Abstract
This data analysis seeks to determine whether changes in the use of advance directives between 2000 and 2010 are related to changing patterns of end-of-life care among nursing home residents receiving dialysis.
Patients with end-stage renal disease receiving dialysis have a symptom burden and prognosis comparable to patients with incurable cancer. They frequently and increasingly receive intensive procedures near the end of life. Because the benefits of these interventions remain controversial, a key question is whether increasing intensity of end-of-life care reflects changes in the extent to which patient preferences are elicited and documented with advance directives. Nursing homes offer an important setting to evaluate advance directive use because they accept full responsibility for care during patient stay.
To shed light on a potentially remediable care gap, we sought to determine whether changes in the use of advance directives between 2000 and 2010 are related to changing patterns of end-of-life care among nursing home residents receiving dialysis.
Methods
We used data from a national registry of patients receiving dialysis linked to Medicare claims and the Minimum Data Set to identify 153 285 nursing home residents who died in 2000 or 2010 with continuous Medicare coverage in the last 6 months of life and a nursing home record between 31 and 365 days before death. The institutional review board at Stanford University and the Veterans Affairs Palo Alto Research Committee approved the study.
We categorized patients according to the presence or absence of 2 advance directive components: a treatment-limiting advance directive (TLD), defined as documentation of any treatment limitations including resuscitation, hospitalization, feeding, and medications; and a surrogate decision maker. We ascertained 2 outcomes in the last month of life: intensive procedures (resuscitation, intubation, or mechanical ventilation) and intensive care unit (ICU) admission with International Classification of Diseases, Ninth Revision and revenue codes.
We estimated the difference between the change in end-of-life care between 2000 and 2010 among patients with 1 or both advance directive components and the change in end-of-life care over the same period among patients with neither advance directive component using modified Poisson regression. The models accounted for demographics, clinical characteristics, regional spending, and correlation of patients within nursing homes.
Results
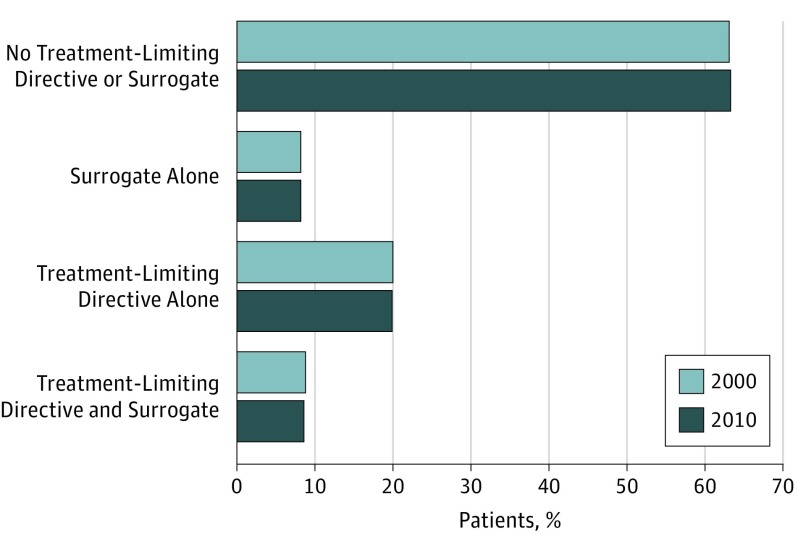
There was little difference in the frequency of TLDs and surrogates in 2000 vs 2010 (Figure). In both years, 63% of patients had neither advance directive component and fewer than 10% had both. Over the same period, the proportion of patients receiving an intensive procedure in the last month of life increased from 16% to 22% (P < .001) and the proportion admitted to an ICU in the last month of life increased from 34% to 47% (P < .001).
Figure. Prevalence of Advance Directives Among 153 285 Nursing Home Residents Receiving Dialysis, 2000 vs 2010 .
P value = .95 for comparison across groups.
Compared with patients who lacked a TLD and surrogate, the adjusted difference in the proportion of patients receiving an intensive procedure in 2000 vs 2010 did not differ for those with a TLD or surrogate alone, whereas it was 7 percentage points smaller among those with a TLD and surrogate (Table). There was no difference across these groups in the proportion of patients admitted to the ICU in the last month of life in 2000 vs 2010.
Table. Frequency of Intensive Procedures and ICU Admission in the Last Month of Life Among 153 285 Nursing Home Residents Receiving Dialysis According to Advance Directive Components, 2000 vs 2010 .
| Advance Directive Componenta | Patients, % | Adjusted Difference in Differences (95% CI)b | |
|---|---|---|---|
| 2000 | 2010 | ||
| Received Intensive Procedure | |||
| No treatment-limiting directive or surrogate | 21 | 28 | [Reference] |
| Surrogate alone | 13 | 22 | 3 (−2 to 7) |
| Treatment-limiting directive alone | 7 | 11 | −2 (−4 to 0) |
| Treatment-limiting directive and surrogate | 6 | 5 | −7 (−10 to −5) |
| Admitted to ICU | |||
| No treatment-limiting directive or surrogate | 40 | 53 | [Reference] |
| Surrogate alone | 31 | 47 | 5 (−1 to 11) |
| Treatment-limiting directive alone | 23 | 37 | 2 (−2 to 6) |
| Treatment-limiting directive and surrogate | 17 | 30 | 2 (−3 to 7) |
Abbreviation: ICU, intensive care unit.
Models adjusted for age, sex, race, years receiving dialysis, nursing home length of stay, hospital referral region spending, dialysis modality, diabetes, ischemic heart disease, heart failure, stroke, chronic lung disease, chronic liver disease, depression, dementia, functional status, and impaired decision making skills.
Change over time is expressed as the difference in differences.
Discussion
The most striking finding from our study of nursing home residents receiving dialysis is the large and persistent gap that exists between what is widely considered standard of care for patients with serious illness—elicitation and documentation of patient goals—and the care that is actually delivered. This gap is noteworthy because advance directives have increased in other segments of the population over the same period.
Hospitalization may be the most effective way to care for some chronically ill patients, while for others it is the path of least resistance that leads to an unintended escalation in care. Enhanced documentation of treatment limitations and surrogates with advance directives may limit intensive procedures near the end of life, but it may not stem the rising tide of ICU care.
References
- 1.Murtagh FE, Addington-Hall JM, Edmonds PM, et al. Symptoms in advanced renal disease: a cross-sectional survey of symptom prevalence in stage 5 chronic kidney disease managed without dialysis. J Palliat Med. 2007;10(6):1266-1276. [DOI] [PubMed] [Google Scholar]
- 2.Saran R, Li Y, Robinson B, et al. US Renal Data System 2015 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2016;67(3 Suppl 1):Svii, S1-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbash IJ, Kahn JM. Assessing the value of intensive care. JAMA. 2015;314(12):1240-1241. [DOI] [PubMed] [Google Scholar]
- 4.McAuley WJ, Buchanan RJ, Travis SS, Wang S, Kim M. Recent trends in advance directives at nursing home admission and one year after admission. Gerontologist. 2006;46(3):377-381. [DOI] [PubMed] [Google Scholar]
- 5.Silveira MJ, Wiitala W, Piette J. Advance directive completion by elderly Americans: a decade of change. J Am Geriatr Soc. 2014;62(4):706-710. [DOI] [PubMed] [Google Scholar]
- 6.Hart JL, Harhay MO, Gabler NB, Ratcliffe SJ, Quill CM, Halpern SD. Variability among US intensive care units in managing the care of patients admitted with preexisting limits on life-sustaining therapies. JAMA Intern Med. 2015;175(6):1019-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]