Abstract
Background
Lung transplantation is a life-saving procedure in patients with end-stage lung disease, and is increasingly performed in Korea.
Methods
We retrospectively evaluated the outcomes of patients who received a lung transplant at Asan Medical Center between January 2008 and December 2016. Thirteen of 54 patients experienced multiorgan transplantation; the remaining 41 who received only lung grafts were included.
Results
The mean age of the lung transplant recipients was 44.6 years; 27 were men and 14 were women. The most frequent reasons were idiopathic interstitial pneumonia (21 of 41 patients, 51.2%), interstitial lung disease (9 of 41, 22.0%), and bronchiolitis obliterans after bone marrow transplantation (7 of 41, 17.1%). The median waiting time was 47 days, and many patients received preoperative intensive care (27 of 41, 65.9%), ventilator support (26 of 41, 63.4%), or extracorporeal life support (19 of 41, 46.3%). All 41 patients received bilateral lung grafts. Ten deaths occurred (24.3%), including 5 cases of early mortality (12.2%) and 5 cases of late mortality (12.2%). The 1-, 3-, and 5-year survival rates were 78.9%, 74.2%, and 69.3%, respectively.
Conclusion
Despite a high percentage of patients who required preoperative intensive care, the transplantation outcomes were acceptable.
Keywords: Lung transplantation, Extracorporeal membrane oxygenation (ECMO), Survival
Introduction
Lung transplantation is indicated for a number of end-stage lung diseases. The International Society for Heart and Lung Transplantation (ISHLT) reports that the number of procedures performed in 253 centers across the world has increased from 1,934 cases in 2003 to 4,080 in 2014 [1]. The first lung transplant was performed in Korea in 1996 [2], and 89 were performed in 2016. The lung transplantation survival rates in Korea are lower than those reported by the ISHLT [1,3], possibly because of differences in the lung allocation score (LAS). The LAS criteria of the Korean Network for Organ Sharing (KONOS) are based on emergency status. We believe that transplant recipients in Korea are likely to require preoperative ventilator support and extracorporeal membrane oxygenation (ECMO), but data on transplant recipients and outcomes are limited. The few relevant studies that reviewed the results of lung transplantation procedures primarily included procedures performed before 2010 [2,4,5]. In this study, we reviewed the preoperative status, including the severity of the patients’ condition, and postoperative outcomes of lung transplant recipients at Asan Medical Center (AMC).
Methods
The records of the 54 patients who underwent lung transplantation at AMC between January 2008 and December 2016 were reviewed. These included 11 cases of heart-lung transplantation, 1 lung-liver transplantation, and 1 heart-lung-liver transplantation. The outcomes of the 11 heart-lung transplantation patients have been previously reported [6]. This study evaluated the 41 patients who only underwent lung transplantation. Potential lung transplant recipients were evaluated by a transplantation committee composed of a pulmonologist, intensivist, cardiothoracic surgeon, anesthesiologist, radiologist, and infectious disease specialist. Preoperative management was determined by recipient lung status. Oxygen was supplied by nasal cannulae, and ventilator support or ECMO was provided as necessary. When a potential donor became available, the donor evaluation committee, consisting of a cardiothoracic surgeon, pulmonologist, and coordinator, reviewed the donor characteristics and decided whether to perform or abandon the transplantation. Transplantation was performed with cardiopulmonary bypass (CPB) and the assistance of a cardiac surgeon. Following transplantation, the patients were transferred to the intensive care unit (ICU) under the care of a pulmonologist and intensivist. When sufficiently recovered, patients were transferred to the general ward and then discharged, and routine follow-up with a pulmonologist was scheduled. The pretransplant diagnosis, age, sex, number of days of preoperative hospitalization including days in the ICU, preoperative ECMO, and ventilator support were retrieved from patient records. Procedure-related variables included duration of surgery, time on CPB, and cold and warm ischemia times. The postoperative outcomes included overall mortality, early mortality within 30 days, late mortality (more than 30 days after transplantation), and transplantation-associated complications that occurred during hospitalization. Values of continuous variables were expressed as means±standard deviation or medians. Survival was analyzed by the Kaplan-Meier method. Statistical analysis was performed using PASW SPSS Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Results
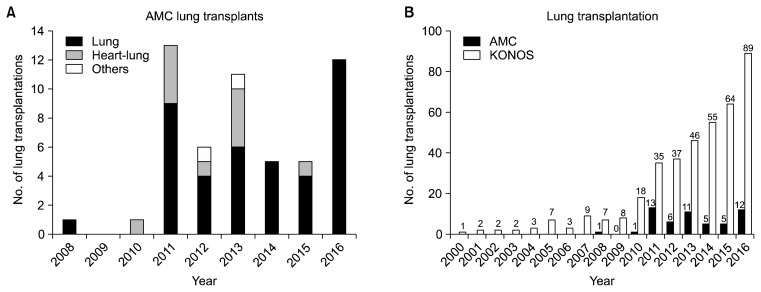
Forty-one patients underwent lung transplantation at AMC between 2008 and 2016 (Fig. 1A). The total number of lung transplants in Korea is shown in Fig. 1B. The first transplant at AMC was performed in October 2008 and the second in 2010. Nine were performed in 2011, including 3 because of humidifier disinfectant-associated lung disease. Twelve transplants were performed in 2016. The recipients included 27 men (65.9%) and 14 women (34.1%) with a mean age of 44.6±16.1 years (range, 6 to 74 years). The lung disease diagnoses of the transplantation recipients are shown in Table 1, and followed the primary diagnostic indications for adult lung transplantation proposed in the 2016 ISHLT heart-lung transplant report [1]. Of the 21 idiopathic interstitial pneumonia (IIP) patients, 17 (41.5%) had idiopathic pulmonary fibrosis, 1 (2.4%) had nonspecific interstitial pneumonia, 1 (2.4%) had typical interstitial pneumonitis, 1 (2.4%) had cryptogenic organizing pneumonia, and 1 (2.4%) had cellular interstitial pneumonitis. Of the 9 interstitial lung disease (ILD) patients without IIP, 3 (7.3%) had acute respiratory distress syndrome (ARDS) because of exposure to toxic chemicals, 3 (7.3%) had ARDS because of infection, 1 (2.4%) had drowning-related ARDS, 1 (2.4%) had ILD, and 1 (2.4%) had pneumoconiosis. The preoperative status of the patients is shown in Table 2. Thirty-two patients (78.0%) were hospitalized before transplantation, 27 of whom (65.9%) spent time in the ICU, 19 (46.3%) received preoperative ECMO support, 26 (63.4%) received ventilator support, and 1 (2.4%) received high-flow oxygen therapy. Lung allocation was based on the Korean LAS criteria shown in Table 3. The median waiting time was 47 days (range, 1 to 386 days). One patient was an outlier with a waiting time of 1,513 days after KONOS registration. Between admission and transplantation, the LAS of 20 patients (48.8%) changed, increasing in 19 (46.3%) and decreasing in one (2.4%) (Table 4); 5 patients (12.2%) experienced more than 1 change in status. Transplantation was performed in 27 patients (65.9%) with a LAS status of 0, 11 (26.8%) with a status of 1, 2 (4.9%) with a status of 2, and 1 (2.4%) with a status of 3. In patients with a change of status, the median waiting time decreased to 17 days and the longest wait decreased to 386 days. The ranges by status were 1–78, 1–180, 1–316, and 1–386 days, respectively. All 41 patients underwent bilateral lung transplantation with CPB support. The average procedure was 611.5±102 minutes, with an average total ischemia time of 254.5±68.1 minutes, warm ischemia time of 148.2±31.5 minutes, cold ischemia time of 105.7±46.4 minutes, and total pump time of 253.2± 61.1 minutes. All patients were intubated and transferred to the ICU after surgery. The duration of the postoperative ICU stay, ventilator support, and hospital stay are shown in Table 5. Two patients received ECMO support, for which they were kept in the ICU for 3 and 11 days, respectively.
Fig. 1.
(A) Number of lung transplantations performed at AMC between 2008 and 2016. The number of lung transplantations performed each year between 2000 and 2016 at AMC is shown in blue. The number of transplantations, including single lung transplantations and multiple organ transplantations, performed in the AMC is also shown. Other transplantations included 1 lung-liver transplantation and 1 heart-lung-liver transplantation. (B) Number of lung transplantations performed in Korea between 2000 and 2016. The number of lung transplantations performed each year between 2000 and 2016, according to the KONOS, is shown. The blue bars show the lung transplantations performed at AMC. AMC, Asan Medical Center; KONOS, Korean Network for Organ Sharing.
Table 1.
Diagnosis of lung transplantation recipients
| Diagnosis | No. of patients (%) |
|---|---|
| IIP | 21 (51.2) |
| Interstitial lung disease, non-IIP | 9 (22.0) |
| Bronchiolitis obliterans | 7 (17.1) |
| Cystic fibrosis | 1 (2.4) |
| Dermatomyositis | 1 (2.4) |
| Lymphangioleiomyomatosis | 1 (2.4) |
| Portopulmonary hypertension | 1 (2.4) |
| Total | 41 (100.0) |
Diagnosis of lung transplant recipients followed the International Society for Heart and Lung Transplantationcriteria. IIP was the most common reason for lung transplantation at Asan Medical Center.
IIP, idiopathic interstitial pneumonia.
Table 2.
Preoperative status of lung transplantation recipients
| Variable | No. of patients (%) | Median (range), day |
|---|---|---|
| Preoperative hospitalization | 32 (78.0) | 25 (1–71) |
| Preoperative ICU care | 27 (65.9) | 20 (1–60) |
| Preoperative ventilator | 26 (63.4) | 15 (1–60) |
| Preoperative ECMO | 19 (46.3) | 14 (1–36) |
Patients on ventilator or ECMO support were kept in the ICU.
ICU, intensive care unit; ECMO, extracorporeal membrane oxygenation.
Table 3.
Korean lung allocation score
| Category | Indications |
|---|---|
| Status 0 | Patient is connected to a ventilator or an extracorporeal membrane oxygenation |
| Status 1 | NYHA stage IV patients with PaO2 of <55 mm Hg on room air |
| NYHA stage IV patients with an average pulmonary pressure of >65 mm Hg or an average right atrial pressure of >15 mm Hg | |
| Cardiac index <2 L/min/m2 | |
| Status 2 | Forced expiratory volume in 1 second <25% on pulmonary function test |
| PaO2 <60 mm Hg on room air | |
| Average right atrial pressure: 10–15 mm Hg | |
| Average pulmonary pressure: 55–65 mm Hg | |
| Cardiac index: 2–2.5 L/min/m2 |
Korean lung allocation score provided by Korean Network for Organ Sharing. Lungs are allocated by the emergency status of the recipient. The survival probability of the recipient is not considered.
NYHA, New York Heart Association.
Table 4.
Pretransplant status of recipients based on the Korean lung allocation score criteriaat the initial KONOS registration
| Category | Initial | Status at the point of transplantation |
|---|---|---|
| Status 0 | 14 (34.1) | 27 (65.9) |
| Status 1 | 8 (19.5) | 11 (26.8) |
| Status 2 | 5 (12.2) | 2 (4.9) |
| Status 3 | 14 (34.1) | 1 (2.4) |
Values are presented as number (%). The number of recipients included in the evaluation was determined by status. At the initial KONOS registration, the numbers of status 0 and status 3 patients were equal. The distribution changed by the time of transplantation, when the majority of the patients were status 0. In the interim, 20 patients changed status, including 19 in whom the status deteriorated.
KONOS, Korean Network for Organ Sharing.
Table 5.
Immediate postoperative results of lung transplant recipients
| Postoperative care | Median (range, outliers), day |
|---|---|
| Postoperative ventilator usage | 7 (2–24, 200, 1,102) |
| Postoperative intensive care unit stay | 13 (3–64, 306, 1,102) |
| Postoperative hospitalization | 59 (3–347, 1,102) |
Immediate postoperative complications included postoperative bleeding in 5 patients (12.2%), 2 of whom (4.9%) underwent surgery to control the bleeding. Three (7.3%) died of uncontrolled bleeding. Twelve patients (26.8%) were kept in the ICU for more than 3 weeks (Table 6). The most frequent reason was failure to wean from ventilator support in 8 patients (19.5%). Thirteen patients (31.7%) were hospitalized for more than 90 days; the median duration was 194 days (range, 93 to 347 days), with 1 outlier stay of 1,102 days. The primary complications of patients requiring long-term hospitalization were infection, failure to wean from mechanical ventilation, and airway problems (Table 7).
Table 6.
Major postoperative complications of patients needing long-term ICU care
| Complication | No. of patients (%) |
|---|---|
| Ventilator weaning failure | 8 (19.5) |
| Gastrointestinal problems (bleeding, ischemia, and ileus) | 3 (7.3) |
| Kidney problems (acute kidney injury and chronic kidney disease) | 3 (7.3) |
| Pneumonia (carbapenem-resistant Acinetobacter baumannii) | 2 (4.9) |
| Brain hemorrhage (subdural hemorrhage and intracranial hemorrhage) | 2 (4.9) |
| Cardiac problem | 2 (4.9) |
| Deep vein thrombosis | 1 (2.4) |
This table summarizes the major complications that occurredin 12 patients who received more than 3 weeks of ICU care. All major complications were counted. Different complications that occurred in a single patient were counted.
ICU, intensive care unit.
Table 7.
Major postoperative complications of patients needing long-term hospitalization
| Complication | No. of patients (%) |
|---|---|
| Infection | 4 (9.8) |
| Failure to wean from bilevel positive airway pressure | 4 (9.8) |
| Airway stenosis | 4 (9.8) |
| Hematologic problems (pancytopenia and thrombocytopenia) | 3 (7.3) |
| Chronic kidney disease | 3 (7.3) |
| Physical weakness (for rehab) | 2 (4.9) |
| Pneumonia | 2 (4.9) |
| Right ventricular outflow tract obstruction | 1 (2.4) |
| Heart failure | 1 (2.4) |
| Ocular ischemic syndrome | 1 (2.4) |
| Bowel infarction | 1 (2.4) |
This table summarizes the major complications that occurred in the 13 patients who were hospitalized for more than 90 days. All major complications were counted. Different complications that occurred in a single patient were counted separately.
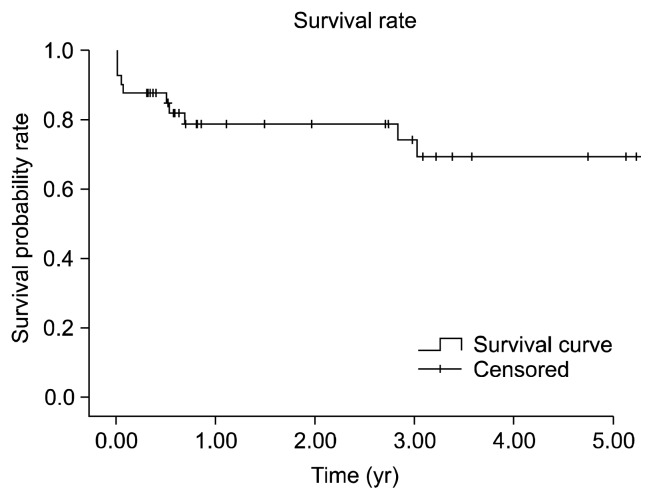
The average follow-up period was 2.21 years (range, 3 days to 6.05 years). Ten patients (24.4%) died during follow-up (Table 8). There were 5 cases of early mortality (12.2%). Three patients (7.3%) died of early, uncontrollable postoperative bleeding with ICU care, and 2 more patients died of carbapenem-resistant Acinetobacter baumannii pneumonia. There were 5 cases of late mortality ( 12.2%): 3 (7.3%) of pneumonia, 1 (2.4%) of invasive fungal sinusitis, and 1 (2.4%) of candidemia. The cumulative survival, estimated by the Kaplan-Meier curve shown in Fig. 2, was 78.9% at 1 year, 74.2% at 3 years, and 69.3% at 5 years. The survival of patients with either ventilator support or ECMO was 79.9% at 1 year, 71.9% at 3 years, and 63.9% at 5 years. Twenty-three patients survived for more than 1 year postoperatively; 2 of these 23 patients had grade >2 bronchiolitis obliterans syndrome/restrictive allograft syndrome (BOS/RAS).
Table 8.
Early and late mortality and causes of death in the study population
| Cause of death | No. of mortality (%) | Postoperative day of death |
|---|---|---|
| Early mortality (within 30 days of transplantation) | ||
| Surgical failure | 3 (7.3) | 3, 3, 3 |
| Carbapenem-resistant Acinetobacter baumannii pneumonia | 2 (4.9) | 17, 24 |
| Late mortality (after 30 days of transplantation) | ||
| Pneumonia | 3 (7.3) | 185, 194, 250 |
| Invasive fungal sinusitis | 1 (2.4) | 1,035 |
| Candidemia | 1 (2.4) | 1,102 |
| Total | 10 (24.4) | |
A total of 10 recipients died, including 5 cases of early mortality and 5 of late mortality.
Fig. 2.
Cumulative survival of lung transplant recipients at Asan Medical Center between 2008 and 2016. The 1-, 3-, and 5-year survival rates were 78.9%, 74.2%, and 69.3%, respectively.
Discussion
This retrospective review of the experience of AMC with lung transplantation found that 75.6% of the recipients were hospital inpatients before the procedure, 63.4% received preoperative ventilator support, and 46.3% received preoperative ECMO life support. The ISHLT registry data indicate that 8.4% of recipients were hospital inpatients and that only 3.2% received preoperative ventilator support. The hazard ratios for 1-year mortality among recipients with preprocedural hospitalization and ventilator support were estimated to be 1.440 and 1.239, respectively [1]. In a report describing outcomes in a large patient sample in the United States, Mason et al. [7] found that postoperative 1-year survival of patients was 62% for those with preoperative mechanical ventilation and 50% for those with ECMO, with hazard ratios of 1.49 and 2.55, respectively. In this study, the overall 1- and 3-year survival rates (78.9% and 74.2%, respectively) and those of recipients with either ventilator or ECMO support (79.9% and 71.9%, respectively) were similar. The 5-year overall survival rate (69.3%) and the 5-year survival rate of recipients with preoperative support (63.9%) were slightly different. The 1-, 3-, and 5-year survival rates of the patients at AMC were not inferior to the rates of 80%, 65 %, and 54% reported by ISHLT [ 1]. It is difficult to compare the results because of the small number of transplantations performed at AMC, but there are a number of ways to account for the differences. First, the 3 recipients of transplants in 2011 for humidifier disinfectant-induced lung disease were young and had no other underlying lung disease. As the procedures were performed to treat an acute condition, a satisfactory recovery might be expected. Second, the 1-year survival rate at AMC (78.9%) and that reported by the ISHLT (80%) are similar because of good ICU care. Although the rate of preoperative hospitalization (78.0%) and the severity of disease (65.9% received ICU care) were high, the care provided by intensivists adequately treated medically reversible diseases and produced favorable results. Finally, the incidence of BOS/RAS was low. Only 2 of the 23 patients who survived for more than 1 year after transplantation had grade 2 BOS/RAS, whereas nearly 50% of the ISHLT patients developed BOS within 5 years after transplantation [1]. This discrepancy may have resulted from differences in the Korean and ISHLT registry populations.
The average operating time was 611.5±102 minutes. Patients with a history of pleurodesis, influenza, pneumonia, and other conditions that increased the possibility of adhesions were taken to the operating room 4 hours before the estimated arrival of the donor lung to ensure sufficient time for adhesiolysis and bleeding control. The average total ischemia of 254.5±68.1 minutes and average total pump time of 253.2±61.1 minutes were both longer than has been reported in previous studies [4]. These increases might have resulted from factors specific to the transplantation procedures at AMC. Considerations of the recipient’s age, disease status, and possible adhesions prompt early arrival in the operating room for careful adhesiolysis and bleeding control. CPB was initiated approximately 1 hour before the estimated time of donor lung arrival. Bilateral pneumonectomy was performed, along with meticulous bleeding control, especially at the posterior mediastinum. The meticulous bleeding control is one of the reasons for the infrequent bleeding events and the small difference between the ischemia and the CPB times. The AMC uses CPB in all cases of lung transplantations because the severe medical condition of recipients makes it difficult to perform transplantation procedures without cardiopulmonary support or with only ECMO support. The advantages of using CPB include performing anastomoses in a clear field, the ease of detecting sources of bleeding after bilateral pneumonectomy; and the stable maintenance of vital signs during anastomosis even when the lungs and vessels are retracted. CPB does not increase the postoperative bleeding tendency. Therefore, transplantation with CPB support will continue as the standard method at AMC.
The survival rates following lung transplantation in Korea are lower than those reported by the ISHLT. The 1-, 3-, and 5-year survival rates of 55.4%, 47.6%, and 44.8%, respectively, reported by KONOS [8] may reflect differences in the Korean and the United Network for Organ Sharing (UNOS) LAS criteria. The UNOS LAS considers not only the current status of the patient but also the expected post-transplant survival probability [9]. KONOS allocates lungs based on emergency status only, as shown in Table 1 [10]. Therefore, recipients in Korea tend to be less clinically stable, which may lead to worse transplantation outcomes.
The main study limitations are the small patient sample and the short follow-up period. However, even though a high percentage of transplant recipients were hospitalized and received preoperative intensive care, the post-transplantation results were not inferior compared to international reports.
In conclusion, lung transplantation in Korea is performed in severely ill patients because of the allocation of lungs by emergency status determined by the LAS. Many recipients are hospital inpatients and may be receiving intensive care with ventilator or ECMO support. Considering these circumstances, the AMC lung transplantation outcomes were not inferior to those reported by the ISHLT.
Acknowledgments
The following members of Asan Medical Center Lung Transplantation Team contributed to data collection and participated in the discussions: Hyeong Ryul Kim and Sung Ho Jung (Department of Thoracic and Cardiovascular Surgery); Dae-Kee Choi and In-Cheol Choi (Department of Anesthesiology); Kyung-Wook Jo, Tae Sun Shim, and Sang-Bum Hong (Departments of Pulmonology and Critical Care Medicine); and Sang-Oh Lee (Department of Infectious Diseases) at University of Ulsan College of Medicine. This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-093).
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Yusen RD, Edwards LB, Dipchand AI, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-third adult lung and heart-lung transplant report-2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant. 2016;35:1170–84. doi: 10.1016/j.healun.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Haam SJ, Lee DY, Paik HC. An overview of lung transplantation in Korea. Transplant Proc. 2008;40:2620–2. doi: 10.1016/j.transproceed.2008.07.114. [DOI] [PubMed] [Google Scholar]
- 3.Korean Network for Organ Sharing. 2015 Annual report [Internet] Seoul: Korean Network for Organ Sharing; 2017. [cited 2017 Jun 21]. Available from: https://www.konos.go.kr/konosis/common/bizlogic.jsp. [Google Scholar]
- 4.Paik HC, Hwang JJ, Kim DH, Joung EK, Kim HK, Lee DY. The 10 years experience of lung transplantation. Korean J Thorac Cardiovasc Surg. 2006;39:822–7. [Google Scholar]
- 5.Paik HC. Current perspective of lung transplantation. J Korean Med Assoc. 2016;59:119–24. doi: 10.5124/jkma.2016.59.2.119. [DOI] [Google Scholar]
- 6.Yun JK, Choi SH, Park SI Asan Medical Center Heart-Lung Transplantation Team. Clinical outcomes of heart-lung transplantation: review of 10 single-center consecutive patients. Korean J Thorac Cardiovasc Surg. 2016;49:157–64. doi: 10.5090/kjtcs.2016.49.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, Blackstone EH. Should lung transplantation be performed for patients on mechanical respiratory support?: the US experience. J Thorac Cardiovasc Surg. 2010;139:765–73.e1. doi: 10.1016/j.jtcvs.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 8.Korean Network for Organ Sharing. Transplantation statistics [Internet] Seoul: Korean Network for Organ Sharing; 2017. [cited 2017 Jun 21]. Available from: http://konos.go.kr/konosis/common/bizlogic.jsp#. [Google Scholar]
- 9.Organ Procurement and Transplantation Network. OPTN policies [Internet] Richmond (VA): Organ Procurement and Transplantation Network; 2017. [cited 2017 Jun 21]. Available from: https://optn.transplant.hrsa.gov/governance/policies/ [Google Scholar]
- 10.Korean Network for Organ Sharing. 2016 Transplantation guideline [Internet] Seoul: Korean Network for Organ Sharing; 2017. [cited 2017 Jun 21]. Available from: https://www.konos.go.kr/konosis/common/bizlogic.jsp. [Google Scholar]