Abstract
Background
Depression among patients with acute myocardial infarction (AMI) is prevalent and associated with an adverse quality of life and prognosis. Despite recommendations from some national organizations to screen for depression, it is unclear whether treatment of depression in patients with AMI is associated with better outcomes. We aimed to determine whether prognosis of patients with treated vs. untreated depression differs.
Methods
The TRIUMPH study is an observational multi-center cohort study that enrolled 4,062 patients aged ≥18 years with AMI between April 11, 2005 and December 31, 2008 from 24 US hospitals. Research coordinators administered the Patient Health Questionnaire-9 (PHQ-9) during the index AMI admission. Depression was defined by a PHQ-9 score of ≥10. Depression was categorized as ‘treated’ if there was documentation of a discharge diagnosis, medication prescribed for depression, or referral for counseling, and as ‘untreated’ if none of these three criteria were documented in the medical records despite a PHQ score ≥10. One-year mortality was compared between patients with AMI having: (1) no depression (PHQ-9 <10; reference); (2) treated depression; and (3) untreated depression adjusting for demographics, AMI severity, and clinical factors.
Results
Overall, 759 (18.7%) patients met PHQ-9 criteria for depression and 231 (30.4%) were treated. Compared with 3303 patients without depression, the 231 patients with treated depression had 1-year mortality rates that were not different (6.1% vs. 6.7%, adjusted HR=1.12, 95% CI: 0.63-1.99). In contrast, the 528 patients with untreated depression had higher 1-year mortality when compared with patients without depression (10.8% vs. 6.1%, adjusted HR=1.91, 95%CI 1.39-2.62).
Conclusions
Although depression in patients with AMI is associated with increased long-term mortality, this association may be confined to patients with untreated depression.
Keywords: depression, myocardial infarction, mortality/survival
Journal Subject Terms: mental health
Introduction
Depression has recently been classified as a risk factor for poor prognosis among patients with an acute coronary syndrome (ACS).1 Depression after acute myocardial infarction (AMI) has been associated with fatal and non-fatal cardiovascular events, adverse health status outcomes, and costs.2–5 It has also consistently been reported to be present in about a quarter of patients with ACS, underscoring the importance of concomitant depressive symptoms at the time of an AMI.6, 7 While it may seem obvious that better detection and treatment of depression would be the first step to address this problem,1, 8 negative findings from several depression intervention studies to reduce cardiovascular events,9–12 and a lack of evidence in support of improved outcomes following depression screening,13 have attenuated the enthusiasm for implementing depression screening initiatives in the ACS care setting.14
It is important, however, to realize that depression is a treatable condition and that most intervention trials conducted in cardiac patients have had success in treating patients’ depressive symptoms and improving patients’ quality of life, important goals in their own right.11, 12, 15, 16 It is unknown however, whether recognizing depression within an ACS setting, and with it, referral to treatment, would be linked with better prognostic outcomes as compared with patients whose depressive symptoms were not treated.
To fill this existing gap in the medical literature, we aimed to examine 1-year mortality rates between patients with treated vs. untreated depression, as compared with patients without depression after AMI. We addressed this question in the multi-center observational TRIUMPH registry, a large prospective AMI registry with information on depressive symptoms, patient characteristics, and AMI prognosis.
Methods
Patients and Study Design
We used data from the Translational Research Investigating Underlying disparities in acute Myocardial infarction Patients’ Health Status (TRIUMPH) study, which has been previously described.17 In brief, it is a prospective observational, 24-center AMI registry that recruited patients with AMI from diverse geographical regions throughout the US between April 11, 2005 and December 31, 2008. Inclusion criteria were age ≥18 years, having elevated cardiac enzymes (creatinine kinase-MB or Troponin-I) within 24 hours of hospital admission and an AMI diagnosis, including long-standing ischemic symptoms or electrocardiographic ST changes. Patients excluded were those who were transferred to the enrolling hospital from another facility after more than 24 hours, patients who were incarcerated, refused to participate, were not able to provide informed consent, or did not speak English or Spanish. Because this study focused upon patients’ depressive symptoms, we additionally excluded patients who had missing depressive symptom evaluations, as measured through patient interviews that included the Patient Health Questionnaire 9-item version (PHQ-9) during the index AMI admission (n=278, 6.4%). Participants underwent detailed interviews between 24-72 hours of admission, detailed chart abstractions and either in-person or telephonic follow-up at 1, 6 and 12 months after admission. Baseline interview data included patients’ socio-economic status and history of depression diagnosis and treatment and the follow-up interviews assessed post-discharge treatment, including antidepressant counselling or antidepressant medications. Interviews and medical chart abstractions were performed by trained research personnel. The local institutional review board at each participating center approved the study protocol and all participants provided written informed consent.
Depression Measures
Depressive Symptoms
Depressive Symptoms that patients were experiencing in the two weeks before the AMI were measured with the 9-item Patient Health Questionnaire (PHQ-9), a well-validated instrument in cardiac populations, including patients with AMI.7, 18–21 The PHQ-9 quantifies the degree to which patients are having depressive symptoms by scoring the DSM-IV criteria underlying a major depressive syndrome. Scores on individual items range from “0” (not at all) to “3” (nearly every day). Overall scores can range from 0 to 27, and a score ≥10 is considered predictive of a clinical diagnosis of a major depressive episode with a sensitivity and specificity of 88%.20
Depression Recognition
Depression Recognition was captured through documentation found in physician notes, discharge diagnoses, discharge medications (documentation of antidepressant use or prescription), and discharge summaries that would indicate that patients had been diagnosed, treated or referred for counseling during the index AMI hospitalization. Indications for the prescription of antidepressants were reviewed, and in cases where patients had antidepressant medications prescribed for other indications than depression (e.g. smoking cessation or neuralgic pain), these patients were not considered as having treated depression. Only those patients with scores ≥10 on the PHQ-9 and documentation of a diagnosis and/or treatment (counseling or antidepressants) in their medical records were considered ‘treated’ prior to discharge, a definition that has been used in prior work.3, 14 In the main analyses of this study, 3 groups were created based on PHQ-9 depression assessment and depression recognition status: (1) no depression (PHQ-9 <10; reference); (2) treated depression; and (3) untreated depression.
1-Year Mortality
1-Year Mortality – Information about 1-year all-cause mortality was obtained from the Social Security Death Master File and available for 96% (n=3,890) of patients in this cohort.
Statistical Analyses
Patient characteristics during the index AMI admission and treatment rates for either depression counseling or antidepressant medications at 1, 6, and 12 months following the index AMI were compared between patients categorized as: (1) no depression (PHQ-9 score <10); (2) treated depression; (3) untreated depression. Student’s t tests or Mann-Whitney U tests were used for continuous variables and Chi-Square tests for categorical variables, as appropriate.
One-year mortality rates were compared between the 3 groups using Kaplan-Meier curves and tested for statistical significance with the log-rank test. Next, Cox Proportional Hazards Models were constructed to calculate hazard ratios for 1-year mortality among the 3 groups (reference category: no depression [PHQ-9 score <10]). To understand the impact of potential confounders on the estimate of the association (the conditional effect or the average effect on the individual), we constructed a series of hierarchical proportional hazard models, with a random effect for site. These models sequentially adjusted for demographics (age, sex, race [African American, other race vs. white race]); socio-economic variables (marital status [married or common law vs. not], education [completed high school education or more vs. not], insurance status [uninsured vs. insured]); and disease severity and clinical factors (left ventricular ejection fraction <40%, Killip class upon arrival [II, III, IV vs. I], systolic blood pressure upon arrival, heart rate upon arrival, ST-elevation AMI, hyperlipidemia, hypertension, peripheral vascular disease, diabetes mellitus, history of cardiovascular disease (myocardial infarction, angina, coronary artery bypass graft, chronic heart failure, cerebrovascular disease), chronic kidney disease, chronic lung disease, history of cancer, current smoking, body mass index, having a family history of coronary artery disease, and history of depression).
To confirm the association between depression recognition and 1-year mortality found in our primary analysis, we conducted a propensity score analysis comparing those with untreated depression (n=528) and those with treated depression (n=231) to evaluate the marginal effect (or the effect on the overall population). All covariables that were included in the primary analysis were included in the propensity model, as well as additional comorbidities and socioeconomic variables, including working status, in-hospital revascularization and number of diseased vessels. Covariable balance between the groups was assessed by standardized differences before and after adjustment to evaluate the effectiveness of the adjustment. We then analyzed 1-year outcomes using Cox regression models adjusting for the propensity score (modeled nonlinearly using restricted cubic splines), as well as any covariables that remained unbalanced between the groups after propensity adjustment (Standardized Difference > 10).22
As a sensitivity analysis, we calculated a variable that combined information on patients’ depression treatment during follow-up. Patients who reported antidepressant and/or counseling treatment at either the 1-month or 6-month follow-up interview, were considered to have had follow-up treatment for depression following discharge. This variable was introduced into the propensity-adjusted model, as an exploratory analysis to examine whether depression treatment, a consequence of depression recognition, was associated with an attenuated risk for the association between depression and 1-year mortality. We then calculated the % change in hazard ratio for the association between the variable depression recognition and 1-year mortality. In these analyses, we also aimed to reduce the risk of survival bias, and defined the analytic cohort as those who survived up to 6 months. We then examined their survival from 6 months onwards, so that only those who were able to provide the follow-up information were included in the model (leaving 687 patients with follow-up data through 18 months in the analyses; 211 with treated depression and 476 with untreated depression).
Missing covariable information was assumed to be missing at random given the minimal missing data, with only 9 covariables having ≤1.6% missing information, except for body mass index, a variable that had 5.5% missing data. On a patient level, 404 (10%) patients had missing covariable information at baseline; the majority of them had missing information for only one variable (n=366), only 7 patients had missing information for 3 variables. We imputed missing data with single imputation using IVEWare (Imputation and Variance Estimation Software; University of Michigan’s Survey Research Center, Institute for Social Research, Ann Arbor, MI). All other statistical analyses were conducted with SAS 9.3 for Windows (SAS Institute, Cary, North Carolina). All tests were two-tailed and considered statistically significant at the α = .05 level.
RESULTS
Among 4,062 eligible patients in TRIUMPH, 3,303 did not have significant depressive symptoms and 759 (18.7%) screened positive for potential depression (PHQ-9 scores ≥10) at the time of their AMI. Of those with depression, 231 (30.4%) were treated to have had depression by their providers and 528 (69.6%) were not. Of the patients with treated depressive symptoms, 159 (69%) were on anti-depressants at the index AMI discharge. Compared with patients who had no depression, patients with PHQ-9 scores ≥10 were younger, more likely to be female, and were less likely married or employed. Patients with significant depressive symptoms also had higher rates of hypertension, diabetes, and chronic lung disease, and to be actively smoking. Patients with depression also were more likely to have relatives with coronary artery disease, a higher heart rate upon AMI admission, and lower rates of ST-elevation AMI (Table 1). Of note, patients with untreated depression were more often of minority race and had lower levels of education, as compared with patients that had no depression and those with treated depression. Mean PHQ-9 scores in patients without depression were 3.1 and 14.7 and 13.7 in patients with treated and untreated depression, respectively (Table 1). Given that somatic manifestations of depression have been shown to be more strongly associated with subsequent mortality,23 we also compared the mean somatic symptom scores (generated from the items on sleep, fatigability, appetite, and psychomotor agitation/retardation) between the treated and untreated depressed groups and found them to be similar; mean score of 7.7±2.1 for the treated group vs. 7.6±2.1 for the untreated group (P=0.76), minimizing the likelihood that the type of depressive symptoms confounded any associations with mortality between the patients with depressive symptoms who were and were not treated. At all follow-up time points, depressed patients who were untreated had treatment rates that were between 3- and 4-times lower than patients who had treated depression (all P-values <0.001) (Table 1).
Table 1.
Patient Characteristics by Depression and Depression Recognition Status.
| Characteristic | PHQ-9 <10 No Depression n=3303 (81.3%) |
PHQ-9 ≥10 Treated Depression n=231 (5.7%) |
PHQ-9 ≥10 Untreated Depression n=528 (16.0%) |
P-Value |
|---|---|---|---|---|
| Demographics | ||||
| Age, mean ± SD (years) | 59.6±12.4 | 55.7±10.9 | 56.6±12.1 | <0.001 |
| Female | 1011 (30.6) | 105 (45.5) | 222 (42.0) | <0.001 |
| Race | <0.001 | |||
| White | 2208 (66.8) | 175 (75.8) | 352 (66.7) | |
| African-American | 889 (26.9) | 37 (16.0) | 129 (24.4) | |
| Other | 206 (6.2) | 19 (8.2) | 47 (8.9) | |
| Socio-Economic Factors | ||||
| Married/Common Law | 1805 (54.7) | 99 (42.9) | 231 (43.8) | <0.001 |
| Education greater than High School | 1651 (50.1) | 120 (51.9) | 237 (45.0) | 0.07 |
| No Insurance/Self-Pay | 708 (21.8) | 59 (25.9) | 135 (25.9) | 0.06 |
| Full or Part-Time Employment | 1704 (51.9) | 70 (30.4) | 215 (41.0) | <0.001 |
| Medical history | ||||
| Dyslipidemia | 1586 (48.0) | 132 (57.1) | 246 (46.6) | 0.019 |
| Hypertension | 2159 (65.4) | 170 (73.6) | 375 (71.0) | 0.003 |
| Peripheral Vascular Disease | 142 (4.3) | 14 (6.1) | 30 (5.7) | 0.20 |
| Diabetes | 941 (28.5) | 98 (42.4) | 203 (38.4) | <0.001 |
| Prior MI | 670 (20.3) | 56 (24.2) | 119 (22.5) | 0.21 |
| Prior Angina | 489 (14.8) | 41 (17.7) | 79 (15.0) | 0.48 |
| Prior PCI | 601 (18.2) | 60 (26.0) | 117 (22.2) | 0.002 |
| Prior CABG | 361 (10.9) | 41 (17.7) | 51 (9.7) | 0.003 |
| Prior CVA | 161 (4.9) | 13 (5.6) | 27 (5.1) | 0.86 |
| Chronic Kidney Disease | 236 (7.1) | 22 (9.5) | 42 (8.0) | 0.36 |
| Chronic Lung Disease | 210 (6.4) | 29 (12.6) | 56 (10.6) | <0.001 |
| Chronic Heart Failure | 254 (7.7) | 34 (14.7) | 56 (10.6) | <0.001 |
| Cancer | 232 (7.0) | 13 (5.6) | 42 (8.0) | 0.50 |
| Currently Smoking | 1219 (37.1) | 112 (48.9) | 260 (49.6) | <0.001 |
| BMI | 29.2±6.2 | 30.7±6.9 | 30.7±7.4 | <0.001 |
| Family history of CAD | 2376 (72.5) | 180 (78.6) | 416 (79.7) | <0.001 |
| In-hospital Treatment | ||||
| ASA | 3196 (96.8) | 216 (93.5) | 497 (94.1) | <0.001 |
| Beta Blocker | 2716 (82.2) | 183 (79.2) | 423 (80.1) | 0.29 |
| Fibrinolytic therapy | 202 (6.1) | 5 (2.2) | 21 (4.0) | 0.009 |
| Antiplatelet | 2257 (68.3) | 148 (64.1) | 335 (63.4) | 0.044 |
| Anticoagulant | 2976 (90.1) | 204 (88.3) | 486 (92.0) | 0.22 |
| Clopidogrel | 2238 (67.8) | 147 (63.6) | 329 (62.5) | 0.034 |
| In-Hospital Revascularization | 2393 (72.4) | 151 (65.4) | 372 (70.5) | 0.053 |
| Cardiac Catheterization | 3051 (92.4) | 207 (89.6) | 489 (92.6) | 0.30 |
| PCI | 2113 (64.0) | 136 (58.9) | 330 (62.5) | 0.26 |
| CABG | 310 (9.4) | 19 (8.2) | 49 (9.3) | 0.84 |
| Clinical characteristics at admission | ||||
| LV Systolic Function <40% | 591 (17.9) | 49 (21.2) | 107 (20.3) | 0.22 |
| Arrival: Killip Class | 0.42 | |||
| I | 2924 (89.3) | 194 (85.5) | 450 (86.9) | |
| II | 285 (8.7) | 27 (11.9) | 53 (10.2) | |
| III | 48 (1.5) | 5 (2.2) | 11 (2.1) | |
| IV | 18 (0.5) | 1 (0.4) | 4 (0.8) | |
| Diseased vessels | 0.05 | |||
| 0 | 263 (8.6) | 24 (11.6) | 47 (9.6) | |
| 1 | 1291 (42.3) | 82 (39.6) | 193 (39.3) | |
| 2 | 786 (25.7) | 43 (20.8) | 149 (30.3) | |
| 3 | 715 (23.4) | 58 (28.0) | 102 (20.8) | |
| Initial Systolic Blood Pressure, mm Hg | 143.6±30.0 | 136.9±32.0 | 143.4±29.7 | 0.005 |
| Initial Heart Rate, beats per minute | 82.0±21.7 | 86.1±23.2 | 84.0±23.1 | 0.005 |
| ST-elevation MI | 1457 (44.1) | 83 (35.9) | 206 (39.0) | 0.007 |
| Baseline Depression Score | ||||
| PHQ-9 | 3.1±2.8 | 14.7±3.7 | 13.7±3.4 | <0.001 |
| Follow-Up Antidepressants or Depression Counseling | ||||
| 1 month follow-up | – | 89 (59.7) | 55 (16.2) | <0.001 |
| 6 month follow-up | – | 92 (65.7) | 63 (20.2) | <0.001 |
| 12 month follow-up | – | 23 (60.5) | 14 (15.6) | <0.001 |
Three groups are compared: patients with (1) PHQ-9 scores <10 (no depression); (2) PHQ-9 scores ≥10 and treated (treated depression); and (3) PHQ-9 scores ≥10 and not treated (untreated depression).
Values are expressed as n (%), unless otherwise specified. Abbreviations: PHQ-9, Patient Health Questionnaire 9-item version; SD, standard deviation; MI, myocardial infarction; PCI, peripheral percutaneous intervention; CABG, coronary artery bypass graft; CVA, cerebrovascular accident; BMI, body mass index (weight (kg)/height (m2)); CAD, coronary artery disease; ASA, LV, left ventricular; ST-Elevation MI, ST-segment elevation myocardial infarction.
1-Year Mortality
When comparing the 1-year mortality rates among the 3 groups, the unadjusted 1-year mortality rate among patients with treated depression was not different from the rate among patients without depression (6.7% [15/223] vs. 6.1% [193/3159]), whereas patients with untreated depression had higher unadjusted mortality rates (10.8% [55/508]) (Figure 1; log rank test P-value of 0.0004). Table 2 provides the risk estimates for mortality after only adjusting for site variability and after complete multivariable adjustment, including site, demographics, socio-economic variables, disease severity, and clinical variables. Patients with treated depression had no different 1-year mortality rates as patients without depression after multivariable adjustment (Hazard Ratio [HR] of 1.12; 95% CI: 0.63-1.99; P=0.71). In contrast, patients with untreated depression had a greater hazard for 1-year mortality as compared with patients without depression (HR of 1.91; 95% CI: 1.39-2.62; P<0.001). After adjusting for the propensity to be treated, among patients with depression, we found a 1-year risk of mortality that was not different for patients with and without treated depression (HR for untreated depression of 1.75; 95% CI: 0.83-3.72; P=0.14).
Figure 1. Kaplan-Meier 1-Year Survival Curves by Depression and Depression Recognition Status.
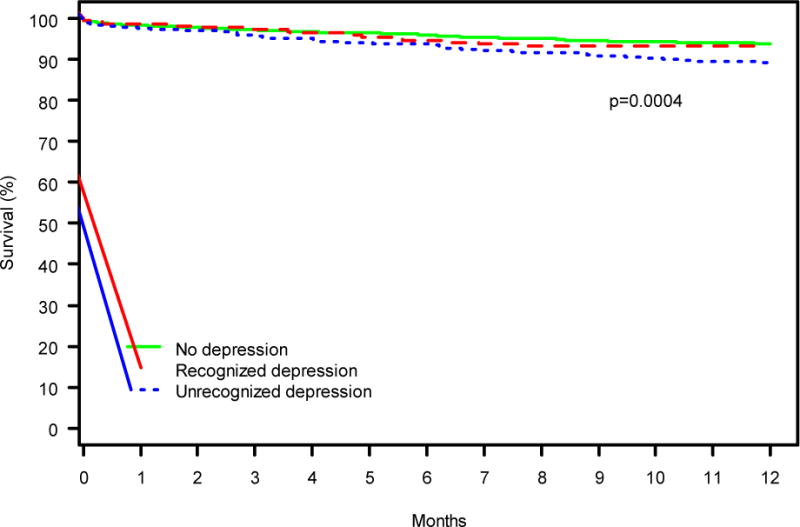
Three groups are compared: patients with (1) PHQ-9 scores <10 (no depression); (2) PHQ-9 scores ≥10 and treated (treated depression); and (3) PHQ-9 scores ≥10 and not treated (untreated depression).
Table 2.
Unadjusted and Adjusted Cox Regression Results For the Association Between Depression Recognition Groups and 1-Year Mortality.
| Model 1 – Unadjusted, except for site | HR | 95% CI | P-Value |
|---|---|---|---|
|
| |||
| Treated Depression(15 out of 223 deceased) | 1.17 | 0.69-2.00 | 0.55 |
| Untreated Depression(193 out of 3159 deceased) | 1.83 | 1.35-2.48 | <.0001 |
| No Depression(reference; 55 out of 508 deceased) | |||
|
| |||
| Model 2 – Adjusted for demographics, socio-economic variables, disease severity, and clinical variables* | HR | 95% CI | P-Value |
|
| |||
| Treated Depression | 1.12 | 0.63-1.99 | 0.71 |
| Untreated Depression | 1.91 | 1.39-2.62 | <.0001 |
| No Depression (reference) | |||
Three groups are compared: patients with (1) PHQ-9 scores <10 (no depression; reference); (2) PHQ-9 scores ≥10 and treated (treated depression); and (3) PHQ-9 scores ≥10 and not treated (untreated depression). Hazard Ratios (HR), corresponding 95% Confidence Intervals (CI), and P-values are presented.
Covariables in the model included: age, sex, race, marital status, education, insurance status, history of dyslipidemia, hypertension, peripheral vascular disease, diabetes, myocardial infarction, angina, coronary artery bypass graft, cerebrovascular accident, chronic kidney disease, chronic lung disease, chronic heart failure, cancer, current smoking, body mass index, family history of coronary artery disease, history of depression requiring treatment, Left ventricular systolic function <40%, Killip Class upon arrival, systolic blood pressure upon arrival, ST-Elevation myocardial infarction.
To reduce the risk of survival bias, we conducted sensitivity analyses while defining the analytic cohort as those who survived up to 6 months and following their 1-year survival time from 6 to 18 months, so that only those who were able to provide the follow-up information were included in the model. Patients with untreated depression had an almost 2.5-fold risk of mortality at 1 year as compared with those who were treated (HR untreated depression = 2.47; 95% CI: 1.01-6.07; P=0.049). After introducing the potential mediator of follow-up depression treatment, this association was no longer statistically significant (HR untreated depression = 2.03; 95% CI: 0.80-5.16; P=0.14), although the effect size was similar. The follow-up depression treatment variable explained 30% of the excess hazard for the association between depression recognition and 1-year mortality.
DISCUSSION
We conducted an observational study to assess the association of depression recognition and subsequent mortality after an AMI. We found that although one-fifth of patients with AMI in this multi-center cohort had significant depressive symptoms, only a third of those with depression were treated in routine clinical care. Moreover, we found that patients with treated depression had 1-year mortality rates that were not different from rates seen in patients without depression, while those with untreated depression had a 70% to 90% higher risk than either patients without depression or with treated depression, even after adjusting for multiple potential confounders for the relationship between depression and mortality. These findings provide important insights into the clinical trajectories of patients with treated and untreated depression following an AMI.
Apart from a signal that was observed towards lesser major adverse cardiac events in acute coronary syndrome patients with depression being assigned to a stepped-care depression treatment program versus those who received usual care,24 most clinical trials have failed to show a cardiovascular benefit from depression treatment.9–11, 15, 25, 26 While our study is observational, there are other important differences with the prior depression trials in coronary artery disease focusing on survival outcomes. Typically, previously published randomized trials in coronary populations have had very stringent inclusion and exclusion criteria that differ from the broader, real-world patients participating in this observational study. Most importantly, studies were not adequately powered to detect a potential survival benefit following depression treatment in coronary artery disease.27 Also, the clinical trials have an important co-intervention, including close monitoring of patients’ depressive symptoms and suicidality for all patients enrolled, that may minimize potential benefits of recognition and treatment to be detected. These highly controlled circumstances do not reflect real-world clinical care, where 70% of patients who screen positive for depressive symptoms do not even receive further follow-up or care for their symptoms. This was especially the case for those with a vulnerable socio-economic profile and non-white race.
While our results warrant further replication among other real-world observational cohorts, a carefully designed randomized clinical trial13, 28, 29 may ideally be needed to test whether depression screening and subsequent treatment versus a control group with care as usual is associated with better cardiovascular outcomes. Given that depression is an important comorbidity in its own right, and that treatment options are available but underused, it is reasonable to screen and treat patients with depression, independent of whether treatment benefits on cardiovascular outcomes exist. This practice has recently also been supported the US Preventive Services Task Force, recommending screening for the adult population, especially in individuals dealing with chronic diseases in their recent statement reviewing the latest available evidence.30 These recommendations are in line with previously published statements from the American Heart Association.31 The findings from this study additionally generate the hypothesis that the higher mortality risk associated with depression in patients with AMI, may be restricted to those with untreated depression.
Given that depression remains widely unrecognized and untreated among patients with AMI and given that our findings documented an association between depression treatment status and mortality, novel strategies to implement depression-screening and treatment programs in the setting of acute coronary care should further be designed and tested for effectiveness. While some programs have been shown to be successful and feasible from a logistic and potentially also from a cost-perspective,32 there is a need to explore additional strategies or to establish the generalizability of previous approaches. From a cardiac risk management standpoint alone and upon further confirmation of our findings, depression evaluation and follow-up may be valuable components of the AMI clinical pathway, akin to lipid and blood pressure management in AMI. Contemporary standard order sets would then refer patients with recognized depression for further depression evaluation and follow-up. Importantly, these strategies should be integrated with additional enhancements of depression care, such as a collaborative care program or the addition of a case manager, in order to be maximally successful.33
Our findings should be interpreted in the context of several potential limitations. First, patients’ depressive symptoms were self-reported and we had no way of formally verifying whether their depressive symptoms also qualified for a DSM diagnosis of major depression.34 However, a self-report questionnaire may be the most feasible way to initially risk-stratify patients that are at increased risk of having depressive symptoms as the time of an AMI. Second, while one of the strengths of this study was access to a large richly documented real-world database of patients with AMI with depressive symptoms assessed at the time of their AMI admission, care provided, and 1-year AMI outcomes, as an observational study it is subject to unmeasured confounding and causality cannot be definitely proven. Third, we did not have detailed information about crossovers, depression therapy compliance over time, and what type and the intensity of counseling patients received for their depression after discharge and cannot define which elements of depression care may have been most strongly associated with better outcomes in patients with depressive symptoms that were treated. Finally, our primary outcome was all-cause mortality, and we were not able to separately link depression recognition with cardiovascular mortality or deaths due to suicide as our study was not designed and powered to examine these separate outcomes. Future studies will further have to examine potential pathways that may explain the excess mortality risk that patients with untreated depression were exposed to.
CONCLUSIONS
This study is the first to provide documentation of an association between depression treatment status at the time of AMI and mortality one year after the AMI, with untreated depression associated with an increased mortality risk as compared with patients whose depression was being treated and non-depressed patients. The magnitude of the association was substantial and robust to multivariable adjustment for a range of clinical and patient-centered characteristics. Although we cannot prove a causal relationship between recognition of depression and improved outcomes, these findings, support current recommendations to implement depression screening in AMI care and support further testing the impact of depression screening protocols in the setting of an AMI.
1) What is new?
Depression following an acute myocardial infarction (AMI) is associated with an increased 1-year mortality risk.
This study is the first to document that this association differs by depression treatment status at the index AMI event.
Patients with untreated depression had a 70% to 90% higher risk of dying 1 year after their AMI than either patients without depression or with treated depression.
2) What are the clinical implications?
The present findings are hypothesis generating and encourage further research to examine the impact of depression recognition and treatment at the time of an AMI on subsequent survival.
Ideally, this should be done through carefully designed randomized controlled trial interventions.
Acknowledgments
Funding Sources
The TRIUMPH study was supported by grants from the National Heart, Lung, and Blood Institute Specialized Center of Clinically Oriented Research in Cardiac Dysfunction and Disease (grant no. P50 HL077113).
Dr. Smolderen is supported by the Patient Centered Outcomes Research Institute [CE-1304-6677].
Dr. Chan is supported by funding from the National Heart Lung and Blood Institute (1R01HL123980).
Dr. Shah is supported by funding from the National Center for Advancing Translational Sciences of the National institutes of Health under Award Numbers UL1TR000454 and KL2TR000455 and the American Heart Association, 15SDG25310017.
The funding organizations and sponsors of the study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Data Access and Responsibility
Dr. Smolderen had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures
The authors report no disclosures or conflicts of interest.
References
- 1.Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, Freedland KE, Jaffe AS, Leifheit-Limson EC, Sheps DS, Vaccarino V, Wulsin L, on behalf of the American Heart Association Statistics Committee of the Council on E, Prevention, the Council on C and Stroke N Depression as a Risk Factor for Poor Prognosis Among Patients With Acute Coronary Syndrome: Systematic Review and Recommendations: A Scientific Statement From the American Heart Association. Circulation. 2014;129:1350–1369. doi: 10.1161/CIR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 2.Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Depression and health-care costs during the first year following myocardial infarction. J Psychosom Res. 2000;48:471–478. doi: 10.1016/s0022-3999(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 3.Smolderen KG, Spertus JA, Reid KJ, Buchanan DM, Krumholz HM, Denollet J, Vaccarino V, Chan PS. The association of cognitive and somatic depressive symptoms with depression recognition and outcomes after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:328–337. doi: 10.1161/CIRCOUTCOMES.109.868588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakatani D, Sato H, Sakata Y, Shiotani I, Kinjo K, Mizuno H, Shimizu M, Ito H, Koretsune Y, Hirayama A, Hori M, Osaka Acute Coronary Insufficiency Study G Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. Am Heart J. 2005;150:652–658. doi: 10.1016/j.ahj.2005.03.062. [DOI] [PubMed] [Google Scholar]
- 5.Frasure-Smith N, Lesperance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61:26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mallik S, Spertus JA, Reid KJ, Krumholz HM, Rumsfeld JS, Weintraub WS, Agarwal P, Santra M, Bidyasar S, Lichtman JH, Wenger NK, Vaccarino V. Depressive symptoms after acute myocardial infarction: evidence for highest rates in younger women. Arch Intern Med. 2006;166:876–883. doi: 10.1001/archinte.166.8.876. [DOI] [PubMed] [Google Scholar]
- 8.Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES. Depression and Coronary Heart Disease. Recommendations for Screening, Referral, and Treatment. A Science Advisory From the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 9.Strik JJ, Honig A, Lousberg R, Lousberg AH, Cheriex EC, Tuynman-Qua HG, Kuijpers PM, Wellens HJ, Van Praag HM. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med. 2000;62:783–789. doi: 10.1097/00006842-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine CJ, Mardekian J, Harrison WM, Barton D, McLvor M. Sertraline treatment of major depression in patients with acute MI or unstable angina. Jama. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 11.Honig A, Kuyper AM, Schene AH, van Melle JP, de Jonge P, Tulner DM, Schins A, Crijns HJ, Kuijpers PM, Vossen H, Lousberg R, Ormel J, investigators M-I Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med. 2007;69:606–613. doi: 10.1097/PSY.0b013e31814b260d. [DOI] [PubMed] [Google Scholar]
- 12.van Melle JP, de Jonge P, Honig A, Schene AH, Kuyper AM, Crijns HJ, Schins A, Tulner D, van den Berg MP, Ormel J, investigators M-I Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry. 2007;190:460–466. doi: 10.1192/bjp.bp.106.028647. [DOI] [PubMed] [Google Scholar]
- 13.Thombs BD, Roseman M, Coyne JC, de Jonge P, Delisle VC, Arthurs E, Levis B, Ziegelstein RC. Does evidence support the American Heart Association’s recommendation to screen patients for depression in cardiovascular care? An updated systematic review. PloS one. 2013;8:e52654. doi: 10.1371/journal.pone.0052654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smolderen KG, Buchanan DM, Amin AA, Gosch K, Nugent K, Riggs L, Seavey G, Spertus JA. Real-world lessons from the implementation of a depression screening protocol in acute myocardial infarction patients: implications for the American Heart Association depression screening advisory. Circ Cardiovasc Qual Outcomes. 2011;4:283–292. doi: 10.1161/CIRCOUTCOMES.110.960013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, Swenson JR, Ghatavi K, Abramson BL, Dorian P, Guertin MC. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 16.Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 17.Arnold SV, Chan PS, Jones PG, Decker C, Buchanan DM, Krumholz HM, Ho PM, Spertus JA. Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH): design and rationale of a prospective multicenter registry. Circ Cardiovasc Qual Outcomes. 2011;4:467–476. doi: 10.1161/CIRCOUTCOMES.110.960468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290:215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGuire AW, Eastwood JA, Macabasco-O’Connell A, Hays RD, Doering LV. Depression screening: utility of the patient health questionnaire in patients with acute coronary syndrome. Am J Crit Care. 2013;22:12–19. doi: 10.4037/ajcc2013899. [DOI] [PubMed] [Google Scholar]
- 22.Normand S, Landrum M, Guadagnoli E, Ayanian J, Ryan TCP, McNeil BJ. Validating recommendations for coronary angiography following an acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 23.Smolderen KG, Spertus JA, Reid KJ, Buchanan DM, Krumholz HM, Denollet J, Vaccarino V, Chan PS. The association of cognitive and somatic depressive symptoms with depression recognition and outcomes after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:328–337. doi: 10.1161/CIRCOUTCOMES.109.868588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davidson KW, Rieckmann N, Clemow L, Schwartz JE, Shimbo D, Medina V, Albanese G, Kronish I, Hegel M, Burg MM. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch Intern Med. 2010;170:600–608. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Jama. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 26.O’Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, Zakhary B, Stough WG, Arias RM, Rivelli SK, Krishnan R, Investigators S-C Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56:692–699. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joynt KE, O’Connor CM. Lessons from SADHART, ENRICHD, and other trials. Psychosom Med. 2005;67(Suppl 1):S63–66. doi: 10.1097/01.psy.0000163454.25036.fc. [DOI] [PubMed] [Google Scholar]
- 28.Hasnain M, Vieweg WV. Is screening cardiac inpatients for depression really feasible? Am Heart J. 2010;160:e29. doi: 10.1016/j.ahj.2010.07.028. author reply e30. [DOI] [PubMed] [Google Scholar]
- 29.Hasnain M, Vieweg WV, Lesnefsky EJ, Pandurangi AK. Depression screening in patients with coronary heart disease: a critical evaluation of the AHA guidelines. J psychosom res. 2011;71:6–12. doi: 10.1016/j.jpsychores.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 30.Siu AL, Force USPST. Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, Garcia FA, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, Pignone MP. Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:380–387. doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- 31.Box TL, McDonell M, Helfrich CD, Jesse RL, Fihn SD, Rumsfeld JS. Strategies from a nationwide health information technology implementation: the VA CART story. J Gen Intern Med. 2010;25(Suppl 1):72–6. doi: 10.1007/s11606-009-1130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, Dornelas E, Duer-Hefele J, Frasure-Smith N, Freedland KE, Haas DC, Jaffe AS, Ladapo JA, Lesperance F, Medina V, Newman JD, Osorio GA, Parsons F, Schwartz JE, Shaffer JA, Shapiro PA, Sheps DS, Vaccarino V, Whang W, Ye S. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA intern med. 2013;173:997–1004. doi: 10.1001/jamainternmed.2013.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbody S, Sheldon T, House A. Screening and case-finding instruments for depression: a meta-analysis. CMAJ. 2008;178:997–1003. doi: 10.1503/cmaj.070281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) 4. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]


