Abstract
Background
Healthcare transition from pediatric to adult care for young adults (YA) with type 1 diabetes (T1D) is associated with risk of adverse outcomes. Consensus recommendations exist from US professional societies on transition care for YA with T1D, but it is not known whether they have been widely adopted. We describe experiences, barriers, and provider characteristics associated with transition care in a national sample of pediatric endocrinologists.
Methods
US pediatric endocrinologists identified through the American Medical Association Physician Masterfile were sent an electronic survey.
Results
Response rate was 16% (164/1020) representing 32 states. The majority of pediatric endocrinologists (age 44 ± 10; years in practice 12 ± 11) were female (67%) and worked in academic centers (75%). Main reasons for transfer were age (49%) and glycemic control (18%). Barriers to transition included ending long-therapeutic relationships with patients (74%), lack of transition protocols (46%), and perceived deficiencies in adult care (42%). The majority of pediatric endocrinologists reported lack of transition training (68%); those who received training were less likely to have difficulty ending patient relationships [odds ratio (OR) = 0.39, P = .03], more likely to perform patient record transfer to adult systems (OR=1.27, P = .006), and less likely to report patient returns to pediatric care after transfer (OR=0.49, P = .01), independent of endocrinologist gender, years in practice, or practice type.
Conclusions
There is wide variation in transition care for YA with T1D among US pediatric endocrinologists despite consensus recommendations. Dissemination of educational programming on transition care and provision of actionable solutions to overcome local health system and perceived barriers is needed.
Keywords: pediatric endocrinologists, pediatric to adult transition, physician survey, type 1 diabetes, young adults
1 | INTRODUCTION
The period of transition from pediatric to adult care for young adults (YA) with type 1 diabetes (T1D) is a difficult time to achieve target glycemic control and maintain follow up.1 Numerous studies have demonstrated that YA with T1D experience poor health outcomes and gaps in care prior to and during the period of healthcare transition regardless of care setting, insurance coverage type, or integration of pediatric and adult centers.2–5 Transition is defined as the overarching process of development from adolescence to adulthood, encompassing a time period of preparation and practice to become a high functioning patient in adult care, whereas transfer is defined as the distinct time point within transition at which care is shifted between pediatric and adult systems.6 While issues related to this transitional period are due to a complex set of factors, prior studies have suggested that timing of and preparation for transfer from pediatric care, which is coordinated by the pediatric provider, has the potential to alter outcomes.6–8 Although expert consensus recommendations exist for transition care specifically pertaining to YA with T1D,9 standardized policies at the health system level in most centers in the U.S. either do not exist or are not widespread. Thus, there likely remains wide variability in care for transitioning YA with T1D which may impact health outcomes.
The American Diabetes Association (ADA) issued a position statement in 2011, based on expert consensus in collaboration with several other professional societies, outlining recommendations for pediatric providers to transition YA with diabetes to adult care. The consensus recommendations incorporated addition of care components unique to YA with T1D, assessment of readiness of the YA to transfer, advice on when to initiate transfer, and guided proper transfer practices.9 There is broad consensus that planning for transition and transfer should be an integral part of standard of care for transition9–12; however, it is unclear whether transition care in the U.S. has become standardized since the recommendations were published or whether barriers exist to implementation.
Although transition care is of great interest to providers caring for YA with T1D, studies examining pediatric provider care practices and perspectives are limited. De Beaufort et al13 reported on transition care in an international sample of pediatric providers in 2010 and demonstrated that despite awareness of transition issues, most pediatric centers did not have a structured transition program and those that did only had local policies and made informal personal contact with cooperating adult centers. To date, there are few, if any, studies specifically focused on pediatric perspectives and transition care in the U.S., which has a very different health care system than other countries with universal health care systems. Furthermore, there have been little to no studies examining transition care and perceived barriers since the publication of the 2011 ADA recommendations where transitional issues in YA with T1D were formally acknowledged.
Patient and adult diabetes provider perspectives in T1D suggest that there is a lack of standardized and appropriate preparation of patients for adult care as well as barriers such as patient/provider reluctance to leave pediatric care.14–16 Reports from pediatric providers transitioning chronic diseases other than T1D, such as inflammatory bowel disease (IBD) and sickle cell disease, demonstrate that there is no standardization in transition care, lack of adherence to formal guidelines, and corroborate many of the barriers reported by T1D YA patients, families, and adult providers.17–19 However, it remains unclear what is actually experienced by U.S. pediatric diabetes providers. Ultimately, it is vital to investigate these remaining questions in order to facilitate transition experiences and outcomes, and to inform transition policies.
The objective of this study was to survey a national sample of pediatric endocrinologists from the U.S. to (1) assess variability in transition care, specifically transfer processes, since the publication of the ADA expert consensus recommendations on transitioning YA with T1D, (2) identify perceptions of principal barriers to transition and associated characteristics of providers and practices, and (3) examine whether receipt of transition training was associated with provider-specific delivery of transition care components.
2 | METHODS
2.1 | Survey development
We developed the Pediatric Provider Transition Care Survey based on prior literature highlighting persistent needs for overcoming barriers to initiating transition and standardization of transfer processes for YA with T1D; this included lack of use of protocols to make transfer decisions, lack of patient record transfer between health systems, and inadequate processes and preparation of patients for adult care.15,16,20 In addition, we utilized similar pediatric transition care surveys from other fields such as IBD as a model.19 The initial survey was reviewed by 8 pediatric and adult endocrinologists as well as primary care and IBD pediatricians. After initial feedback, the survey was revised and administered to a group of 10 pediatric diabetes providers (nurse practitioners and endocrinologists) involved in T1D transition at the Children’s Hospital of Philadelphia.
The final version of the survey had 22 questions and was able to be completed in less than 10 minutes. Survey questions were organized into different themes including: (1) transfer practices, (2) perceived differences between pediatric and adult care which impacted initiation of transfer, (3) receipt of transition training, (4) barriers to transition care, and (5) desired solutions to overcome barriers. Response format to survey questions included (1) multiple choice with “other” free response options and (2) frequency of performing a pre-specified practice as never, rarely, sometimes, often, or always. In addition, demographic information of respondents and practices was obtained with a set of eight brief questions.
A copy of the survey is available on reader request. This study was approved by the institutional review board at the University of Pennsylvania, Philadelphia, PA.
2.2 | Survey administration
Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Pennsylvania.21 A link to the Redcap-based survey was embedded in an email and sent to physicians within the American Medical Association (AMA) Masterfile with the specific associated titles of “pediatric” and “endocrinologist” or “diabetes”. The Masterfile is compiled by the AMA to keep record of all physicians since 1906 that have completed medical school or post-graduate training in the U.S.
We fielded the survey in three waves between August and November 2015. Responses were anonymous and there was no compensation for completing the survey. Survey responses were included in analysis if respondents noted seeing more than 10 patients with T1D in their practice and if all questions related to transition practices were answered.
2.3 | Statistical analysis
Data were analyzed using STATA for Windows version 14.0 software (StataCorp LP, College Station, Texas). Descriptive statistics were reported as mean and standard deviation or proportion. Multiple logistic regression was utilized to examine how respondent characteristics related to survey responses. In addition, associations based on receipt of transition training (yes/no) were explored. Specifically, respondent characteristics considered for multivariate modeling included: age, gender, years in practice, and practice type. Given possible collinearity of characteristics, associations of the four predictor variables were assessed using linear regression. Age and years in practice were the only highly correlated pair of variables (R2 = 0.89); age, therefore, was omitted as a variable in analysis. Gender, years in practice, and practice type were chosen as the final set of predictor variables. Statistical significance was defined for P-values <.05.
3 | RESULTS
3.1 | Survey response rate
A total of 1320 physicians in the U.S. were listed as “pediatric” and “endocrinologist” or “diabetes” in the AMA Masterfile in August 2015. As a comparison, the American Board of Pediatrics had granted 1635 diplomate certificates to pediatric endocrinologists as of December 2014 (www.abp.org). Of the 1320, the survey was e-mailed successfully to a final total of 1020 pediatric endocrinologists.
We received 164 responses (16% response rate). Of the 164, 22 surveys were excluded per a priori exclusion criteria. A total of 142 surveys were analyzed.
3.2 | Pediatric endocrinologist and practice characteristics
Respondents were 44 ± 10 years old and had been practicing for 12 ± 11 years. The majority was female (67%) and Caucasian (72%), worked in an academic medical center (76%), in a metropolitan setting (71%), and had 25%–50% of their patient panel covered by a public insurance plan (73%). A total of 32 states were represented from the continental U.S.: 36% from the Northeast, 25% from the South, 23% from the Midwest, and 15% from the West. For comparison, in aggregate data on the pediatric endocrinologist workforce reported by the American Board of Pediatrics as of December 2015, mean age was 53.6 years and 77% were female; in addition, based on regional distributions, our sample represented 9.0%–14.3% of pediatric endocrinologists in each of the aforementioned geographical regions (www.abp.org). Refer to Table 1 for additional demographic information.
TABLE 1.
Pediatric endocrinologist and practice characteristics (n = 142)
| N | Mean ± SD or % | |
|---|---|---|
| Age (years) | 142 | 44.1 ± 10.3 |
| Gender (female) | 142 | 67 |
| Race | 140 | |
| Caucasian | 72 | |
| African American | 5 | |
| Asian/Pacific Islander | 19 | |
| Hispanic | 3 | |
| Other | 1 | |
| Years in practice | 142 | 12.1 ± 10.8 |
| US region of practice | 140 | |
| Northeast | 36 | |
| South | 25 | |
| Midwest | 23 | |
| West | 16 | |
| Practice setting | 141 | |
| Metropolitan | 71 | |
| Suburban | 26 | |
| Rural | 3 | |
| Practice type | 141 | |
| Academic medical center | 76 | |
| Private single specialty practice | 18 | |
| Private multi-specialty practice | 4 | |
| Private solo practice | 2 | |
| Number of patients with type 1 diabetes in Physician panel | 142 | |
| >200 | 48 | |
| 101–200 | 18 | |
| 51–100 | 20 | |
| 26–50 | 10 | |
| <25 | 5 | |
| Percentage of T1D patients ages ≥18 years | 142 | |
| 0 | 11 | |
| 25 | 81 | |
| 50 | 6 | |
| 75 | 2 | |
| 100 | 0 | |
| Percentage of patients on public insurance | 142 | |
| 0 | 4 | |
| 25 | 25 | |
| 50 | 48 | |
| 75 | 19 | |
| 100 | 4 |
SD, standard deviation.
In the current study, older respondents were more likely to be male (t = 2.76, P < .001) and in practice for longer (t = 31.61, P < .001). In addition, those practicing in academic settings were more likely to be in metropolitan areas (t = 4.66, P < .001). There were no associations between practice setting or type with age or years in practice (P > .05 for all comparisons).
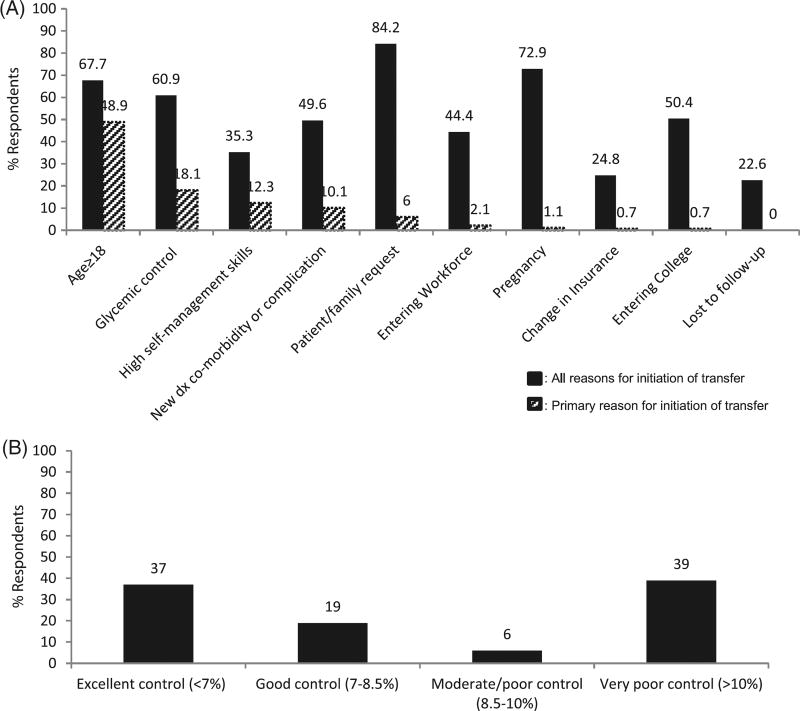
3.3 | Transfer practices
Respondents considered patient/family request for transfer (84%), pregnancy (73%), age ≥18 years (68%), glycemic control (61%), entering college (50%), and a new diagnosis of diabetes-related comorbidity or complication (50%) as reasons to initiate transfer. When noting the primary reason for initiation of transfer, there was wide variability with half of respondents (49%) endorsing age ≥18 years, 18% endorsing glycemic control, and 12% endorsing high self-management skills (Fig. 1A). Regarding glycemic control, there was no organized response, with equal endorsement of prioritization for transfer of patients who had excellent and very poor glycemic control (Fig. 1B). There was no difference in transfer decisions with glycemic control based on respondent gender, years in practice, or practice type.
FIGURE 1.
(A) Reasons for transfer to adult care. (B) Priority of transfer by glycemic control category [% glycated hemoglobin (HbA1c)].
Regarding patient record transfer to adult care, 55% of respondents endorsed sending medical records with the patient, 20% reported no communication, 15% endorsed record transfer in the form of a clinical summary letter, 7% had a phone conversation with the adult provider, and 3% used a transition template summary.
A total of 83% of respondents stated that they never/rarely received feedback from the adult provider after the YA transferred care. Half endorsed patients returning to their care after transfer sometimes whereas 3% reported that this occurred most of the time.
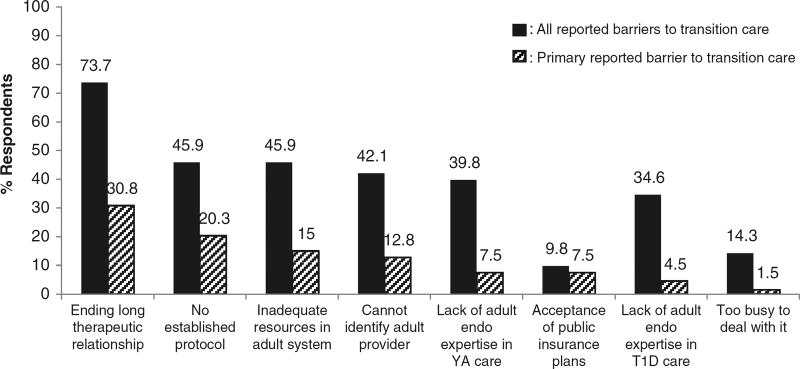
3.4 | Barriers to transition care
The majority of respondents noted ending a long-therapeutic relationship with the patient as a barrier (74%) and the main barrier (31%) to transition (Figure 2). Respondents who endorsed this were more likely to be female (OR = 1.26, P = .006), have more practice experience (OR = 1.07, P = .03), and were less likely to have Medicaid patients (OR = 0.61, P = .005).
FIGURE 2.
Barriers to transition care.
Nearly half of respondents (46%) reported lack of an established transition protocol as a barrier and 20% reported it as a main barrier to transition care (Figure 2). Respondents with more practice experience did not perceive lack of protocol as a barrier compared with their less experienced counterparts (OR = 0.91, P = .002).
3.5 | Perceived deficiencies in adult systems
A large proportion of respondents considered deficiencies in the adult healthcare system as barriers to initiation of transfer, such as inadequate resources to care for YA with T1D (46%), inability to identify adult providers who care for YA with T1D (42%), lack of adult provider expertise in YA care (40%), and lack of adult provider expertise in T1D care (35%). A total of 15% of respondents noted that inadequate resources within the adult healthcare system were the main barrier to transition care, with 13% noting the inability to identify adult providers (Fig. 2).
When asked about which resources were perceived to be lacking in adult systems, respondents felt that mental health services (79%), availability of a social worker (69%), and diabetes device-downloading capabilities (48%) were lacking.
3.6 | Impact of receipt of transition training on transition care
The majority of respondents reported that they had not received an introduction to or training in transition care (68%) (eg, a webinar, national or regional CME-accredited lecture, lecture in local academic center, professional academic or medical society information/resources). Respondents who received transition training were more likely to be practicing in academic centers (OR = 3.39, P = .008), have less difficulty transitioning patients due to ending a long-therapeutic relationship (OR = 0.39, P = .03), were more likely to perform record transfer to adult providers (OR = 1.27, P = .006), and reported fewer patient returns to pediatric care after transfer to adult care (OR = 0.49, P = .01) (Table 2). Notably, respondents endorsed lack of transition protocol as a barrier to proper transition care regardless of whether they received transition training (46%) (OR = 0.89, P = 0.71) (Table 2).
TABLE 2.
Associations between receipt of transition training and respondent characteristics/perceived barriers/transition care components
| Odds ratio1 | 95% CI | P-value | |
|---|---|---|---|
| Gender | 1.09 | 0.45–2.64 | .86 |
| Years in practice | 1.02 | 0.98–1.07 | .99 |
| Academic center | 3.39 | 1.38–8.28 | .008 |
| Ending long-therapeutic relationship | 0.39 | 0.14–0.98 | .03 |
| Lack of transition protocol | 0.89 | 0.34–2.30 | .81 |
| Record transfer | 1.27 | 1.05–1.49 | .006 |
| Return to pediatric care after transfer | 0.71 | 0.43–0.91 | .01 |
CI, confidence interval.
Models adjusted for gender, years in practice, and practice type comparing respondents who received transition training vs. those who did not.
3.7 | Solutions to improve transition care
The majority of respondents desired a joint discussion of the patient/family and adult provider prior to transfer (70%), an algorithm for referring patients (64%), a transition readiness assessment tool (63%), transition materials for patients (63%), and transition-specific visits (55%) to aid in transition care. A smaller proportion wanted access to a list of adult providers/practices which accept YA with T1D (39%) or a transition event (36%).
DISCUSSION
In this national survey of pediatric endocrinologists, there was wide variation in transition care with regards to transfer processes. Barriers to transition included having to end long-therapeutic relationships with patients, lack of transition protocols, and perceived deficiencies in adult care. The majority of respondents had not received transition care training; those that received training were more likely to practice in an academic medical center. Receipt of training impacted several provider-specific care practices including the ability to end relationships more easily in order to transition patients, improvement of record transfer to adult providers, and less frequent return of patients to pediatric care after transfer. Nevertheless, even for respondents who had received transition training, lack of established transition protocols in their practice settings was still reported as a major barrier.
While the ADA expert consensus recommendations provide guidance to pediatricians on transitioning YA with T1D to adult care, there remains wide variability in transition care amongst US pediatric endocrinologists. These variations could indicate lack of knowledge of appropriate transition care or represent local and regional environments which affect policies surrounding transition. In studies examining transition care for IBD, pediatric gastroenterologists endorsed both knowledge and policy barriers.19 Thus, additional transition care training and acknowledgement of variations in local practice environments during policy development are needed.
Variations could also stem from the lack of literature and detailed guidance on how to appropriately select patients who will successfully transition to adult care. In the current study, lack of a transition protocol was noted by many respondents as a barrier to transition care, which may speak to the need for more specific detailed guidance on transition practices as opposed to overarching general guidelines which are currently available. This underscores the importance of the use of tools to help guide pediatric endocrinologists in making more evidence-based decisions on selection of patients to transition, such as the transition readiness assessment questionnaire (TRAQ) or Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART) framework, which identifies modifiable and non-modifiable factors that confer likelihood of success in transfer to adult-oriented care.8,22
Regarding reasons for transfer initiation, while the consensus recommendations emphasized assessment of diabetes self-management skills as a focal point, only a small proportion of respondents in the current study reported high self-management skills to be the main reason for transfer.9 In fact, the majority of respondents endorsed age over 18 years and glycemic control as the most common reasons for transfer; however, age cutoffs and glycemic control criteria are neither mentioned nor recommended for use in the guidelines. For age, conflicts between practice and guidelines may be due to restrictions imposed by insurance and institutional policies which dictate the transition time period. For glycemic control, it is puzzling that poorly controlled patients were prioritized for transfer equally to excellently controlled patients. It may be that pediatric endocrinologists struggle in caring for poorly controlled patients and feel that their care could be improved with a new provider in adult care. Another explanation could be that poor glycemic control, if a product of patient disengagement in care, could indicate a poor therapeutic relationship between pediatric endocrinologist and patient; thus, it is easier to transfer them to adult care. Given that poorly controlled patients may be more prone to worsening glycemic control after transfer to adult care, this needs to be explored further in qualitative studies.23
In addition to variation in transfer initiation, there was wide variation in the processes of patient record transfer. Reponses ranged from medical records sent with the patient to no information sent, and no receipt of feedback from adult to pediatric providers. Although some of the respondents who endorsed lack of record transfer may have been unable to identify an adult provider to communicate with, it is still concerning that standardized sharing of patient information is not routinely performed at transfer. In a recent study, adult endocrinologists endorsed lack of record transfer as a key barrier to caring for YA with diabetes leaving pediatric care.13,20 Lack of receipt of records may place undue burden on adult endocrinologists receiving patients who have been in a pediatrician’s care for years. In addition, effective communication between a new patient and their first adult endocrinologist could be hampered if the patient senses lack of knowledge about their history and interprets this as lack of investment in their care.24 Conversely, without proper feedback from adult to pediatric providers, disorganized transfer processes and unsatisfactory experiences for patients and providers may go unchecked.5,13,14 Thus, patient record transfer appears to be paramount in maintaining various relationships within transition care.
Regarding barriers to transition, most respondents reported an emotional attachment to the patient as a main barrier. This was more prevalent in respondents who were female, had been in practice longer, and had fewer Medicaid patients. While other studies examining patient-provider relationships across transition have identified emotional attachment as a barrier to transition,25,26 the impact of gender differences and patient-specific characteristics on this relationship has not been studied and is worthy of further exploration. In particular, the prospect of disparities in transition care delivery based on insurance and socioeconomic status needs to be explored given that YA with health disparities often have the worst health outcomes of their peer group and may suffer from not having as strong emotional attachments to their healthcare providers.27,28
Apart from emotional attachment, part of the reticence of pediatric endocrinologists to let go of their patients could also be due to perceptions of inadequate care delivered in adult systems. The majority of respondents felt that adult providers were not trained to care for YA with T1D. In addition, respondents felt that mental health resources were lacking in adult care. The current study did not distinguish primary care physicians (PCPs) from adult endocrinologists as receiving adult providers. Thus, it is difficult to assess whether respondent perception of inadequate YA/T1D expertise in adult providers was based on referral relationships with adult endocrinologists vs. PCPs who do not have as much training or resources to care for diabetes patients. Nevertheless, it would be important to further define pediatric endocrinologist perceptions of adult providers and systems as they may impact transition care. In a recent study, comparing training of adult endocrinologists vs. PCPs in caring for YA with T1D, adult endocrinologists reported higher levels of training in ADA standards of care and insulin administration while PCPs felt more proficient in depression screening and management.29 In another study, adult endocrinologists endorsed lacking mental health services to properly address YA needs.20 Given that YA with T1D need providers who are both proficient in diabetes care and mental health,9,10 bridging gaps in access to mental health resources and training in adult systems is important to accommodate YA needs.
Receipt of transition training impacted several respondent perceptions and practices. It is not surprising that respondents in academic centers were more likely to receive transition training compared with non-academic practices given increased access to new research and educational activities. However, it is encouraging that respondents who received transition training were less likely to report ending a long-therapeutic relationship as a barrier, more often completed medical record transfer to adult care, and had less return of patients to pediatric care after transfer. Thus, although guidelines and initial awareness surrounding transition issues for YA with T1D occurred in 2011,9 renewed efforts in educating and training pediatric endocrinologists on issues related to transition care should be a priority in both academic and non-academic practices.
Lastly, solutions endorsed by respondents to overcome barriers in transition care included use of algorithms for referral of patients and transition readiness tools. This again speaks to the need for more detailed guidance than is currently available. Recommendations could be provided with more actionable solutions such as use of checklists to grade self-management skills, training in coordination between pediatric care teams and families to decide timing of transfer proactively, and definition of standardized criteria based on recent literature for assessing readiness to transition. These could be components of a larger standardized transition protocol either at the local or national health system level. Efforts to promote development of standardized protocols should be encouraged given the recent addition of studies that have examined YA outcomes of various transition care delivery models for T1D.30–34
There are several limitations to this study. This survey was limited to physicians with an e-mail address on file with the AMA which could have caused selection bias. However, total eligible pediatric endocrinologists in our study available through the AMA Masterfile approximated the total number of diplomates awarded by the American Board of Pediatrics, and our response rate was higher or comparable to other physician survey studies in T1D, thus mitigating some of these concerns.13,20 In addition, as this was a survey of pediatric endocrinologists, it may underrepresent perspectives of non-endocrinology or non-physician diabetes pediatric providers who may have differing viewpoints. Lastly, given lower representation of rural and non-academic practices, there may be underrepresentation of transition care practices and barriers from these sectors which would be important to explore further.
In conclusion, our results show that despite the existence of expert consensus recommendations on transition care for YA with T1D, pediatric endocrinologists in the U.S. continue to report wide variations in care and persistent barriers. The findings of this national survey highlight several remaining needs of pediatric endocrinologists, including more detailed guidance on transition and transfer processes as well as more rigorous and standardized selection criteria for patients who will ultimately be successful in transition. Given the positive impact of transition training on reported barriers and transition processes in this study, there should be wide dissemination of programming to promote education on topics related to transition care and provision of actionable solutions. Lastly, biases and perceived differences in care paradigms and cultures between pediatric and adult systems should be explored further as it remains unclear if these issues are a barrier to adequate and complete transition of YA with T1D to adult care.
Acknowledgments
This work was supported by the Raymond and Joanne Welsh and G. Clayton Kyle foundations. This work was conducted with support from the University of Pennsylvania Society for Clinical Research Coordination and Management and University of Pennsylvania CTSA for use of RedCap.
References
- 1.Lyons SK, Becker DJ, Helgeson VS. Transfer from pediatric to adult health care: effects on diabetes outcomes. Pediatr Diabetes. 2014;15(1):10–17. doi: 10.1111/pedi.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pacaud D, Yale J, Stephure D, Trussell R, Davies H. Problems in transition from pediatric care to adult care for individuals with diabetes. Can J Diabetes. 2005;29(1):13–18. [Google Scholar]
- 3.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HAW. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26(4):1052–1057. doi: 10.2337/diacare.26.4.1052. [DOI] [PubMed] [Google Scholar]
- 4.Kipps S, Bahu T, Ong K, et al. Current methods of transfer of young people with type 1 diabetes to adult services. Diabet Med. 2002;19(8):649–654. doi: 10.1046/j.1464-5491.2002.00757.x. [DOI] [PubMed] [Google Scholar]
- 5.Busse FP, Hiermann P, Galler A, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67(3):132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- 6.Lyons SK, Libman IM, Sperling Ma. Diabetes in the adolescent: transitional issues. J Clin Endocrinol Metab. 2013;98(12):4639–4645. doi: 10.1210/jc.2013-2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polfuss M, Babler E, Bush LL, Sawin K. Family perspectives of components of a diabetes transition program. J Pediatr Nurs. 2015;30(5):748–756. doi: 10.1016/j.pedn.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz LA, Brumley LD, Tuchman LK, et al. Stakeholder validation of a model of readiness for transition to adult care. JAMA Pediatr. 2013;167(10):939–946. doi: 10.1001/jamapediatrics.2013.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters A, Laffel LMB, American Diabetes Association Transitions Working Group Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. A position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society) Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics and American College of Physicians, Transitions Clinical Report Authoring Group AA of FP. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 11.Standards of medical care in diabetes-2016. Diabetes Care. 2016;39(S1):86–93. [Google Scholar]
- 12.Pihoker C, Forsander G, Fantahun B, et al. ISPAD Clinical Practice Consensus Guidelines 2014 Compendium: the delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes. 2014;15(S20):86–101. doi: 10.1111/pedi.12181. [DOI] [PubMed] [Google Scholar]
- 13.de Beaufort C, Jarosz-Chobot P, Frank M, de Bart J, Deja G. Transition from pediatric to adult diabetes care: smooth or slippery? Pediatr Diabetes. 2010;11(1):24–27. doi: 10.1111/j.1399-5448.2009.00524.x. [DOI] [PubMed] [Google Scholar]
- 14.Garvey KC, Wolpert HA, Laffel LM, Rhodes ET, Wolfsdorf JI, Finkelstein JA. Health care transition in young adults with type 1 diabetes: barriers to timely establishment of adult diabetes care. Endocr Pract. 2013;19(6):1–22. doi: 10.4158/EP13109.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garvey KC, Beste MG, Luff D, Atakov-Castillo A, Wolpert HA, Ritholz MD. Experiences of health care transition voiced by young adults with type 1 diabetes: a qualitative study. Adolesc Health Med Ther. 2014;5:191–198. doi: 10.2147/AHMT.S67943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hilliard ME, Perlus JG, Clark LM, et al. Perspectives from before and after the pediatric to adult care transition: a mixed-methods study in type 1 diabetes. Diabetes Care. 2014;37(2):346–354. doi: 10.2337/dc13-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gray WN, Maddux MH. Current transition practices in pediatric IBD. Inflamm Bowel Dis. 2016;22(2):372–379. doi: 10.1097/MIB.0000000000000642. [DOI] [PubMed] [Google Scholar]
- 18.Stollon NB, Paine CW, Lucas MS, et al. Transitioning adolescents and young adults with sickle cell disease from pediatric to adult health care: provider perspectives. J Pediatr Hematol Oncol. 2015;37(8):577–583. doi: 10.1097/MPH.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paine CW, Stollon NB, Lucas MS, et al. Barriers and facilitators to successful transition from pediatric to adult inflammatory bowel disease care from the perspectives of providers. Inflamm Bowel Dis. 2014;20(11):2083–2091. doi: 10.1097/MIB.0000000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garvey KC, Telo GH, Needleman JS, Forbes P, Finklestein JALL. Health care transition in young adults with type 1 diabetes: perspectives of adult endocrinologists in the U.S. Diabetes Care. 2016;39(2):190–197. doi: 10.2337/dc15-1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul A Harris, Robert T, Robert T, Jonathon P, Nathaniel Gonzalez BSCS. Jose GC. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wood DL, Sawicki GS, Miller MD, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–422. doi: 10.1016/j.acap.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 23.Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062–e1070. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010;12(1):94–104. doi: 10.1111/j.1442-2018.2009.00506.x. [DOI] [PubMed] [Google Scholar]
- 25.Ritholz MD, Wolpert H, Beste M, Atakov-Castillo A, Luff D, Garvey KC. Patient-provider relationships across the transition from pediatric to adult diabetes care: a qualitative study. Diabetes Educ. 2013;40(1):40–47. doi: 10.1177/0145721713513177. [DOI] [PubMed] [Google Scholar]
- 26.Fernandes SM, Khairy P, Fishman L, et al. Referral patterns and perceived barriers to adult congenital heart disease care: results of a survey of U.S. pediatric cardiologists. J Am Coll Cardiol. 2012;60(22):2411–2418. doi: 10.1016/j.jacc.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 27.Berry JG, Bloom S, Foley S, Palfrey JS. Health inequity in children and youth with chronic health conditions. Pediatrics. 2010;126(Suppl. 3):S111–S119. doi: 10.1542/peds.2010-1466D. [DOI] [PubMed] [Google Scholar]
- 28.Gallegos-Macias AR, Macias SR, Kaufman E, Skipper B, Kalishman N. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes. 2003;4(1):19–23. doi: 10.1034/j.1399-5448.2003.00020.x. [DOI] [PubMed] [Google Scholar]
- 29.Lyons SK, Helgeson VS, Witchel SF, Becker DJKM. Physicians’ self-perceptions of care for emerging adults with type 1 diabetes. Endocr Pract. 2015;21(8):903–909. doi: 10.4158/EP14553.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sequeira PA, Pyatak EA, Weigensberg MJ, et al. Let’s Empower and Prepare (LEAP): evaluation of a structured transition program for young adults with type 1 diabetes. Diabetes Care. 2015;38(8):1412–1419. doi: 10.2337/dc14-2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with type 1 diabetes aged 15–25 years. Diabet Med. 2007;24(7):764–769. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- 32.Cadario F, Prodam F, Bellone S, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71(3):346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- 33.Vidal M, Jansa M, Anguita C, et al. Impact of a special therapeutic education programme in patients transferred from a paediatric to an adult diabetes unit. Eur Diabetes Nurs. 2004;1(1):23–27. [Google Scholar]
- 34.Steinbeck KS, Shrewsbury VA, Harvey V, et al. A pilot randomized controlled trial of a post-discharge program to support emerging adults with type 1 diabetes mellitus transition from pediatric to adult care. Pediatr Diabetes. 2015;16(8):634–639. doi: 10.1111/pedi.12229. [DOI] [PubMed] [Google Scholar]