Abstract
We examined risks for first hospitalization and the rate, risk factors, costs, and 1‐year outcome of 30‐day readmission among patients admitted for complications of cirrhosis. Data were retrospectively analyzed for adult patients with cirrhosis residing in Minnesota, Iowa, or Wisconsin and admitted from 2010 through 2013 at both campuses of the Mayo Clinic Hospital in Rochester, MN. Readmission was captured at the two hospitals as well as at community hospitals in the tristate area within the Mayo Clinic Health System. The incidence of hospitalization for complications of cirrhosis was 100/100,000 population, with increasing age and male sex being the strongest risks for hospitalization. For the 2,048 hospitalized study patients, the overall 30‐day readmission rate was 32%; 498 (24.3%) patients were readmitted to Mayo Clinic hospitals and 157 (7.7%) to community hospitals, mainly for complications of portal hypertension (52%) and infections (30%). Readmission could not be predicted accurately. There were 146 deaths during readmission and an additional 105 deaths up to 1 year of follow‐up (50.4% total mortality). Annual postindex hospitalization costs for those with a 30‐day readmission were substantially higher ($73,252) than those readmitted beyond 30 days ($62,053) or those not readmitted ($5,719). At 1‐year follow‐up, only 20.4% of patients readmitted within 30 days were at home. In conclusion, patients with cirrhosis have high rates of hospitalization, especially among men over 65 years, and of unscheduled 30‐day readmission. Readmission cannot be accurately predicted. Postindex hospitalization costs are high; nationally, the annual costs are estimated to be more than $4.45 billion. Only 20% of patients readmitted within 30 days are home at 1 year. (Hepatology Communications 2018;2:188–198)
Abbreviations
- CI
confidence interval
- HBC
hepatitis C virus
- HBV
hepatitis B virus
- HR
hazard ratio
- ICD‐9‐CM
International Classification of Diseases
- Ninth Revision
Clinical Modification
- MCHS
Mayo Clinic Health System
- MELD
Model for End‐Stage Liver Disease
- MELD‐Na
Model for End‐Stage Liver Disease plus serum sodium
Introduction
The incidence and risk factors for hospitalization for complications of cirrhosis are not clearly known. Patients with cirrhosis require hospitalization for a variety of complications, and survivors of the initial hospitalization are at risk for readmission. The unscheduled readmission rates for patients with cirrhosis are reported to range from 20% to 37% at 30 days and up to 53% at 90 days.1, 2, 3 A high readmission rate is believed to be predicted by the severity of liver disease as determined by the Model for End‐Stage Liver Disease (MELD) score and comorbidities.1, 2, 3 These data, however, come from tertiary care referral centers where readmissions may occur outside the tertiary care health system. Recently, Tapper et al.4 reported in a multistate population‐based cohort a 30‐day readmission rate of 12.9% and a 90‐day readmission rate of 21.2%, much lower than those of previous studies. However, the data lacked the necessary variables required to determine risk factors for both admission and readmission, and it was unclear whether the admission was the first hospitalization for cirrhosis.4 The costs incurred and the long‐term outcomes were not studied.
In this report, we present incidence and risk factors for first hospitalization for complications of cirrhosis and outcomes (including 1 year), risk factors, and costs of a multistate all‐payer cohort study of patients with cirrhosis who required readmission within 30 days.
Methods
DATA
The Mayo Clinic Institutional Review Board approved the study. All authors had access to the study data and reviewed and approved the final manuscript.
Data were obtained for patients with complications of cirrhosis who were hospitalized from January 1, 2010, through December 31, 2013. Population incidence rates for first‐ever hospitalization were determined among patients within Olmsted County, Minnesota. Population‐based epidemiologic research can be conducted in this county because medical care is effectively self‐contained in the community with two major health care providers serving almost the entire population.5 The index hospitalization was at two campuses of the Mayo Clinic Hospital located in Rochester, MN (Olmsted County), which serve as tertiary‐care referral centers. Readmissions were captured at these hospitals as well as from the Mayo Clinic Health System (MCHS), a family of clinics, hospitals, and health care facilities serving over 60 communities in Minnesota, Iowa, and Wisconsin and covering a population of 2.6 million. We identified unique index hospitalizations for adults (≥18 years) who were discharged with diagnoses consistent with cirrhosis as defined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) codes and according to a validated protocol.6 To be included, patients had to reside in Minnesota, Iowa, or Wisconsin and have a diagnosis of cirrhosis (571.2, 571.5, 571.6) and a first admission with one or more of the following complications: esophageal varices with bleeding (code 456.0), esophageal varices without bleeding (456.1), varices in disease classified elsewhere with bleeding (456.2), varices in disease classified elsewhere without bleeding (456.21), spontaneous bacterial peritonitis (567.23), hepatorenal syndrome (572.4), and/or hepatic encephalopathy (572.2). We tested the validity of the ICD‐9‐CM codes in an administrative database from Olmsted County by using a medical‐linked system within the Rochester Epidemiology Project to identify patients. This set of ICD‐9‐CM codes identified patients with cirrhosis with high accuracy (sensitivity and specificity greater than 90%). Ascites (789.5) did not add to the accuracy of diagnosis of cirrhosis. Individuals were excluded from the study if they 1) had elective admissions for scheduled therapeutic procedures, such as transarterial chemoembolization for hepatocellular carcinoma; 2) denied access to their electronic health records for research purposes (6%); 3) died during the initial hospitalization (6.7%); 4) received a liver transplant before or during the study period; and 5) had only a temporary address.
ETIOLOGY OF CIRRHOSIS
The pathogenesis of cirrhosis was determined from the medical record and classified as alcoholic liver disease (documented history of alcohol misuse and absence of other risk factors); nonalcoholic steatohepatitis (cirrhosis in the presence of obesity and absence of other causes of liver disease); viral (presence of markers of hepatitis B virus [HBV] and/or hepatitis C virus [HCV] and absence of other causes for cirrhosis); immune (autoimmune hepatitis, primary biliary cirrhosis, primary sclerosing cholangitis); and other (such as hemochromatosis, α‐1 antitrypsin deficiency, and cardiac cirrhosis). Patients with HCV or HBV with a remote history of alcohol use were grouped under viral. Patients with current misuse of alcohol and markers of HCV or HBV were classified as alcoholic cirrhosis.
OUTCOMES
The primary outcomes were risks for first hospitalization and 30‐day inpatient readmission; the secondary outcomes were cost and status at 1 year. Comorbidity and illness severity were controlled for by using the Charlson comorbidity index.7 Data were collected by the Mayo Clinic Life Science System (a data repository) and the Data Discovery and Query Builder (a query toolset; IBM) and manually reviewed by investigators. Data collected regarding the initial hospitalization and readmission included demographic characteristics, cause of cirrhosis, length of hospital stay, comorbidities, laboratory values (at admission and discharge dates), standardized costs, and the primary reason for admission. The MELD score and the MELD plus serum sodium (MELD‐Na) score were calculated within 48 hours of admission and within 48 hours before hospital discharge by applying standard formulas.8, 9, 10
COSTS
Standardized costs for all billed inpatient and outpatient services for patients followed exclusively at Mayo Clinic and the two hospital campuses in Rochester were analyzed for the index hospitalization and up to 365 days after index discharge. Patients with follow‐up at the MCHS were excluded from the economic analysis. Hospitalization costs included professional and hospital services for the inpatient stay as well as for time spent in the emergency department or observation preceding admission. Some patients had only outpatient costs after index discharge. Costs, retrieved from the Mayo Clinic Rochester Cost Data Warehouse, were created by applying Medicare reimbursement to professional services, multiplying service‐line hospital charges by Medicare's cost report cost‐to‐charge ratios, and adjusting for inflation with the gross domestic product implicit price deflator. Disposition at 1 year was determined by review of electronic health records. For those patients whose medical records did not specify status at 1 year, survival status at 1 year was confirmed by phone call.
STATISTICAL ANALYSIS
Data were summarized as median (interquartile range) or mean (range) for continuous outcomes or counts and percentages for categorical outcomes. We used Wilcoxon rank sum tests for continuous data and the χ2 test or Fisher exact test for categorical data to determine differences between groups. Two‐tailed P values are reported, with P < 0.05 considered statistically significant. The C statistic was computed for the readmission regression model using admission and discharge variables. The validity of the models was confirmed by cross‐validation analyses using a random sample of 50% of the patients. To account for the potentially skewed distribution of health care costs, we used a generalized linear model with gamma distribution and logarithmic link that adjusted for sex, age, severity, age‐weighted sum of comorbid conditions, 30‐day readmission status, and baseline laboratory values.
Results
PATIENT POPULATION, ADMISSION, AND READMISSION RATES
Between January 1, 2010, and December 31, 2013, there were 7,915 patients admitted with complications of cirrhosis at two Mayo Clinic Hospital campuses in Rochester. After applying the inclusion and exclusion criteria, we identified 2,075 unique index admissions (Fig. 1). On manual review, we found that 27 patients did not have cirrhosis, and these patients were excluded. Therefore, 2,048 patients were included in our cohort. The causes of cirrhosis were as follows: alcoholic cirrhosis (n = 637, 31.1%), nonalcoholic steatohepatitis (n = 571, 27.9%), viral (n = 372, 18.2%), autoimmune (n = 148, 7.2%), and other (n = 320, 15.6%). The age‐adjusted incidence rate for admission for complications of cirrhosis was 100.1 (95% confidence interval [CI], 90.3, 109.8) per 100,000 population. The population used for adjusting was the 2010 U.S. census for Olmsted County. Age over 65 years and male sex were the greatest risks for index hospitalization, regardless of year of admission (Table 1; Fig. 2; Supporting Table S1). Admission rates for nonalcoholic steatohepatitis, autoimmune, and other causes increased with age, with the highest rates for admission in the over 65‐year age group. For alcoholic liver disease, admission rates leveled off after age 50 but peaked in the 50 to 65‐year age group for viral cause of cirrhosis. These admission trends for different causes of cirrhosis held true for both male and female sexes.
Figure 1.
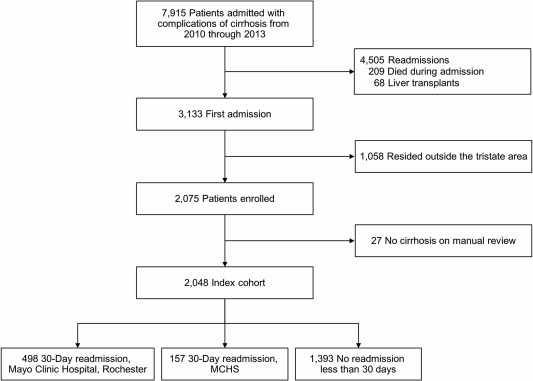
Flow diagram for enrollment and exclusion of the study patients. The tristate area is Minnesota, Iowa, and Wisconsin.
Table 1.
Incidence of Hospital Admission (2010 Through 2013) per 100,000 Population
| Age‐Adjusted Admission Rate (95% CI) | |||
|---|---|---|---|
| Admission | Women | Men | Total, Age‐Adjusted Admission Rate |
| All admissions | 80.2 (68.2‐92.2) | 122.8 (106.9‐138.8) | 100.1 (90.3‐109.8) |
| Alcohol | 14.5 (9.5‐19.6) | 43.5 (34.2‐52.8) | 28.1 (22.9‐33.2) |
| Autoimmune | 8.2 (4.4‐12.0) | 10.1 (5.4‐14.8) | 9.0 (6.0‐11.9) |
| Nonalcoholic steatohepatitis | 17.9 (12.3‐23.5) | 27.4 (19.9‐34.9) | 22.3 (17.7‐26.9) |
| Viral | 5.0 (2.0‐7.9) | 10.5 (6.0‐15.0) | 7.6 (5.0‐10.3) |
| Other | 33.8 (26.1‐41.6) | 30.3 (22.3‐38.2) | 32.1 (26.6‐37.7) |
Figure 2.
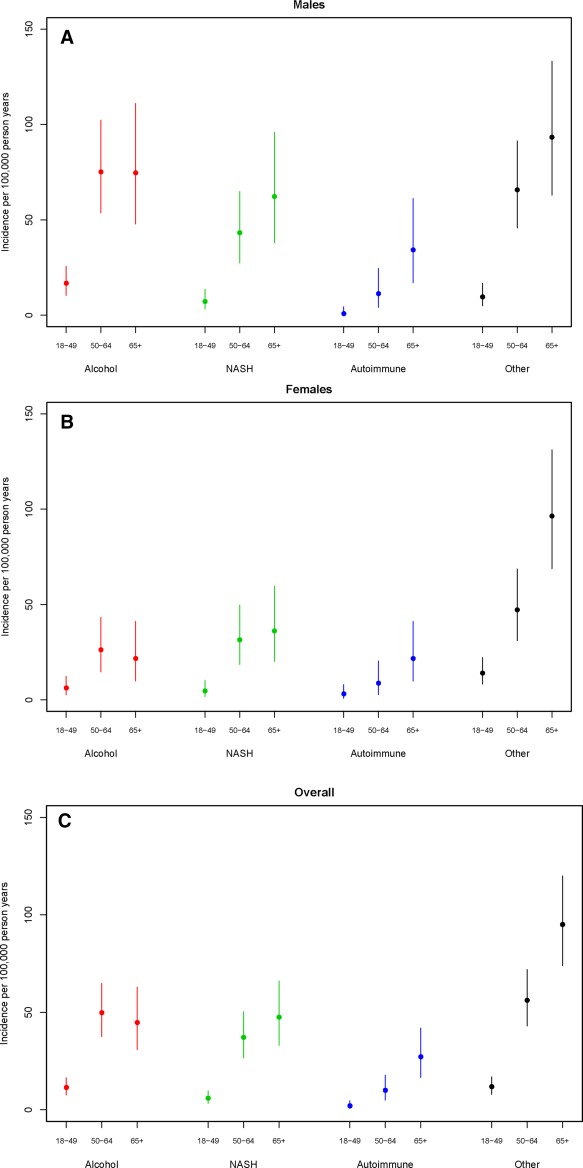
Incidence of hospitalization per 100,000 patient years for Olmsted County, Minnesota, by age, sex, and cause of cirrhosis. (A) Male sex; (B) female sex; (C) overall. Abbreviation: NASH, nonalcoholic steatohepatitis. Data point represents incidence and lines through the data point represent 95% confidence intervals.
Within 30 days, there were 498 readmissions at Mayo Clinic Hospital campuses in Rochester (24.3% of the index cohort) and 157 readmissions (7.7%) at community hospitals within the MCHS. The total 30‐day readmission rate was thus 32%. That is, of the 655 patient readmissions, 76% were to the Rochester hospitals and 24% to MCHS hospitals; 1,393 patients who were not readmitted within 30 days were the control group. The median interquartile range time to first readmission was 12 (5.75‐20) days. In‐hospital mortality among the readmission group was not different between the cohort at Mayo Clinic Hospital campuses in Rochester and the MCHS cohort (P = 0.73).
Demographic information, clinical characteristics, and details of each patient's index admission are listed in Table 2. The median age of patients in the index cohort was 60 years; 58.6% of patients were men (n = 1,200) and 89.6% were non‐Hispanic whites (n = 1,836). Comparisons of age and race between patients readmitted within 30 days and patients not readmitted within 30 days did not differ; men were statistically more likely to be readmitted than women on univariable analysis (P < 0.001) (Table 2).
Table 2.
Characteristics of the Index Hospital Admission
| Characteristic | Readmitted Within 30 Days (n = 655)a | Not Readmitted Within 30 Days (n = 1,393)a | P Value |
|---|---|---|---|
| Age, years | 60 (52‐70) | 60 (51‐70) | 0.66 |
| Men, % | 62.4 | 57.4 | <0.001 |
| Race, % | |||
| Non‐Hispanic white | 89.2 | 89.8 | 0.99 |
| Length of stay, days | 5 (3‐10) | 4 (2‐6) | <0.001 |
| Date of index admission | |||
| WBC count (/1,000 mm3) | 8.3 (5.6‐12.5) | 7.4 (5.1‐10.6) | <0.001 |
| Platelet count (/1,000 mm3) | 138 (84‐214) | 136 (82‐200) | <0.001 |
| Serum albumin level (g/dL) | 2.9 (2.5‐3.3) | 3.0 (2.5‐3.4) | 0.02 |
| MELD score | 18 (12.0‐23.0) | 14 (10.0‐19.0) | <0.001 |
| MELD‐Na score | 21 (14.4‐27.5) | 17.1 (12.9‐22.5) | <0.001 |
| Date of discharge from the index admission | |||
| MELD score | 17 (11.0‐24.0) | 13 (9.5‐18.0) | <0.001 |
| MELD‐Na score | 20.2 (14.0‐26.0) | 16 (11.2‐20.8) | <0.001 |
| Cause of cirrhosis, n (%) | |||
| Alcohol | 262 (40) | 375 (27) | <0.001 |
| Nonalcoholic steatohepatitis | 125 (19) | 446 (32) | <0.001 |
| Autoimmune disease | 59 (9) | 89 (6.4) | 0.059 |
| Viral | 137 (21) | 235 (16.9) | 0.007 |
| Other | 72 (11) | 248 (17.8) | 0.008 |
| Disposition, % | |||
| Home | 39.4 | 67.5 | <0.001 |
| Skilled nursing facility | 33.7 | 21.6 | <0.001 |
| Rehabilitation facility | 2.2 | 1.1 | 0.07 |
| Home hospice care | 6.8 | 5.2 | 0.18 |
| Nursing home | 17.9 | 4.6 | <0.001 |
Values are expressed as median (interquartile range) unless otherwise specified.
Abbreviations: WBC, white blood cell.
REASONS FOR READMISSION
Infection was the most common reason for readmission at tertiary‐care hospitals within 30 days and at specific time points (7, 14, and 30 days). At community hospitals, hepatic encephalopathy without obvious infection and ascites and its complications were the most common reasons for readmission (Table 3).
Table 3.
Reasons for 30‐Day Readmission
| Reason | Mayo Clinic Hospital, Rochester Campuses, (n = 498) | Mayo Clinic Health System, Community Hospitals, % (n = 157) |
|---|---|---|
| Infection | 32.7 | 22.0 |
| Hepatic encephalopathy without obvious infection | 8.6 | 29.5 |
| Renal dysfunction | 21.2 | 14.6 |
| Bleeding esophageal varices | 12.0 | 5.2 |
| Ascites and complications | 10.2 | 28.0 |
| Alcohol‐related causes | 8.0 | 0 |
| Cardiovascular‐related admission | 4.4 | 0.7 |
| Non‐liver‐related cause | 1.2 | 0 |
| Other | 1.7 | 0 |
VARIABLES ASSOCIATED WITH 30‐DAY READMISSION
Among patients readmitted within 30 days, 57% had alcoholic liver disease (40% alcoholic cirrhosis, 17% alcoholic cirrhosis and hepatitis C infection). Alcoholic liver disease was a significant readmission predictor (hazard ratio [HR], 1.469; 95% CI, 1.142, 1.863; P = 0.004). Readmitted patients had higher white blood cell counts (P < 0.001), higher MELD and MELD‐Na scores (P < 0.001), lower albumin levels (P = 0.02), and longer lengths of stay (P < 0.001) (Table 2). Laboratory data compared between both groups are summarized in Table 4. There were 24 significant variables associated with 30‐day readmission in univariate analysis; only MELD and MELD‐Na scores; serum creatinine, sodium, total bilirubin, and alkaline phosphatase levels; international normalized ratio; and white blood cell count were statistically significant both at admission and discharge dates. The MELD‐Na score (HR, 1.047; 95% CI, 1.034, 1.060; P < 0.001) was a marginally better predictor than MELD score (HR, 1.044; 95% CI, 1.029, 1.054; P < 0.001).
Table 4.
Laboratory Parameters and Meld Score at Admission and on The Discharge Date
| Variable | Admission Date | Discharge Date | ||||
|---|---|---|---|---|---|---|
| Readmitted Within 30 Days (n = 498) | Not Readmitted Within 30 Days (n = 1,393) | P Value | Readmitted Within 30 Days (n = 498) | Not Readmitted Within 30 Days (n = 1,393) | P Value | |
| Creatinine (mg/dL) | 1.0 (0.7‐1.7) | 0.9 (0.7‐1.3) | 0.001 | 1.0 (0.7‐1.5) | 0.9 (0.7‐1.2) | <0.001 |
| Sodium (mmol/L) | 135 (131‐139) | 137 (134‐139) | <0.001 | 136 (133‐139) | 138 (135‐140) | <0.001 |
| Total bilirubin (mg/dL) | 2.0 (0.8‐5.0) | 1.4 (0.7‐3.1) | <0.001 | 1.8 (0.8‐5.6) | 1.3 (0.7‐2.9) | <0.001 |
| Serum albumin (g/dL) | 2.9 (2.5‐3.3) | 3.0 (2.5‐3.4) | 0.02 | 2.9 (2.5‐3.4) | 3.1 (2.6‐3.5) | 0.053 |
| AST (U/L) | 63 (37‐130) | 53 (34‐101) | 0.37 | 54 (33‐101) | 48 (33‐85) | <0.001 |
| ALT (U/L) | 38 (23‐68) | 33 (21‐64) | 0.67 | 33 (20‐60) | 31 (19‐56) | 0.20 |
| ALP (U/L) | 132 (88‐227) | 113 (80‐173) | <0.001 | 123 (85‐195) | 109 (76‐165) | <0.001 |
| INR | 1.4 (1.2‐1.9) | 1.3 (1.1‐1.6) | 0.006 | 1.4 (1.2‐1.8) | 1.3 (1.1‐1.6) | <0.001 |
| Hemoglobin (g/dL) | 10.9 (9.4‐12.5) | 11.2 (9.6‐12.7) | 0.14 | 10 (9.0‐11.3) | 10.4 (9.3‐11.8) | <0.001 |
| WBC count (×109/L) | 8.3 (5.6‐12.5) | 7.4 (5.1‐10.6) | <0.001 | 7 (4.9‐9.9) | 6.4 (4.5‐8.6) | <0.001 |
| Platelet count (×109/L) | 138 (84‐214) | 136 (82‐200) | <0.001 | 122 (71‐198) | 128 (79‐194) | 0.96 |
| MELD score category, n (%)a | ||||||
| MELD score, median (IQR) | 18 (12.0‐23.0) | 14 (10.0‐19.0) | <0.001 | 17 (11‐24) | 13 (9.5‐18.0) | <0.001 |
| MELD ≤ 15 | 152 (40.5) | 564 (58.8) | <0.001 | 156 (41.6) | 591 (61.6) | <0.001 |
| MELD 16‐20 | 89 (23.7) | 193 (20.1) | 87 (23.2) | 219 (22.8) | ||
| MELD 21‐30 | 104 (27.7) | 161 (16.8) | 108 (28.8) | 130 (13.5) | ||
| MELD > 30 | 30 (8.0) | 42 (4.4) | 24 (6.4) | 20 (2.1) | ||
| MELD‐Na score category, n (%)a | ||||||
| MELD‐Na score, median (IQR) | 21 (14.4‐27.5) | 17.1 (12.9‐22.5) | <0.001 | 20.2 (14‐26) | 16 (11.2‐20.8) | <0.001 |
| MELD‐Na ≤ 15 | 96 (25.6) | 357 (37.3) | <0.001 | 112 (29.9) | 439 (45.9) | <0.001 |
| MELD‐Na 16‐20 | 78 (20.8) | 265 (27.7) | 72 (19.2) | 241 (25.2) | ||
| MELD‐Na 21‐30 | 150 (40.0) | 265 (27.7) | 144 (38.4) | 241 (25.2) | ||
| MELD‐Na > 30 | 51 (13.6) | 70 (7.3) | 47 (12.5) | 36 (3.8) | ||
Unless otherwise indicated.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; INR, international normalized ratio; IQR, interquartile range; WBC, white blood cell.
The best model to predict 30‐day readmission used the MELD‐Na score on the discharge date, length of stay, and platelet count on the admission day; however, the C statistic was only 0.63. The score for predicting readmission was calculated as 0.1207 × exp(0.0139 × [platelet count/10,000 mm3 on admission date] + 0.0139 × [length of stay] + 0.0459 × [MELD‐Na score on discharge date]). Inclusion of alcoholic liver disease as a variable did not improve the C statistic of the model (0.64).
COSTS OF HOSPITALIZATION AND READMISSION
No difference was shown in index hospitalization costs for patients with and without a 30‐day readmission ($25,610 versus $25,571). However, there was a substantial difference in postindex hospitalization costs among the three groups ($73,252 for patients readmitted within 30 days and $62,053 for those readmitted beyond 30 days versus $5,719 for patients not readmitted) (Fig. 3). Costs among the patients discharged to a skilled nursing facility or discharged to nursing homes or home hospice care after the index admission could not be captured. Additional detailed and summarized descriptive costs (1 year after initial hospitalization) for patients with and without a 30‐day readmission are presented in Supporting Table S2.
Figure 3.
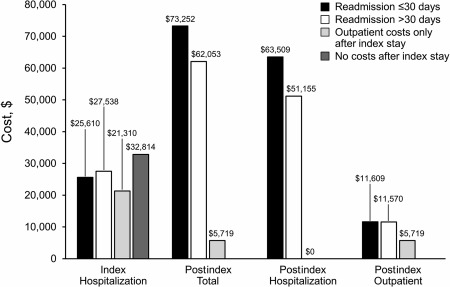
Average standardized costs per patient for patients with and without 30‐day readmission.
OUTCOME 1 YEAR AFTER HOSPITAL DISCHARGE
Among the 498 patients readmitted in Rochester within 30 days, the 1‐year mortality rate was higher than for those not readmitted (50.4% versus 15.9%, P = 0.001). There were 146 in‐hospital deaths during readmission and 105 out‐of‐hospital deaths, or 251 total deaths (50.4%) within 1 year of the initial hospital admission. Readmitted patients were discharged home less frequently after index admission than those without a 30‐day readmission (39.4% and 67.5%, P < 0.001) and more often to a skilled nursing facility (33.7% and 21.6%, P < 0.001). A higher MELD score and lower platelet count were associated with discharge to a nursing home or to home hospice care. The readmission group had a median of three readmissions during the 1‐year follow‐up. At the end of 1 year, only 102 patients (20.5%) were at home, 36 (7.2%) were in skilled nursing facilities, 13 (2.6%) were in rehabilitation centers, and 96 (19.3%) were either in hospice care or nursing homes.
Discussion
Our study has six key findings. First, age and male sex are risk factors for index admission for complications of cirrhosis regardless of year of admission. Second, readmission rates are high in this population. Third, the best readmission predictive model, which includes MELD‐Na, length of stay, and platelet count, has poor discriminative ability. Fourth, postindex hospitalization costs for those with 30‐day readmission are substantially higher than those without 30‐day readmission; based on these costs, the cost of readmission nationally is estimated to be more than $4.45 billion annually. Fifth, the lowest costs incurred are for patients who have no readmissions at 1 year. Finally, the 1‐year outcome for any patient with cirrhosis readmitted within 30 days is dismal, with only 20% of patients alive and at home.
Our previous study of all admissions for cirrhosis in the country, which used the National Inpatient Sample database, suggested that there were 659,000 admissions for cirrhosis in the United States in 2011.11 If we apply the admission rate of 100 per 100,000 population for initial hospitalization for cirrhosis in Olmsted County, the number of initial hospitalizations for cirrhosis in the United States for 2011 is estimated to have been 310,000. Therefore, roughly one half of all admissions in the United States for cirrhosis are initial admissions and the rest are assumed to be readmissions. The highest risk for readmission was increasing age, which is concerning, especially among patients over 65 years. As a result, Medicare costs for hospitalization for cirrhosis are likely to increase. These patients are also unlikely to be candidates for a liver transplant given their age; therefore, they are at high mortality risk. In addition, the caregiver burden is likely to fall on the younger productive population and to put their job security at risk.
Our readmission rates of 32% are consistent with those of previous studies from single tertiary‐care centers.1, 2 A report of a multistate population‐based cohort study showed the 30‐day rate of readmission to be only 12.9%.4 It is unclear how precise the diagnosis of cirrhosis was in that study and whether the admission was the first for complications of cirrhosis; cirrhosis severity was not known, and long‐term outcomes were not available. If only tertiary‐care center hospitalizations are captured, the number of readmissions may also be underestimated.12 Our data are probably reflective of the true readmission risk because they are derived from both referral and community hospitals and include only patients resident within a geographically localized area. Of note, according to the U.S. Census Bureau, demographic data, education, income, and health insurance status from the tristate area of Minnesota, Iowa, and Wisconsin are similar to that of the rest of the country.13
The independent predictors of 30‐day readmission were cirrhosis severity (as determined by a higher MELD‐Na score), length of stay, and platelet count. Patients with longer hospitalizations may have more complicated disease and are at greater risk for health care‐associated infection. In fact, infection was a major reason for 30‐day readmission of patients in both referral and community hospitals. However, the North American Consortium for the Study of End‐Stage Liver Disease prospectively evaluated a cohort of patients with cirrhosis and found that a longer length of stay was associated with reduced 90‐day readmission; a 30‐day readmission rate was not studied.3
The model used to predict risk of 30‐day readmission was developed with goals of helping in discharge planning and targeting patients at high‐risk for readmission, but it had only moderate discriminative ability. Inability to accurately predict readmissions is consistent with a systematic review of risk prediction models for hospital readmission in general.14 Quality of care, patient satisfaction, coordination of care with the provider, postdischarge follow‐up, and individual patient factors, such as demographic characteristics, patient capacity for self‐care, cultural norms, and socioeconomic and health insurance status, are all associated with readmission risk but are not easily measurable. Although age was not a significant factor for readmission, the degree of frailty among individual patients and the inability of a caregiver to cope with parental illness may be unmeasurable risk factors both for admission and for readmission. The absence of an accurate model to predict groups of patients at risk for readmission will hamper efforts to decrease readmission.
We chose to focus on 30‐day readmissions instead of a longer period, such as 90‐day readmission, because a shorter time to readmission is more likely related to the index hospitalization than a longer period. Moreover, the Centers for Medicare and Medicaid Services has focused on reducing the rate of 30‐day readmission.15 When incentives were provided in the Affordable Care Act, readmission rates decreased.16 The annual costs among our patients readmitted within 30 days were $67,533 higher than for patients not readmitted within 1 year, even though costs for the index hospitalization were similar. The true costs are likely to be far higher (we estimated $4.45 billion for 310,000 readmissions) because the costs of nursing home, skilled nursing facility, and home health care were not captured. The key to reducing costs nationally is to identify which risk factors account for readmission and, more importantly, which factors favor a patient remaining an outpatient.
Our study also illustrates the high mortality rate and poor outcomes for patients within 1 year following hospital discharge. Infection and alcoholic liver disease were the major causes of readmissions, but infection and alcoholic liver disease at index admission were not factors independently predictive of readmission. Male sex was a risk factor for readmissions, likely related to the higher prevalence of alcoholic cirrhosis among male individuals. Patients with alcoholic liver disease are prone to infections,17 and patients with cirrhosis and health care‐associated infections have been reported to be at risk for readmission.18 Continued alcohol use also impairs cognitive function and may be associated with poor adherence to follow‐up visits and medication use.19 We made every effort to determine drinking patterns following hospital dismissal but could not glean this information with confidence from the records available in this retrospective study. Patients who are alcoholics may also have less social support than other patients. Even though patients are usually discharged after adequate control of their infection, they remain at high risk for subsequent infections requiring hospitalization, and these infections are usually a different type compared to the initial infection.20 Therefore, reduction of health care‐associated infections may be another strategy to reduce hospital readmissions. Strategies to reduce readmission could also include more aggressive measures to combat alcoholism, but efforts in this direction may have only limited success.
Hepatic encephalopathy has emerged as a leading reason for readmission. From our study, overt hepatic encephalopathy was the most common cause of readmission within community hospitals, similar to findings of the prospective North American Consortium for the Study of End‐Stage Liver Disease study from major North American referral centers.3 Patients with hepatic encephalopathy have impaired cognitive and affective capabilities that may lead to poor adherence with medication regimens and hospital follow‐up visits. The residual effects of hepatic encephalopathy on cognitive function may result in learning impairment despite appropriate treatment.21 Moreover, patients with even mild cognitive impairment may have a greater risk of hospitalization than patients with normal cognition.22 Therefore, education of caregivers may be a strategy that can be used to reduce readmission in this high‐risk group.
The strengths of our study include identification of patients with cirrhosis with a high degree of accuracy, follow‐up from the first hospitalization for cirrhosis, capture of readmissions at community hospitals, determination of risk factors associated with readmissions, and annual cost and disposition data. Our study, however, also has limitations. First, this study is not a true community‐based study because possible readmissions at hospitals outside our system are not captured in the database. Second, factors influencing readmission, such as socioeconomic status, patient income, level of education, and patient capacity for self‐care were not analyzed. Finally, we did not validate the model to predict risk of 30‐day readmission in an external cohort.
In summary, this study identified age and sex as major risk factors for initial hospitalization and a high rate of 30‐day readmission in patients with cirrhosis. The MELD‐Na score, platelet count, and length of stay are independent predictors of readmission, but the model to predict risk for readmission had poor discriminative ability. Postindex hospitalization costs for those readmitted are high, especially so in the group readmitted within 30 days. Moreover, at 1 year, only a minority of patients have their care managed at home, highlighting the devastating outcome of readmission for complications of cirrhosis. In the absence of a model that accurately identifies patient groups at high risk for readmission, strategies to reduce readmission may not be successful.
Supporting information
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep4.1137/full.
eTable 1.
eTable 2. Detailed Descriptive Standardized Costs for Patients With and Without 30‐Day Readmission
Potential conflict of interest: Nothing to report.
Supported by National Institutes of Health (NIH) Grant Number AA 21788 from the National Institute on Alcohol Abuse and Alcoholism (to V.H.S. and P.S.K.) and was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (to S.C.), a component of the NIH; support also received from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery (to B.J.B. and S.L.V.). In addition, this study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the NIH under Award Number R01AG034676.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Berman K, Tandra S, Forssell K, Vuppalanchi R, Burton JR Jr, Nguyen J, et al. Incidence and predictors of 30‐day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol 2011;9:254‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol 2012;107:247‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia‐Tsao G, et al. The 3‐month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology 2016;64:200‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tapper EB, Halbert B, Mellinger J. Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population‐based cohort study. Clin Gastroenterol Hepatol 2016;14:1181‐1188.e2. [DOI] [PubMed] [Google Scholar]
- 5. Melton LJ 3rd. History of the Rochester Epidemiology Project. Mayo Clin Proc 1996;71:266‐274. [DOI] [PubMed] [Google Scholar]
- 6. Nehra MS, Ma Y, Clark C, Amarasingham R, Rockey DC, Singal AG. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol 2013;47:e50‐e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative databases. J Clin Epidemiol 1992;45:613‐619. [DOI] [PubMed] [Google Scholar]
- 8. Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end‐stage liver disease. Hepatology 2001;33:464‐470. [DOI] [PubMed] [Google Scholar]
- 9. Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al.; United Network for Organ Sharing Liver Disease Severity Score Committee . Model for end‐stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003;124:91‐96. [DOI] [PubMed] [Google Scholar]
- 10. Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, et al. Hyponatremia and mortality among patients on the liver‐transplant waiting list. N Engl J Med 2008;359:1018‐1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Allen AM, Kim WR, Moriarty JP, Shah ND, Larson JJ, Kamath PS. Time trends in the health care burden and mortality of acute on chronic liver failure in the United States. Hepatology 2016;64:2165‐2172. [DOI] [PubMed] [Google Scholar]
- 12. Chirapongsathorn S, Kamath PS. Hospital readmissions in decompensated cirrhosis. Am J Gastroenterol 2015;110:940. [DOI] [PubMed] [Google Scholar]
- 13. United States Census Bureau . QuickFacts: Minnesota; Iowa; Wisconsin. http://www.census.gov/quickfacts/table/PST045215/27,19,55. Accessed April 26, 2017.
- 14. Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, et al. Risk prediction models for hospital readmission: a systematic review. JAMA 2011;306:1688‐1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The White House . Jumpstarting the economy and investing for the future. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed December 15, 2017.
- 16. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med 2016;374:1543‐1551. [DOI] [PubMed] [Google Scholar]
- 17. Chan C, Levitsky J. Infection and alcoholic liver disease. Clin Liver Dis 2016;20:595‐606. [DOI] [PubMed] [Google Scholar]
- 18. Emerson CB, Eyzaguirre LM, Albrecht JS, Comer AC, Harris AD, Furuno JP. Healthcare‐associated infection and hospital readmission. Infect Control Hosp Epidemiol 2012;33:539‐544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag 2005;1:189‐199. [PMC free article] [PubMed] [Google Scholar]
- 20. O'Leary JG, Reddy KR, Wong F, Kamath PS, Patton HM, Biggins SW, et al.; North American Consortium for the Study of End‐Stage Liver Disease . Long‐term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clin Gastroenterol Hepatol 2015;13:753‐759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bajaj JS, Schubert CM, Heuman DM, Wade JB, Gibson DP, Topaz A, et al. Persistence of cognitive impairment after resolution of overt hepatic encephalopathy. Gastroenterology 2010;138:2332‐2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Callahan KE, Lovato JF, Miller ME, Easterling D, Snitz B, Williamson JD. Associations between mild cognitive impairment and hospitalization and readmission. J Am Geriatr Soc 2015;63:1880‐1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep4.1137/full.
eTable 1.
eTable 2. Detailed Descriptive Standardized Costs for Patients With and Without 30‐Day Readmission


