Abstract
Use of electronic nicotine delivery systems (ENDS) has increased substantially over the past decade. However, unlike smoking, which is systematically captured by clinicians through routine screening and discrete documentation fields in the electronic health record (EHR), unknown is the extent to which clinicians are documenting patients’ use of ENDS.
Data were gathered from medical visits with patients aged 12 and older (N = 9,119; 55% male) treated in a large, integrated healthcare system. We used natural language processing to assess the incidence rates of clinician documentation of patients’ ENDS use in unstructured tobacco comments in the EHR, and the words most frequently documented in relation to ENDS, from 2006–2015.
ENDS documentation in the EHR increased dramatically over time (from 0.01 to 9.5 per 10,000 patients, p < 0.0001), particularly among adults aged 18–24 and 25–44. Most prevalent were “e-cig,” “electronic cigarettes”, and “vape,” with much variation in spelling and phrasing of these words. Records of adolescent and young adult patients were more likely to contain the word “vape”, and less likely to have “e-cig” and “electronic cigarette” than records of adults (ps < 0.0001). The relatively low observed number of patients with ENDS terms in the EHR suggested vast under documentation.
While healthcare providers are increasingly documenting patients’ use of ENDS in the EHR, overall documentation rates remain low. Discrete EHR fields for standard screening and documentation of ENDS that reflect the language used by patients would provide more complete longitudinal population-level surveillance of ENDS use and its association with short- and long-term health outcomes.
Keywords: Electronic nicotine delivery systems, Electronic health record, Integrated healthcare, Natural language processing, Adolescents, Clinicians, E-cigarettes, Vaping, Semantics
1. Introduction
Electronic nicotine delivery systems (ENDS), including e-cigarettes, have become increasingly popular since entering the US market in 2007 (Singh et al., 2016; King et al., 2015). While there is some evidence that ENDS may be safer nicotine delivery products than combustible cigarettes (Farsalinos and Polosa, 2014; McRobbie et al., 2014; Farsalinos et al., 2016; Nolan et al., 2016) and may help some people quit smoking (Hartmann-Boyce et al., 2016), their long-term safety and potential for harm and harm reduction are unknown. To be able to assess the long-term population health effects associated with ENDS use, researchers need the means to accurately identify the incidence and prevalence of ENDS use across the lifespan.
ENDS surveillance is limited in that many nationally representative surveys are conducted infrequently with a substantial lag between time of data collection and publication of results (Ayers et al., 2016). Tracking ENDS use through routine documentation within healthcare visits could yield important surveillance data for studying population-level harm and harm reduction effects. National guidelines strongly recommend that tobacco screening in healthcare settings be expanded to include ENDS questions as part of standard health examinations (American Heart Association, 2016; The American Academy of Pediatrics Issues Sweeping Recommendations on Tobacco and E-Cigarettes, 2015), and healthcare providers are increasingly discussing ENDS use with patients (Nickels et al., 2016; Steinberg et al., 2015; Brown-Johnson et al., 2016). Routine clinician screening and documentation of ENDS use in the EHR could be linked to other healthcare data for retrospective and prospective analyses essential to assessing ENDS’ safety and harm reduction effectiveness.
Currently, healthcare system surveillance of ENDS is limited because few healthcare systems have discrete EHR fields for ENDS documentation, clinicians receive little training on ENDS screening, and in general, clinicians inconsistently document use in free-text comment fields (Winden et al., 2015). Qualitative research has demonstrated differences in ENDS terminology by consumer age group and product type, suggesting that screening questions should reflect the range of terms used by patients (Alexander et al., 2016). These challenges currently limit the ability of healthcare systems to systematically screen for, detect, and monitor this key emerging health behavior.
To better guide the development of ENDS surveillance in healthcare systems, we sought to: 1) describe trends in how clinicians document ENDS use in the free-text comments of the EHR in a large integrated healthcare system from 2006 to 2015, stratified by patient age, and 2) compare the terms used to document ENDS use among adolescents and adults.
2. Methods
2.1. Data source
Data were gathered from medical visits with patients aged 12 and older within Kaiser Permanente Northern California (KPNC) between 2006 and 2015. KPNC is a nonprofit healthcare delivery system serving 4 million members. KPNC provides integrated medical and behavioral health treatment to a racially and socioeconomically diverse patient population that is representative of the geographic catchment area (Gordon, 2006). To construct our sample, we identified KPNC members with any text in the tobacco comments section of the EHR from 2006 to 2015.
2.2. Measures
Using natural language processing, we identified provider documentation of ENDS use in the tobacco comments field of the social history section of the KPNC EHR (i.e., free-text comment fields unrelated to tobacco were not included). We created a list of specific keywords appearing within free text fields that refer to ENDS, such as “e-cig”, “electronic”, or “vape” that was informed by commonly used terms in previous ENDS research (Pearson et al., 2017; Cole-Lewis et al., 2015; Myslin et al., 2013), and used the SAS INDEX function (substring match) in an iterative process to identify all variations of these keywords. When we identified a matching text string, we isolated the entire word or candidate text in which the string was embedded. When new potential text strings were found, the full comments were manually reviewed for inclusion, alternative candidate strings, and exclusionary criteria (Appendix A). We only included keywords that referenced ENDS use (e.g., ‘electronic cigarette’ but not ‘electronic signature’). We included the first (earliest) documented reference to ENDS use for each individual in our analyses to estimate the number of new documented ENDS users each year. We extracted patient sex, race/ethnicity, age and smoking status (current, former, and never smoker) at the earliest record of documented ENDS use, as well as the department where ENDS was documented, from the EHR.
2.3. Analysis
Analyses were performed using SAS© software, version 9.3. We first calculated the annual incidence rate of ENDS use documentation in the EHR (number of newly documented users per 10,000 patients) annually from 2006 to 2015. Next, we fitted Poisson regression models to analyze incidence rates as a function of sex, race/ethnicity, and year, stratified by age group. To calculate the annual percent change in incidence rates and 95% confidence intervals, we exponentiated model coefficients for each year (compared to the previous year), producing adjusted rate ratios. We then plotted annual incidence rates by age to visualize the relative rate increases across different age groups. Finally, we described the cumulative frequencies of distinct keywords during the study period and used chi-square tests to examine differences by age group.
3. Results
After removing duplicate comments, we identified 3,049,457 comments in the tobacco comments field of the EHR between 2006 and 2015. Of these, 16,915 comments (0.55%) contained mentions of ENDS use (Appendix A). After selecting the first comment documenting ENDS use for each patient, the final sample consisted of 9119 unique patients aged 12 and older.
The sample was 55% male; 67% White, 12% Asian/Hawaiian/Pacific Islander, 10% Hispanic, 6% African American, and 5% Other. The median neighborhood income of the sample was $69,000 (IQR = $36,039); 80% had only a commercial plan, 5% had only Medicaid, 1% had only Medicare, and 14% had more than one type of insurance.
At the time of first documented ENDS use, 1% were aged 12–17, 15% were 18–24, 43% were 25–44, 33% were 45–64 and 8% were > 65; 57% were current smokers, 35% were former smokers, and 8% were never smokers. Compared to the general KPNC population, patients with documented ENDS use were more likely to be male, White, aged 18–44, and current smokers. For patients aged 12–17, ENDS documentation occurred in pediatrics (44%), internal medicine (32%), obstetrics/gynecology (8%), specialty care (14%) and anesthesia (2%). For patients 18 years and older, ENDS documentation occurred in internal medicine (67%), specialty care (16%), obstetrics/gynecology (9%), anesthesia (3%), surgery or transplant (2%), emergency department (2%) and hospital (1%).
The rate of incident documented ENDS use increased exponentially from 2006 to 2015, from 0.01 newly documented users/10,000 patients in 2006 to 9.5 newly documented users/10,000 patients in 2015. Incidence rates at each time point were consistently higher among patients aged 18–24 and 25–65 relative to those aged 12–17 or > 65 (Fig. 1). Using Poisson multivariable regression, we found the largest annual increases occurred from 2011 to 2012 and 2012–2013 for all age groups. Adjusting for annual changes in race and sex distributions, the rate of incident documented ENDS use increased seven-fold (adjusted RR = 6.93, 95%CI = 6.36–7.55) among patients aged 12–17 from 2011 to 2012, six-fold (adjusted RR = 5.93, 95%CI = 5.87–6.00) among patients aged 18–24, and five-fold (adjusted RR = 4.99, 95%CI = 4.96–5.02) among patients aged 25–44 from 2012 to 2013 (ps < 0.0001). From 2014 to 2015, the incidence of ENDS use increased moderately among patients aged 12–17 (adjusted RR = 1.22, 95%CI = 1.20–1.24) and 18–24 (adjusted RR = 1.11, 95%CI = 1.11–1.12), while ENDS incidence declined for all other age groups (ps < 0.0001).
Fig. 1.
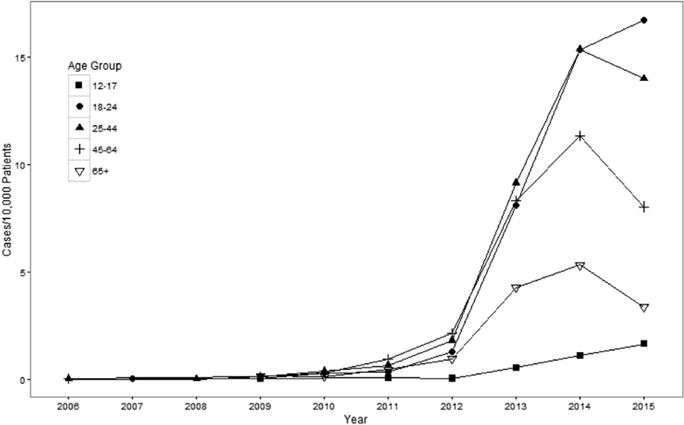
Annual Unadjusted Incidence Rate of ENDS Use Documentation by Patient Age Group, Kaiser Permanente Northern California, 2006–2015.
Notes (Singh et al., 2016). All rate ratios were significant at p < 0.0001 except for the rate changes from 2010 to 2011 and 2014–2015 among 18–24 year olds, the change from 2009–2010 among those ages 65+, and the change from 2006–2008 among patients ages 25–44. (King et al., 2015) The crude rate ratio for an age group can be calculated by dividing the rate in one year (e.g., 2015) by the rate in the previous year (2014). However, reported rate ratios in the text were calculated with adjustment for race and sex, resulting in different estimates for certain time points.
The most common keywords used to document ENDS use were variants of “e-cig” (49%), “electronic cigarette” (25%), and “vape” (28%) (Table 1). About half of the documented comments for patients aged 25 and older included “e-cig”, compared to 42% among 12–17 year olds. Patients aged > 65 were more likely to have documented use of “electronic cigarettes” (37%) than those aged 45–64 (28%), 25–44 (22%), 18–24 (18%), and 12–17 (6%). Adolescents were more likely than adults to have variations of “vape” in their comments, with 50% of comments for 12–17 year olds including the word “vape,” compared to only 37%, 31%, 23%, and 15% of patients aged 18–24, 25–44, 45–64, and > 65, respectively. “Pen” was also more commonly referenced in comments among 12–17 and 18–24 year olds, with 10% and 7%, respectively, of comments containing this term, compared to 1% of comments among those > 65 (ps < 0.05).
Table 1.
Short-hand text strings used to describe ENDS use by patient age group, Kaiser Permanente Northern California, 2006–2015.*
| Category | Short-hand text strings | Age group, in years
|
p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| 12–17 (N = 95) n (%) |
18–24 (N = 1347) n (%) |
25–44 (N = 3905) n (%) |
45–64 (N = 3012) n (%) |
65+ (N = 758) n (%) |
Overall (N = 9117) n (%) |
|||
| E-cigarette | ‘ecig’ ‘e cig’ ‘e-cig’ |
40 (42.1) | 622 (46.2) | 1926 (49.3) | 1529 (50.8) | 381 (50.3) | 4498 (49.3) | 0.039 |
| Vape | ‘vappen’ ‘vap’ ‘vait’ ‘vapo’ ‘vape’ ‘vaping’ |
47 (49.5) | 503 (37.3) | 1211 (31.0) | 677 (22.5) | 114 (15.0) | 2552 (28.0) | < 0.0001 |
| Electronic cigarette | ‘lectric’ ‘tronic’ ‘ectron’ ‘elect’ ‘ctonic’ |
6 (6.32) | 240 (17.8) | 858 (22.0) | 852 (28.3) | 278 (36.7) | 2234 (24.5) | < 0.0001 |
| Pen | ‘pen’ ‘-pen’ ‘epen’ ‘e pen’ |
9 (9.47) | 87 (6.46) | 165 (4.23) | 74 (2.46) | 8 (1.06) | 343 (3.76) | < 0.0001 |
| Smokeless cigarette | ‘smokeless cig’ ‘smokes smokeless tobac’ ‘nicotine smokeless cig’ ‘smokeless nicotene cigs’ ‘smokeless nicotine cigs’ ‘smokeless inhaled nicotene’ ‘smokeless eletroinic cig’ ‘puffs of smokeless tob’ |
0 | 7 (0.52) | 12 (0.31) | 22 (0.73) | 1 (0.13) | 42 (0.46) | 0.078* |
| Liquid cigarette | ‘liquid’ ‘liqid cigarette’ |
0 | 0 | 12 (0.31) | 5 (0.17) | 0 | 17 (0.19) | 0.149* |
| E-smoke | ‘e smoke’ ‘e-smoke’ ‘esmoke’ |
1 (1.05) | 1 (0.07) | 3 (0.08) | 7 (0.23) | 0 | 12 (0.13) | 0.075* |
| Digital cigarette | ‘digi’ | 0 | 0 | 4 (0.10) | 4 (0.13) | 0 | 8 (0.09) | 0.669* |
| E-hookah | ‘ehooka’ ‘e-hooka’ ‘ehouka’ ‘e-houka’ ‘ehucca’ ‘e-hucca’ ‘ehoka’ ‘e-hoka’ ‘ehuka’ ‘e-huka’ |
0 | 1 (0.07) | 0 | 0 | 0 | 1 (0.01) | 0.241* |
Notes. Multiple strings may be contained in the same comment for an individual.
p-Values calculated using Fisher’s Exact test to account for sparse sample sizes.
Certain keyword text strings were more likely than others to occur in the same comment. In 9119 comments, “vape” and “pen” co-occurred 296 times; “e-cig” and “vape” 156 times; “electronic” and “vape” 60 times, and “e-cig” and “electronic” 18 times. No other strings co-occurred > 10 times.
4. Discussion
This study is novel in its examination of clinicians’ documentation of adolescent and adult ENDS use in the EHR. Incidence rates of documented ENDS use have increased dramatically over the past decade, particularly for young adults, confirming the need to standardize ENDS use screening in healthcare settings. Reliable EHR documentation would provide longitudinal population-level data useful for ENDS surveillance linkable to other EHR health information for examining associated short- and long-term health outcomes.
We observed exponential increases in ENDS use documentation from 2006 to 2015, mirroring increased prevalence of ENDS use in the US over this period (Singh et al., 2016; King et al., 2015). Further, our sample of patients documented with ENDS use had a smoking prevalence reflective of national surveillance data: 57% were current smokers, 35% were former smokers, and 8% were never smokers, while national data indicate that among adult e-cigarette users, 59% were current smokers, 30% were former smokers, and 11% were never smokers (QuickStats, 2016). Despite this relative increase and comparability in our sample characteristics, our findings indicate that in absolute terms, a minority of ENDS use is being documented in the healthcare system, and the actual incidence of patients’ ENDS use is grossly underestimated. To help close this gap, healthcare systems must provide clinicians across disciplines with training on screening for ENDS use (e.g., to ensure that they know the differences between ENDS and cigarettes) and develop and incorporate automated EHR prompts with discrete screening questions and documentation fields in the EHR so that clinicians can document patients’ ENDS use in routine practice. Further, discrete ENDS EHR fields could trigger patient-provider discussions about ENDS use, and help clinicians to effectively target patients for evidence-based tobacco cessation interventions as we learn more about the potential of ENDS for harm and harm reduction.
Notably, while rates of incident ENDS use documentation peaked in 2014 for adults aged 25 and older, they continued to increase in 2015 for adolescents and young adults. The increase may be attributable to increased ENDS uptake, and indeed, national data indicate that rates of ENDS use have surpassed rates of tobacco smoking among youth (Singh et al., 2016). The continued increase may also reflect greater awareness and inquiry among pediatric and adolescent medicine providers as a result of recent guideline recommendations and an increase in patient-initiated conversations (Pepper et al., 2015). Additional research is needed to disentangle these effects. Notably, there was substantial variabililty in documented ENDS use across departments and less than half of ENDS documentation occurred in pediatrics among patients aged 12–17. Given emerging evidence that ENDS use may serve as a gateway to tobacco smoking among youth (Chatterjee et al., 2016), routine documentation in pediatrics, in particular, would allow for a more thorough assessment of the longitudinal impact of ENDS use on changes in smoking status and health.
ENDS use is a complex and dynamically evolving behavior and its definition requires careful characterization. Our study, with its qualitative text analysis, highlights the need for EHR screening questions to be age-appropriate and reflect the current terminology used by consumers (Alexander et al., 2016). Adolescent and young adult records were more likely to include the words “vape” and “pen”, and less likely to include the words “e-cig” and “electronic cigarette” than adult records. Findings are consistent with recent qualitative data on ENDS suggesting that young adults are more likely than adults to correctly use the term “vapor” rather than smoke, perhaps reflecting targeted advertising to this population (Alexander et al., 2016). Moreover, recent evidence from ENDS “Google searches” in the US indicates that searches are shifting from e-cigarette to vaping-focused terms (Ayers et al., 2016). Healthcare providers should use inclusive language when screening patients for ENDS use, for example, “Do you currently use any type of e-cigarette or vaping device?” Further, they must characterize other aspects of ENDS use, including frequency of use, product design (e.g., closed vs open systems, nicotine containing versus non-nicotine containing products), product flavoring, and use with other substances (e.g., cannabis).
As healthcare systems strive to improve patient outcomes, consistent precise methods to capture behavioral health data can help reduce individual and population health risks. National data suggest that the majority of US physicians are discussing ENDS with their patients who smoke cigarettes (Nickels et al., 2016), and EHR modifications to include discrete fields for the capture of ENDS will be important to identify associated short- and long-term health outcomes and to evaluate associated transitions in the use of combustible tobacco products (i.e., initiation, relapse, quitting). However, healthcare systems have several challenges to consider, including EHR customization cost, shifting terminology, and clinician training and concerns regarding data entry burden and integration of screening into existing clinical workflows. Automated EHR prompts for screening for ENDS use at the same time as tobacco smoking and including ENDS screening as part of the definition of Meaningful Use (Healthit.gov, 2014) may minimize clinician burden and maximize the likelihood that ENDS screening is incorporated into routine clinical care.
This study has several limitations. Data are from one healthcare system and rates of ENDS use and documentation may not be generalizable to other healthcare systems. Details about frequency and quantity of ENDS use, the type of ENDS product, the concentration of nicotine in the product, and reasons for ENDS use were not available in the EHR. This study only captures clinician documentation of patients’ ENDS use and there is the possibility that conversations about patients’ use of ENDS occurred and were not documented. Further, results reflect how the documented incidence of ENDS use has changed over time, rather than the true incidence of ENDS use. Finally, though we observed notable differences in ENDS terminology by patient age group, we cannot be certain that the data reflect the patients’ own language versus the clinicians’ translation of the conversation.
Supplementary Material
Acknowledgments
This study was funded by a Kaiser Permanente Delivery Science Rapid Analysis Program Grant and a grant from the Tobacco-Related Disease Research Program (24XT-0008).
Dr. Prochaska’s tobacco-related research is funded by the National Cancer Institute (R01CA204356), the National Heart, Lung, and Blood Institute (R01HL117736), and the State of California Tobacco-Related Disease Research Program (24RT-0035 and 25IR-0032). She has consulted to Pfizer, which makes smoking cessation medications, and has been an expert witness for plaintiffs’ counsel in court cases against tobacco companies.
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ypmed.2017.08.009.
Footnotes
All other authors declare no conflict of interest.
References
- Alexander JP, Coleman BN, Johnson SE, Tessman GK, Tworek C, Dickinson DM. Smoke and vapor: exploring the terminology landscape among electronic cigarette users. Tob Regul Sci. 2016;2(3):204–213. doi: 10.18001/TRS.2.3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Heart Association. FACTS: E-cigarettes and Public Health: The Next Generation of Cigarettes. Washington DC: 2016. [Google Scholar]
- Ayers JW, Althouse BM, Allem JP, Leas EC, Dredze M, Williams RS. Revisiting the rise of electronic nicotine delivery systems using search query surveillance. Am J Prev Med. 2016;50(6):e173–181. doi: 10.1016/j.amepre.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown-Johnson CG, Burbank A, Daza EJ, et al. Online patient-provider e-cigarette consultations: perceptions of safety and harm. Am J Prev Med. 2016;51(6):882–889. doi: 10.1016/j.amepre.2016.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee K, Alzghoul B, Innabi A, Meena N. Is vaping a gateway to smoking: a review of the longitudinal studies. Int J Adolesc Med Health. 2016 doi: 10.1515/ijamh-2016-0033. [DOI] [PubMed] [Google Scholar]
- Cole-Lewis H, Pugatch J, Sanders A, et al. Social listening: a content analysis of E-cigarette discussions on twitter. J Med Internet Res. 2015;17(10):e243. doi: 10.2196/jmir.4969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Ther Adv Drug Saf. 2014;5(2):67–86. doi: 10.1177/2042098614524430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos K, Cibella F, Caponnetto P, et al. Effect of continuous smoking reduction and abstinence on blood pressure and heart rate in smokers switching to electronic cigarettes. Intern Emerg Med. 2016;11(1):85–94. doi: 10.1007/s11739-015-1361-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon NP. How does the Adult Kaiser Permanente Membership in Northern California compare with the larger community? Kaiser Permanente Member Health Survey. 2006 https://pdfs.semanticscholar.org/2c62/b108b3bddcaca5f79b3af0daea8a91d358ac.pdf?_ga=2.119037577.1815730576.1498011998-1842743218.1498011998.
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216. doi: 10.1002/14651858.CD010216.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthit.gov. Step 5: achieve meaningful use stage 1. 2014 https://www.healthit.gov/providers-professionals/achieve-meaningful-use/core-measures/record-smoking-status.
- King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010–2013. Nicotine Tob Res. 2015;17(2):219–227. doi: 10.1093/ntr/ntu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev. 2014;12:CD010216. doi: 10.1002/14651858.CD010216.pub2. [DOI] [PubMed] [Google Scholar]
- Myslin M, Zhu SH, Chapman W, Conway M. Using twitter to examine smoking behavior and perceptions of emerging tobacco products. J Med Internet Res. 2013;15(8):e174. doi: 10.2196/jmir.2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickels AS, Warner DO, Jenkins SM, Tilburt J, Hays JT. Beliefs, practices, and self-efficacy of US physicians regarding smoking cessation and electronic cigarettes: a National Survey. Nicotine Tob Res. 2016 doi: 10.1093/ntr/ntw194. [DOI] [PubMed] [Google Scholar]
- Nolan M, Leischow S, Croghan I, et al. Feasibility of electronic nicotine delivery systems in surgical patients. Nicotine Tob Res. 2016;18(8):1757–1762. doi: 10.1093/ntr/ntw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JL, Amato MS, Wang X, et al. How US smokers refer to E-cigarettes: an examination of user-generated posts from a web-based smoking cessation intervention, 2008–2015. Nicotine Tob Res. 2017;19(2):253–257. doi: 10.1093/ntr/ntw206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper JK, Gilkey MB, Brewer NT. Physicians’ counseling of adolescents regarding e-cigarette use. J Adolesc Health. 2015;57(6):580–586. doi: 10.1016/j.jadohealth.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QuickStats. Cigarette smoking status* among current adult E-cigarette users, dagger by age group - National Health Interview Survey, section sign United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(42):1177. doi: 10.15585/mmwr.mm6542a7. [DOI] [PubMed] [Google Scholar]
- Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students - United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65(14):361–367. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- Steinberg MB, Giovenco DP, Delnevo CD. Patient-physician communication regarding electronic cigarettes. Prev Med Rep. 2015;2:96–98. doi: 10.1016/j.pmedr.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American Academy of Pediatrics Issues Sweeping Recommendations on Tobacco and E-Cigarettes. Washington DC: press release. 10/26/2015. [Google Scholar]
- Winden TJ, Chen ES, Wang Y, Sarkar IN, Carter EW, Melton GB. Towards the standardized documentation of e-cigarette use in the electronic health record for population health surveillance and research. AMIA Jt Summits Transl Sci Proc, 2015. 2015:199–203. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


