Abstract
Recent studies describe the clinical implications of sickle cell disease (SCD) stigma. However, little is known about its link to depressive symptoms or its relative influence on the association between depressive symptoms and SCD pain. We examined whether internalized stigma about SCD moderated the relation between depressive symptoms and pain among 69 adults attending a SCD clinic who reported pain episodes and healthcare use over the past three months. Unadjusted bivariate analyses showed a marginal association between depressive symptoms and SCD pain frequency (r = .21, p < .10). Further analyses adjusting for health care use indicated a moderating effect of internalized stigma (b = −.10, p < .05): a significant association between depressive symptoms and pain was observed among participants low in internalized stigma, but this relationship was attenuated at moderate and high stigma levels. These results denote counterintuitive consequences of internalized attitudes about SCD and suggest a need for further study of the psychosocial and clinical implications of SCD stigma.
Keywords: sickle cell disease, stigma, pain, depressive symptoms
Sickle cell disease (SCD) is a genetic blood disorder that affects more than 100,000 people in the United States. SCD occurs when an anomalous form of hemoglobin (an oxygen-transporting protein) causes red blood cells to assume a sickle shape (Ballas, Gupta, & Adams-Graves, 2012). Sickled cells obstruct the blood vessels and inhibit the flow of oxygen and vital nutrients throughout the body, affecting multiple organ systems and contributing to increased risk of infection and a host of other health problems (Ballas et al., 2012; Darbari et al., 2008). The most commonly investigated characteristic of SCD, however, is severe and unpredictable episodes of acute pain that often lead to high rates of health care utilization and hospital admissions. The repeated experience of acute SCD pain episodes (and their affiliated hospitalizations) is not only associated with premature mortality (Darbari, Ballas, & Clauw, 2014; Darbari et al., 2013), but also exerts significant financial, emotional, and psychological tolls (Woods & Karrison, 1997; Yang, Shah, Watson, & Mankad, 1995).
Over the past three decades, cross-sectional and prospective studies overwhelmingly suggest that depression and its concomitant symptoms are associated with several aspects of the SCD experience, including pain (Alao & Cooley, 2001; Asnani, Fraser, Lewis, & Reid, 2010; Laurence, George, & Woods, 2006; Levenson et al., 2008; Schaeffer et al., 1999), disease severity (Laurence et al., 2006; Sogutlu, Levenson, McClish, Rosef, & Smith, 2011) and health care utilization (Grant, Gil, Floyd, & Abrams, 2000). Such findings have led some researchers to consider the amelioration of depressive symptoms as an essential component in the treatment of SCD (Hasan, Hashmi, Alhassen, Lawson, & Castro, 2003). Yet, most efforts to understand the association between depressive symptoms and SCD pain tend to overlook the contribution of relevant psychosocial variables that could potentially impact the association (Bediako, 2009; Caird, Camic, & Thomas, 2011; Edwards et al., 2005).
Stigma – the social devaluation that a person experiences or anticipates from others – is an important factor that might influence both depressive symptoms and health related outcomes (Earnshaw & Quinn, 2012). Several studies have shown that the combination of stigma and depressive symptoms has a deleterious impact on health and well being: that is, people who experience high levels of both depression and stigma tend to use fewer health services and are less likely to adhere to medication regimens (Cooper, Corrigan, & Watson, 2003; Corrigan, Druss, & Perlick, 2014; Henderson, Evans-Lacko, & Thornicroft, 2013), thereby facilitating an adverse cycle of depression, stigma, and worse outcomes.
Stigma is highly pertinent to the experience of SCD patients, as many individuals encounter extraordinary social challenges in living with and managing the disease. Difficulties in obtaining adequate comprehensive care, problems associated with negative encounters with medical staff, and dealing with persistent stereotypes of being malingerers or “drug seekers” are well documented aspects of the SCD experience (Derlega, Maduro, Janda, Chen, and Goodman, in press; Harris, Barker, & Parker, 1998; Haywood et al., 2014; Lattimer et al., 2010). The overall theme of these experiences highlights the importance of focusing on social interactions that occur within the SCD milieu. Positive social interactions might be threatened when discordant perceptions about SCD (or its treatment) exist between patients and close significant others, the general public, or health care professionals. Indeed, a recent mixed methods investigation (Ola, Yates, & Dyson, 2016) pointed to the importance of the social environment as a unique and significant predictor of depressive symptoms among adults living with SCD. Ola et al. (2016) suggested that more studies on the global impact of social factors on SCD outcomes are needed. However, relatively little empirical evidence exists about stigma in the specific context of SCD-related pain, despite findings that indicate a robust association between stigma and chronic pain in general (Cohen, Quintner, Buchanan, Nielsen, & Guy, 2011; Holloway, Sofaer-Bennett, & Walker, 2007; Monsivais, 2013; Slade, Molloy, & Keating, 2009; Waugh, Byrne, & Nicholas, 2014).
Jenerette and colleagues were perhaps the first to propose direct links among depression, stigma, and SCD outcomes (Jenerette, Funk, & Murdaugh, 2005). However, their original study did not include a direct assessment of stigma. Over the past decade, instruments developed specifically for persons living with SCD indicate that stigma is a multidimensional construct that is also associated with a range of psychological and clinical outcomes (Bediako et al., 2016; Jenerette, Brewer, Crandell, & Ataga, 2012). For example, Jenerette et al. (2012) developed and administered the Sickle Cell Disease Health-Related Stigma Scale (SCD-HRSS) to a sample of 77 adults living in North Carolina and noted a positive association between stigma and depressive symptoms. Further, to support the idea of interrelationships among stigma, pain, and depression, Jenerette and colleagues found that participants who had more than three pain episodes that required hospitalizations during the past year reported greater stigma and more depressive symptoms than those who had fewer than three episodes (Jenerette et al., 2012). In another study, Bediako et al. (2016) administered the Measure of Sickle Cell Stigma (MoSCS) to 262 adults in the Baltimore/Washington, DC region and reported that SCD stigma was comprised of four factors: Internalized Stigma (negative personal feelings or guilt about having SCD); Social Exclusion (the extent to which individuals experience social/interpersonal rejection because of their SCD status); Disclosure Concerns (apprehension in disclosing one's SCD status to others); and Expected Discrimination (the anticipation that one will be negatively stereotyped or discriminated against because of their SCD status). All of the stigma factors except Disclosure Concerns were associated with perceived disease severity and health care utilization for acute SCD pain (Bediako et al., 2016).
Both sets of studies have important limitations. For example, a critique of the SCD-HRSS offered by Bediako and colleagues (2016) is that it appears to focus primarily on public stigma (e.g., interpersonal perceptions of being stigmatized by others) rather than self-stigma (e.g., internalized perceptions that reflect one's attitudes about self-worth). Research has suggested that self/internalized stigma is negatively associated with health status disclosure (Drapalski et al., 2013; Tsai et al., 2013), self-esteem and self-efficacy (Overstreet, Earnshaw, Kalichman, & Quinn, 2013), and specific health behaviors (Vartanian & Novak, 2011). Because of our primary interest in evaluating intrapersonal aspects of the SCD experience, we made internalized stigma the focal point of the present study. Second, a major shortcoming of the MoSCS scale is that its association with traditional psychosocial measures – such as depressive symptoms – is not known. Thus, definitive statements about relationships between psychosocial variables and specific aspects of stigma cannot be offered until this gap is filled. Finally, a shared limitation of both studies is the researchers’ use of health care utilization for SCD pain as a primary outcome variable, rather than the individual's direct report of pain. Findings from the landmark study of SCD pain epidemiology (Smith et al., 2008) suggest that adults experience pain much more frequently than is commonly thought and that a sole focus on health care use underestimates an accurate appraisal of the experience of SCD pain. In addition to assessing participants’ health care utilization, sound studies should also collect data about the frequency of SCD pain episodes directly from participants.
The current study seeks to address these limitations of previous research on SCD-related stigma in three important ways. First, it explicitly investigates the internalized stigma construct. Second, it incorporates a validated measure of depressive symptoms that is appropriate for chronic pain populations. Finally, it obtains a direct index of SCD pain frequency via patient report. By addressing these limitations, this is perhaps the first study to simultaneously evaluate relationships among stigma, depressive symptoms, and patient-reported pain in SCD. Based on the manner in which these variables have been conceptualized in the research literature, we expect to observe positive associations among them, such that greater stigma should be associated with greater depressive symptoms and both should be positively associated with greater SCD pain frequency as reported by patients. In addition – as an exploratory aim – we also investigate whether internalized stigma about SCD moderates the association between depressive symptoms and pain frequency reports.
Methods
Participants
Participants were 71 adults who were at least 21 years of age and seen at a university-affiliated hematology clinic in the Midwestern United States. Eligible participants were diagnosed with one of the major types of SCD hemoglobinopathy (e.g., SS, SC, or Sβ thalassemia + or 0) and able to speak or read English. Two participants did not complete measures of depressive symptoms or stigma (described below) and were excluded from subsequent analyses. Thus, the final sample included complete data from 35 women and 34 men (mean age = 35.4 years; SD = 12.5 years).
Design and Procedures
The study was designed as a cross-sectional, within-group investigation. Participants completed a survey that assessed demographic variables, pain, stigma, and psychosocial functioning. All surveys were completed in the waiting area or in a private consultation room of the clinic. After returning completed surveys to the research staff, participants were given a $10 gift card to a local grocery. Informed consent was obtained according to procedures approved by the university's institutional review board.
Measures
Pain Frequency
A single self-reported item assessed the primary outcome variable, pain frequency. Participants noted the number of distinct sickle cell pain episodes they experienced over the last three months. Past research indicates that SCD patients are quite accurate in recalling pain episodes over this length of time and has shown that this method corroborates highly with data from medical chart reviews (Bediako & Neblett, 2011; Edwards, Telfair, Cecil, & Lenoci, 2001).
Depressive Symptoms
Depressive symptoms were measured with 6-items taken from the Brief Symptom Inventory (BSI; Derogatis & Spencer, 1993). Participants reported the extent to which they experienced certain problems over the past 3 months (e.g., “feeling hopeless about the future”; “feeling no interest in things”), using a scale ranging from 0 (not at all) to 4 (extremely). In the present study, the items were summed and averaged such that higher scores were an index of greater psychological symptoms. The alpha coefficient for the 6 items used in this study was .86.
Internalized Stigma
Internalized stigma was assessed with a subscale from the Measure of Sickle Cell Stigma (MoSCS), an 11-item instrument that measures disease-specific stigma (Bediako et al., 2016). Participants indicated their level of agreement with three items that assess negative feelings or guilt about having SCD (e.g., “I feel that I'm not as good as others because I have sickle cell disease”; “I feel guilty because I have sickle cell disease”; “Having sickle cell disease makes me feel that I am a bad person”). Responses ranged from 1 (completely false) to 6 (completely true) and higher scores indicated greater levels of stigma. Bediako and colleagues (2016) reported Cronbach alpha coefficients for the Internalized Stigma subscale as .78 and .84 in two samples of adults living with SCD in the Midwestern and Mid-Atlantic United States, respectively. In the present study, Cronbach's alpha for the Internalized Stigma measure was .82.
Health Care Utilization
We asked participants to specify their visits to health care providers for sickle cell-related events. We operationalized health care utilization as the total number of visits to a hospital, clinic, or emergency department setting over the past three months. Prior research also indicates that adults living with SCD have a high degree of accuracy in recalling their health care use over this time period and our approach in assessing health care use is similar to that of other studies (Haywood et al., 2014; McCrae & Lumley, 1998).
Results
We examined the primary study variables for data-recording accuracy, missing values, and violations of normality, linearity, and homoscedasticity. All values for the variables were within plausible value ranges. We identified three outliers for the pain frequency variable and also noted that scores on this variable were positively skewed (value = 2.24, SE = .29) and kurtotic (value = 6.20, SE = .56). After conducting a log-10 transformation of the pain frequency scores, skewness and kurtosis values were within acceptable ranges at .08 and −.37, respectively. Consequently, we report all bivariate and multivariate analyses of the pain frequency variable with the log-transformed values. One case was identified as an outlier, but was retained in the dataset because: (a) the standardized score did not exceed 3 standard deviations from the log-transformed mean; and (b) excluding this case did not alter the results of the study.
Overall, the sample reported a median of 3.0 pain episodes over the past three months (range 0-20). Participants also reported relatively low levels of both depressive symptoms (M = 1.10, SD = .90; range 0-3) and internalized stigma (M = 1.59, SD = .98, range 1-6). As expected, health care utilization was positively associated with SCD pain frequency (r = .52, p < .001), indicating that health care use increased as participants reported more frequent pain episodes. Depressive symptoms were marginally associated in bivariate analyses with SCD pain frequency (r = .21, p < .10) and with health care utilization (r = .21, p < .10), demonstrating a trend for greater depressive symptoms to be related to more frequent reports of pain and increased health care use. Internalized stigma was associated with neither SCD pain frequency (r = −.11, p = .36) nor health care utilization (r = −.05, p = .71). Depressive symptoms and internalized stigma, however, were positively related (r = .35, p < .005) – suggesting that endorsement of more depressive symptoms was associated with higher levels of internalized SCD stigma.
We explored whether internalized stigma moderated the association between depressive symptoms and SCD pain frequency by utilizing the PROCESS macro in SPSS 23.0 (Field, 2013; Hayes, 2013). Our analysis consisted of a forced entry regression in which SCD pain episodes over the past three months (adjusted for health care utilization) were the primary outcome variable. We calculated mean-centered values of the predictor (depressive symptoms) and the moderator (internalized stigma), and also included an internalized stigma by depressive symptom interaction term in order to evaluate the combined effects of both variables in the model. Analyses were evaluated across 5,000 bootstrapped samples.
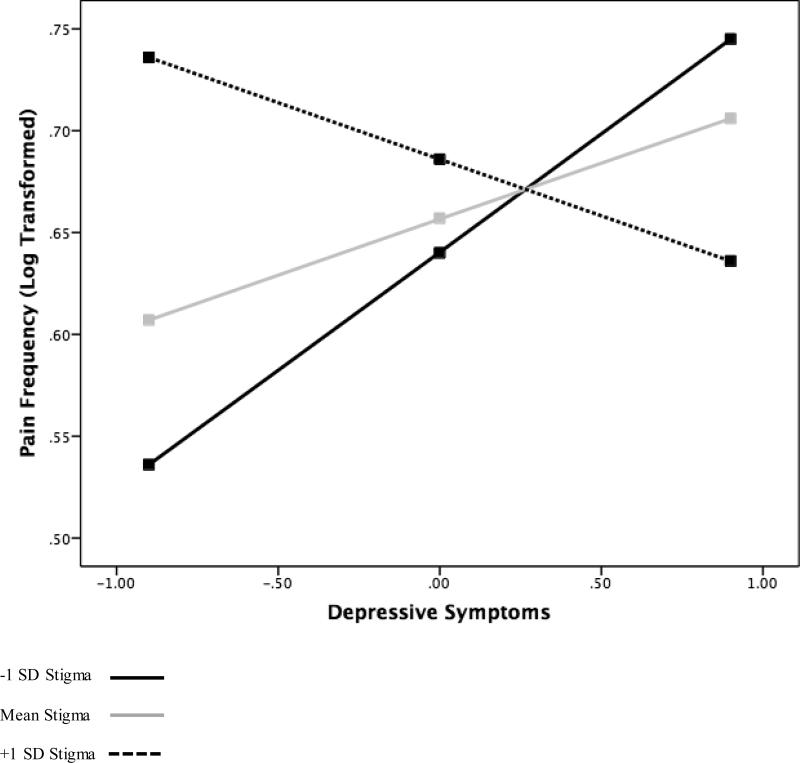
A summary of this analysis is shown in Table 1. The model accounted for 35.4% of the variance in SCD pain episode frequency. After adjusting for internalized stigma, the internalized stigma/depressive symptoms interaction, and health care utilization, depressive symptoms were not associated with pain episode frequency (b = .06, p = .25). Similarly, internalized stigma was not associated with pain episode frequency (b = .03, p = .51) after adjusting for depressive symptoms, the internalized stigma/depressive symptoms interaction, and health care utilization. The interaction term, however, was statistically significant (b = −.10, p < .05), indicating that the effect of depressive symptoms on SCD pain episode frequency was linearly dependent upon internalized stigma. We inspected the conditional effects of depressive symptoms on pain episode frequency at three distinct values of internalized stigma: the mean and +/− 1 standard deviation units from the mean. The results, shown in Figure 1, indicate that at low levels of internalized stigma, the association between depressive symptoms and pain episode frequency is positive and statistically significant (b = .12, p < .05). At mean and high levels of internalized stigma, the relative strength of the association between depressive symptoms and pain episode frequency were similar (absolute values of the coefficients were approximately .06). However, neither effect was statistically significant (p values > .20). Interestingly, at high levels of internalized stigma, the relation between depressive symptoms and pain episode frequency was negative. This pattern of results suggests that internalized stigma moderates the relation between depressive symptoms and pain episode frequency in SCD, such that the association is only significant at lower levels of internalized stigma. At mean and higher levels of stigma, there is no statistically significant linear association between depressive symptoms and SCD pain.
Table 1.
Linear model of predictors of SCD pain frequencya
| b | SE B | t | p | |
|---|---|---|---|---|
| Constant | 5.33 | .714 | 7.741 | .000 |
| Depressive Symptoms (centered) | 2.06 | .917 | 2.243 | .028 |
| Internalized Stigma (centered) | −.27 | .598 | −.447 | .657 |
| Depressive Symptoms * Internalized Stigma | −1.16 | .537 | −2.153 | .035 |
R2 = .148
Figure 1.
Simple slopes equations of the regression of SCD pain frequency on depressive symptoms at three levels of internalized stigma
Discussion
The experience of SCD pain takes place in a broad psychological and social context. However, few studies have viewed the link between depressive symptoms and SCD pain through a psychosocial lens. The present study examined associations among internalized stigma, depressive symptoms, and SCD pain. It also evaluated whether internalized stigma moderated the relationship between depressive symptoms and pain frequency in a sample of 69 adults living with SCD. Bivariate analyses indicated mixed findings; there was a marginally positive association between depressive symptoms and SCD pain frequency, a positive association between depressive symptoms and internalized stigma, and no association between internalized stigma and SCD pain frequency. Finally, results of a statistical test for moderation showed that internalized stigma moderated the association between depressive symptoms and SCD pain frequency such that a positive relationship was observed between the two variables – but only at low levels of stigma.
Although these results focus on SCD pain frequency as the primary outcome, they appear to be consistent with Jonassaint and colleagues’ systematic review of 12 studies that found only a modest association between depression and health care utilization in SCD (Jonassaint, Jones, Leong, & Frierson, 2016). Common thinking about relationships among stigma, depressive symptoms, and pain might suggest that SCD-related stigma would exacerbate the depressive symptom-pain link; yet, our findings diverge from this line of thinking and appear to indicate that moderate and high levels of stigma interfere with or disrupt the typical psychosocial processes that occur in a chronic illness context. Findings from a recent study by Watson & Angell (2013) might provide a possible explanation for our results. Watson & Angell (2013) suggested that stigma is not only indicative of identification with a marginalized group, but also of disidentification with a dominant majority. Regardless of whether individuals embrace negative stereotypes about their stigmatized group, their knowledge that such stereotypes exist may lead them to expect unfair treatment from the dominant majority. In the case of individuals living with a chronic illness, this presents a particular challenge in that patients are faced with an additional psychological burden of reconciling the fact that they must seek health care services from a “system” that they expect to treat them unfairly. The weight of reconciling this burden may be more pronounced for individuals who report higher stigma. Theories of social cognition suggest that the more uncomfortable people feel when they experience dissonant thoughts or discordant perceptions, the more motivated they are to reduce the discomfort (Fiske, 2004; Gilovich, Keltner, Chen, & Nisbett, 2016). Collectively, this suggests that individuals who feel completely excluded from the majority (i.e., those who report greater internalized stigma) may also experience greater psychological tension than their counterparts who report less internalized stigma. Subsequently, the use of other psychological and behavioral responses (e.g., increased anxiety or mistrust) might interfere with or obfuscate the association between depressive symptoms and pain – therefore explaining why the relationship between depressive symptoms and SCD pain is relatively weaker among those who report higher levels of internalized stigma.
To illustrate this point, consider that in the United States, SCD patients often constitute a marginalized group (Bediako & Haywood, 2009; Bediako & Moffitt, 2011; Haywood et al., 2014). Individual differences in the availability of health care resources, access to quality comprehensive care, and the quality of relationships with health care providers suggest that there should be considerable variability in the extent to which patients expect inequitable treatment. However, when there is a need to seek health care services (for an acute pain episode, for example), those who have greater internalized stigma about SCD may experience an additional psychological burden related to a belief that they do not deserve or cannot obtain access to services that will facilitate pain relief. Thus, people with high levels of internalized stigma may under-report, ignore, or minimize their pain in order to shorten or defer potentially anxiety-arousing interactions with those in the health care system who might treat them unfairly. In contrast, people with low levels of internalized SCD stigma may not have such experiences; therefore, the depressive symptom/pain link appears “normal” for individuals who report lower levels of stigma. Patients with moderate and high levels of internalized stigma may implicitly or intentionally deny physical pain as a mechanism to protect themselves from the psychological or emotional pain of further social devaluation. While our interpretations of these findings are speculative, future theory-driven research that provides a greater in-depth description of adult experiences with health care is a potentially promising area for further psychosocial research (Haywood et al., 2013).
There are a few limitations to note about the study. First, because our study was conducted with adult patients who were seen in a single clinic, it is unclear whether these results generalize to the broader population of adults living with SCD. It is important for future research to utilize a larger sample from diverse community settings in order to enhance the generalizability of the findings, especially given the relatively low rates of pain and health care use reported by this sample. Second, we relied on a self-reported measure of SCD pain frequency. While using medical records would have provided a more objective assessment, such records are inherently biased because they only capture “official” contacts with the traditional health care system. As stated earlier, Smith et al. (2008) clearly showed in their careful study of the epidemiology of SCD pain that most episodes are experienced at home. Therefore, the participant's self-reported frequency of SCD pain episodes is perhaps the most valid and accurate assessment. Third, we also acknowledge a relatively low rate of depressive symptoms among our sample, which may be an artifact of the instrument that we utilized. Although the BSI is an instrument with strong psychometric properties (Derogatis & Spencer, 1993), we may have obtained different results if we had used an instrument that provides a clinical diagnosis of depression rather than one that primarily describes symptoms. Finally, the cross-sectional design of our study does not permit causal inferences. Although our results indicate that the relationship between depressive symptoms and SCD pain frequency changes as a result of internalized stigma about the condition, we have yet to identify specific components or mechanisms that cause this change. Further empirical research is necessary before an explanatory model can be articulated.
Despite these limitations, the current study has several strengths. First, notwithstanding the small sample, we had acceptable statistical power to detect effects and obtained relatively robust effect sizes. Second, we measured two of our three primary variables (i.e., internalized stigma and depressive symptoms) with instruments that were psychometrically sound and commonly used in studies with this patient population. We also ensured that our data appropriately met the assumptions of the statistical techniques we employed. In addition, we made the necessary transformation of the pain frequency variable in order to address issues of skewness and kurtosis, thereby reducing the overestimation that might have led to spurious findings. Finally, our focus on internalized stigma represents a unique perspective that distinguishes this work from approaches that rely on global measurement of the stigma construct and extends previous work that failed to concurrently assess depressive symptoms, patient-reported pain frequency, and stigma (Bediako et al., 2016; Jenerette et al., 2012). We see this as a significant strength because our approach is consistent with the recent research literature which suggests that assessing the multidimensional nature of stigma increases the likelihood of a more distinctive comprehension of how stigma operates, which might then lead to the development of more efficient and effective interventions (Earnshaw, Smith, Cunningham, & Copenhaver, 2015).
If the results of this study were replicated in more definitive studies with larger samples, two clinical implications would be apparent. First, there would be evidence to suggest that a sole focus on the relationship between negative affect and SCD pain is incomplete without considering the moderating role of other psychosocial factors. Second, such studies would demonstrate a need for greater attention to the multidimensional nature of stigma in the clinical milieu. Research by Bediako et al. (2016) suggests that even though internalization of SCD stigma is not a common occurrence, there is a significant clinical impact when it manifests. Additional research is needed to further elucidate the ways in which the internalization of SCD-related stigma operate to affect pain and other important outcomes that affect the overall quality of life of adults living with this condition.
Acknowledgments
This research was supported by Grant K07HL108742 awarded to SMB by the National Heart, Lung and Blood Institute of the National Institutes of Health. BMH and LSM were supported by a National Institute of General Medical Sciences Initiative for Maximizing Student Development Grant (R25GM55036) awarded to the University of Maryland, Baltimore County. The content of this manuscript is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health.
References
- Alao AO, Cooley E. Depression and sickle cell disease. Harvard Review of Psychiatry. 2001;9:169–177. doi: 10.1080/10673220127896. doi:10.1080/10673220127896. [DOI] [PubMed] [Google Scholar]
- Asnani MR, Fraser R, Lewis NA, Reid ME. Depression and loneliness in Jamaicans with sickle cell disease. BMC Psychiatry. 2010;10 doi: 10.1186/1471-244X-10-40. doi:10.1186/1471-244x-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballas SK, Gupta K, Adams-Graves P. Sickle cell pain: A critical reappraisal. Blood. 2012;120:3647–3656. doi: 10.1182/blood-2012-04-383430. doi:10.1182/blood-2012-04-383430. [DOI] [PubMed] [Google Scholar]
- Bediako SM. Psychosocial aspects of sickle cell disease: A primer for African American psychologists. In: Neville HA, Tynes BM, Utsey SO, editors. Handbook of African American psychology. Sage; Thousand Oaks, CA: 2009. pp. 417–427. [Google Scholar]
- Bediako SM, Haywood C. Sickle cell disease in a “postracial” America. Journal of the National Medical Association. 2009;101:1065–1066. doi: 10.1016/s0027-9684(15)31075-0. doi.org/10.1016/S0027-9684(15)31075-0. [DOI] [PubMed] [Google Scholar]
- Bediako SM, Lanzkron S, Diener-West M, Onojobi G, Beach MC, Haywood C., Jr. The Measure of Sickle Cell Stigma: Initial findings from the Improving Patient Outcomes through Respect and Trust study. Journal of Health Psychology. 2016;21:808–820. doi: 10.1177/1359105314539530. doi:10.1177/1359105314539530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bediako SM, Moffitt KR. Race and social attitudes about sickle cell disease. Ethnicity & Health. 2011;16:423–429. doi: 10.1080/13557858.2011.552712. doi:10.1080/13557858.2011.552712. [DOI] [PubMed] [Google Scholar]
- Bediako SM, Neblett EW., Jr. Optimism and perceived stress in sickle-cell disease: The role of an Afrocultural social ethos. Journal of Black Psychology. 2011;37:234–253. doi:10.1177/0095798410385681. [Google Scholar]
- Caird H, Camic PM, Thomas V. The lives of adults over 30 living with sickle cell disorder. British Journal of Health Psychology. 2011;16:542–558. doi: 10.1348/135910710X529278. doi:10.1348/135910710X529278. [DOI] [PubMed] [Google Scholar]
- Cohen M, Quintner J, Buchanan D, Nielsen M, Guy L. Stigmatization of patients with chronic pain: The extinction of empathy. Pain Medicine. 2011;12:1637–1643. doi: 10.1111/j.1526-4637.2011.01264.x. doi:10.1111/j.1526-4637.2011.01264.x. [DOI] [PubMed] [Google Scholar]
- Cooper AE, Corrigan PW, Watson AC. Mental illness stigma and care seeking. Journal of Nervous and Mental Disease. 2003;191:339–341. doi: 10.1097/01.NMD.0000066157.47101.22. doi:10.1097/00005053-200305000-00010. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest. 2014;15:37–70. doi: 10.1177/1529100614531398. doi:10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- Darbari DS, Ballas SK, Clauw DJ. Thinking beyond sickling to better understand pain in sickle cell disease. European Journal of Haematology. 2014;93:89–95. doi: 10.1111/ejh.12340. doi:10.1111/ejh.12340. [DOI] [PubMed] [Google Scholar]
- Darbari DS, Castro O, Taylor JG, Fasano R, Rehm J, Gordeul VR, Minniti CP. Severe vaso-occlusive episodes associated with use of systemic corticosteroids in patients with sickle cell disease. Journal of the National Medical Association. 2008;100:948–951. doi: 10.1016/S0027-9684(15)31410-3. doi:10.1016/S0027-9684(15)31410-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbari DS, Wang Z, Kwak M, Hildesheim M, Nichols J, Allen D, Taylor Vi JG. Severe painful vaso-occlusive crises and mortality in a contemporary adult sickle cell anemia cohort study. PLoS ONE. 2013;8:1–1. doi: 10.1371/journal.pone.0079923. doi:10.1371/journal.pone.0079923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derlega VJ, Maduro RS, Janda LH, Chen IA, Goodman BM., III What motivates individuals with sickle cell disease to talk with others about their illness? Reasons for and against sickle cell disease disclosure. Journal of Health Psychology. doi: 10.1177/1359105316649786. in press doi:10.1177/1359105316649786. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Spencer PM. Brief Symptom Inventory: Administration scoring and procedures manual. 3rd ed. National Computer Systems; Minneapolis, MN: 1993. [Google Scholar]
- Drapalski AL, Lucksted A, Perrin PB, Aakre JM, Brown CH, DeForge BR, Boyd JE. A model of internalized stigma and its effects on people with mental illness. Psychiatric Services. 2013;64:264–269. doi: 10.1176/appi.ps.001322012. doi:10.1176/appi.ps.001322012. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. Journal of Health Psychology. 2012;17:157–168. doi: 10.1177/1359105311414952. doi:10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Cunningham CO, Copenhaver MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: Implications for depressive symptoms. Journal of Health Psychology. 2015;20:1083–1089. doi: 10.1177/1359105313507964. doi:10.1177/1359105313507964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards CL, Scales MT, Loughlin C, Bennett GG, Harris-Peterson S, De Castro LM, Killough A. A brief review of the pathophysiology, associated pain, and psychosocial issues in sickle cell disease. International Journal of Behavioral Medicine. 2005;12:171–179. doi: 10.1207/s15327558ijbm1203_6. doi:10.1207/s15327558ijbm1203_6. [DOI] [PubMed] [Google Scholar]
- Edwards R, Telfair J, Cecil H, Lenoci J. Self-efficacy as a predictor of adult adjustment to sickle cell disease: One-year outcomes. Psychosomatic Medicine. 2001;63:850–858. doi: 10.1097/00006842-200109000-00020. doi.org/10.1097/00006842-200109000-00020. [DOI] [PubMed] [Google Scholar]
- Field A. Discovering statistics using IBM SPSS statistics. Sage Publications; London: 2013. [Google Scholar]
- Gilovich T, Keltner D, Chen S, Nisbett RE. Social psychology. W. W. Norton & Company; New York, NY: 2016. [Google Scholar]
- Fiske ST. Social beings: A core motives approach to social psychology. John W. Wiley & Sons; New York, NY: 2004. [Google Scholar]
- Grant MM, Gil KM, Floyd MY, Abrams M. Depression and functioning in relation to health care use in sickle cell disease. Annals of Behavioral Medicine. 2000;22:149–157. doi: 10.1007/BF02895779. doi:10.1007/bf02895779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris A, Barker N, Parker C. Adults with sickle cell disease: Psychological impact and experience of hospital services. Psychology, Health, & Medicine. 1998;3:171–179. doi:10.1080/13548509808402233. [Google Scholar]
- Hasan SP, Hashmi S, Alhassen M, Lawson W, Castro O. Depression in sickle cell disease. Journal of the National Medical Association. 2003;95:533–537. [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York, NY: 2013. [Google Scholar]
- Haywood C, Jr., Lanzkron S, Bediako S, Strouse JJ, Haythornthwaite J, Carroll CP, Beach MC. Perceived discrimination, patient trust, and adherence to medical recommendations among persons with sickle cell disease. Journal of General Internal Medicine. 2014;29:1657–1662. doi: 10.1007/s11606-014-2986-7. doi:10.1007/s11606-014-2986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. American Journal of Public Health. 2013;103:777–780. doi: 10.2105/AJPH.2012.301056. doi:10.2102/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disability & Rehabilitation. 2007;29:1456–1464. doi: 10.1080/09638280601107260. doi:10.1080/09638280601107260. [DOI] [PubMed] [Google Scholar]
- Jenerette CM, Brewer CA, Crandell J, Ataga KI. Preliminary validity and reliability of the Sickle Cell Disease Health-Related Stigma Scale. Issues in Mental Health Nursing. 2012;33:363–369. doi: 10.3109/01612840.2012.656823. doi:10.3109/01612840.2012.656823. [DOI] [PubMed] [Google Scholar]
- Jenerette CM, Funk M, Murdaugh C. Sickle cell disease: A stigmatizing condition that may lead to depression. Issues in Mental Health Nursing. 2005;26:1081–1101. doi: 10.1080/01612840500280745. doi:10.1080/01612840500280745. [DOI] [PubMed] [Google Scholar]
- Jonassaint CR, Jones VL, Leong S, Frierson GM. A systematic review of the association between depression and health care utilization among children and adults with sickle cell disease. British Journal of Haematology. 2016 doi: 10.1111/bjh.14023. doi: 10.1111/bjh.14023. [DOI] [PubMed] [Google Scholar]
- Lattimer L, Haywood C, Lanzkron S, Ratanawongsa N, Bediako SM, Beach MC. Problematic hospital experiences among adult patients with sickle cell disease. Journal of Health Care for the Poor and Underserved. 2010;21:1114–1123. doi: 10.1353/hpu.2010.0940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurence B, George D, Woods D. Association between elevated depressive symptoms and clinical disease severity in African-American adults with sickle cell disease. Journal of the National Medical Association. 2006;98:365–369. [PMC free article] [PubMed] [Google Scholar]
- Levenson JL, McClish DK, Dahman BA, Bovbjerg VE, de A. Citero V, Penberthy LT, Smith WR. Depression and anxiety in adults with sickle cell disease: The PiSCES project. Psychosomatic Medicine. 2008;70:192–196. doi: 10.1097/PSY.0b013e31815ff5c5. doi:10.1097/PSY.0b013e31815ff5c5. [DOI] [PubMed] [Google Scholar]
- McCrae JD, Lumley MA. Health status in sickle cell disease: Examining the roles of pain coping strategies, somatic awareness, and negative affectivity. Journal of Behavioral Medicine. 1998;21:35–55. doi: 10.1023/a:1018763404868. doi:10.1023/a:1018763404868. [DOI] [PubMed] [Google Scholar]
- Monsivais DB. Decreasing the stigma burden of chronic pain. Journal of the American Association of Nurse Practitioners. 2013;25:551–556. doi: 10.1111/1745-7599.12010. doi:10.1111/1745-7599.12010. [DOI] [PubMed] [Google Scholar]
- Ola BA, Yates SJ, Dyson SM. Living with sickle cell disease and depression in Lagos, Nigeria: A mixed methods study. Social Science & Medicine. 2016;161:27–36. doi: 10.1016/j.socscimed.2016.05.029. doi:10.1016/j.socscimed.2016.05.029. [DOI] [PubMed] [Google Scholar]
- Overstreet NM, Earnshaw VA, Kalichman SC, Quinn DM. Internalized stigma and HIV status disclosure among HIV-positive Black men who have sex with men. AIDS Care. 2013;25:466–471. doi: 10.1080/09540121.2012.720362. doi:10.1080/09540121.2012.720362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer JJW, Gil KM, Burchinal M, Kramer KD, Nash KB, Orringer E, Strayhorn D. Depression, disease severity, and sickle cell disease. Journal of Behavioral Medicine. 1999;22:115–126. doi: 10.1023/a:1018755831101. doi:10.1023/a:1018755831101. [DOI] [PubMed] [Google Scholar]
- Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Medicine. 2009;10:143–154. 112. doi: 10.1111/j.1526-4637.2008.00540.x. doi:10.1111/j.1526-4637.2008.00540.x. [DOI] [PubMed] [Google Scholar]
- Smith WR, Penberthy LT, Bovbjerg VE, McClish DK, Roberts JD, Dahman B, Roseff SD. Daily assessment of pain in adults with sickle cell disease. Annals of Internal Medicine. 2008;148:94–101. doi: 10.7326/0003-4819-148-2-200801150-00004. doi.org/10.7326/0003-4819-148-2-200801150-00004. [DOI] [PubMed] [Google Scholar]
- Sogutlu A, Levenson JL, McClish DK, Rosef SD, Smith WR. Somatic symptom burden in adults with sickle cell disease predicts pain, depression, anxiety, health care utilization, and quality of life: The PiSCES project. Psychosomatics: Journal of Consultation and Liaison Psychiatry. 2011;52:272–279. doi: 10.1016/j.psym.2011.01.010. doi:10.1016/j.psym.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Weiser SD. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Annals of Behavioral Medicine. 2013;46:285–294. doi: 10.1007/s12160-013-9514-6. doi:10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity. 2011;19:757–762. doi: 10.1038/oby.2010.234. doi:10.1038/oby.2010.234. [DOI] [PubMed] [Google Scholar]
- Watson AC, Angell B. The role of stigma and uncertainty in moderating the effect of procedural justice on cooperation and resistance in police encounters with persons with mental illnesses. Psychology, Public Policy, and Law. 2013;19:30–39. doi: 10.1037/a0027931. doi:10.1037/a0027931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waugh OC, Byrne DG, Nicholas MK. Internalized stigma in people living with chronic pain. The Journal of Pain. 2014;15:e1–e10. doi: 10.1016/j.jpain.2014.02.001. doi:10.1016/j.jpain.2014.02.001. [DOI] [PubMed] [Google Scholar]
- Woods K, Karrison T. Hospital utilization patterns and costs for adult sickle. Public Health Reports. 1997;112:44. [PMC free article] [PubMed] [Google Scholar]
- Yang YM, Shah AK, Watson M, Mankad VN. Comparison of costs to the health sector of comprehensive and episodic health care for sickle cell disease patients. Public Health Reports. 1995;110:80–86. [PMC free article] [PubMed] [Google Scholar]