Abstract
Background
Adolescents with brain injury (BI) often experience impairment in participation, which is an important predictor of outcomes.
Objective
Describe the Social Participation and Navigation (SPAN) program, and report participant feedback and preliminary outcomes.
Method
Four adolescents and four coaches participated. SPAN included a mobile app, online didactic information, and peer coaching. Adolescents met weekly with coaches via video-conference, developed participation goals, and plans to achieve goals. Social and behavioral functioning before and after was assessed, and feedback about SPAN was collected.
Results
SPAN was well received. Participants used the app to define and achieve goals. Medium to large effect sizes were found on adolescent self-reported measures, with negligible effects on parent-report measures. Positive and critical feedback is described.
Conclusions
Findings support the usability of SPAN, which has the potential to improve social participation of adolescents with a history of TBI through an innovative use of technology and peer coaching.
Keywords: Pediatric traumatic brain injury, peer coaching, social participation
Adolescents with Traumatic Brain Injury (TBI) often experience significant and persistent deficits in social competence.1,2 Specific impairments in social cognition include recognition of emotions,3–5 theory of mind, including the ability to make inferences about feelings and intentions of others,6–8 and social problem solving.9 These deficits result in limitations in their social performance and participation in school and the community as well as social isolation, lack of meaningful friendships, and exclusion from social opportunities.10–17 Social competence is an important predictor of a number of outcomes following TBI including overall adjustment, academic achievement, and quality of life.2,18 Additionally, TBI often results in changes in social communication and behavior that lead to alterations in existing relationships and make establishing new friendships more difficult.19–21 TBI survivors can have difficulty reading cues in social situations, including irony and sarcasm, and generating socially appropriate responses.22 Increased emotional lability, anger, and impulsivity may also tax existing relationships23; fatigue, low levels of initiation, and difficulties with goal setting may limit pursuit of social activities outside of school. Because most students with TBI do not appear visibly different from before, peers may have difficulty attributing changes in their interactions to the injury and may limit future contact because the relationship has changed.
Social participation is defined as the nature and extent of an individual’s involvement in social situations that may occur in a variety of contexts including home, school, and the community.24 Social participation contributes to enhanced quality of life, physical heath, and daily functioning of adolescents with and without disabilities.11,13,25–28 Pediatric TBI adversely affects social participation in a variety of ways. Hospitalization and activity restrictions remove children from their typical forms of participation (e.g., sports). Children with more severe injuries may have to give up preferred activities permanently, creating lasting changes in the nature of their participation. Seizures and visual impairments may prevent some adolescents with TBI from being able to drive to activities like their peers, and anxiety around re-injury may hamper participation at previous levels. Finally, deficits in participation may also contribute to the documented employment limitations in adolescents and young adults with TBI.29–32
Facilitating social participation may contribute to improvements in a range of important functional outcomes; however, research aimed at developing social participation is severely lacking.33 Further, a number of barriers to identifying and addressing social participation challenges exist. First, in clinical settings, adolescents with TBI and their parents may focus on physical, cognitive, and behavioral problems rather than pro-social functioning, so social participation might not be identified as a concern. Second, providers may not have resources to offer families because evidence-based approaches to promoting social participation are lacking.33 While there are interventions that are designed to address social concerns following TBI, they target social skills as well as promotion of social relationships and even these have shown limited effectiveness and generalization.34–36 Most social-skills-type interventions operate from the assumption that the adolescent lacks knowledge or understanding of social rules, roles, and routines (e.g., PEERS curriculum;37). However, this is not the case for adolescents with a history of TBI.38 Rather, many adolescents with a history of TBI possess the required social knowledge, but lack awareness of social deficits, do not apply knowledge to real world settings,38 have difficulties with self-regulation38 and evaluating solutions when problem solving in social situations, and often select developmentally immature strategies for solving social problems.39 Glang and colleagues36 designed a school-based problem-solving intervention aimed at increasing social contacts for children and adolescents with a history of TBI. While improvements were noted during the study period, they were not maintained over time. A third barrier is that school-based interventions may be challenging to implement given difficulties coordinating with school administration and limited time during the school day. Finally, it has been demonstrated that the family system is a crucial part of positive recovery after pediatric TBI40,41; however, as patients progress toward adolescence, the impact of peers and their social milieu becomes increasingly relevant. The importance of peers combined with evidence that peer coaches are effective in facilitating behavioral change42–44 points toward the use of peers or peer groups to promote social participation.45–47
In addition to the dearth of evidence-based interventions, there are significant barriers to the delivery of these interventions. Outpatient services may be unavailable altogether, or families may be forced to travel to obtain appropriate care. Geographical access barriers may be overcome by delivering intervention through an internet or telehealth medium. Recent studies suggest that telehealth approaches provide an effective means of delivering interventions to adolescents with TBI and their families while reducing barriers such as time, distance, and available transportation.48 According to a recent report from the Pew Internet and American Life Project,49,50 adolescents are using smartphones and social networks at increasing rates, underscoring the potential utility of telehealth approaches for intervening with adolescents.
In summary, there is a need for accessible, peer-mediated, evidence-based, and participation-focused interventions for adolescents with TBI. Researchers have proposed a number of strategies to address this need, including the use of peer coaches,51,52 access to intervention materials after program completion,36 and interventions that focus on the development of problem-solving skills and promote developmentally appropriate social strategies.39 Following these recommendations, we developed a new program, Social Participation and Navigation (SPAN), to facilitate social participation in adolescents with TBI. The SPAN program is a multi-pronged intervention developed to address limitations of previous intervention methods. SPAN is a technologically supported integration of mobile app-based training, peer-coach support, and online didactic content around key aspects of social participation, including social communication and problem-solving skills, identification and remediation of barriers to participation, and connecting to others. SPAN is an innovative solution that takes advantage of ongoing technological advances in smartphone design and capabilities.
This report describes the SPAN program and reports preliminary usability and feasibility data from a 4-week feasibility trial. Our aims were to: (1) describe the SPAN program; (2) determine usability of the SPAN program for adolescents with TBI, supported by trained college student coaches, to establish and achieve a social participation goal; and (3) identify areas for modification prior to a larger 10-week implementation pilot trial. As an exploratory examination of efficacy, we also examined changes in adolescent and parent reported outcomes over the course of the 4-week trial to evaluate the utility of our outcome measures and explore potential benefits of a 4-week version of the program.
Method
Prior to engaging adolescents and coaches in the SPAN program, we developed the program and program materials in an iterative process, with feedback from stakeholders and focus groups. Results of that process are described elsewhere.53 Participants in the current project were four adolescents who sustained a complicated mild to severe TBI during childhood (mean age at injury = 7.27 years). See Table 1 for detailed demographic information. To qualify for the study, adolescents had to be sufficiently recovered to actively participate in the intervention. Parents were asked to rate their satisfaction with their adolescent’s level of social participation, and children were only included if parents described dissatisfaction with either the quality or quantity of their adolescent’s social participation and a desire for their adolescent to improve their level of social participation. After parents provided informed consent and participating adolescents provided assent, both completed measures of social competence, behavior, and communication. Adolescents then received an orientation to SPAN, built their SPAN profile (see description next), and were introduced to their coach via Skype videoconference. Each adolescent and his or her coach met weekly via videoconference to identify and implement social participation goals. At completion of the 4-week trial, participants and their parents completed questionnaires regarding ease of use and satisfaction with the program, as well as the measures of social competence, behavior, and communication completed at baseline.
Table 1.
Detailed participant demographic information.
| Adolescent | Gender | Age | Age At Injury | Mechanism Of Injury | Injury Details | GCS | LOS |
|---|---|---|---|---|---|---|---|
| 1 | Female | 14 | 5 Yrs 2 Mo | Hit Head On Metal Pole | Subarachnoid Hemorrhage; Skull Fracture | 15 | 1 |
| 2 | Male | 14 | 11 Yrs 5 Mo | ATV Accident Without A Helmet | Subdural Hematoma | 3 | 5 |
| 3 | Female | 17 | 6yrs 7 Mo | Fell Down Stairs | Parenchymal Contusion, Extra-Axial Hematoma, Skull Fracture | 10 | 5 |
| 4 | Female | 15 | 5 Yrs 11 Mo | Trampled And Dragged By Horse | Subdural Hemorrhage, Extra-Axial Hemorrhage, Depressed Skull Fracture | 8 | 91 |
Note. GCS = Glasgow Coma Scale score; LOS = Length of hospital stay; yrs = years; mo = months.
The SPAN program
The SPAN program has three main components: a dedicated iPhone app, a website with Key Topics and Brief Tips (described below), and weekly videoconferencing sessions (via Skype) with a trained college-student coach. The program is designed to allow adolescents with TBI to develop and implement social participation goals with individual support from a coach. Figure 1 is an overview of SPAN. With the initial log on, the app asks the adolescent a series of questions to “build my profile.” Questions focus on the participant’s interests and likes, current level of participation, current supports and challenges, and strategies for achieving goals.
Figure 1.
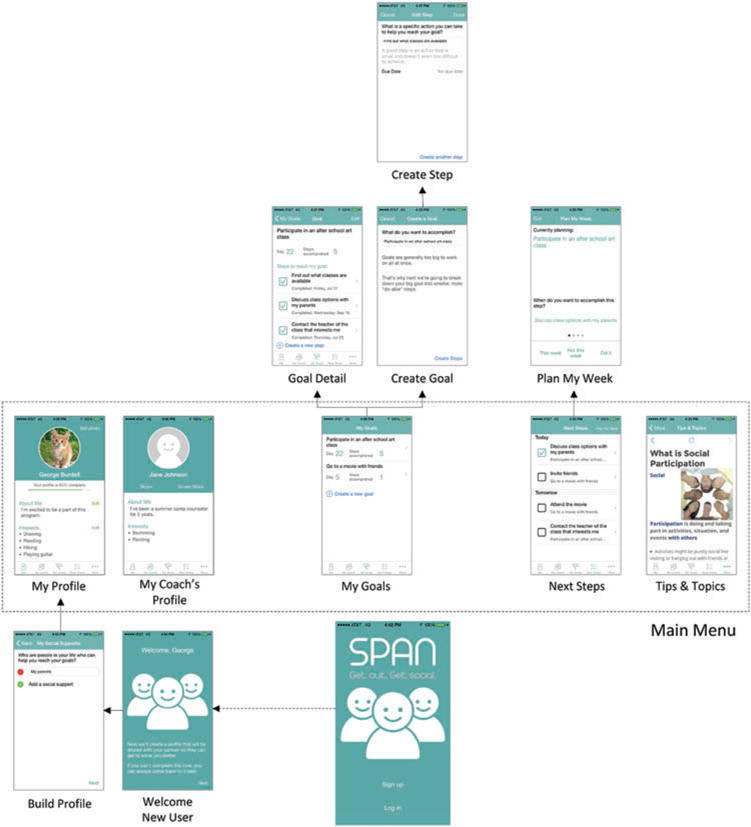
Overview of SPAN app. Images show screen shots from the initial log on page, as well as the processes of building a user profile, setting goals, and identifying steps to achieve goals.
Coaches
SPAN was designed to include undergraduate college student coaches; however, for the current project, coaches were graduate students in speech-language pathology, neuroscience, and occupational therapy with prior knowledge of TBI. A training manual and 2-hour coach training were developed by an interdisciplinary team (one occupational therapist, one clinical psychologist, and two speech-language pathologists) drawing on existing manuals from programs providing coaching and problem-solving training to adolescents with TBI.54–56 All coaches participated in weekly virtual group supervision with a clinical psychologist and occupational therapist. Coaches were located at two of the participating sites and had additional meetings with their on-site supervisors as needed. Coaches kept detailed session notes and recorded their sessions to ensure fidelity to the principles of the intervention. Coach-adolescent sessions were about 45–60 min long. During this time, the coach would discuss events from the past week, review plan from last session (highlighting steps the adolescent was scheduled to completed since last session), identify barriers to step/goal achievement, problem solve around identified barriers, plan for upcoming steps, and celebrate successes. In total, coaches spent approximately three hours engaged in SPAN related activities per week: one hour with adolescent participation, one hour with the on-site mentor, and at least one hour of virtual supervision. Coaches also provided feedback about the challenges encountered throughout the program, using the app, and the coaching process.
Procedures
The program began when the adolescent initially logged in to the app, which prompted the adolescent with a series of questions to “build my profile.” Next, during the initial videoconference meeting, the coach and adolescent shared their profiles and discussed current activities and potential participation goals. During a second videoconference session, the participant and coach used the app goal-planning feature to establish a specific participation goal and defined specific steps and timelines for goal achievement. In subsequent coaching sessions, the coach and participant reviewed progress toward achieving goals, modified steps and timelines as needed, identified and problem solved around potential barriers, and identified strategies to facilitate successful goal achievement. Texts and e-mails were used as reminders to implement steps and reinforce step completion.
Didactic content
Coaches and participants were encouraged to access information on a dedicated website that contained didactic information and Key Topics. The website content was developed to provide an introduction to SPAN as well as information regarding: (1) social participation, (2) goal setting and problem solving around social participation, (3) staying positive, and (4) staying in control/self-regulation. We developed Brief Tips on the same topics, as well as Tips for joining a conversation, so participants and coaches had a one-page resource with heuristics to support the Key Topics, allowing access to strategies on the fly while implementing planned steps.
Measures
Participant and parent satisfaction
We developed a brief questionnaire to assess ease of use and helpfulness of various aspects of the program. Items assessed satisfaction with a number of themes: overall program (i.e., Program was too long/short, the program was what I expected), the mobile app (i.e., I liked using the app to set goals, the app was useful, using the app was easy), Brief Tips and Key Topics (i.e., Brief Tips/Key Topics were easy to understand, liked using the Brief Tips/Key Topics, and Brief Tips/Key Topics were useful), and coaching (i.e., working with my coach was easy, I liked working with my coach, the coaching was useful). Parents, participants and coaches responded using a Likert-type scale from 1 (strongly disagree) to 5 (strongly agree). The questionnaire also included open-ended questions for all aspects of the program (e.g., what did you like most about the program, what did you like least about the program) for all aspects of the program to gather additional information and inform program revision.
Goal achievement
We assessed the number and type of goals achieved by each participant. Data were gathered from coaches reports in their session notes, which were based on their review of goals and planned steps entered into the app and weekly discussions with their participants.
Social competence and problems
Participants completed the Youth Self Report (YSR) and their parents completed the Child Behavior Checklist (CBCL;57 to provide information about perceived social competence and social problems. Both scales have excellent reliability and validity, and the CBCL social competence scales were recommended as part of the pediatric TBI common Data Elements.58 The CBCL includes 20 items measuring the child’s participation in hobbies, games, sports, jobs, chores, friendship, and activities. These items comprise the Social Competence index, which provided a measure of perceived social competence. The score for total behavior problems and the subscale score for social problems were examined to identify potential improvements in problem behaviors that adversely affect social participation. The CBCL and YSR were collected pre- and post-intervention to evaluate how these measures function within the parameters of the intervention and to assess perceived change in social competence, social problems, and total problems.
Results
Four white adolescents (3 girls and 1 boy) ages 14–17 (M = 15.73) with a history of complicated mild to severe TBI (mean time since injury = 8.46 years) participated in the project. Participant characteristics are shown in Table 1. Participants had a range of injury severity (2 severe TBI, 1 moderate TBI, 1 complicated mild TBI; Table 1). Three of the participants had experienced largely positive recoveries with minimal functional impairments, while one participant continued to experience significant impairments associated with her injury. This range of injury severity and extent of recovery allowed for examination of the feasibility and utility of SPAN across adolescents with a range of functioning.
Due to the small sample size, nonparametric Wilcoxon Signed Rank tests were used to examine pre–post scores. Also, given the small sample size, we used effect sizes (Cohen’s d) as a preliminary estimate of intervention effects.
Feedback and user satisfaction from questionnaires
Adolescent, parent, and coach feedback and user satisfaction ratings were obtained via questionnaires. Responses to open-ended questions are presented in Tables 2 and 3, the categories presented in the tables are consistent with the categories assessed on the satisfaction questionnaire, and responses reported by more than one person are noted in the tables. Responses pertaining to the benefits of SPAN are presented in Table 2. Overall, all felt that the program and app provided appropriate scaffolding for goal setting and management, and coach involvement was noted as a very positive aspect of the intervention. However, adolescents, parents, and coaches also provided critical feedback and suggestions for improving SPAN which are presented in Table 3. The most common critical feedback and suggestions for adaptations included clarifying parent involvement, limiting complexity of language, and additional support in identifying appropriate goals and steps for achieving goals.
Table 2.
Participant reported positive aspects and benefits of SPAN program.
| Category | Adolescent Response | Parent Response | Coach Response |
|---|---|---|---|
| Program | ● Helped Organize And Set Goals.
(3) ● Gave Adolescent A New Way Of Looking At Social Participation. ● Organized Format That Made Planning Straightforward And Manageable. ● Having Coach Help Through Each Part Of Goal Setting And Planning. |
● Helped To Organize, Set And Achieve
Goals. ● I Liked That We Could Skype Instead Of Meet Face To Face ● Loved Seeing Adolescent Set Achievable Goals, Think In New Ways And Utilize Coaching Sessions. ● Breaking Things Down And Learning Tips And Tricks For Setting Goals. ● Social Participation Step Review And Planning. ● Flexibility With Scheduling. |
● Step By Step Process Leads To Real
Outcomes. ● Working Together To Share Ideas And Build Rapport Was Beneficial. ● Limited Time Frame. ● Rewarding To Interact With Adolescent And Share Ideas On The Process Of Goal Setting, Step Formation, And Choosing Strategies.(2) ● The Coaching Manuals Included Guidelines For Planning Sessions ● Supervision Helped With Planning Future Sessions And Problem Solving Previous Sessions. |
| App | ● Good Layout For
Goals. ● Organization Break Down Each Goal Was Helpful. |
● Helped Adolescent Organize Goals In
A Cohesive Manner (2) ● Step By Step Process Is Good. ● Good Focus For Goal Setting (3) |
● Good To Have Access To Tips And
Topics Via App. ● Easy Navigation. ● Planning Wizard Displays Goals Nicely. ● Built In Information For Problem Solving And Goal Setting Was Useful. ● Being Able To View The Adolescent’s Goals And Profile. |
| Tips/Topics | ● Offered Foundation For Social Participation. (2) | N/A | ● Brief And Easily Summarizes
Ideas. ● Social Participation Tip Mostly Used. ● Liked The Organization Of The Website For Quick Referral To A Page During Sessions. ● ABCDE Problem Solving Technique Is An Easy And Useful Approach. ● Excellent Content. |
| Key Topics | ● Gave Me Specific Guidelines On How
To Socialize. ● Helped Explain Some Things About The Process. |
● Good Information | ● Social Participation Topic Mostly
Used. ● Covered A Broad Range Of Possibilities ● Provided Potential Steps And Strategies. ● Excellent Content. |
| Coaching | ● Provided Feedback On Goals And How
To Reach Them. ● Liked Not Being In The Process Alone. ● Helps Goal-Setting Process Go Smoothly. (2) ● Liked Coach’s Ideas For Goal Setting. ● Positive Relationship With Coach (2) |
● Coach Was Helpful For The Adolescent
To Communicate With And Help Generate Goals. (3) ● Coach Helped Adolescent Navigate Steps To Reaching And Setting Goals. ● Excellent Way For Adolescent To Reach Goals ● Positive Relationship With Coach (3) |
● Valuable Experience For Both
Parties. ● Liked Working And Building Rapport With Adolescent. (2) ● Skype Sessions Were Beneficial. ● Observing Adolescents Thought Process For Evaluating Goals And Action Plans. |
Note. Numbers in parentheses following comments indicate the number of respondents (if more than one) that reported the same or similar comment.
Table 3.
Critical feedback and suggestions to improve SPAN.
| Category | Adolescent response | Parent response | Coach response |
|---|---|---|---|
| Program | ● Increase trial time
(2) ● Increase and define parent involvement |
● Increase trial time
(2) ● Increase and define parent involvement |
● Increase trial time (2) |
| App | ● Need for push notifications and
reminders ● Ability to customize look and feel of app ● Streamline steps vs. strategies ● Intro or wizard to using the app when first opened ● Gaining access to the app was difficult ● Beneficial for everyone (parents) to have access to the app as well. |
● Intro to app for adolescents to
use ● Needs more prompting and reminders (3) ● Need verification of tasks completed ● Improve style and visual appeal. ● Could only access app on 1 device ● Tech issues |
● Need for push notifications and
reminders (2) ● App count days working on goal from entry date, not date of beginning work on the goal ● Planning wizard and next steps can be repetitive. |
| Tips/topics | ● Time consuming to look
over ● Color scheme issues |
● Too much reading | ● Stylization of text to be edited for
ease and of reading ● Change layout on site to be less busy |
| Key topics | ● Text-dense and
overwhelming ● Color scheme issues |
● Text-dense and
overwhelming ● Too much reading |
● Not generally used in the
trial ● Change layout on site to be less busy ● Make more interactive modules using multimedia ● Make topics more enjoyable to read (stylization and length) ● Addition of tips (memory, organization, and budgeting) that may help in social outings. |
| Coaching | ● Length of meetings should be as needed, not set time. | ● Session time seemed too long. | ● Streamline
supervision ● Identification and screening of adolescents who are self-motivated |
Note. Numbers in parentheses following comments indicate the number of respondents (if more than one) that reported the same or similar comment.
Overall, Key Topics and Brief Tips were under used. These documents were designed to provide adolescents and families with information about strategies to overcome barriers to goal achievement. While coaches valued the Key Topics and Brief Tips, parents and adolescents reported rarely using these tools because they were “not very user friendly” and suggested ways to improve how the information was presented (Table 3). Both adolescents and parents recommended a clearer definition of parental involvement in the program, and more prompts for task completion. Finally, adolescents suggested the integration of a wizard or tutorial when the app is first opened.
Adolescent, parent, and coach feedback on questionnaires was largely positive with specific suggestions for change. Parents, adolescents, and coaches reported being mostly satisfied with the overall SPAN program, as well as the coaching aspect of the program. Not all participants used the Key Topics and Brief Tips, therefore, only those who used this part of the program provided satisfaction ratings on it. Overall, both parents and coaches reported that they felt that the program was too short, while adolescents had more neutral ratings regarding program length.
Goals of adolescents
Social participation goals were selected through review of adolescent and parent baseline forms and discussion and brainstorming during coaching sessions. Table 4 presents identified goals and key steps to achieve the goals. An important aspect of the program was working with the coach to refine goals. For example, coaches prompted adolescents to think of alternative steps for achieving their goals, helped adolescents break larger goals into smaller more attainable goals, and encouraged adolescents to reach out to people in their support networks for help with goal attainment. For example, one participant initially selected a complex goal of spending more time with her family, with specific family members included as each step to achieve this goal. The participant then realized that goal achievement was not realistic within the specified time line, worked with her coach to break this complex goal into more realistic goals (e.g., selecting a smaller number of family members for one event), and prioritized steps (e.g., choosing which family members she would target first). A second participant identified a goal of taking a more active role in class activities. While his teacher was supportive of this goal, his peers were not as receptive. The participant processed his disappointment with his coach, and with the coach’s support developed a new plan to continue working toward this goal. His teacher was able to communicate the purpose of the adolescent’s new role in class, and peers were much more receptive after this discussion. In all cases, participants made progress toward their goals by completing planned steps. Two of the four participants completed all steps, achieved their goals, and identified additional goals to work after completion of the SPAN program.
Table 4.
Overview of goals adolescent worked on during SPAN.
| Goals | Steps for goal achievement |
|---|---|
| Become more social and meet new friends | (1) Talk to new people (2) Do more one-on-one work with classmates to build more intimate acquaintances. |
| Spend more time with extended family | (1) Call grandmother to schedule a visit. |
| Plan an outing with friends | (2) Start a conversation with friends to gather interest and ideas. |
| Keep up with existing friendships | (3) Text friends more often. (4) Make plans to hang out outside of school. (5) Talk to people in person more often. |
| Hang out with friends outside of school | (1) Use occasions (holidays, birthdays, etc.)
to make plans. (2) Engage in activities that keep you occupied. |
| Practice cello more regularly in a social way | (1) Talk to acquaintances (2) Talk to and practice with cello instructor (3) Discuss music interests, theory, or practice techniques with other musicians. |
| Invite a friend to go to the amusement park | (1) Decide which friend to invite. (2) Invite friend to the park. (3) Follow through with plan and go to amusement park with friend. |
Outcome data
Data are shown in Table 5. Wilcoxon signed rank tests revealed no statistically significant differences between pre- and post-intervention scores (all p’s >.05). Effect size calculations revealed an increase on the adolescent Youth Self Report measure (YSR) social competence index (d = .56) and a decrease in social problems (d = .91) and total problems (d = 1.16). There were negligible changes in the same domains on the parent-report measure (CBCL; see Table 5).
Table 5.
Mean (standard deviation) scores of parent-reported (CBCL) and adolescent-reported (YSR) behavior.
| CBCL |
Teen report /YSR |
|||||
|---|---|---|---|---|---|---|
| Pre | Post | Cohen’s d | Pre | Post | Cohen’s d | |
| Social competency | 56.00 (8.87) | 57.00 (14.70) | 0.08 | 48.25 (9.91) | 52.50 (4.12) | 0.56 |
| Social problems | 56.25 (9.32) | 58.00 (13.47) | 0.15 | 55.25 (4.65) | 52.00 (2.00) | 0.91 |
| Total problems | 47.00 (doi:10.80) | 46.50 (14.93) | 0.04 | 48.25 (5.56) | 42.75 (3.77) | 1.16 |
Note. CBCL = Child Behavior Checklist; YSR = Youth Self Report; Cohen’s d: small effect size = 0.3; medium effect size = 0.5; large effect size = 0.8
Discussion
Findings generally support the feasibility and usability of the SPAN program to promote the achievement of social participation goals in adolescents with TBI. Overall, feedback from adolescents, parents, and coaches suggested that SPAN was well received, and none of the suggested improvements challenged the main tenets or structure of the program. Although the coaching component was positively viewed and coaching sessions were seen as adding significantly to the value of the program, some aspects of the program were underused or less successful than intended, especially for adolescent with more severe impairments. Participants and coaches recommended modifications including improvement in the app functionality, clarification of the type and level of parental involvement, and improvement of the Key Topics and Brief Tips materials.
Arguably the most successful aspect of the intervention was the use of peer coaches and coaching sessions to identify social participation goals and develop action plans, with coaches potentially serving as the catalyst to promote change. This is not surprising as peers often exert greater influence on adolescent behavior, particularly social behavior, than parents and other adults,59,60 and feedback from a peer coach may be more powerful than that of a therapist who likely differs from the adolescent in a number of ways (e.g., age, interests social experiences).46,61–63
In addition to findings supporting the usability of the SPAN program and feasibility of the measures and structure of the program, ancillary findings suggested that the abbreviated program might have improved adolescents’ perceived behavioral and social functioning. Medium to large effects were noted on the adolescent self-report behavioral measures, with improvement in social competence, and decreased social problems and total problems. These findings were surprising given the brief nature of the trial and are encouraging regarding the potential benefits of the SPAN program. Findings also highlight that focusing on problem solving and goal setting in everyday settings was a potentially successful means of improving social functioning.27,30 The lack of change on parent-report behavioral measures may be a reflection of the intentionally minimal parent involvement in the study (i.e., the program aimed to foster independent social problem solving), or because participants did not share details about the sessions with their parents. Adolescents’ own perceptions of their social functioning are critical, however, so adolescent self-report measures are an important measure of outcome.
One surprising finding of the present study was the limited use of the Key Topics and Brief Tips materials. Coaches reported valuing these materials, so it is unclear what prevented them from recommending or reviewing materials with participants, or what prevented participants from using these resources. Perhaps four weeks did not allow time for participants to encounter the types of problems that would prompt use of the Key Topics. Another possibility was the lack of full integration of the Topics and Tips within the app. The Topics and Tips were accessed through a link, which was located under the “more” tab on the main menu bar, and consequently may not have been as readily accessible. Further, their didactic, rather than interactive, nature may have been unappealing to adolescents, as participants noted that Topics and Tips were text-heavy and difficult to navigate.
Based on feedback from this usability trial, we have made several modifications to the SPAN program, and these are currently being tested in a 10–week implementation pilot trial. We clarified the nature and amount of parental involvement and communication during the baseline assessment visit and in coach training, and added baseline questions for parents and adolescents about potential barriers and need for parental support (e.g., support with session scheduling or scaffolding of concepts). The study coordinator also now sends weekly updates to the parents with information about goal progress and barriers to success. Key Topics and Brief Tips materials were improved by streamlining text and removing jargon, and improving readability of the documents overall. Finally, we modified the app to improve the app experience for all users, including implementing push notification with reminders for upcoming tasks and deadlines, updating and streamlining the goal-setting wizard to provide greater scaffolding for the adolescent in developing a plan to achieve goals, and adding the ability to make due dates for tasks further out than one week. We added a help function and a walk through tutorial for each section of the app, which are accessible by clicking on a question mark on any page within the app. We also developed tutorial documents to orient users to the app and help them navigate the various functions. Finally, we hope to develop a screen sharing functionality within the app that will allow coaches and adolescents to simultaneously view app content and responses as needed.
While the findings of this current project support the usability and feasibility of the SPAN program, they should be considered in light of their limitations. First, the sample in the present project was extremely small, and while this provided valuable information regarding the usability of the app as well as the program in general, a larger pilot trial is needed to examine social participation and behavioral outcomes, as well as possible mediators and moderators of treatment effects. Further, coaches were graduate students with previous experience and knowledge of brain injury as peer coaches, while the program was designed to be used by undergraduate coaches, who have limited experience with TBI. The upcoming 10-week implementation pilot trial will utilize undergraduate students as coaches, and it will be important to examine whether outcomes satisfaction with the coaching portion of the program continue to be as positive. Finally, future studies need to examine how adolescents with a range of injury severity and functional impairments respond to the intervention. While our small sample did have a range of injury severity, most participants have had a positive recovery with few lasting impairments. One participant continued to experience significant impairments, and struggled more with the intervention than the others enrolled in the project.
Overall, findings from the present study were positive and support usability and acceptability of an app/web-based program with peer coaching to support social participation. Feedback regarding specific aspects of the app was used to modify materials prior to completion of a larger implementation trial. The SPAN program has the potential to improve social involvement of adolescents with a history of TBI through an innovative use of technology and peer coaching. In addition to potentially improving the functioning of adolescents with a history of TBI, training of undergraduate college student coaches can provide an opportunity to build an understanding of TBI in the broader community and encourage them to consider careers working with individuals with TBI or other neurological conditions.64–66
Acknowledgments
The authors would like to thank our participants and coaches for their time and important feedback. We also thank Michele Jacquin, graduate student at Tufts University Department of Occupational Therapy, who assisted with data collection and analysis.
Funding
This research was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) Grant # H133G130272. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS) in the USA. The contents of this manuscript were developed under a grant from the The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should assume endorsement by the Federal Government.
Footnotes
Color versions of one or more of the figures in this article can be found online at http://www.tandfonline.com/ipdr.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Yeates KO, Bigler ED, Dennis M, et al. Social outcomes in childhood brain disorder: a heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin. 2007;133(3):535–556. doi: 10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society: JINS. 2004;10(3):412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt AT, Hanten GR, Li X, et al. Emotion recognition following pediatric traumatic brain injury: longitudinal analysis of emotional prosody and facial emotion recognition. Neuropsychologia. 2010;48(10):2869–2877. doi: 10.1016/j.neuropsychologia.2010.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tonks J, Williams WH, Frampton I, et al. Reading emotions after child brain injury: a comparison between children with brain injury and non-injured controls. Brain Injury. 2007;21(7):731–739. doi: 10.1080/02699050701426899. [DOI] [PubMed] [Google Scholar]
- 5.Turkstra LS, McDonald S, DePompei R. Social information processing in adolescents: data from normally developing adolescents and preliminary data from their peers with traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2001;16(5):469–483. doi: 10.1097/00001199-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Turkstra LS, Dixon TM, Baker KK. Theory of Mind and social beliefs in adolescents with traumatic brain injury. NeuroRehabilitation. 2004;19(3):245–256. [PubMed] [Google Scholar]
- 7.Stronach ST, Turkstra LS. Theory of mind and social beliefs in adolescents with traumatic brain injury. Aphasiology. 2004;22:1054–1070. doi: 10.1080/02687030701632187. [DOI] [PubMed] [Google Scholar]
- 8.Dennis M, Simic N, Agostino A, et al. Irony and empathy in children with traumatic brain injury. Journal of the International Neuropsychological Society: JINS. 2013;19(3):338–348. doi: 10.1017/S1355617712001440. [DOI] [PubMed] [Google Scholar]
- 9.Hanten G, Cook L, Orsten K, et al. Effects of traumatic brain injury on a virtual reality social problem solving task and relations to cortical thickness in adolescence. Neuropsychologia. 2011;49(3):486–497. doi: 10.1016/j.neuropsychologia.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bedell GM, Cohn ES, Dumas HM. Exploring parents’ use of strategies to promote social participation of school-age children with acquired brain injuries. The American Journal of Occupational Therapy. 2005;59(3):273–284. doi: 10.5014/ajot.59.3.273. [DOI] [PubMed] [Google Scholar]
- 11.Bedell GM, Dumas HM. Social participation of children and youth with acquired brain injuries discharged from inpatient rehabilitation: a follow-up study. Brain Injury. 2004;18(1):65–82. doi: 10.1080/0269905031000110517. [DOI] [PubMed] [Google Scholar]
- 12.Gauvin-Lepage J, Lefebvre H. Social inclusion of person with moderate head injuries: the points of view of adolescents with brain injuries, their parents and professionals. Brain Injury. 2010;24(9):1087–1097. doi: 10.3109/02699052.2010.494593. [DOI] [PubMed] [Google Scholar]
- 13.Law M, Anaby D, DeMatteo C, et al. Participation patterns of children with acquired brain injury. Brain Injury. 2011;25(6):587–595. doi: 10.3109/02699052.2011.572945. [DOI] [PubMed] [Google Scholar]
- 14.Mealings M, Douglas J. School’s a big part of your life: adolescent perspectives of their school participation following traumatic brain injury brain impairment. Brain Impairment. 2010;11:1–16. [Google Scholar]
- 15.Prigatano GP, Gray JA. Parental concerns and distress after paediatric traumatic brain injury: a qualitative study. Brain Injury: [BI] 2007;21(7):721–729. doi: 10.1080/02699050701481605. [DOI] [PubMed] [Google Scholar]
- 16.Sharp NL, Bye RA, Llewellyn GM, et al. Fitting back in: adolescents returning to school after severe acquired brain injury. Disability and Rehabilitation. 2006;28(12):767–778. doi: 10.1080/09638280500386668. [DOI] [PubMed] [Google Scholar]
- 17.Van Tol E, Gorter JW, Dematteo CA, et al. Participation outcomes for children with acquired brain injury: a narrative review. Brain Injury: [BI] 2011;25(13–14):1279–1287. doi: 10.3109/02699052.2011.613089. [DOI] [PubMed] [Google Scholar]
- 18.Stancin T, Drotar D, Taylor HG, et al. Health-related quality of life of children and adolescents after traumatic brain injury. Pediatrics. 2002;109(2):E34. doi: 10.1542/peds.109.2.e34. [DOI] [PubMed] [Google Scholar]
- 19.Prigatano GP, Gupta S. Friends after traumatic brain injury in children. The Journal of Head Trauma Rehabilitation. 2006;21(6):505–513. doi: 10.1097/00001199-200611000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Rosema S, Crowe L, Anderson V. Social function in children and adolescents after traumatic brain injury: a systematic review 1989–2011. Journal of Neurotrauma. 2012;29(7):1277–1291. doi: 10.1089/neu.2011.2144. [DOI] [PubMed] [Google Scholar]
- 21.Turkstra LS, Politis AM, Forsyth R. Cognitive-communication disorders in children with traumatic brain injury. Developmental Medicine & Child Neurology. 2015;57(3):217–222. doi: 10.1111/dmcn.12600. [DOI] [PubMed] [Google Scholar]
- 22.Ryan NP, Catroppa C, Beare R, et al. Predictors of longitudinal outcome and recovery of pragmatic language and its relation to externalizing behavior after pediatric traumatic brain injury. Brain and Language. 2015;142:86–95. doi: 10.1016/j.bandl.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Ryan NP, Anderson V, Godfrey C, et al. Predictors of very-long-term sociocognitive function after pediatric traumatic brain injury: evidence for the vulnerability of the immature “social brain”. Journal of Neurotrauma. 2014;31(7):649–657. doi: 10.1089/neu.2013.3153. [DOI] [PubMed] [Google Scholar]
- 24.Bedell G, Haley S, Coster WJ, et al. Participation readiness at discharge from inpatient rehabilitation in children and adolescents with acquired brain injuries. Pediatric Rehabilitation. 2002;5(2):107–116. doi: 10.1080/1363849021000013540. [DOI] [PubMed] [Google Scholar]
- 25.Eccles JS, Barber BL, Stone M, et al. Extracurricular Activities and Adolescent Development. Journal of Social Issues. 2003;59(4):865–889. doi: 10.1046/j.0022-4537.2003.00095.x. [DOI] [Google Scholar]
- 26.Larson RW, Verma S. How children and adolescents spend time across the world: work, play, and developmental opportunities. Psychological Bulletin. 1999;125(6):701–736. doi: 10.1037/0033-2909.125.6.701. [DOI] [PubMed] [Google Scholar]
- 27.Mahoney JL, Cairns BD, Farmer TW. Promoting interpersonal competence and educational success through extracurricular activity participation. Journal of Educational Psychology. 2003;95(2):409–418. doi: 10.1037/0022-0663.95.2.409. [DOI] [Google Scholar]
- 28.Rutter M. Psychosocial resilience and protective mechanisms. The American Journal of Orthopsychiatry. 1987;57(3):316–31. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 29.Hofgren C, Esbjornsson E, Sunnerhagen KS. Return to work after acquired brain injury: facilitators and hindrances observed in a sub-acute rehabilitation setting. Work. 2010;36(4):431–439. doi: 10.3233/WOR-2010-1039. [DOI] [PubMed] [Google Scholar]
- 30.Sale P, West M, Sherron P, et al. Exploratory analysis of job separations from supported employent for person with traumatic brain injury. Journal of Head Trauma Rehabilitation. 1991;6:1–11. doi: 10.1097/00001199-199109000-00004. [DOI] [Google Scholar]
- 31.Wehman P, Kregel J, Sherron P, et al. Critical factors associated with the successful supported employment placement of patients with severe traumatic brain injury. Brain Injury: [BI] 1993;7(1):31–44. doi: 10.3109/02699059309008154. [DOI] [PubMed] [Google Scholar]
- 32.Winkler D, Unsworth C, Sloan S. Factors that lead to successful community integration following severe traumatic brain injury. Journal of Head Trauma Rehabilitation. 2006;21(1):8–21. doi: 10.1097/00001199-200601000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Agnihotri S, Lynn Keightley M, Colantonio A, et al. Community integration interventions for youth with acquired brain injuries: A review. Developmental Neurorehabilitation. 2010;13(5):369–382. doi: 10.3109/17518423.2010.499409. [DOI] [PubMed] [Google Scholar]
- 34.Gresham FM, Sugai G, Horner RH. Interpreting outcomes of social skills training for students with high-incidence disabilities. Exceptional Children. 2001;67(3):331–344. doi: 10.1177/001440290106700303. [DOI] [Google Scholar]
- 35.Cooley E, Glang A, Voss J. Making connections: helping children with acquired brain injury build freiendships. In: Glang A, Singer GHS, Todis B, editors. Acquired Brain Injury: The School’s Response. Baltimore, MD: Paul H. Brookes; 1997. [Google Scholar]
- 36.Glang A, Todis B, Cooley E, et al. Building social networks for children and adolescents with traumatic brain injury: A school-based intervention. Journal of Head Trauma Rehabilitation. 1997;12(2):32–47. doi: 10.1097/00001199-199704000-00005. [DOI] [Google Scholar]
- 37.Laugeson EA. The PEERS® curriculum for school based professionals: social skills training for adolescents with autism spectrum disorder. New York, NY: Routledge; 2013. [Google Scholar]
- 38.Ylvisaker M, Adelson PD, Braga LW, et al. Rehabilitation and ongoing support after pediatric TBI: twenty years of progress. Journal of Head Trauma Rehabilitation. 2005;20(1):95–109. doi: 10.1097/00001199-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Janusz JA, Kirkwood MW, Yeates KO, et al. Social problem-solving skills in children with traumatic brain injury: long-term outcomes and prediction of social competence. Child Neuropsychology. 2002;8(3):179–194. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- 40.Wade SL, Taylor HG, Drotar D, et al. Parent-adolescent interactions after traumatic brain injury - Their relationship to family adaptation and adolescent adjustment. Journal of Head Trauma Rehabilitation. 2003;18(2):164–176. doi: 10.1097/00001199-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Taylor HG, Yeates KO, Wade SL, et al. Bidirectional child-family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society: JINS. 2001;7(6):755–767. doi: 10.1017/S1355617701766118. [DOI] [PubMed] [Google Scholar]
- 42.Dennis JM, Phinney JS, Chuateco LI. The role of motivation, parental support, and peer support in the academic success of ethnic minority first-generation college students. Journal of College Student Development. 2005;46(3):223–236. doi: 10.1353/csd.2005.0023. [DOI] [Google Scholar]
- 43.Carter EW, Kennedy CH. Promoting access to the general curriculum using peer support strategies. Research Practice Persons with Severe Disabilities. 2006;31(4):284–292. doi: 10.1177/154079690603100402. [DOI] [Google Scholar]
- 44.Joseph DH, Griffin M, Hall RF, et al. Peer coaching: an intervention for individuals struggling with diabetes. The Diabetes Educator. 2001;27(5):703–710. doi: 10.1177/014572170102700511. [DOI] [PubMed] [Google Scholar]
- 45.Braga LW, Rossi L, Moretto ALL, et al. Empowering preadolescents with ABI through metacognition: preliminary results of a randomized clinical trial. NeuroRehabilitation. 2012;30(3):205–212. doi: 10.3233/NRE-2012-0746. [DOI] [PubMed] [Google Scholar]
- 46.Turkstra L, Burgess S. Social skills intervention for adolescents with TBI. Neurophysiology and Neurogenic Speech and Language Disorders. 2007;17:15–19. doi: 10.1044/nnsld17.3.15. [DOI] [Google Scholar]
- 47.Wiseman-Hakes C, Stewart ML, Wassertnan R, et al. Peer group training of pragmatic skills in adolescents with acquired brain injury. The Journal of Head Trauma Rehabilitation. 1998;13(6):23–38. doi: 10.1097/00001199-199812000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following pediatric brain injury. Journal of Consulting and Clinical Psychology. 2006;74(3):445–454. doi: 10.1037/0022-006X.74.3.445. [DOI] [PubMed] [Google Scholar]
- 49.Lenhart A. Teen, social media and technology overview. 2015 Available from: http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/
- 50.Lenhart A, Smith A, Anderson M, et al. Teens, technology and friendships. Available from: http://www.pewinternet.org/2015/8/06/teens-technology-and-friendships/
- 51.Selman RL, Schultz LH. Making a friend in youth. Chicago, IL: University of Chicago Press; 1990. [Google Scholar]
- 52.Selman RL, Watts CL, Schultz LH. Fostering friendship: pair therapy for treatment and prevention. New York, NY: Aldine de Gruyter; 1997. [Google Scholar]
- 53.Bedell G, Wade S, Turkstra L, et al. Informing design of an app-based coaching intervention to promote social participation of teenagers with traumatic brain injury. Developmental Neurorehabilitation. 2016 doi: 10.1080/17518423.2016.1237584. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 54.Haarbauer-Krupa J, Meulenbroek P, Gibbs J, et al. The BRAIN program: A model for transition to adult lives for teens with acquired brain injury. The Journal of Head Trauma Rehabilitation. 2010;25:396–397. [Google Scholar]
- 55.Wade SL, Stancin T, Kirkwood M, et al. Counselor-assisted problem solving (CAPS) improves behavioral outcomes in older adolescents with complicated mild to severe TBI. The Journal of Head Trauma Rehabilitation. 2014;29(3):198–207. doi: 10.1097/HTR.0b013e31828f9fe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Head strong for life. 2014 Available from: http://www.headstrongforlife.org.
- 57.Achenbach TM. Manual for the self-report for ages 11–18. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 58.McCauley SR, Wilde EA, Anderson VA, et al. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. Journal of Neurotrauma. 2012;29(4):678–705. doi: 10.1089/neu.2011.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berndt TJ. Developmental changes in conformity to peers and parents. Developmental Psychology. 1979;15(6):608–616. doi: 10.1037/0012-1649.15.6.608. [DOI] [Google Scholar]
- 60.Chein J, Albert D, O’Brien L, et al. Peers increase adolescent risk taking by enhancing activity in the brain’s reward circuitry. Developmental Science. 2011;14(2):F1–F10. doi: 10.1111/j.1467-7687.20. doi:10.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hibbard MR, Cantor J, Charatz H, et al. Peer support in the community: initial findings of a mentoring program for individuals with traumatic brain injury and their families. The Journal of Head Trauma Rehabilitation. 2002;17(2):112–131. doi: 10.1097/00001199-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 62.Kolakowsky-Hayner SA, Wright J, Shem K, et al. An effective community-based mentoring program for return to work and school after brain and spinal cord injury. NeuroRehabilitation. 2012;31(1):63–73. doi: 10.3233/NRE-2012-0775. [DOI] [PubMed] [Google Scholar]
- 63.Struchen MA, Davis LC, Bogaards JA, et al. Making connections after brain injury: development and evaluation of a social peer-mentoring program for persons with traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2011;26(1):4–19. doi: 10.1097/HTR.0b013e3182048e98. [DOI] [PubMed] [Google Scholar]
- 64.Duckenfield M, Madden SJ. An orientation to service learning. In: Madden SJ, editor. Service Learning Across the Curriculum: Case Applications in Higher Education. New York, NY: University Press of America; 2000. pp. 1–8. [Google Scholar]
- 65.Jacoby B. Service learning in today’s higher education. In: Jacoby B, editor. Service Learning in Higher Education. San Francisco, CA: Jossey-Cass; 1996. pp. 3–25. [Google Scholar]
- 66.Taylor TP, Pancer SM. Community service experiences and commitment to volunteering. Journal of Applied Social Psychology. 2007;37:320–345. doi: 10.1111/jasp.2007.37.issue-2. [DOI] [Google Scholar]


