Abstract
Full radial posterior lateral meniscus root tears are frequently associated with injuries to the anterior cruciate ligament. Left unrepaired, they result in loss of the meniscus hoop stress function and can lead to overload of the lateral compartment and early degenerative changes. Arthroscopic suture repairs show successful results with long-term follow-up. However, previously described suture repair techniques have often required special instrumentation and can be technically demanding. This Technical Note describes the use of an accessory portal through the patellar tendon as a safe and easy method for repairing full posterior radial tears of the lateral meniscus.
Posterior lateral meniscus root tears (PLMRTs) are well defined and must be considered serious lesions because they result in loss of the meniscus hoop stress function.1 If they are not repaired, the lateral compartment is exposed to unfavorable dynamic contact mechanics similar to those resulting from a partial or even total lateral meniscectomy in the case of full radial tears.2, 3 Meniscal preservation with suture repair is currently considered the gold standard of treatment, with very good results at long-term follow-up.4, 5, 6 Although a number of surgical techniques have been described, it is well recognized that these can be very technically demanding.4, 5, 6, 7, 8 The aim of this Technical Note is to present an easy and safe method to repair PLMRTs using a simple all-inside suture technique through an accessory central midline portal described by Gillquist and Hagberg9 in 1976.
Surgical Technique
Magnetic Resonance Imaging Assessment
Preoperative magnetic resonance imaging (Fig 1) aids in the evaluation of meniscal pathology and in identification of associated injuries. In conjunction with the history and clinical examination, this allows the surgeon an appropriate index of suspicion of pathology likely to be encountered and therefore the ability to request the appropriate instrumentation and implants in advance. The surgical technique is presented in Video 1.
Fig 1.
Magnetic resonance images of a right knee showing anterior cruciate ligament rupture and a concomitant posterior lateral meniscus root tear. (A) Sagittal view showing anterior cruciate ligament tear. (B) Coronal view with lateral tibial plateau bone bruise (asterisk); a hypersignal is visible close to the lateral root of the posterior horn, suggesting a meniscal root tear (arrow).
Patient Setup
The patient is placed supine on the operating table in the standard arthroscopy position with a lateral post just proximal to the knee, at the level of the padded tourniquet, and a foot roll to prevent the hip from externally rotating and to maintain 90° of knee flexion. In this way, the knee can be moved freely through the full range of motion.
Skin Landmarks
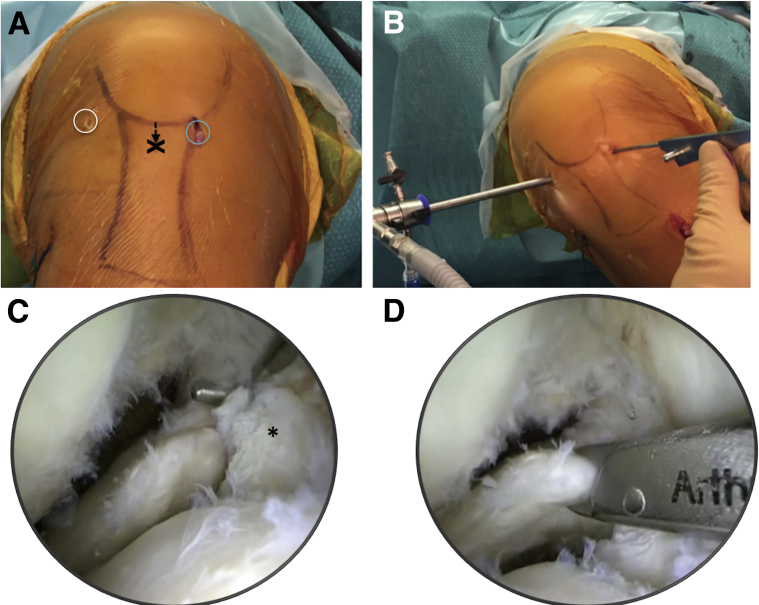
Three skin landmarks are marked before application of the povidone-iodine–coated cutaneous drape: high anterolateral portal, anteromedial portal, and central midline portal (Fig 2).
Fig 2.
Right knee. (A) External view showing high anterolateral portal (white circle), high medial portal (blue circle), and central midline portal locations (X represents the portal and the arrow indicates the 8 mm below the tip of the patella). (B) External view showing anterolateral viewing and anteromedial instrumentation for evaluation of the posterior horn of the lateral meniscus. (C) Arthroscopic view from the high anterolateral portal showing a full radial posterior-horn lateral meniscus tear. The asterisk indicates the root fragment. (D) The tear is evaluated for reducibility and reparability.
Incision and Exploration
The anterolateral portal is created at the highest position possible. This is at the level of the inferior border of the patella and approximately 4 mm lateral to the lateral border of the patellar tendon.10 The anteromedial portal is created just adjacent to the medial edge of the patellar tendon and the inferior border of the patella (Fig 2A). A full diagnostic arthroscopy is performed, and associated cartilage lesions and medial meniscus tears are treated. The knee is placed in the figure-of-4 position, and the PLMRT is probed to determine the tear morphology. Tear repairability is then assessed. When the root fragment is large enough to allow suture anchor placement and when satisfactory approximation of the edges of the tear can be achieved with an arthroscopic forceps, repair with suture anchors through the central portal can be performed (Fig 2 B-D).
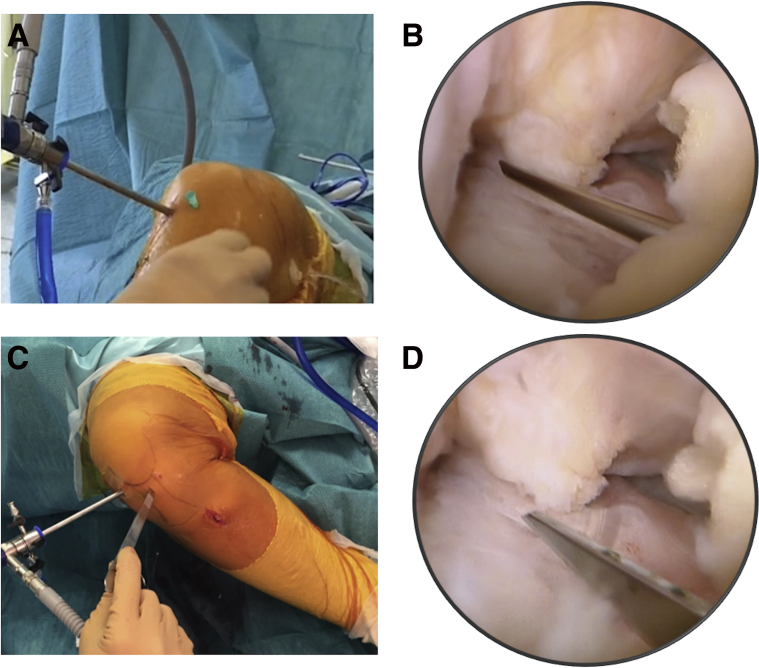
The central midline portal is created, as described by Gillquist and Hagberg,9 through the patellar tendon (Figs 2 and 3). A needle is placed about 8 mm below the inferior margin of the patella. Satisfactory positioning and orientation of the needle are checked under arthroscopic vision. The central portal is then created with a surgical knife using the same direction as the needle. The intra-articular emergence of the surgical blade through the fat pad is checked under arthroscopic vision (Fig 3).
Fig 3.
Creation of central midline portal in a right knee. (A) External view showing needle placement 8 to 10 mm below the inferior pole of the patella. (B) Arthroscopic view showing needle localization of the optimum portal location. (C) The portal is created with a surgical knife in the same location and with the same orientation as the optimally positioned needle. (D) The intra-articular emergence of the surgical blade through the fat pad is checked to avoid iatrogenic injury.
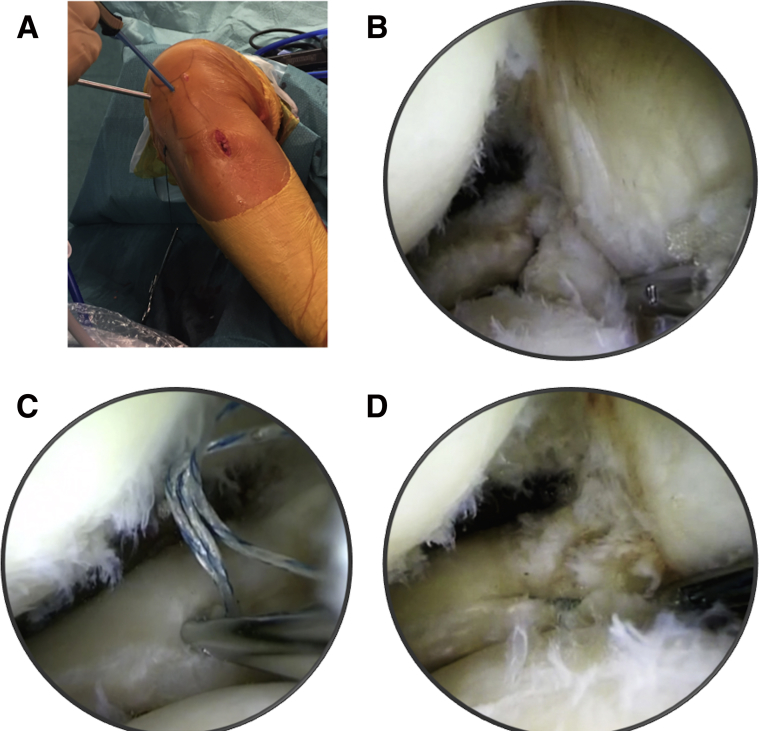
Suture Anchor Repair
If an anterior cruciate ligament (ACL) tear is present, the lateral meniscus is addressed before ligament reconstruction. A simple all-inside meniscal repair device (Ultra Fast-Fix; Smith & Nephew, Andover, MA) is introduced through the central midline portal to perform horizontal suture placement after debridement of the tear (Fig 4). Abrasion of the lesion is achieved with a shaver or spinal needle to increase the vascularization and healing of the tear. The first anchor is placed within the anterior fragment of the meniscal root close to the ACL tibial insertion. The device is then reloaded to enable a second anchor to be placed within the posterior fragment of the meniscal root, thus creating a horizontal suture configuration. The suture is gently pulled, and the pretied sliding knot is advanced to obtain reduction of the tear. The suture is cut by pushing a trigger in the knot pusher–suture cutter. The stability of the radial tear of the meniscus is checked with a probe (Fig 4). Surgical steps, pearls and pitfalls of the technique are summarized in Table 1.
Fig 4.
Posterior-horn lateral meniscus repair in a right knee. (A) The knee is placed in the figure-of-4 position, and the all-inside meniscal repair device (Ultra Fast-Fix) is introduced through the central midline portal while the arthroscope is positioned in the anterolateral portal. (B) Arthroscopic view from high anterolateral portal. The first anchor is placed in the root remnant. (C) The second anchor is placed in the meniscus fragment. (D) Tear reduction is achieved by tensioning the sutures with the knot pusher–suture cutter device.
Table 1.
Surgical Steps, Pearls, and Pitfalls of Repair Technique of Radial Tears of Lateral Meniscus Using Central Midline Portal
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Portals | To avoid the fat pad, a high anterolateral portal should be used. It allows a wider field of view and facilitates visualization of the lateral meniscus. | If the anterolateral portal is too low, the fat pad can impede visualization. |
| Using an accessory central midline portal allows the anterolateral portal to be free for visualization exclusively and allows less tangential suture insertion than from the anteromedial portal. | ||
| Instrumentation | Arthroscope placement in the anterolateral portal allows a more direct view. | One should avoid incorrectly thinking that switching portals between the arthroscope and the suture device will be easier than using a separate Gillquist portal for instrumentation. |
| A cannula should be used to protect the suture device when penetrating into the joint. | ||
| Suture placement | Horizontal suture should be placed after debridement. | It is not comfortable to perform suture placement from the lateral portal by use of the figure-of-4 position. |
| Penetration of the posterior capsule with the suture device must be avoided because this can result in over-reduction of the tear. |
Discussion
Full radial posterior lateral meniscus tears within 9 mm of the center of the root attachment are classified by LaPrade et al.1 as type II meniscal root tears. The basis for this cutoff is biomechanical studies that have shown significantly altered biomechanics of the posterior meniscal roots when full radial tears occur within this zone.11, 12 PLMRTs are usually traumatic in origin and have been reported in up to 12% of patients with ACL ruptures.13 Biomechanically, this type of lesion results in loss of meniscal hoop strength and meniscal extrusion.6, 14, 15 Clearly, such injuries have severe biomechanical consequences, which have been described as functionally equivalent to a total meniscectomy.3
The main objectives of suture repair of PLMRTs are to restore normal loading and to reduce the risk of early degenerative changes. In the rare case of root avulsion (type V root tear) or when the root remnant is too small to allow anchor placement, tibial tunnel drilling and pullout techniques are preferred.11, 12 For type II root tears (also described in the literature as full radial PLMRTs), several arthroscopic repair techniques have been described with good results.4, 5, 6, 7 However, the majority are widely recognized as technically challenging because of the need for either performing complicated techniques or using special devices. Our technique has the advantages of simplicity and the use of a device for suturing that is in common use. Regardless of the suture device used, the difficulty in accessing the location of the tear, the tear's morphology (often with a small root remnant), the requirement for a figure-of-4 position, and the joint environment (lateral tibial spine, Hoffa fat pad) are some of the main obstacles of this demanding procedure. This is made more arduous by the requirement of previously described techniques to frequently switch portals throughout the procedure to obtain the best angle for suture insertion. This makes the procedure more difficult because viewing from the anteromedial portal provides a less satisfactory view of the tear and makes accurate suture placement challenging. Moreover, these techniques often require additional surgical steps that considerably complicate the procedure, such as relaying of multiple sutures with an increased risk of soft-tissue entrapment.5, 6 Song et al.4 reported a small sample of 15 patients with radial tears extending to the posterior horn of the lateral meniscus repaired with a side-to-side technique, in contrast to more complicated pullout techniques. They reported a 100% clinical success rate, which supports our philosophy of using anchors to repair this kind of lesion.
In the described technique, the use of a central midline portal for instrumentation provides a less tangential approach to the meniscus and direct access for all-inside suture device placement. Furthermore, this allows the anterolateral portal to be used for perfect visualization without the need to switch the arthroscope from the lateral side to the medial side to allow suturing. Our technique also has the advantage of avoiding the lateral tibial spine—both anchors can be easily inserted, under direct vision, without any obstruction. The simplicity afforded by the Gillquist portal makes this technique an important consideration for radial tears within 9 mm of the center of the meniscus root insertion (types II and IV), which are also the most frequent variants. Advantages and disadvantages of the technique are summarized in Table 2.
Table 2.
Advantages and Disadvantages of Repair Technique of Radial Tears of Lateral Meniscus Using Central Midline Portal
| Advantages |
| The approach is less tangential to the lesion. |
| The lateral tibial spine is avoided. |
| The surgeon can easily perform suture placement with 1 hand in a figure-of-4 position. In contrast, in an extreme figure-of-4 position, the proximity of the knee to the operating table may limit access to the anterolateral portal for device insertion. |
| A direct view is achieved, which allows the surgeon to control the quality of the suture. |
| Disadvantages |
| An additional arthroscopic portal is required. |
| There is a theoretical risk of patellar tendinitis. |
| There is a potential risk of anchor migration in the joint in the case of improper anchor seating. |
The use of a central midline accessory portal for full radial PLMRTs makes a previously technically demanding procedure much less challenging. In our experience, it is an easy, safe, and reproducible option without any specific complications.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.T. receives support from Arthrex. B.S-C. receives support from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for suture repair of full radial posterior lateral meniscal tear using central portal. The technique is shown in a right knee undergoing concomitant anterior cruciate ligament reconstruction.
References
- 1.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A., Kelly N., Baad M. Dynamic contact mechanics of radial tears of the lateral meniscus: Implications for treatment. Arthroscopy. 2012;28:372–381. doi: 10.1016/j.arthro.2011.08.287. [DOI] [PubMed] [Google Scholar]
- 3.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 4.Song H.S., Bae T.Y., Park B.Y., Shim J., In Y. Repair of a radial tear in the posterior horn of the lateral meniscus. Knee. 2014;21:1185–1190. doi: 10.1016/j.knee.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 5.Anderson L., Watts M., Shapter O. Repair of radial tears and posterior horn detachments of the lateral meniscus: Minimum 2-year follow-up. Arthroscopy. 2010;26:1625–1632. doi: 10.1016/j.arthro.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Ahn J.H., Lee Y.S., Yoo J.C., Chang M.J., Park S.J., Pae Y.R. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:67–75. doi: 10.1016/j.arthro.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Moulton S.G., Bhatia S., Civitarese D.M., Frank R.M., Dean C.S., LaPrade R.F. Surgical techniques and outcomes of repairing meniscal radial tears: A systematic review. Arthroscopy. 2016;32:1919–1925. doi: 10.1016/j.arthro.2016.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Soejima T., Tabuchi K., Noguchi K. An all-inside repair for full radial posterior lateral meniscus tears. Arthrosc Tech. 2016;5:e133–e138. doi: 10.1016/j.eats.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillquist J., Hagberg G. A new modification of the technique of arthroscopy of the knee joint. Acta Chir Scand. 1976;142:123–130. [PubMed] [Google Scholar]
- 10.Sonnery-Cottet B., Archbold P., Zayni R. High lateral portal for sparing the infrapatellar fat-pad during ACL reconstruction. Orthop Traumatol Surg Res. 2011;97:870–873. doi: 10.1016/j.otsr.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade C.M., Jansson K.S., Dornan G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 12.Padalecki J.R., Jansson K.S., Smith S.D. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 13.West R.V., Kim J.G., Armfield D., Harner C.D. Lateral meniscal root tears associated with anterior cruciate ligament injury: Classification and management (SS-70) Arthroscopy. 2004;20:e32–e33. (abstr) [Google Scholar]
- 14.Brody J.M., Lin H.M., Hulstyn M.J., Tung G.A. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239:805–810. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 15.Cho S., Ko S., Woo J.K. Meniscus-stabilizing function of the meniscofemoral ligament: Experimental study of pig knee joints. Arthroscopy. 2006;22:872–877. doi: 10.1016/j.arthro.2006.04.081. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for suture repair of full radial posterior lateral meniscal tear using central portal. The technique is shown in a right knee undergoing concomitant anterior cruciate ligament reconstruction.