki and Tsuneaki Yoshinaga).
Abbreviations
| Aα-chain amyloidosis | Fibrinogen Aα-chain amyloidosis |
| ESRD | End-stage renal disease |
| LMD | Laser microdissection |
| LC-MS/MS | Liquid chromatography-tandem mass spectrometry |
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Ostertag B. Familiere amyloid-erkrankung. Z. Menschl. Vererbungs Konstit. Pehre. 1950;30:105–115. [Google Scholar]
- 2.Benson M.D. Ostertag revisited: The inherited systemic amyloidosis without neuropathy. Amyloid. 2005;12:75–87. doi: 10.1080/13506120500106925. [DOI] [PubMed] [Google Scholar]
- 3.Nichols W.C., Dwulet F.E., Liepnieks J., Benson M.D. Variant apolipoprotein AI as a major constituent of a hemian hereditary amyloid. Biochem. Biophys. Res. Commun. 1988;156:762–768. doi: 10.1016/S0006-291X(88)80909-4. [DOI] [PubMed] [Google Scholar]
- 4.Benson M.D., Liepnieks J., Uemichi T., Wheeler G., Correa R. Hereditary renal amyloidosis associated with a mutant fibrinogen α-chain. Nat. Genet. 1993;3:252–255. doi: 10.1038/ng0393-252. [DOI] [PubMed] [Google Scholar]
- 5.Pepys M.B., Hawkins P.N., Booth D.R., Vigushin D.M., Tennent G.A., Soutar A.K., Totty N., Nguyen O., Blake C.C., Terry C.J., et al. Human lysozyme gene mutations cause hereditary systemic amyloidosis. Nature. 1993;362:553–557. doi: 10.1038/362553a0. [DOI] [PubMed] [Google Scholar]
- 6.Benson M.D., Liepnieks J., Yazaki M., Yamashita T., Hamidi Asl K., Guenther B., Kluve-Beckerman B. A new human hereditary amyloidosis: The result of a stop-codo mutation in the apolipoprotein AII gene. Genomics. 2001;72:272–277. doi: 10.1006/geno.2000.6499. [DOI] [PubMed] [Google Scholar]
- 7.Nasr S.H., Dasari S., Hasadsri L., Theis J.D., Vrana J.A., Gertz M.A., Muppa P., Zimmermann M.T., Grogg K.L., Dispenzieri A., et al. Novel type of renal amyloidosis derived from apolipoprotein C-II. J. Am. Soc. Nephrol. 2017;28:439–445. doi: 10.1681/ASN.2015111228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valleix S., Verona G., Jourde-Chiche N., Nédelec B., Mangione P.P., Bridoux F., Mangé A., Dogan A., Goujon J.M., Lhomme M., et al. D25V apolipoprotein C-III variant causes dominant hereditary systemic amyloidosis and confers cardiovascular protective lipoprotein profile. Nat. Commun. 2016;7:10353. doi: 10.1038/ncomms10353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uemichi T., Liepnieks J.J., Benson M.D. Hereditary renal amyloidosis with a novel variant fibrinogen. J. Clin. Investig. 1994;93:731–736. doi: 10.1172/JCI117027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uemichi T., Liepnieks J.J., Yamada T., Gertz M.A., Bang N., Benosn M.D. A frame shift mutation in the Fibrinogen A α-chain gene in a kindred with renal amyloidosis. Blood. 1996;87:4197–4203. [PubMed] [Google Scholar]
- 11.Hamidi Asl L., Liepnieks J.J., Uemichi T., Rebibou J.M., Justrabo E., Droz D., Mousson C., Chalopin J.M., Benson M.D., Delpech M., et al. Renal amyloidosis with a frame shift mutation in Fibrinogen Aα-chain gene producing a novel amyloid protein. Blood. 1997;90:4799–4805. [PubMed] [Google Scholar]
- 12.Kang H.G., Bybee A., Ha I.S., Park M.S., Gilbertoson J.A., Cheong H.I., Choi Y., Hawkins P.N. Hereditary amyloidosis in early childhood associated with a novel insertion-deletion (indel) in the fibrinogen Aα chain gene. Kidney Int. 2005;68:1994–1996. doi: 10.1111/j.1523-1755.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- 13.Gillmore J.D., Lachmann H.J., Rowczenio D., Gilbertoson J.A., Zeng C.H., Liu Z.H., Li L.S., Wechalekar A., Hawkins P.N. Diagnosis, pathogenesis, treatment, and prognosis of hereditary fibrinogen Aα-chain amyloidosis. J. Am. Soc. Nephrol. 2009;20:444–451. doi: 10.1681/ASN.2008060614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yazaki M., Yoshinaga T., Sekijima Y., Nishio S., Kanizawa Y., Kametani F., Miyashita K., Hachiya N., Higuchi K., Ikeda S. The first pure form of Ostertag-type amyloidosis in Japan: A sporadic case of hereditary fibrinogen Aα-chain amyloidosis associated with a novel frameshift variant. Amyloid. 2015;22:142–144. doi: 10.3109/13506129.2015.1037389. [DOI] [PubMed] [Google Scholar]
- 15.Rowczenio D., Stensland M., de Souza G.A., Strøm E.H., Gilbertson J.A., Taylor G., Rendell N., Minogue S., Efebera Y.A., Lachmann H.J., et al. Renal amyloidosis associated with 5 novel variants in the fibrinogen A alpha cahin protein. Kidney Int. Rep. 2017;2:461–469. doi: 10.1016/j.ekir.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garnier C., Briki F., Nedelec B., Le Pogamp P., Dogan A., Rioux-Leclercq N., Goude R., Beugnet C., Martin L., Delpech M., et al. VLITL is a major cross-b-sheet signal for fibrinogen Aα-chain frameshift variants. Blood. 2017;130:2799–2807. doi: 10.1182/blood-2017-07-796185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stangou A.J., Banner N.R., Hendry B.M., Rela M., Portmann B., Wendon J., Monaghan M., MacCarthy P., Buxton-Thomas M., Mathias C., et al. Hereditary fibrinogen Aα-chain amyloidosis: Phenotypic characterization of a systemic disease and the role of liver transplantation. Blood. 2010;115:2998–3007. doi: 10.1182/blood-2009-06-223792. [DOI] [PubMed] [Google Scholar]
- 18.Mourad G., Delabre J.P., Garigue V. Cardiac amyloidosis with the E526V mutation of the fibrinogen Aα-chain. N. Engl. J. Med. 2008;358:2847–2848. doi: 10.1056/NEJMc0805012. [DOI] [PubMed] [Google Scholar]
- 19.Lachmann H.J., Booth D.R., Booth S.E., Bybee A., Gilbertson J.A., Gillmore J.D., Pepys M.K., Hawkins P.N. Misdiagnosis of hereditary amyloidosis as AL (primary) amyloidosis. N. Engl. J. Med. 2002;346:1786–1791. doi: 10.1056/NEJMoa013354. [DOI] [PubMed] [Google Scholar]
- 20.Machado J.R., da Silva M.V., de Menezes Neves P.D.M., de Oliveira F.A., Corrêa R.R.M., Rodrigues W.V.D., Benson M.D., dos Reis M.A. Fibrinogen A α-chain amyloidosis: Report of the first case in Latin America. Amyloid. 2013;20:52–55. doi: 10.3109/13506129.2012.763029. [DOI] [PubMed] [Google Scholar]
- 21.Tavares I., Oliveira J.P., Pinho A., Moreira L., Rocha L., Santos J., Pinheiro J., Costa P.P., Lobato L. Unrecognized fibrinogen Aα-chain amyloidosis: Results from targeted genetic testing. Am. J. Kidney Dis. 2017;70:235–243. doi: 10.1053/j.ajkd.2017.01.048. [DOI] [PubMed] [Google Scholar]
- 22.Tavares I., Lobato L., Matos C., Santos J., Moreira P., Saraiva M.J., Henriques A.C. Homozygosity for the E526V mutation in fibrinogen A alpha-chain amyloidosis: The first report. Case Rep. Nephrol. 2015 doi: 10.1155/2015/919763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao Y., Wang S.X., Zhang Y.K. Hereditary fibrinogen Aα-chain amyloidosis caused by the E526V mutation: A case report and literature review. Beijing Da Xue Xue Bao Yi Xue Ban. 2014;46:802–804. (In Chinese) [PubMed] [Google Scholar]
- 24.Yazaki M., Fushimi T., Tokuda T., Kametani F., Yamamoto K., Matsuda M., Shimojo H., Hoshii Y., Higuchi K., Ikeda S. A patient with severe renal amyloidosis associated with an immunoglobulin γ-heavy chain fragment. Am. J. Kidney Dis. 2004;43:E23–E28. doi: 10.1053/j.ajkd.2003.12.056. [DOI] [PubMed] [Google Scholar]
- 25.Weisel J.W. Fibrinogen and fibrin. Adv. Protein Chem. 2005;70:247–299. doi: 10.1016/S0065-3233(05)70008-5. [DOI] [PubMed] [Google Scholar]
- 26.Weisel J.W., Litvinov R.I. Mechanism of fibrin polymerization and clinical implications. Blood. 2013;121:1712–1719. doi: 10.1182/blood-2012-09-306639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kant J.A., Fornace A.J., Jr., Saxe D., Simon M.I., McBride O.W., Crabtree G.R. Evolution and organization of the fibrinogen locus on chromosome 4: Gene duplication accompanied by transposition and inversion. Proc. Natl. Acad. Sci. USA. 1985;82:2344–2348. doi: 10.1073/pnas.82.8.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koopman J., Haverkate F., Grimbergen J., Lord S.T., Mosesson M.W., DiOrio J.P., Siebenlist K.R., Legrand C., Soria J., Soria C., et al. The molecular basis for fibrinogen Dusart (Aa554 Arg->Cys) and its association with abnormal fibrinogen polymerization and thrombophilia. J. Clin. Investig. 1993;91:1637–1643. doi: 10.1172/JCI116371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Margaglione M., Vecchione G., Santacroce R., D’Angelo F., Casetta B., Papa M.L., Grandone E., Di Minno G. A frameshift mutation in the human fibrinogen α-chain gene (α (499) Ala frameshift stop) leading to dysfibrinogen San Giovanni Rotondo. Thromb. Haemost. 2001;86:1483–1488. [PubMed] [Google Scholar]
- 30.Serpell L.C., Benson M.D., Liepnieks J.J., Fraser P.E. Structural analyses of fibrinogen amyloid fibrils. Amyloid. 2007;14:199–203. doi: 10.1080/13506120701461111. [DOI] [PubMed] [Google Scholar]
- 31.Ericzon B.G., Wilczek H.E., Larsson M., Wijayatunga P., Stangou A., Pena J.R., Furtado E., Barroso E., Daniel J., Samuel D., et al. Liver Transplantation for Hereditary Transthyretin Amyloidosis: After 20 Years Still the Best Therapeutic Alternative? Transplantation. 2015;99:1847–1854. doi: 10.1097/TP.0000000000000574. [DOI] [PubMed] [Google Scholar]
- 32.Coelho T., Maia L.F., da Silva A.M., Cruz M.W., Planté-Bordeneuve V., Suhr O.B., Conceiçao I., Schmidt H.H., Trigo P., Kelly J.W., et al. Long-term effects of tafamidis for the treatment of transthyretin familial amyloid polyneuropathy. J. Neurol. 2013;260:2802–2814. doi: 10.1007/s00415-013-7051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berk J.L., Suhr O.B., Obici L., Sekijima Y., Zeldenrust S.R., Yamashita T., Heneghan M.A., Gorevic P.D., Litchy W.J., Wiesman J.F., et al. Repurposing Diflunisal for Familial Amyloid Polyneuropathy: A Randomized Clinical Trial. JAMA. 2013;310:2658–2667. doi: 10.1001/jama.2013.283815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coelho T., Adams D., Silva A., Lozeron P., Hawkins P.N., Mant T., Perez J., Chiesa J., Warrington S., Tranter E., et al. Safety and efficacy of RNAi therapy for transthyretin amyloidosis. N. Engl. J. Med. 2013;369:819–829. doi: 10.1056/NEJMoa1208760. [DOI] [PubMed] [Google Scholar]
- 35.Benson M.D., Kluve-Beckerman B., Zerdenrust S.R., Siesky A.M., Bodenmiller D.M., Showalter A.D., Sloop K.W. Targeted suppression of an amyloidogenic transthyretin with antisense oligonucleotides. Muscle Nerve. 2006;33:609–618. doi: 10.1002/mus.20503. [DOI] [PubMed] [Google Scholar]
- 36.Katoh N., Matsuda M., Tsuchiya-Suzuki A., Ikeda S. Regression of gastroduodenal amyloid deposition in systemic AL amyloidosis after intensive chemotherapies. Br. J. Haematol. 2011;153:535–538. doi: 10.1111/j.1365-2141.2010.08503.x. [DOI] [PubMed] [Google Scholar]
- 37.Katoh N., Matsushima A., Kurozumi M., Matsuda M., Ikeda S. Marked and rapid regression of hepatic amyloid deposition in a patient with systemic light chain (AL) amyloidosis after high-dose melphalan therapy with stem cell transplantation. Intern. Med. 2014;53:1991–1995. doi: 10.2169/internalmedicine.53.2065. [DOI] [PubMed] [Google Scholar]
- 38.Landau H., Hassoun H., Rosenzweig M.A., Maurer M., Liu J., Flombaum C., Bello C., Hoover E., Riedel E., Giralt S., et al. Bortezomib and dexamethasone consolidation following risk-adapted melphalan and stem cell transplantation for patients with newly diagnosed light-chain amyloidosis. Leukemia. 2013;27:823–828. doi: 10.1038/leu.2012.274. [DOI] [PubMed] [Google Scholar]
- 39.Okuda Y., Takasugi K. Successful use of a humanized anti-interleukin-6 receptor antibody, tocilizumab, to treat amyloid a amyloidosis complicating juvenileidiopathic arthritis. Arthritis Rheum. 2006;54:2997–3000. doi: 10.1002/art.22118. [DOI] [PubMed] [Google Scholar]
- 40.Okuda Y., Ohnishi M., Matoba K., Jouyama K., Yamada A., Sawada N., Mokuda S., Murata Y., Takasugi K. Comparison of the clinical utility of tocilizumab and anti-TNF therapy in AA amyloidosis complicating rheumatic diseases. Mod. Rheumatol. 2014;24:137–143. doi: 10.3109/14397595.2013.854048. [DOI] [PubMed] [Google Scholar]
- 41.Gillmore J.D., Stangou A.J., Lachmann H.J., Goodman H.J., Wechalekar A.D., Acheson J., Tennent G.A., Bybee A., Gilbertson J., Rowczenio D., et al. Organ transplantation in hereditary apolipoprotein AI amyloidosis. Am. J. Transplant. 2006;6:2342–2347. doi: 10.1111/j.1600-6143.2006.01507.x. [DOI] [PubMed] [Google Scholar]
- 42.Magy N., Liepnieks J.J., Yazaki M., Kluve-Beckerman B., Benson M.D. Renal transplantation for apolipoprotein AII amyloidosis. Amyloid. 2003;10:224–228. doi: 10.3109/13506120309041739. [DOI] [PubMed] [Google Scholar]