Abstract
Approaches to management of combined anterior cruciate ligament (ACL) and high-grade medial collateral ligament (MCL) injuries remain controversial. Some studies suggest that with grade III MCL injuries, patients may benefit from concurrent MCL reconstruction to restore stability and prevent increased stress on the ACL graft. We present a technique for simultaneous ACL/MCL reconstructions using a single Achilles tendon allograft.
Combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL) injuries are a common knee injury pattern. Though studies have demonstrated favorable results with isolated ACL reconstruction,1, 2 others suggest that surgical treatment of the MCL in combined injuries may be advantageous to avoid chronic valgus instability2 and increased stress on the ACL graft.3, 4, 5, 6 We advocate combined ACL/MCL reconstructions for those with ACL insufficiency and grade 3 MCL injuries. Grade 3 MCL injuries imply injury to the posteromedial knee complex and imply rotatory instability. These injuries are diagnosed preoperatively via MRI and valgus stress tests (3+ laxity at 30° of knee flexion and 1-2+ laxity at full extension) and confirmed intraoperatively with stress radiographs7 and medial compartment gapping greater than 1 cm during arthroscopic examination.8 Although many surgical options have been offered to remedy grade 3 MCL injuries, a recent systematic review failed to demonstrate a clear consensus on the optimal method to treat these high-grade medial-sided knee injuries.9 We present a technique that uses a single allograft to reconstruct the ACL and MCL (Video 1).
Surgical Technique
Preparation allows flexibility needed during combined ACL/MCL reconstructions. A radiolucent table (Mizuho OSI, Union City, CA) facilitates identification of fluoroscopic landmarks. Arthroscopy equipment is positioned toward the operative table's head to allow unencumbered imaging. An Achilles allograft with a 10 × 22-mm bone plug is prepared with a 10-mm-wide, unsutured soft tissue tail.
Patient positioning accommodates 90° of knee flexion and hyperflexion beyond 110°; these positions facilitate ACL footprint orientation and independent ACL femoral tunnel drilling through an anteromedial portal, respectively. To meet these requirements, the operative leg is flexed to 90°, a Schure leg holder (SchureMed, Abington, MA) secures the foot, and a stress post (Mizuho OSI) is placed at the level of the tourniquet. This setup allows for limb external rotation required to access the medial knee during MCL reconstruction.
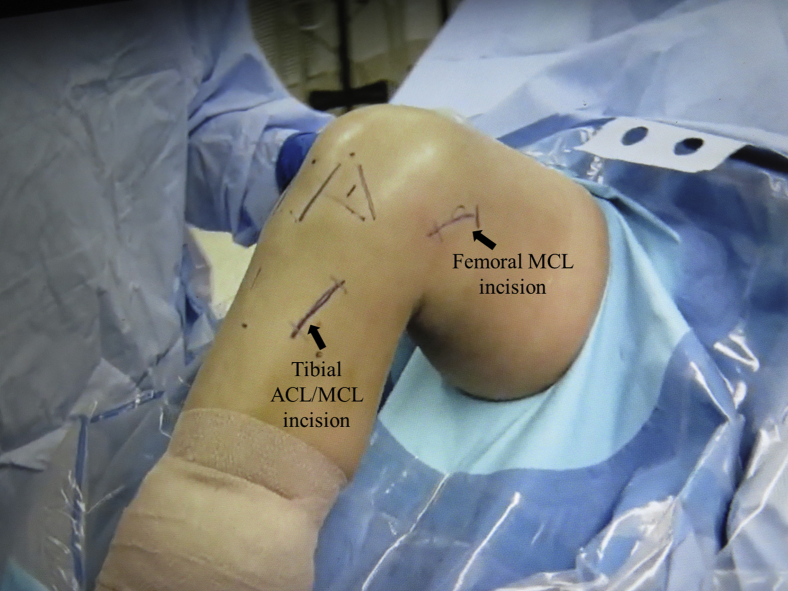
An examination under anesthesia is performed. Increased laxity with valgus stress at 30° of knee flexion suggests injury to the MCL. If valgus laxity persists when the knee is fully extended, injury to the posterior oblique ligament, ACL, and/or posterior cruciate ligament should be suspected. In equivocal cases, stress examination can repeated using fluoroscopy and a Telos stress device (Metax, Hungen, Germany). Increased medial joint widening of 1.7 and 3.2 mm with valgus stress at full extension and 20° of knee flexion, respectively, correlates with a grade III MCL injury.7 Portal sites are selected to ensure that femoral-independent drilling can occur through an anteromedial portal, whereas incisions are positioned over the MCL attachment sites to facilitate tunnel creation (Fig 1). Independent femoral drilling allows creation of a tibial tunnel without regard for femoral tunnel malposition. Although the anterolateral portal remains adjacent to the patellar tendon to allow visualization of the ACL footprints, the anteromedial portal is planned more inferiomedially. The anteromedial portal is established by passing a spinal needle at a trajectory such that it (1) intersects the notch's lateral wall as perpendicular as possible while maintaining space for the reamer to pass the medial femoral condyle and (2) enters the medial compartment inferiorly without injuring the medial meniscus.
Fig 1.
Right knee, exterior view of medial knee. Incisions on the medial side of the knee are centered over the proximal and distal attachments of the MCL. (MCL, medial collateral ligament.)
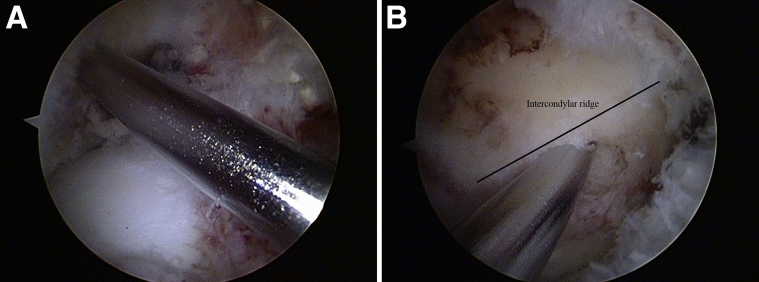
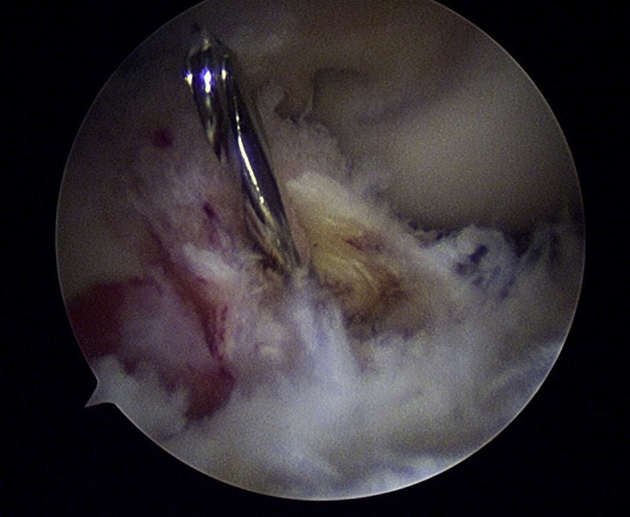
The retained fibers of the ACL footprint serve as a guide for the femoral socket. With the knee flexed at 90°, the center of the debrided footprint is marked using a microfracture awl. Adequate starting position, adjacent to the bifurcate and beneath the intercondylar ridges, is confirmed by reinserting the arthroscope into the anteromedial portal and viewing the notch's lateral wall. With the arthroscope returned to the anterolateral portal, a 2.4-mm Beath-Pin guidewire is inserted through the anteromedial portal and positioned into the microfracture hole (Fig 2). The knee is gently hyperflexed to 110°, and the guidewire is passed from the pilot hole through the lateral femoral condyle. Superolateral pin orientation assisted by knee hyperflexion and levering the pin inferomedially during passage through the condyle reduces the risk of a short femoral tunnel and back-wall compromise during reaming (Fig 3). To avoid iatrogenic injury to the articular cartilage, the 10-mm half-moon acorn reamer is manually introduced over the guidewire and with the blade facing away from the condyle. The tunnel is drilled to a 5-mm depth, and adequacy of the back wall is confirmed prior to completion of the tunnel. The Beath Pin is used to pass a loop of suture through the lateral femoral condyle.
Fig 2.
Right knee, interior view. Prior to reaming, a guidewire is centered within the native femoral insertion site when viewing from the anterolateral (A) and anteromedial (B) portals.
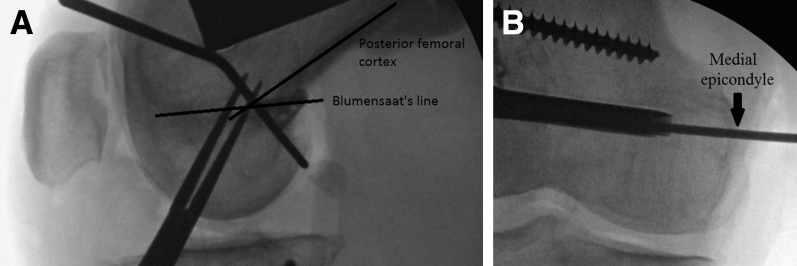
Fig 3.
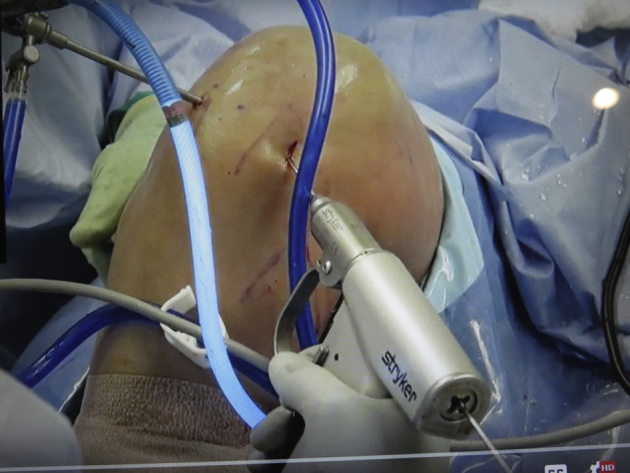
Right knee, exterior view. To avoid an iatrogenically short femoral socket and/or back wall compromise during reaming, the guidewire is manipulated inferomedially while the knee is flexed to 110°.
To accommodate the MCL reconstruction, the skin is incised inferior and posteromedial to the pes anserinus. The dissection is continued until MCL fibers are encountered 7 to 10 cm distal to the joint line. The distal MCL fibers are split longitudinally to expose the MCL's broad tibial insertion. The tip of the aiming guide, set at 60°, is positioned within the center of the ACL tibial footprint. The guide's other end is centered within or slightly proximal to the exposed MCL tibial insertion and assists guidewire passage from the posteromedial tibia into the native ACL tibial footprint (Fig 4). As a result of the aiming guide constraints, a second wire must often be directed freehand distally from the exposed MCL tibial insertion and into the native ACL tibial footprint (Fig 5). The trajectory of this guidewire is much steeper than traditional ACL reconstruction techniques. The guidewire is over-reamed with a 10-mm reamer. The intra-articular suture loop is retrieved out the tibial tunnel.
Fig 4.
Right knee, interior view. Ideally, the guidewire is passed into the center of the native ACL tibial footprint. (ACL, anterior cruciate ligament.)
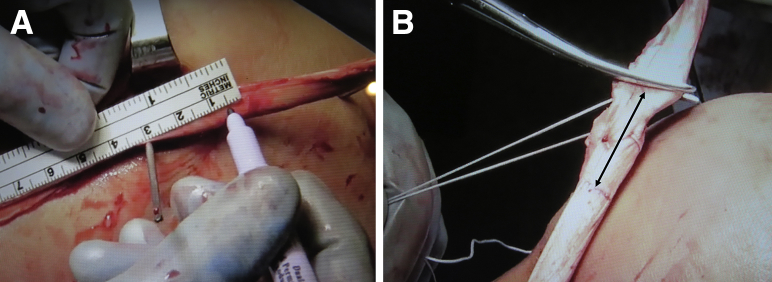
Fig 5.
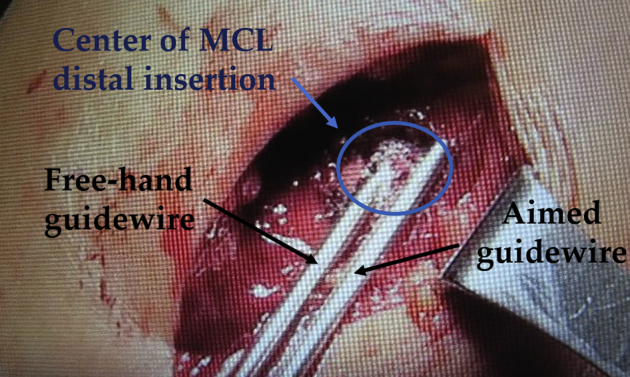
Right knee, exterior view of the proximal medial tibia. The ACL tibial guide often places the guidewire outside the center of the distal superficial MCL insertion. Therefore, a second guidewire must be passed freehand from the center of the distal superficial MCL insertion into the center of the native ACL tibial footprint. (ACL, anterior cruciate ligament; MCL, medial collateral ligament.)
The graft is shuttled retrograde, and the bone plug lodged into the femoral socket. The tunnel is prepared using a tap followed by placement of an interference screw anterior to the graft. The graft tail is grasped with a clamp and cycled. With tension applied to the graft at 20° of knee flexion, an interference screw is inserted posterior to the graft within the tibial tunnel. The excess graft becomes the substrate for the MCL reconstruction.
Identification of the medial epicondyle by palpation and imaging is paramount to MCL femoral tunnel placement (Fig 6). A 4-cm incision is created overlying this bony landmark. Dissection proceeds through layer 1 until the fibers of the superficial MCL are encountered and traced to their proximal attachment. Fluoroscopy assists in identifying the MCL's femoral attachment (Fig 7). Radiographic landmarks for the femoral insertion of the MCL are well documented.10 To determine the isometry of tunnel placement, a suture is held at the tibial tunnel entrance and passed around the guidewire, and the knee is taken through a range of motion. If the suture does not lengthen during ranging, the guidewire is located at the isometric point. If not, the guide pin location is modified until isometry has been attained. Once the femoral attachment site is confirmed, the Beath Pin guidewire is passed from this point across the distal femur. The guidewire is projected proximally and anteriorly to avoid penetration of the notch and the ACL tunnel.
Fig 6.

Right knee, exterior view of the distal medial femur. While the knee is flexed to avoid interference from the contralateral knee, the location of the medial epicodyle is identified fluoroscopically to assist in creation of an incision that allows access to the MCL's femoral attachment site. (MCL, medial collateral ligament.)
Fig 7.
Once the incision had been made, more precise localization of the native MCL attachment site is confirmed using fluoroscopic intersection of the posterior cortex with the Blumensaat line. (MCL, medial collateral ligament.)
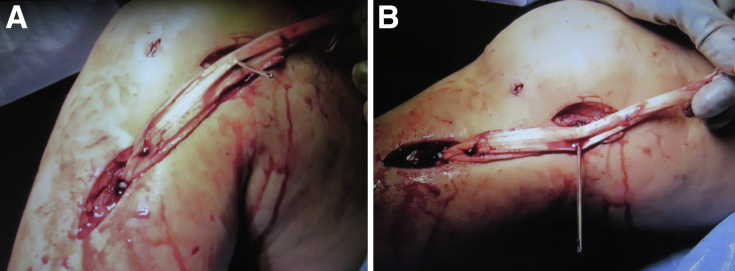
The soft tissue portion of the graft is swung proximally over the wire to (1) identify the length of graft needed and (b) confirm isometry of the graft (Fig 8). A point 25 mm beyond the guidewire is marked and excess graft excised (Fig 9A). The soft tissue remaining beyond the guidewire represents the graft that will be docked into the femoral socket. A no. 2 FiberWire suture (Arthrex, Naples, FL) is woven through this portion of the graft and with both suture tails exiting the end of the graft (Fig 9B).
Fig 8.
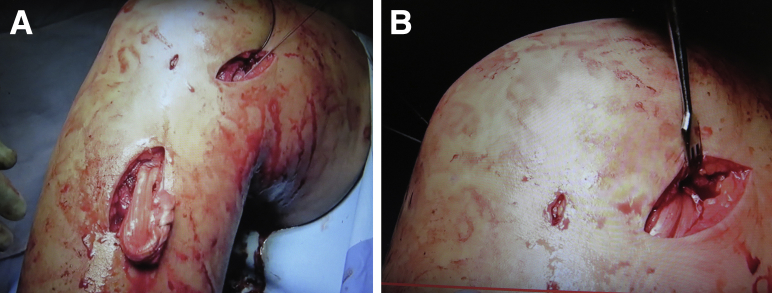
Right medial knee, exterior view. Isometry is confirmed by passing the graft over the wire and taking the knee through flexion (A) and extension (B). If placed isometrically, the graft should not slide or bunch on the wire.
Fig 9.
Right medial knee, exterior view. (A) The graft is marked at a site corresponding to the entrance of the MCL femoral tunnel and 25 mm beyond this point. This region corresponds to the graft that will be inserted into the MCL femoral socket. (B) This section of the graft is prepared with a Bunnell-type suture configuration while the excess graft is excised. (MCL, medial collateral ligament.)
The native MCL remaining around the guidewire is split longitudinally 1 cm proximally and 2 cm distally to allow graft recession. An 8-mm-diameter acorn reamer is used to create a 25-mm-long femoral socket. A looped suture is passed through the tunnel across the condyle to facilitate graft passage.
A curved clamp is passed distally within layer 2 superficial to the native MCL. Once visible within the distal incision, the clamp is opened to create a subcutaneous tunnel for the graft. The graft sutures are grasped and used to pass the graft subcutaneously and into the femoral socket (Fig 10). The graft is tensioned with a laterally directed force with the knee flexed to 30°, cycled, and, with a varus force applied, secured using an interference screw. Pearls and pitfalls of the technique are listed in Table 1.
Fig 10.
Right medial knee, exterior view. The graft is passed subcutaneously and beneath the pes anserinus (A) and lodged into the MCL femoral socket (B). (MCL, medial collateral ligament.)
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The lateral stress post is placed at the level of the tourniquet, while the foot rest is positioned so that the knee is flexed to 90°. The arthroscopy tower is positioned adjacent to the contralateral hip to allow the C-arm to enter the operative field perpendicular to the knee. This arrangement facilitates “perfect lateral” images for fluoroscopic localization of MCL attachment sites. Knee flexion to 110° or more and dropping hand inferomedially during guidewire placement decreases the risk of back wall compromise and an iatrogenically short ACL femoral tunnel. Half-moon reamers or sentinel reamers reduce the risk of iatrogenic injury to the articular cartilage of the medial femoral condyle during creation of the ACL femoral socket. MCL femoral origin can be fluoroscopically localized prior to the incision. This step minimizes the size of the incision and ensures access to the medial epicondyle. Bunnell-suture configuration limits suture potentially getting exposed to the interference screw. Allograft can be placed between and sewn to the remaining fibers of the native MCL. |
Too medial anteromedial portal risks iatrogenic injury to the articular surface of the medial femoral condyle. Too lateral anteromedial portal placement may lead to compromise of the posterior femoral condyle. Anterior and proximal placement of the tibial MCL attachment site can result in nonanatomic MCL reconstruction and pre-mature graft failure. |
ACL, anterior cruciate ligament; MCL, medial collateral ligament.
Postoperative Rehabilitation
Postoperatively, the patient is nonweightbearing for 3 weeks followed by partial weightbearing in an extension brace for the next 3 weeks. The patient is prescribed prophylactic anticoagulant for 2 weeks. Physical therapy including gentle range of motion begins at 2 weeks with motion progression to 90° of flexion by 6 weeks and full flexion by 10 weeks. At 6 weeks postoperatively, full weightbearing begins and the hinged brace is replaced with a short brace. Light jogging is expected to commence by 4 months and return to sports at 6 to 9 months.
Discussion
The use of a single allograft to simultaneously reconstruct the ACL and MCL offers several advantages over traditional techniques (Table 2). Although the use of allograft risks slower biologic incorporation,11 disease transmission,12 and higher failure rates,13 allograft can avoid morbidity associated with harvesting autograft tissue. Simultaneously harvesting the patellar tendon and quadriceps tendon potentially extends the rehabilitation time for full recover of the extensor mechanism and increases the risk of a patella fracture.14 The use of semitendinosus and gracilis tendon autograft eliminates an important medial-sided stabilizer and can restrict the ability of the hamstring to resist anterior tibial translation.14
Table 2.
Advantages/Disadvantages
| Advantages | Disadvantages |
|---|---|
| Single allograft decreases the cost and potential disease transmission. | Technique does not allow for reconstruction of posterior oblique ligament. |
| Single tibial tunnel decreases risk of tunnel convergence and implant costs. | Tibial tunnel can be time consuming to create. |
| Procedure can re-create ACL/MCL through limited incisions. | Acute angle of MCL tibial tunnel may predispose MCL component of graft to fatigue. |
| Allograft use may facilitate more rapid rehabilitation. | The location of the tibial MCL tunnel may be slightly proximal. |
| Allograft use does not compromise secondary stabilizers to anterior translation and/or valgus stresses and eliminates donor site morbidity. | Allograft ACL/MCL reconstruction is subjected to increased risk of graft failure, especially among younger patients. |
ACL, anterior cruciate ligament; MCL, medial collateral ligament.
Using a single allograft (1) reduces potential for disease transmission and (2) eliminates the cost and preparation time associated with using 2 grafts. Technically, the single tibial tunnel technique removes a procedural step and negates the risk of converging or abutting tunnels. Although not scientifically evaluated, the use of a single tibial tunnel potentially limits the location of the tibial insertion of the MCL to a slightly more proximal location. Though our empirical evidence has not demonstrated this reconstruction technique to be problematic, the clinical implications may be an area for future research.
Another potential shortcoming of this technique is its inability to reconstruct the posterior oblique ligament. The importance of re-creating the posterior oblique ligament to restore valgus and anteromedial rotatory stability remains controversial. Studies have demonstrated that although the posterior oblique ligament assumes minimal tension during valgus stress, the ligament plays a key role in limiting internal rotation with the knee in full extension.15 Furthermore, sectioning of the posterior oblique ligament adds further strain to the superficial MCL during external rotation.16 Although a recent systematic review of a heterogenous collection of medial-sided reconstruction techniques suggested that “anatomic” reconstructions have improved subjective and objective outcomes,9 the clinical impact of not separately reconstructing the posterior oblique ligament has not been completely elucidated.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: N.B. received support from the American Academy of Orthopaedic Surgeons (AAOS), as expenses covered for Meetings for AAOS Resident Assembly as part of the Executive Committee. R.A.G. receives institutional support for expert testimony from two different law firms (both depositions were done on behalf of patients involved in worker's compensation claims and all R.A.G. had treated) and research support for phase IV clinical trial from Aesculap; in addition, the following relationships/conditions/circumstances are present: Programming Committee, American Orthopaedic Association and American Association of Orthopaedic Surgeons; Social Media Task Force, Arthroscopy Association of North America; and Council of Delegates, American Orthopaedic Society of Sports Medicine. R.W. receives royalties from Zimmer-Biomet; has stock/stock options in Ivy Sports Medicine, Orthonet, and OrthoSensor. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
The research was performed at the Milton S. Hershey Medical Center, Hershey, Pennsylvania.
Supplementary Data
The patient is positioned with a stress post at the level of the tourniquet and the knee held at 90° of flexion. Examination under anesthesia and diagnostic arthroscopy confirm presence of the ACL and MCL injury on the right knee. The center of the native ACL footprint, adjacent to the bifurcate and beneath the intercondylar ridges, is marked using a microfracture awl. A guidewire is inserted through the anteromedial portal, positioned into the microfracture hole, passed through the lateral femoral condyle, and over-reamed with a half-moon acorn reamer. The center of the distal superficial MCL tibial insertion is identified distal to the pes anserinus. The tip of the aiming guide facilitates passage of a guidewire from the MCL tibial insertion to the native ACL tibial footprint. A second wire must often be directed freehand distally from the center of the exposed MCL tibial insertion and into the native ACL tibial footprint. The guidewire is over-reamed with a 10-mm reamer. The graft is shuttled retrograde through the sockets, the bone plug lodged into the femoral socket, and graft secured with both sockets using interference screws. The medial epicondyle is identified by palpation and fluoroscopic guidance. A guidewire is passed from the center of the native MCL femoral insertion across the distal femur. The excess graft is swung proximally over the guidewire to determine the length of graft needed and confirm isometry of the MCL tunnel placement. The 25 mm of graft beyond the guidewire is prepared using a woven stitch, the graft is sized, and excess graft excised. An acorn reamer is used to create a 25-mm-long femoral socket. The graft is shuttled subcutaneously just superficial to the native MCL and lodged into the femoral socket. After the knee is cycled, the knee is held at 30° of knee flexion and varus stress applied, the tensioned graft is secured within the femoral socket using an interference screw. (ACL, anterior cruciate ligament; MCL, medial collateral ligament.)
References
- 1.Halinen J., Lindahl J., Hirvensalo E., Santavirta S. Operative and non-operative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: A prospective randomized study. Am J Sports Med. 2006;34:1134–1140. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]
- 2.Grant J.A., Tannenbaum E., Miller B.S., Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28:110–122. doi: 10.1016/j.arthro.2011.08.293. [DOI] [PubMed] [Google Scholar]
- 3.Mancini E.J., Kohen R., Esquivel A.O., Cracchiolo A.M., Lemos S.E. Comparison of ACL strain in the MCL-deficient and MCL-reconstructed knee during simulated landing in a cadaveric model. Am J Sports Med. 2017;45:1090–1094. doi: 10.1177/0363546516685312. [DOI] [PubMed] [Google Scholar]
- 4.Ahn J.H., Lee S.H. Risk factors for knee instability after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2936–2942. doi: 10.1007/s00167-015-3568-x. [DOI] [PubMed] [Google Scholar]
- 5.Zaffagnini S., Bignozzi S., Martelli S., Lopomo N., Marcacci M. Does ACL reconstruction restore knee stability in combined lesions? An in vivo study. Clin Orthop Relat Res. 2007;454:95–99. doi: 10.1097/BLO.0b013e31802b4a86. [DOI] [PubMed] [Google Scholar]
- 6.Battaglia M.J., 2nd, Lenhoff M.W., Ehteshami J.R. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: A biomechanical evaluation in a cadaveric model. Am J Sports Med. 2009;37:305–311. doi: 10.1177/0363546508324969. [DOI] [PubMed] [Google Scholar]
- 7.Laprade R.F., Bernhardson A.S., Griffith C.J., Macalena J.A., Wijdicks C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am J Sports Med. 2010;38:330–338. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 8.Wilson T.C., Satterfield W.H., Johnson D.L. Medial collateral ligament “tibial” injuries: Indication for acute repair. Orthopedics. 2004;27:389–393. doi: 10.3928/0147-7447-20040401-15. [DOI] [PubMed] [Google Scholar]
- 9.DeLong J.M., Waterman B.R. Surgical techniques for the reconstruction of medial collateral ligament and posteromedial corner injuries of the knee: A systematic review. Arthroscopy. 2015;31:2258–2272.e1. doi: 10.1016/j.arthro.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Wijdicks C.A., Griffith C.J., LaPrade R.F. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. 2009;91:521–529. doi: 10.2106/JBJS.H.00909. [DOI] [PubMed] [Google Scholar]
- 11.Bhatia S., Bell R., Frank R.M. Bony incorporation of soft tissue anterior cruciate ligament grafts in an animal model: Autograft versus allograft with low-dose gamma irradiation. Am J Sports Med. 2012;40:1789–1798. doi: 10.1177/0363546511435637. [DOI] [PubMed] [Google Scholar]
- 12.Mroz T.E., Joyce M.J., Steinmetz M.P., Lieberman I.H., Wang J.C. Musculoskeletal allograft risks and recalls in the United States. J Am Acad Orthop Surg. 2008;16:559–565. doi: 10.5435/00124635-200810000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., MOON Consortium, Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hetsroni I., Mann G. Combined reconstruction of the medial collateral ligament and anterior cruciate ligament using ipsilateral quadriceps tendon-bone and bone-patellar tendon-bone autografts. Arthrosc Tech. 2016;5:e579–e587. doi: 10.1016/j.eats.2016.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffith C.J., Wijdicks C.A., LaPrade R.F., Armitage B.M., Johansen S., Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. 2009;37:140–148. doi: 10.1177/0363546508322890. [DOI] [PubMed] [Google Scholar]
- 16.Wijdicks C.A., Griffith C.J., LaPrade R.F. Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med. 2009;37:1771–1776. doi: 10.1177/0363546509335191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned with a stress post at the level of the tourniquet and the knee held at 90° of flexion. Examination under anesthesia and diagnostic arthroscopy confirm presence of the ACL and MCL injury on the right knee. The center of the native ACL footprint, adjacent to the bifurcate and beneath the intercondylar ridges, is marked using a microfracture awl. A guidewire is inserted through the anteromedial portal, positioned into the microfracture hole, passed through the lateral femoral condyle, and over-reamed with a half-moon acorn reamer. The center of the distal superficial MCL tibial insertion is identified distal to the pes anserinus. The tip of the aiming guide facilitates passage of a guidewire from the MCL tibial insertion to the native ACL tibial footprint. A second wire must often be directed freehand distally from the center of the exposed MCL tibial insertion and into the native ACL tibial footprint. The guidewire is over-reamed with a 10-mm reamer. The graft is shuttled retrograde through the sockets, the bone plug lodged into the femoral socket, and graft secured with both sockets using interference screws. The medial epicondyle is identified by palpation and fluoroscopic guidance. A guidewire is passed from the center of the native MCL femoral insertion across the distal femur. The excess graft is swung proximally over the guidewire to determine the length of graft needed and confirm isometry of the MCL tunnel placement. The 25 mm of graft beyond the guidewire is prepared using a woven stitch, the graft is sized, and excess graft excised. An acorn reamer is used to create a 25-mm-long femoral socket. The graft is shuttled subcutaneously just superficial to the native MCL and lodged into the femoral socket. After the knee is cycled, the knee is held at 30° of knee flexion and varus stress applied, the tensioned graft is secured within the femoral socket using an interference screw. (ACL, anterior cruciate ligament; MCL, medial collateral ligament.)